Abstract
Background and purpose Hemiarthroplasty as treatment for femoral neck fractures has increased markedly in Sweden during the last decade. In this prospective observational study, we wanted to identify risk factors for reoperation in modular hemiarthroplasties and to evaluate mortality in this patient group.
Patients and methods We assessed 23,509 procedures from the Swedish Hip Arthroplasty Register using the most common surgical approaches with modular uni- or bipolar hemiarthroplasties related to fractures in the period 2005–2010. Completeness of registration (individual procedures) was 89–96%. The median age was 85 years and the median follow-up time was 18 months.
Results 3.8% underwent reoperation (any further hip surgery), most often because of implant dislocation or infection. The risk of reoperation (Cox regression) was higher for uncemented stems (hazard ratio (HR) = 1.5), mainly because of periprosthetic femoral fractures. Bipolar implants had a higher risk of reoperation irrespective of cause (HR = 1.3), because of dislocation (1.4), because of infection (1.3), and because of periprosthetic fracture (1.7). The risk of reoperation due to acetabular erosion was lower (0.30) than for unipolar implants, but reoperation for this complication was rare (1.7 per thousand). Procedures resulting from failed internal fixation had a more than doubled risk; the risk was also higher for males and for younger patients. The surgical approach had no influence on the risk of reoperation generally, but the anterolateral transgluteal approach was associated with a lower risk of reoperation due to dislocation (HR = 0.7). At 1 year, the mortality was 24%. Men had a higher risk of death than women (1.8).
Interpretation We recommend cemented hemiarthroplasties and the anterolateral transgluteal approach. We also suggest that unipolar implants should be used, at least for the oldest and frailest patients.
During the last decade, there has been a remarkable increase in hemiarthroplasties as treatment for the approximately 6,500 individuals in Sweden each year who sustain displaced femoral neck fractures. In 1998, only 3% were treated with hemiarthroplasty whereas in 2010 the proportion had increased to 61% (Swedish National Board of Health and Welfare, CitationThorngren 2011). Since 2005, the Swedish Hip Arthroplasty Register (SHAR) has been recording hemiarthroplasty procedures nationally.
The main reason for receiving a hemiarthroplasty is a femoral neck fracture, and the patients are generally elderly and frail. In 2005, a wide range of implant types and brands were in use. With increasing knowledge from clinical trials (Jalovaara and Virkkunen Citation1991, Ravikumar and Marsh Citation2000, Blomfeldt et al. Citation2005) and national hemiarthroplasty registers, the use of a number of implants—mainly monoblock-type—has decreased and has now almost stopped (Leonardsson et al. Citation2012). In the few countries with national hemiarthroplasty registration (and with reports on hemiarthroplasty head type), most of the implants used today are modular unipolar or bipolar (Rogmark et al. Citation2010, Furnes and Gjertsen Citation2011, CitationGarellick et al. 2011, Graves et al. Citation2011).
In this prospective observational study, we wanted to identify risk factors for reoperation in modular hemiarthroplasties. Any further hip surgery after a hemiarthroplasty is strenuous for an ageing patient. Whether or not the procedure is related to the implant itself is probably of minor importance to the patient in comparison to the general peroperative stress. In view of this, we chose any reoperation as our endpoint. Our second aim was to evaluate postoperative mortality in patients treated with hemiarthroplasty.
Patients and methods
The SHAR has 100% coverage regarding clinics performing hemiarthroplasty surgery in Sweden. In 2005, the completeness of procedures was 89% and from 2006 through 2010 it was 96% (Garellick et al. Citation2011, Leonardsson et al. Citation2012). The data are collected by a contact secretary at each clinic and sent to the SHAR through the internet. Hemiarthroplasty procedures are included in the SHAR irrespective of diagnosis. In addition to diagnoses and clinical data, surgical details (i.e. surgical approach, type of implant and fixation) are recorded. Cognitive impairment is classified by the surgeon simply as “none”, “suspected”, or “evident”. The SHAR also registers reoperations (any further open surgery of the hip), including open reductions of dislocated hemiarthroplasties, and revisions (reoperation with exchange or removal of any of the components or the entire prosthesis).
