Abstract
Background and purpose Revision total hip arthroplasty (THA) due to recurrent dislocations is associated with a high risk of persistent instability. We hypothesized that the use of dual-mobility cups would reduce the risk of re-revision due to dislocation after revision THA.
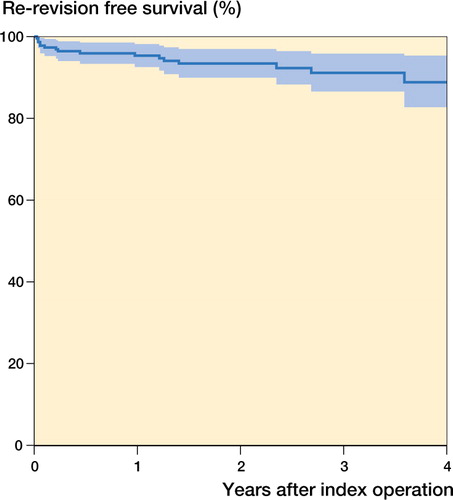
Patients and methods 228 THA cup revisions (in 228 patients) performed due to recurrent dislocations and employing a specific dual-mobility cup (Avantage) were identified in the Swedish Hip Arthroplasty Register. Kaplan-Meier survival analysis was performed with re-revision due to dislocation as the primary endpoint and re-revision for any reason as the secondary endpoint. Cox regression models were fitted in order to calculate the influence of various covariates on the risk of re-revision.
Results 58 patients (25%) had been revised at least once prior to the index cup revision. The surgical approach at the index cup revision was lateral in 99 cases (44%) and posterior in 124 cases (56%). Median follow-up was 2 (0–6) years after the index cup revision, and by then 18 patients (8%) had been re-revised for any reason. Of these, 4 patients (2%) had been re-revised due to dislocation. Survival after 2 years with the endpoint revision of any component due to dislocation was 99% (95% CI: 97–100), and it was 93% (CI: 90–97) with the endpoint revision of any component for any reason. Risk factors for subsequent re-revision for any reason were age between 50–59 years at the time of the index cup revision (risk ratio (RR) = 5 when compared with age > 75, CI: 1–23) and previous revision surgery to the relevant joint (RR = 1.7 per previous revision, CI: 1–3).
Interpretation The risk of re-revision due to dislocation after insertion of dual-mobility cups during revision THA performed for recurrent dislocations appears to be low in the short term. Since most dislocations occur early after revision THA, we believe that this device adequately addresses the problem of recurrent instability. Younger age and prior hip revision surgery are risk factors for further revision surgery. However, problems such as potentially increased liner wear and subsequent aseptic loosening may be associated with the use of such devices in the long term.
Treatment of repeated dislocations after total hip arthroplasty (THA) is challenging, and often has poor outcome (Alberton et al. Citation2002, Gioe Citation2002, Patel et al. Citation2007). This is especially true of dislocations that occur in elderly patients, after THA resulting from femoral neck fractures (Iorio et al. Citation2001) and following THA revision surgery (Khatod et al. Citation2006). The use of augments or constrained acetabular liners has been advocated in order to treat persistent THA instability. Constrained liners minimize the risk of dislocation but the rate of aseptic loosening of such devices is high in the long term (Yun et al. Citation2005, Williams et al. Citation2007)
A different concept in the treatment of recurrent THA instability has been available since the introduction of dual-mobility or tripolar cups (Farizon et al. Citation1998). The principle of such constructs is the encasement of a regular-size femoral head component inside a larger-size polyethylene liner that in turn articulates with and moves within a metal shell fixed to acetabular bone. The use of such implants has been described in both primary and revision THA (Langlais et al. Citation2008, Philippot et al. Citation2009a, Bouchet et al. Citation2011, Boyer et al. Citation2012).
We investigated re-revision rates of dual-mobility cups after revision THA that was performed due to recurrent dislocations and recorded in the Swedish Hip Arthroplasty Register. We hypothesized that the use of dual-mobility cups would result in a low risk of re-revision due to dislocation after revision THA in the short term. As a secondary endpoint, we analyzed the risk of re-revision for any reason and identified risk factors for re-revision.
