Abstract
Background and purpose The association between excessive early migration of acetabular cups and late aseptic revision has been scantily reported. We therefore performed 2 parallel systematic reviews and meta-analyses to determine the association between early migration of acetabular cups and late aseptic revision.
Methods One review covered early migration data from radiostereometric analysis (RSA) studies, while the other focused on revision rates for aseptic loosening from long-term survival studies. Thresholds for acceptable and unacceptable migration were classified according the Swedish Hip Arthroplasty Register and the Australian National Joint Replacement Registry: < 5% revision at 10 years.
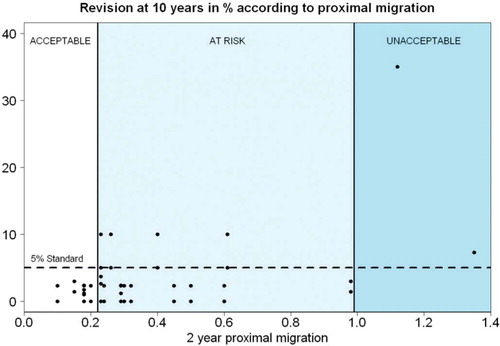
Results Following an elaborate literature search, 26 studies (involving 700 cups) were included in the RSA review and 49 studies (involving 38,013 cups) were included in the survival review. For every mm increase in 2-year proximal migration, there was a 10% increase in revision rate, which remained after correction for age, sex, diagnosis, hospital type, continent, and study quality. Consequently, proximal migration of up to 0.2 mm was considered acceptable and proximal migration of 1.0 mm or more was considered unacceptable. Cups with proximal migration of between 0.2 and 1.0 mm were considered to be at risk of having revision rates higher than 5% at 10 years.
Interpretation There was a clinically relevant association between early migration of acetabular cups and late revision due to loosening. The proposed migration thresholds can be implemented in a phased evidence-based introduction, since they allow early detection of high-risk cups while exposing a small number of patients.
Globally, several hundred thousand total hip prostheses (THPs) are implanted each year and this number is expected to double within the next 2 decades (Kurtz et al. Citation2005, Citation2007). It is crucial to monitor the safety and quality of THP to prevent harm to patients and to minimize costs to society (i.e. reduction of the future revision burden). Most of the new THP designs are on the market without having shown safety or effectiveness (Sheth et al. Citation2009). This has resulted in the use of several THPs with high failure rates, such as the Wagner cup, the Link V cup, and the Mecron cup (Mogensen et al. Citation1982, Snorrason et al. Citation1990, Clarius et al. Citation2010). In response to these problems, several countries have developed guidelines to guarantee patient safety, e.g. the NICE guidelines (2003). Furthermore, it has become increasingly evident that a phased evidence-based introduction, which is common for pharmaceuticals, is needed to regulate the introduction of new THPs to the market (Malchau 2000, McCulloch et al. Citation2009, Schemitsch et al. Citation2010). This should include systematic assessment and early detection of the major cause of THP failure, which is aseptic loosening necessitating revision surgery (SHAR 2009, AJR 2010).
Although it may take 10 years before the final stages of loosening are apparent on conventional radiographs, it is possible to detect loosening early postoperatively with radiostereometric analysis (RSA). Since, RSA allows in vivo, 3D measurement of the migration of THPs with an accuracy of 0.2 mm for translations and 0.5 degrees for rotations (Kärrholm et al. Citation1994, Hauptfleisch et al. Citation2006), only a small number of patients have to be exposed to potentially unsafe THPs. RSA could therefore play an important role in the phased evidence-based introduction of new THP.
In this systematic review and meta-analysis, we concentrated on the acetabular cup. We hypothesized that early migration of the acetabular cup, measured through RSA, is associated with late revision for aseptic loosening. We therefore systematically reviewed the association between early migration and late revision for aseptic loosening of the acetabular cup in primary THP. This could eventually lead to clinical guidelines, to be used in a phased introduction of new THP.
Material and methods
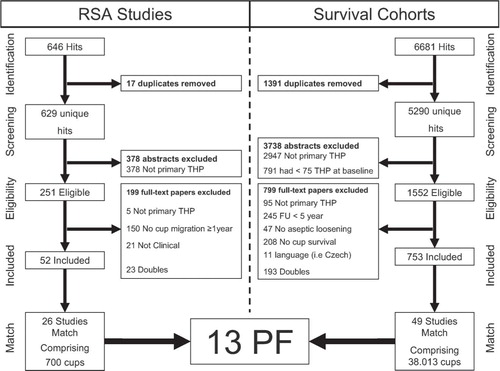
We performed 2 parallel systematic reviews (international registration number NTR3128; www.trialregister.nl) on studies of patients treated with THP for primary osteoarthritis (OA), secondary osteoarthritis (SA), and fractures of the proximal femur (FF). One review covers early migration data of acetabular cups from RSA studies. In the other, we determined the long-term revision rates for aseptic loosening of acetabular cups from survival studies (). During all phases of the review process, a referee (RN) with over 20 years of experience in both RSA and THP was available for advice.
Figure 1. PRISMA flow chart of both reviews. Details of the 13 PF can be found in Table 1. RSA: radiostereometric analysis; THP: total hip prosthesis; FU: follow-up; PF: combination of prosthesis type and fixation method.