In accordance with Swedish law, all patients receive information and are free to withdraw their participation in the registration at any point. All records in the SHAR are linked to the patients by the individual and unique 10-digit identity number given to all Swedish citizens at birth and to immigrants after entering the country.
25,913 hemiarthroplasty procedures were recorded in the SHAR from 2005 through 2010. Inclusion criteria for this study were a fracture-related hemiarthroplasty (acute fracture or secondary procedure after failed internal fixation) and use of a modular unipolar or bipolar implant. Consequently, monoblock-type implants (i.e. Austin-Moore, Thompson, and ETS Endo) were excluded. Also, 19 Austin-Moore stems with modular heads were excluded. In addition, we included only procedures performed with one of the predominant surgical approaches (Leonardsson et al. Citation2012), i.e. the anterolateral transgluteal approach with the patient in a lateral position (Gammer Citation1985), the anterolateral transgluteal approach with the patient in a supine position (Hardinge Citation1982), and the posterior approach with the patient in a lateral position (Moore Citation1957). After exclusion of 2,404 cases that did not meet the inclusion criteria, 23,509 procedures in 22,642 patients were eligible for the study (867 patients had bilateral hemiarthroplasties during the study period).
71% of the procedures were performed on women. Median age at the time of surgery was 85 (42–104) years for women and 84 (19–105) years for men. Most procedures were performed on patients over 75 years (). Acute fractures accounted for 95% (n = 22,441) of the procedures, including femoral neck fractures (n = 22,109) and other fractures of the hip and femur (n = 332).
Table 1. Number of procedures (%) performed on patients in the different age groups
The Gammer and the Moore surgical approaches predominated (41% and 49%, respectively), whereas only a small proportion were performed by the Hardinge approach (10%). Slightly more than half of the hemiarthroplasties were bipolar and 97% of the implants were cemented. The Lubinus SP II and the Exeter polished stems were the most commonly used cemented stems whereas the Corail collarless was the most used uncemented stem. The Mega Caput (in Sweden, recently renamed the LINK Unipolar head) and the Vario Cup were the most used unipolar and bipolar implant heads (). The majority of uncemented stems (73%) were implanted with bipolar heads, most often using the Ultima Monk design.
Table 2. The most common stems and implant heads in the different groups
Completeness regarding ASA grade and classification of cognitive impairment, as previously described (Leonardsson et al. Citation2012), increased during the study period, reaching 78% and 86% in 2008, 88% and 86% in 2009, and 91% and 89% in 2010. For our calculations, we used only the available ASA and cognitive impairment data from 2008 through 2010. A larger proportion of men than women were ASA grade 3 and 4 (). The patients were followed until death or December 31, 2010, whichever came first. The median follow-up time was 18 (0–72) months. The patients who were still alive at the end of the study had a median follow-up time of 24 (0–72) months.
Table 3. ASA grade and classification of cognitive impairment 2008–2010 (number of procedures (%))
Statistics
For the statistical calculations, we used the computer software PASW Statistics 18 (IBM Corp., Somers, NY). The patients were stratified into 3 age groups: less than 75 years, 75 to 85 years, and more than 85 years at the time of surgery. Cox regression analyses on reoperation (generally, and for the 4 most common reasons for reoperation) were performed with covariates including age group, sex, diagnosis (acute fracture or secondary procedure after failed internal fixation), type of stem (uncemented, cemented polished, or cemented matte), type of implant head (unipolar or bipolar), and surgical approach. The 2 anterolateral transgluteal approaches (Gammer and Hardinge) were combined in the Cox regression calculations. A separate Cox regression analysis was carried out including only procedures from 2008 through 2010. In addition to the above-mentioned covariates, this analysis also included ASA grade and classification of cognitive impairment. Because of the uneven distribution between the ASA grades, healthy patients and patients with mild systemic disease (grades 1 and 2) were assigned to one group in the regression analyses, as were patients classified as grades 3, 4, and 5 (patients with severe systemic disease, patients with severe systemic disease that is a constant threat to life, and moribund patients). Similarly, patients classified as having suspected and evident cognitive impairment were analyzed as one group. Mortality was calculated regardless of whether or not the patients had been reoperated. The 1-year mortality risk was calculated in a Cox regression analysis, with the covariates age group, sex, implant fixation (cemented or uncemented), ASA grade, and classification of cognitive impairment. This analysis included only procedures from 2008 through 2010. Our calculations included hazard ratios, the chi-square test, and 95% confidence intervals (CIs). We also performed a survival analysis according to Kaplan-Meier up to 5 years, and for comparison we used log-rank test. The limit for significance was set at p ≤ 0.05. Log-minus-log plots were evaluated, and the assumption of proportional hazards was fulfilled.