Patients and methods
Source of data
Our data were derived from the Swedish Hip Arthroplasty Register (SHAR, Annual Report 2010). All primary and revision THAs performed in Sweden since 1979, both in public and private orthopedic units, have been reported to the Register. In this study, we used the reoperation database, which includes personal identification numbers from the start of the Register in 1979. Information on the type of implant, fixation, and technical details are recorded from the case records of each reoperation and are entered into the database. All THA cup revision procedures performed due to recurrent dislocation of a previously inserted THA, registered in the SHAR up to December 31, 2010 and employing a specific dual-mobility cup (Avantage; Biomet, Warsaw, IN) were extracted. All types of cup revisions—irrespective of the number of previous cup revisions—were eligible, and both isolated cup revisions and combined cup and stem revisions were included. 228 cup revisions in 228 patients making use of the above-mentioned dual-mobility cup were identified, the first such procedure being recorded in 2004. 2 different types of Avantage cups had been used: the uncemented, hydroxyapatite-coated version and the cemented, polished version ().
The term “revision” was defined as an intervention where 1 or more components of the prosthesis are exchanged or where the whole prosthesis is removed. Thus, other types of reoperations where the implant was left untouched, e.g. closed reductions or incision and drainage, were disregarded in this study.
The SHAR has been repeatedly validated, and the completeness has been found to be about 99% for primary hip arthroplasties and 94% for revision hip arthroplasties (Soderman 2000).
Statistics
Descriptive statistics employed frequencies, means, 95% confidence intervals (CI), median values, and ranges. Differences between categorical data were analyzed using the chi-square test or Fisher’s exact test where appropriate.
Kaplan-Meier survival analysis was performed with re-revision of any component due to dislocation as the primary endpoint and re-revision of any component for any reason as the secondary endpoint. Life tables and survival functions with CI were calculated. Follow-up started on the day of cup revision using the dual-mobility cup (index cup revision), and ended on the day of re-revision, death, emigration, or December 31, 2010, whichever came first. The survival analysis was discontinued before less than 25 cases remained at risk, i.e. after 4 years.
Cox proportional hazards models were fitted to analyze the influence of various covariates on the relative risk (RR) of revision due to dislocation, or for any reason, using the Breslow method for handling ties. The covariates sex, age (< 50, 50–59, 60–75, and > 75 years), primary diagnosis, number of previous revision surgeries to the relevant joint, and surgical approach (lateral or posterior) were initially investigated as singular covariates, resulting in crude RR values. All covariates were subsequently entered into the model and adjusted RR values were calculated. The assumption of proportional hazards in the adjusted model was investigated by calculating the correlation coefficient ρ between transformed survival time and the scaled Schoenfeld residuals, accompanied by plots of scaled Schoenfeld residuals against transformed time for each covariate. We found no evidence that the assumption of proportionality was violated (p > 0.5 for all covariates included in the model; p = 0.8 for the global model test).
The level of statistical significance was set at p < 0.05. Statistical analyses were performed using the R software package (version 2.14.1).
Results
Characteristics of the study population
Median follow-up time was 2 (0–6) years. The population studied consisted of 144 females and 84 males, and for half of the population the age at the time of the index cup revision was above 75 years (). At the time of primary THA, primary osteoarthritis had been the underlying diagnosis for 157 patients (69%), followed by fracture in 34 (15%) and inflammatory arthritis in 16 (7%).
Table 1. Age at index cup revision
The median time between the primary THA and the index cup revision was 7 (0–28) years. In 170 patients (75%), no previous revision surgery had been performed prior to the index cup revision, i.e. the index cup revision was the first revision surgery after primary THA. 44 patients (19%) had undergone one previous revision surgery, and 14 (6%) had undergone 2 or more revisions prior to the index cup revision. In 92 patients (41%), the surgical approach at the procedure preceding the index cup revision had been direct lateral, while in 131 (58%) a posterior approach had been used (5 cases had missing data).