Results
888 reoperations (3.8%) were performed during the study period and 715 of these (3.0%) were revisions (). The most common reasons for reoperation and revision were implant dislocation and infection, accounting for three-quarters of the procedures (). Of the 41 reoperations due to acetabular erosion, 29 were on unipolar implants and 12 were on bipolar implants.
Table 4. Number (%) of reoperations and revisions in different categories
Table 5. Numbers and causes of reoperations and revisions
Reoperation for any reason
The Cox regression analysis () using reoperation for any reason as endpoint revealed a higher risk for males than for females (HR = 1.2, CI: 1.06–1.4). Hemiarthroplasties performed secondary to failed internal fixation had a more than doubled risk of reoperation (2.1; 1.7–2.6). Patients in the 2 younger age groups had higher risk of reoperation than those in the oldest age group (HR = 1.8, CI: 1.5–2.2; and HR = 1.2, CI: 1.0–1.3). The risk for uncemented stems was 1.5 (CI: 1.1–2.1) times higher than that for cemented matte stems, whereas bipolar implant heads were associated with a 1.3 (CI: 1.1–1.5) times higher risk of reoperation than unipolar. A survival analysis for reoperation of unipolar and bipolar implants is shown in Figure 1. The surgical approach did not significantly influence the risk of reoperation for any reason (CI: 0.80–1.06).
Figure. Proportion not reoperated
Survival analysis (Kaplan-Meier) regarding reoperation for patients treated with unipolar and bipolar hemiarthroplasties, with 95% confidence intervals.
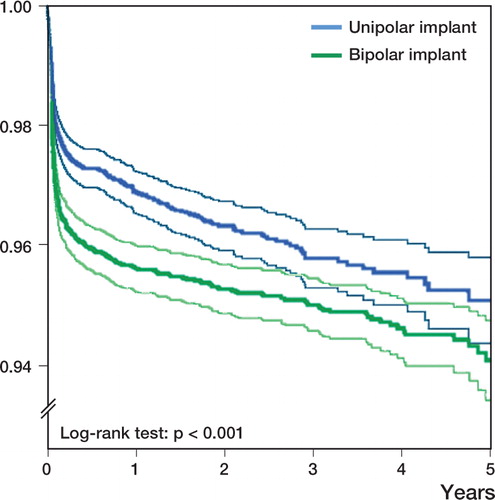
Table 6. Hazard ratios (Cox regression analysis) with 95% CIs for reoperation generally and for specific reasons
Reoperation for specific reasons
The risk of reoperation because of implant dislocation was higher in hemiarthroplasty procedures performed after failed internal fixation (HR = 2.5, CI: 1.8–3.8) than in those performed for acute fracture, and the risk was also higher for patients less than 75 years old (HR = 1.7, CI: 1.2–2.3) than for those older than 85 years. Cemented polished stems had a lower risk than cemented matte stems (HR = 0.65, CI: 0.52–0.81), whereas the use of bipolar implant heads instead of unipolar heads increased the risk by 1.4 (CI: 1.1–1.8) times. Use of an anterolateral transgluteal surgical approach gave a lower risk of this complication (HR = 0.72, CI: 0.58–0.89).
The risk of reoperation because of infection was 2.6 (CI: 1.8–3.8) times higher for hemiarthroplasties performed after failed internal fixation, and almost twice as high for patients less than 75 years of age (HR = 1.8, CI: 1.2–2.5) compared to those older than 85 years. The use of a bipolar head also tended to be associated with this complication (HR = 1.3, CI: 1.0–1.7).
The risk of reoperation because of fracture was more than doubled in men (HR = 2.2, CI: 1.5–3.0); uncemented implants and cemented polished stems proved to be particularly strong risk factors compared to cemented matte stems (HR = 20, CI: 9–44; and HR = 13, CI: 7–25). A bipolar implant head had a 1.7 (CI: 1.1–2.5) times higher risk than a unipolar head.
The risk of reoperation because of acetabular erosion was higher for the 2 younger age groups compared to patients older than 85 years (HR = 46, CI: 6–355; and HR = 20, CI: 3–144) whereas bipolar implant heads had substantially lower risk than unipolar (HR = 0.30, CI: 0.15–0.61).
Reoperation—with ASA grade and cognitive impairment included
In a separate analysis of procedures performed from 2008 through 2010 with covariates including ASA grade and classification of cognitive impairment in addition to the above-mentioned ones, neither ASA grade nor classification of cognitive impairment was identified as a statistically significant risk factor for reoperation. This was also the case after subgroup analysis of the different reasons for reoperation.
Mortality
The 1-year mortality was 24%, and at the end of the study period 44% of the patients had died. Men had a higher mortality than women at one year (32% vs. 20%; p < 0.001) and at the end of the study period (53% vs. 40%; p < 0.001) (). A Cox regression analysis including patients operated from 2008 through 2010 revealed a 1.8 (CI: 1.6–1.9) times higher risk of death during the first postoperative year for men. The method of implant fixation was not a statistically significant risk factor ().
Table 7. Number of patients (%) who had died at 1 year postoperatively and at the end of the study period (n = 22,642)
Table 8. Hazard ratios (Cox regression analysis) with 95% CI for mortality during the first postoperative year, including patients operated from 2008 through 2010 (valid number of patients in the analysis = 9,679)
Discussion
We found a number of factors that influenced the risk of reoperation after hemiarthroplasty. The most important findings were the higher risk of reoperation for patients with bipolar implant heads and for those with uncemented implants.
The higher risk for bipolar implant heads might indicate some general problems with these implants. Prolonged surgery time due to assembly of the bipolar head may play a role. This finding could be incidental, or related to some unknown confounder. It is, however, in agreement with previous analyses from the Register on different stem-head combinations (Garellick et al. Citation2010), which showed an increased risk of revision for bipolar hemiarthroplasty compared to unipolar, using the same stem (Lubinus and Exeter stems with their unipolar and bipolar heads, respectively). Register analyses have also shown a higher risk of reoperation because of dislocation for the Vario Cup implant head (which accounts for almost half of the bipolar heads) compared to other bipolar implant heads (Garellick et al. Citation2010).
Our results contrast with the experience from the Australian National Joint Replacement Registry, where bipolar implants have had a lower risk of revision than unipolar implants, at least in younger patients after long follow-up (Graves et al. Citation2011). This might be attributable to differences between the hemiarthroplasty populations in Australia and Sweden regarding the case-mix in the different age groups.
On the other hand, patients operated with unipolar heads were more likely to undergo reoperation due to acetabular erosion. The total rate of erosion requiring surgery was very low, however, at only 1.7 per thousand. As erosion is mainly a long-term problem, the concern about this complication may be more legitimate in a younger patient group with longer remaining life expectancy. We only assessed acetabular erosions that lead to reoperation, and lack information about patients who might have symptoms from erosion, which for various reasons do not lead to surgery. The total number of patients with erosion may be higher than the rate we observed (Baker et al. Citation2006, Hedbeck et al. Citation2011). Patient-reported outcomes, e.g. hip function and pain, were not addressed in the present study. In all, based on our findings, unipolar implant heads appear to be the most advantageous ones, at least for the majority of patients, who have a relatively short remaining life expectancy. In Sweden, the retail price of the most common bipolar heads (i.e. Vario Cup and UHR Universal Head) is at least 50% higher than that of the corresponding unipolar heads (Mega Caput and V40 Unipolar). This higher cost might be motivated for patients with a relatively long remaining life expectancy, but this remains to be shown.