Index cup revisions
The index cup revision was an isolated cup revision in 187 cases (82%) or part of a total hip revision including stem revision in 41 patients (18%). Details of the revised cups are given in . During the index cup revision, 200 dual-mobility cups (88%) were cemented and 28 (12%) were uncemented. The surgical approach at the index cup revision was direct lateral in 99 cases (44%) and posterior in 124 (56%), with missing data in 5 cases. Metal backing of the dual-mobility cup by the use of Müller-, Burch-Schneider-, or trabecular metal reinforcement rings was performed in 12 patients (5%), whereas no such constructions were used in 211 cases (93%), with missing information in 5 cases. A variety of stems were combined with the inserted dual-mobility cups in cases where a total hip revision was undertaken ().
Table 2. Types and numbers of revised during the index procedure
Table 3. Types of revision stems used together with a dual-mobility cup at index cup revision a
Re-revisions of dual-mobility cups
At the time of follow-up, 18 (8%) of the hips revised with a dual-mobility cup at the index cup revision had been re-revised. 5 (2%) had been re-revised due to deep infection, 4 (2%) due to dislocation, 4 (2%) due to aseptic loosening, 3 (1.5%) due to periprosthetic fracture, and 2 (1%) for other reasons (). The median time between the index cup revision and re-revision of any component was 0.7 years (0.1–5). 10 of the re-revisions were performed during the first year after the index cup revision.
Table 4. Details of re-revised patients
Revision-free survival after 2 years with the endpoint revision of any component due to dislocation was 99% (CI: 97–100) according to the Kaplan-Meier method. Survival with the endpoint revision of any component for any reason was 93% (CI: 90–97) after 2 years and 89% (CI: 83–95) after 4 years (). For the subgroup of patients who had not undergone revision surgery prior to the index cup revision, 4-year survival was 94% (CI: 90–98) with re-revision of any component for any reason as the endpoint.
Risk factors for re-revision of dual-mobility cups
We considered age, sex, diagnosis at primary THA, the type of surgical approach at the index procedure, and the number of previous revisions of the revised hip to be relevant covariates exerting a possible influence on the risk of re-revision due to dislocation, or for any reason.
The factors influencing the endpoint re-revision due to dislocation were initially investigated by calculating crude RR in a Cox regression model. Only age between 50 and 59 years was a risk factor for re-revision due to dislocation (RR = 13, CI: 1–146). An interpretable multiple regression model with adjusted RR could not be calculated due to the low number of events, i.e. only 4 re-revisions due to dislocation in 228 cases, resulting in excessive confidence intervals.
Crude RRs were then calculated in a Cox regression model with the endpoint re-revision of any component for any reason (). Age between 50 and 59 years and a diagnosis of inflammatory arthritis at the time of the primary THA were risk factors for re-revision for any reason in the unadjusted model. The adjusted multiple Cox regression model indicated that age between 50 and 59 years was a risk factor for re-revision (RR = 6, CI: 1–23). The number of previous revision surgeries to the relevant joint was also a risk factor for re-revision for any reason (RR = 1.7 (CI: 1–3) for every previous revision surgery). In contrast, sex, diagnosis, and surgical approach at the index cup revision did not have a clinically relevant effect on the risk of re-revision for any reason.
Table 5. Cox regression analysis of risk factors for revision of any component for any reason a
Discussion
Our review of 228 dual-mobility cups inserted as THA revision components indicates a relatively low frequency of re-revisions due to dislocation within 2 years, although all the patients in our cohort were revised due to dislocation of the previous THA, and 25% of all the patients had undergone 1 or more previous revision surgeries.
In cases of recurrent dislocations, the use of constrained cups has been advocated (Bremner et al. Citation2003, Shapiro et al. Citation2003, Callaghan et al. Citation2004, Goetz et al. Citation2004). On the other hand, high revision rates after the use of constrained implants have also been described (Anderson et al. Citation1994, Berend et al. 2005, Della Valle et al. Citation2005, Yun et al. Citation2005). In an attempt to identify the modes of failure of a constrained tripolar implant, it was found that in 43 revised components the causes of revision included failure at the bone-implant interface and failure of the retaining mechanism (Guyen et al. Citation2008).