In addition to implant heads, the stems also had an influence on the reoperation risk. Uncemented implants had a 50% higher risk of reoperation than cemented matte implants, mainly due to fracture. This is in accordance with reports from the Australian National Joint Replacement Registry (Graves et al. Citation2011). There have been few randomized trials comparing cemented and uncemented hemiarthroplasties, and only 3 assessing contemporary uncemented implants. In 2 of these, no statistically significant differences were seen regarding hip function or major complications such as reoperation (Figved et al. Citation2009, Deangelis et al. Citation2012). One recent study showed higher rates of complications and periprosthetic fractures and also a poorer early functional outcome for uncemented stems (Taylor et al. Citation2012). In all 3 studies, mortality was similar in the 2 groups.
The designs of the different brands of cemented polished stems are similar, with a straight stem shape in most cases, whereas the matte ones differ somewhat within the group—with both straight and curved stems. The substantially higher risk of reoperation because of fracture for the polished stems has been reported previously (Lindahl et al. Citation2005, Garellick et al. Citation2010). Of the matte stems, the curved Lubinus SPII accounted for 78% in the present study. Only 10 of the 10,816 patients operated with this stem sustained periprosthetic fractures that led to reoperation. The lower risk of reoperation because of implant dislocation for polished stems may be related to the distribution of implant heads—which differ between matte and polished stems—rather than being related to the stem design itself.
Hemiarthroplasty surgery performed as a secondary procedure after failed internal fixation was associated with a more than doubled risk of reoperation regardless of reason, as well as when due to dislocation and infection. This is in accordance with the findings of Frihagen et al. (Citation2007), although the statistical power in that study was too low to reach significance for the different reasons for reoperation.
The surgical approach had no statistically significant influence on the risk of reoperation in general. However, the anterolateral transgluteal approach had a lower risk of reoperation due to dislocation than the posterior approach, a finding that matches previous reports (Varley and Parker Citation2004, Enocson et al. Citation2008). Notably, closed reductions of dislocated arthroplasties are not recorded in the SHAR. Thus, the true number of implant dislocations is greater than the number in this study. Recurrent dislocation in particular can affect the elderly patient for a long time, and is a potential cause of persistent reduction in health-related quality of life (Enocson et al. Citation2009). Our findings suggest that the anterolateral transgluteal surgical approach should be recommended for hemiarthroplasty procedures.
The younger age groups at the time of fracture had higher risk of reoperation irrespective of cause—and also because of implant dislocation, infection, and acetabular erosion. A younger patient with a more active lifestyle may be more at risk of dislocation and acetabular erosion. Surgeons might also be more inclined to use nonoperative treatment for elderly patients than for younger patients. Apart from this, higher age may protect the patient from complications and reoperation because of shorter remaining lifetime.
Males had a higher risk of reoperation, mainly due to fracture. This is in accordance with reports from Australia, at least for unipolar hemiarthroplasties (Graves et al. Citation2011).
Consistent with previous reports, male hip fracture patients also had higher mortality than female patients (Soderqvist et al. Citation2009, Kannegaard et al. Citation2010, Sterling Citation2011). Even when we adjusted for ASA grade and classification of cognitive impairment, the mortality risk was still higher in men.
The method of fixation was not a risk factor for mortality during the first postoperative year. In a recent registry study, the risk of death was higher with cemented hemiarthroplasties in the first postoperative day, but at 1 week, 1 month, and 1 year postoperatively the risk was higher with uncemented implants (Costain et al. Citation2011).
Altogether, the choice of implant and technique can be somewhat of an orthopedic cruise between Scylla and Charybdis; the choice leading to a lower risk of one complication also leads to a higher risk of another. This means that we need to rank the different complications in terms of importance, taking into account the frequency of the complication, the magnitude of the increase in risk, and how severe the particular complication is to the patient.