The introduction of dual-mobility cups in primary THA results in a low risk of postoperative dislocation. In a case-control study on primary THA performed by a single surgeon through a posterior approach, no dislocations were found after the use of a dual-mobility cup in 105 patients, whereas 5 dislocations occurred in the control group consisting of 108 patients operated with a conventional 28-mm metal head and a polyethylene cup (Bouchet et al. Citation2011). In a series of 150 patients who were operated with a dual-mobility cup due to primary osteoarthritis, no dislocation was observed after 7 years of follow-up (Bauchu et al. 2008). An analysis of 384 cases operated with dual-mobility cups at primary THA revealed 14 dislocations and 13 cases of aseptic loosening after a mean follow-up time of 15 years (Philippot et al. Citation2009b). In patients with cervical neck fracture, the risk of dislocation of the inserted THA was reduced by use of a dual-mobility cup (Tarasevicius et al. Citation2010).
Revision surgery is associated with a higher risk of dislocation than primary THA, and dislocation rates of up to 28% have been reported (Parvizi et al. Citation2008). In accordance with the findings described after primary THA, various studies have indicated that the use of dual-mobility cups in revision surgery can also be associated with a reduced risk of dislocation. Acetabular revisions of 88 THAs using cemented dual-mobility cups resulted in one dislocation and 2 cases of aseptic loosening at a minimum follow-up time of 2 years (Langlais et al. Citation2008). Acetabular revision surgery in 163 hips with a dual-mobility cup resulted in a dislocation rate of 4% at a mean follow-up of 12 years (Philippot et al. Citation2009a). Leiber-Wackenheim et al. (Citation2011) operated 59 cases with recurrent dislocation using an uncemented dual-mobility cup and reported 1 early dislocation without recurrence after a mean follow-up time of 8 years.
Obviously, the use of such cups cannot guarantee that there will be no further dislocations. Some studies on dual-mobility cups inserted as revision components have even found dislocation frequencies that are close to those observed after revision surgery using conventional cups. In a retrospective study of 31 hips revised with a tripolar articulation due to recurrent dislocation, 2 patients required further revision surgery due to persistent instability (Levine et al. Citation2008). 3 of 54 patients treated with a dual-mobility cup due to recurrent dislocation of a previous THA experienced re-dislocation after a minimum follow-up time of 2 years (Guyen et al. Citation2009). Acetabular revisions using an uncemented dual-mobility cup in 23 patients resulted in 2 cases of dislocation and 1 case of early loosening (Massin and Besnier Citation2010).
The question of whether the use of dual-mobility cups is associated with an increased risk of aseptic loosening must be considered. These cups should not be subject to traction forces to the same extent as constrained liners, and might therefore not have a higher risk of aseptic loosening than conventional cups. The incidence of revision due to aseptic loosening in our study cohort was small, but longer follow-up is necessary to determine the risk of loosening. There has been very little literature on the subject of aseptic loosening after insertion of dual-mobility cups in revision THA. 2 cases of aseptic loosening were found in the previously mentioned study of 88 revision THAs using cemented dual-mobility cups after a minimum follow-up of 2 years (Langlais et al. Citation2008). Insertion of an uncemented dual-mobility cup due to recurrent dislocation in 59 cases of revision THA resulted in a high frequency of peri-acetabular radiolucencies at follow-up after 8 years, but no cup revisions due to aseptic loosening were described (Leiber-Wackenheim et al. Citation2011). Philippot et al. (Citation2008) evaluated 438 primary dual-mobility sockets after 17 years. They reported 13 loose cups, 23 intraprosthetic dislocations, and 7 revisions because of polyethylene wear. The potential long-term problem with convex polyethylene articulation surfaces can be expected to decrease using currently available high-molecular-weight polyethylene.
A weakness of the present study is that we only report cases of re-revision due to dislocation, but not postoperative dislocations treated with closed reduction. The registration of closed reductions is notoriously unreliable, as such procedures are frequently performed in emergency departments and often no operative records are kept. Closed reductions of primary or revision THAs are therefore not reported to the Register. On the other hand, judging by our own experience, dislocations of dual-mobility cups reflect a high degree of joint instability and recurrent dislocations will most often ensue. Thus, revision surgery must be considered the most common procedure in order to treat dislocations of the Avantage cup, and—in contrast to closed reductions—these procedures are reported to the Register. Our study also suffers from a short follow-up, but most re-revisions due to dislocation would have been performed during the first 2 years after the index procedure (Phillips et al. Citation2003).