One limitation to a nationwide registration is the issue of selection bias, with possible unknown confounders. Also so far no patient-reported outcomes have been registered. There could certainly be a number of patients with complications or symptoms that do not result in surgery. Another type of bias might be related to individual selection of implants and surgical technique at the different hospitals. 30 of 65 hospitals used only either bipolar or unipolar implants; four hospitals accounted for 72% of the total number of uncemented stems, whereas the majority of the units (47) contributed with cases that were operated using either approach (anterolateral or posterior). The observation of diversity related to operating unit is common in registry studies and difficult to handle, because some hospitals may use a uniform treatment algorithm, e.g. the same implant type, fixation, and surgical approach for all patients. The large number of operating units, many of them using several alternatives, should at least partially compensate for this problem. Also, especially after the first 2 years of the registration, completeness of reporting by the different hospitals is highly consistent, with only a few units reporting less than 90% of cases—thus reducing the risk of skewed results due to different reporting rates. Some hospitals may not, however, report all their reoperations even though they do have routines for this. Finally, the classification of cognitive impairment is not done according to a validated form. Instead, the patients are graded by the surgeon based on the patient’s appearance and records of previous investigations of cognitive impairment. There is a risk that some patients may be incorrectly classified as having evident or suspected cognitive impairment as a result of a transient confusion related to the injury.
The strengths of this prospective observational study are the large number of patients and the high degree of completeness.
In summary, we recognize that methodologically, register studies are observational and hypothesis generating. Nonetheless, our findings indicate that there is a problem with bipolar implants, leading to a higher risk of reoperation. The reason for this is currently unclear and requires further investigation. Unipolar hemiarthroplasty appears advantageous, at least for the oldest patients with short remaining life expectancy and thus a minor risk of acetabular erosion. Cemented implants are associated with lower risk of reoperation in hip fracture patients, suggesting that they should be preferred—together with the anterolateral transgluteal surgical approach in order to reduce the risk of dislocation.
OL: principal author of the manuscript, general planning, and calculation and interpretation of data. JK, KÅ, GG, CR: general planning, scientific advice, interpretation of data, and review of the manuscript. All authors read and approved the final manuscript.
This work was supported by grants from the Swedish Research Council, the Greta and Johan Kock Foundation, the H. Järnhardt Foundation, the Malmö University Hospital Research Foundation, and the Research and Development Council of Region Skåne, Sweden.
We thank Ms Kajsa Erikson, Ms Karin Pettersson, and Ms Karin Lindborg for their invaluable efforts in the Swedish Hip Arthroplasty Register and Mr Jan Åke Nilsson for statistical support and advice. We also thank all the reporting clinics in Sweden.
No competing interests declared.
Notes
- Baker RP, Squires B, Gargan MF, Bannister GC. Total hip arthroplasty and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck. A randomized, controlled trial. J Bone Joint Surg (Am) 2006; 88 (12):2583-9.
- Blomfeldt R, Tornkvist H, Ponzer S, Soderqvist A, Tidermark J. Internal fixation versus hemiarthroplasty for displaced fractures of the femoral neck in elderly patients with severe cognitive impairment. J Bone Joint Surg (Br) 2005; 87 (4):523-9.
- Costain DJ, Whitehouse SL, Pratt NL, Graves SE, Ryan P, Crawford RW. Perioperative mortality after hemiarthroplasty related to fixation method. Acta Orthop 2011; 82 (3): 275-81.
- Deangelis JP, Ademi A, Staff I, Lewis CG. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: A prospective randomized trial with early follow-up. Journal of orthopaedic trauma. 2012; 26 (3):135-40.
- Enocson A, Tidermark J, Tornkvist H, Lapidus LJ. Dislocation of hemiarthroplasty after femoral neck fracture: Better outcome after the anterolateral approach in a prospective cohort study on 739 consecutive hips. Acta Orthop 2008; 79 (2): 211-7.
- Enocson A, Pettersson H, Ponzer S, Tornkvist H, Dalen N, Tidermark J. Quality of life after dislocation of hip arthroplasty: A prospective cohort study on 319 patients with femoral neck fractures with a one-year follow-up. Qual Life Res 2009; 18 (9): 1177-84.
- Figved W, Opland V, Frihagen F, Jervidalo T, Madsen JE, Nordsletten L. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures. Clin Orthop 2009; (467) (9):2426-35.
- Frihagen F, Madsen JE, Aksnes E, Bakken HN, Maehlum T, Walloe A, Comparison of re-operation rates following primary and secondary hemiarthroplasty of the hip. Injury 2007; 38 (7): 815-9.
- Furnes O, Gjertsen JE. Norwegian Arthroplasty Register/Norwegian Hip Fracture Register. Annual report 2011 2011;http://nrlweb.ihelse.net/Rapporter/Rapport2011.pdf.
- Gammer W. A modified lateroanterior approach in operations for hip arthroplasty. Clin Orthop 1985; (199): 169-72.
- Garellick G, Kärrholm J, Herberts P. Swedish Hip Arthroplasty Register. Annual report 2009 2010; http://www.shpr.se/Libraries/Documents/AnnualReport-2009.sflb.ashx.
- Garellick G, Kärrholm J, Rogmark C. Swedish Hip Arthroplasty Register. Annual report 2010 2011; http://www.shpr.se/Libraries/Documents/AnnualReport-2010-3.sflb.ashx.
- Graves S, Davidson D, de Steiger R. AOA National Joint Replacement Registry. Annual report 2011 2011; http://www.dmac.adelaide.edu.au/aoanjrr/documents/AnnualReports2011/AnnualReport_2011_WebVersion.pdf.
- Hardinge K. The direct lateral approach to the hip. J Bone Joint Surg (Br) 1982; 64 (1):17-9.
- Hedbeck CJ, Blomfeldt R, Lapidus G, Tornkvist H, Ponzer S, Tidermark J. Unipolar hemiarthroplasty versus bipolar hemiarthroplasty in the most elderly patients with displaced femoral neck fractures: A randomised, controlled trial. Int Orthop 2011; 35 (11): 1703-11.
- Jalovaara P, Virkkunen H. Quality of life after primary hemiarthroplasty for femoral neck fracture. 6-year follow-up of 185 patients. Acta Orthop Scand 1991; 62 (3): 208-17.
- Kannegaard PN, van der Mark S, Eiken P, Abrahamsen B. Excess mortality in men compared with women following a hip fracture. National analysis of comedications, comorbidity and survival. Age Ageing 2010; 39 (2): 203-9.
- Leonardsson O, Garellick G, Kärrholm J, Åkesson K, Rogmark C. Changes in implant choice and surgical technique for hemiarthroplasty. 21,346 procedures from the Swedish Hip Arthroplasty Register 2005-2009. Acta Orthop 2012; 83 (1): 7-13.
- Lindahl H, Malchau H, Herberts P, Garellick G. Periprosthetic femoral fractures classification and demographics of 1049 periprosthetic femoral fractures from the swedish national hip arthroplasty register. J Arthroplasty 2005; 20 (7): 857-65.
- Moore AT. The self-locking metal hip prosthesis. J Bone Joint Surg (Am) 1957; 39 (4):811-27.
- Ravikumar KJ, Marsh G. Internal fixation versus hemiarthroplasty versus total hip arthroplasty for displaced subcapital fractures of femur--13 year results of a prospective randomised study. Injury 2000; 31 (10): 793-7.
- Rogmark C, Spetz CL, Garellick G. More intramedullary nails and arthroplasties for treatment of hip fractures in Sweden. Acta Orthop 2010; 81 (5): 588-92.
- Soderqvist A, Ekstrom W, Ponzer S, Pettersson H, Cederholm T, Dalen N, Prediction of mortality in elderly patients with hip fractures: A two-year prospective study of 1,944 patients. Gerontology 2009; 55 (5): 496-504.
- Sterling RS. Gender and race/ethnicity differences in hip fracture incidence, morbidity, mortality, and function. Clin Orthop 2011; (469): 1913-8.
- Swedish National Board of Health and Welfare. [cited 2012 Mar 15] http://www.socialstyrelsen.se/english
- Taylor F, Wright M, Zhu M. Hemiarthroplasty of the hip with and without cement: A randomized clinical trial. J Bone Joint Surg (Am) 2012; 94 (7):577-83.
- Thorngren KG. National Hip Fracture Register – Rikshöft. Annual report 2010 2011; http://rikshoft.se/se/images/stories/arsrapporter/arsrapport2010.pdf.
- Varley J, Parker MJ. Stability of hip hemiarthroplasties. Int Orthop 2004; 28 (5): 274-7.