In conclusion, our review of 228 dual-mobility cups inserted as revision implants due to dislocation of previous THA indicates that the risk of re-revision due to dislocation was low. Thus, the use of this device appears to address the clinically relevant problem of recurrent instability after THA revision surgery. However, the proposed advantage of such designs has to be weighed against the potential weakness of increased wear, osteolysis, and loosening in the long run, and longer follow-up of larger cohorts is mandatory before firm conclusions can be drawn. In addition, we found that younger age at the time of the index cup revision and previous revision surgery of the same joint increased the risk of subsequent re-revision.
NPH: statistical analysis, and writing and revision of the manuscript; AS and RJW: revision of the manuscript; JK: database preparation, statistical analysis, and revision of the manuscript.
We thank all the Swedish orthopedic surgeons and secretaries who contributed data.
NPH has received institutional support or lecturer’s fees from several orthopaedic implant manufacturers including Biomet. Biomet was, however, not involved in either study design, data analysis or preparation of the present manuscript.
- Alberton GM, High WA, Morrey BF. Dislocation after revision total hip arthroplasty: an analysis of risk factors and treatment options. J Bone Joint Surg (Am) 2002; 84 (10): 1788-92.
- Anderson MJ, Murray WR, Skinner HB. Constrained acetabular components. J Arthroplasty 1994; 9 (1): 17-23.
- Bauchu P, Bonnard O, Cypres A, Fiquet A, Girardin P, Noyer D. The dual-mobility POLARCUP: first results from a multicenter study. Orthopedics (Suppl 2) 2008; 31 (12).
- Berend KR, Lombardi AV, Jr., Mallory TH, Adams JB, Russell JH, Groseth KL. The long-term outcome of 755 consecutive constrained acetabular components in total hip arthroplasty examining the successes and failures. J Arthroplasty (Suppl 3) 2005; 20 (7): 93-102.
- Bouchet R, Mercier N, Saragaglia D. Posterior approach and dislocation rate: a 213 total hip replacements case-control study comparing the dual mobility cup with a conventional 28-mm metal head/polyethylene prosthesis. Orthop Traumatol Surg Res 2011; 97 (1): 2-7.
- Boyer B, Philippot R, Geringer J, Farizon F. Primary total hip arthroplasty with dual mobility socket to prevent dislocation: a 22-year follow-up of 240 hips. Int Orthop 2012; 36 (3): 511-8.
- Bremner BR, Goetz DD, Callaghan JJ, Capello WN, Johnston RC. Use of constrained acetabular components for hip instability: an average 10-year follow-up study. J Arthroplasty (Suppl 1) 2003; 18 (7): 131-7.
- Callaghan JJ, O’Rourke MR, Goetz DD, Lewallen DG, Johnston RC, Capello WN. Use of a constrained tripolar acetabular liner to treat intraoperative instability and postoperative dislocation after total hip arthroplasty: a review of our experience. Clin Orthop 2004; (429): 117-23.
- Della Valle CJ, Chang D, Sporer S, Berger RA, Rosenberg AG, Paprosky WG. High failure rate of a constrained acetabular liner in revision total hip arthroplasty. J Arthroplasty (Suppl 3) 2005; 20 (7): 103-7.
- Farizon F, de Lavison R, Azoulai JJ, Bousquet G. Results with a cementless alumina-coated cup with dual mobility. A twelve-year follow-up study. Int Orthop 1998; 22 (4): 219-24.
- Gioe TJ. Dislocation following revision total hip arthroplasty. Am J Orthop (Belle Mead. NJ) 2002; 31 (4): 225-7.
- Goetz DD, Bremner BR, Callaghan JJ, Capello WN, Johnston RC. Salvage of a recurrently dislocating total hip prosthesis with use of a constrained acetabular component. A concise follow-up of a previous report. J Bone Joint Surg (Am) 2004; 86 (11): 2419-23.
- Guyen O, Lewallen DG, Cabanela ME. Modes of failure of Osteonics constrained tripolar implants: a retrospective analysis of forty-three failed implants. J Bone Joint Surg (Am) 2008; 90 (7): 1553-60.
- Guyen O, Pibarot V, Vaz G, Chevillotte C, Bejui-Hugues J. Use of a dual mobility socket to manage total hip arthroplasty instability. Clin Orthop 2009; 467 (2): 465-72.
- Iorio R, Healy WL, Lemos DW, Appleby D, Lucchesi CA, Saleh KJ. Displaced femoral neck fractures in the elderly: outcomes and cost effectiveness. Clin Orthop 2001; (383): 229-42.
- Khatod M, Barber T, Paxton E, Namba R, Fithian D. An analysis of the risk of hip dislocation with a contemporary total joint registry. Clin Orthop 2006; (447): 19-23.
- Langlais FL, Ropars M, Gaucher F, Musset T, Chaix O. Dual mobility cemented cups have low dislocation rates in THA revisions. Clin Orthop 2008; (466) (2): 389-95.
- Leiber-Wackenheim F, Brunschweiler B, Ehlinger M, Gabrion A, Mertl P. Treatment of recurrent THR dislocation using of a cementless dual-mobility cup: a 59 cases series with a mean 8 years’ follow-up. Orthop Traumatol Surg Res 2011; 97 (1): 8-13.
- Levine BR, Della Valle CJ, Deirmengian CA, Breien KM, Weeden SH, Sporer SM, Paprosky WG. The use of a tripolar articulation in revision total hip arthroplasty: a minimum of 24 months’ follow-up. J Arthroplasty 2008; 23 (8): 1182-8.
- Massin P, Besnier L. Acetabular revision using a press-fit dual mobility cup. Orthop Traumatol Surg Res 2010; 96 (1): 9-13.
- Parvizi J, Picinic E, Sharkey PF. Revision total hip arthroplasty for instability: surgical techniques and principles. J Bone Joint Surg (Am) 2008; 90 (5): 1134-42.
- Patel PD, Potts A, Froimson MI. The dislocating hip arthroplasty: prevention and treatment. J Arthroplasty (Suppl 1) 2007; 22 (4): 86-90.
- Philippot R, Farizon F, Camilleri JP, Boyer B, Derhi G, Bonnan J, Fessy MH, Lecuire F. Survival of cementless dual mobility socket with a mean 17 years follow-up. Rev Chir Orthop Reparatrice Appar Mot 2008; 94 (8): e23-7.
- Philippot R, Adam P, Reckhaus M, Delangle F, Verdot FX, Curvale G, Farizon F. Prevention of dislocation in total hip revision surgery using a dual mobility design. Orthop Traumatol Surg Res 2009a; 95 (6): 407-13.
- Philippot R, Camilleri JP, Boyer B, Adam P, Farizon F. The use of a dual-articulation acetabular cup system to prevent dislocation after primary total hip arthroplasty: analysis of 384 cases at a mean follow-up of 15 years. Int Orthop 2009b; 33 (4): 927-32.
- Phillips CB, Barrett JA, Losina E, Mahomed NN, Lingard EA, Guadagnoli E, Baron JA, Harris WH, Poss R, Katz JN. Incidence rates of dislocation, pulmonary embolism, and deep infection during the first six months after elective total hip replacement. J Bone Joint Surg (Am) 2003; 85 (1): 20-6.
- Shapiro GS, Weiland DE, Markel DC, Padgett DE, Sculco TP, Pellicci PM. The use of a constrained acetabular component for recurrent dislocation. J Arthroplasty 2003; 18 (3): 250-8.
- Söderman P. On the validity of the results from the Swedish National Total Hip Arthroplasty register. Acta Orthop Scand (Suppl 296) 2000; 71: 1-33.
- Swedish Hip Arthropasty Register. Annual Report. 2010. http://www.shpr.se/en/Publications/DocumentsReports.aspx
- Tarasevicius S, Busevicius M, Robertsson O, Wingstrand H. Dual mobility cup reduces dislocation rate after arthroplasty for femoral neck fracture. BMC Musculoskelet Disord 2010; 11: 175.
- Williams JT, Jr., Ragland PS, Clarke S. Constrained components for the unstable hip following total hip arthroplasty: a literature review. Int Orthop 2007; 31 (3): 273-7.
- Yun AG, Padgett D, Pellicci P, Dorr LD. Constrained acetabular liners: mechanisms of failure. J Arthroplasty 2005; 20 (4): 536-41.