Systematic review of RSA studies
Literature search. A thorough literature search was performed together with a medical librarian (JP) to reduce bias by increasing the likelihood of retrieving all relevant studies (Vochteloo et al. Citation2010). The following bibliographies were searched up to 2009: PubMed, Embase, Web-of-Science, and the Cochrane library. Relevant articles were screened for additional references. Also, a separate search was conducted in 9 leading orthopedic and biomechanical journals (Acta Orthop, Clin Orthop Relat Res, J Arthroplasty, J Bone Joint Surg (Am and Br), Knee Surg Sports Traumatol Arthrosc, J Orthop Res, J Biomech, and Clin Biomech). Finally, Google Scholar was used. Articles in English, French, Italian, Spanish, Dutch, and German were considered. The search strategy consisted of the following components, each defined by a combination of controlled vocabulary and free text terms: (1) RSA, and (2) joint replacement. See Appendix (Supplementary data) for more details concerning the strategy and terms used.
Inclusion and exclusion analysis. Initial screening based on the title and abstract of RSA studies was performed by BP to identify studies on patients treated with THP for OA, SA or FF. In cases where the information in the abstract did not suffice or where there was any doubt, studies remained eligible. The full text of eligible studies was independently evaluated in duplicate by 2 reviewers (BP and MN). The inclusion criteria for RSA studies were (1) primary THP, and (2) minimal RSA follow-up of 1 year, measuring acetabular cup migration. Non-clinical studies (animal studies and phantom studies) were excluded.
Data extraction
BP and MN independently extracted migration data in duplicate from the RSA studies. Since the failure mechanism of acetabular cups involves increasing proximal migration and increasing inclination, the data extraction of RSA studies comprised proximal migration and inclination of the acetabular cup until the second postoperative year (Stocks et al. 1995). Data concerning patient demographics and regional influences were also extracted to allow for confounder correction (Pijls et al. Citation2011).
Quality assessment. The quality of the RSA studies was independently appraised in duplicate by BP and MN at the level of outcome using the AQUILA methodological score (Pijls et al. Citation2011). For the RSA studies, we modified the AQUILA score by removing items that were not considered relevant for early migration, such as long-term follow-up and revision assessment.
Systematic review of survival studies
Literature search. The search strategy and bibliographies were the same as those in the RSA review, with the exception of the components of the search strategy. The search strategy for the survival studies consisted of the following components, each defined by a combination of controlled vocabulary and free text terms: (1) joint replacement, (2) implant failure, and (3) survival analysis. In the search strategy, no distinction was made between total knee prostheses (TKPs) and total hip prostheses (THPs), because some authors have reported on both TKPs and THPs (Ryd Citation1992). See Appendix for more details on strategy and terms.
Inclusion and exclusion analysis. The procedure for screening of the survival studies for eligibility and subsequent inclusion and exclusion analysis was identical to the procedures for the RSA studies with the exception of inclusion and exclusion criteria. The inclusion criteria for survival studies were (1) primary THP; (2) follow-up of 5, 10, 15, 20, or 25 years (in the final analysis only 10 years of follow-up was used); (3) endpoint revision surgery for aseptic loosening of the acetabular cup, or indication for revision surgery when there was poor general health or patient decline; and (4) survival or percentage revised should be available for specific follow-up (see point 2). Studies with less than 75 THPs at baseline were excluded.
Data extraction. BP and MN independently determined the revision rates in duplicate for aseptic loosening of the acetabular cups at 5-year intervals from the survival studies. Data concerning patient demographics and regional influences were extracted to allow for confounder correction.
Quality assessment. The quality of the survival studies was independently evaluated by BP and MN at the level of outcome using the AQUILA methodological score (Pijls et al. Citation2011).
Analysis
A detailed description of the analysis, methodology, and a worked example is given in the Appendix (see Supplementary data). To determine the association between early migration and late revision, we matched the results from the RSA review to the results of the survival review according to the type of prosthesis and fixation method (e.g. cement or bone ingrowth) here abbreviated to PF. Since PF is determined by technical factors known to be associated with both migration and a high likelihood of revision for aseptic loosening, matching according to PF prevents confounding by PF (NJR 2009, SHAR 2009, AJR 2010). Depending on the studies available, it is possible that there would be more than 1 combination of matching RSA and survival studies for a particular PF. For instance, if there are 3 RSA studies and 2 survival studies of the same PF, then there would be 6 possible combinations (3 times 2). All combinations were considered in the analysis. A meta-analysis for the revision rate at 10 years was performed. A model for the censoring mechanism was employed to reconstruct the data and then a generalized linear mixed model with study as a random effect was applied to estimate the survival at 10 years and its confidence interval (Fiocco et al. Citation2009a,b, 2011, Putter et al. Citation2009). Regarding the RSA studies, pooling of migration results at the level of PF was based on weights according to study size (N).
Adjustment for confounding
Since migration data and revision rate data were extracted from different studies, it was possible that differences between study populations might confound the observed association. In order to address this issue, we determined the degree of similarity of the population from RSA and survival study combinations, expressed by a match score, for age, sex, diagnosis, hospital type, and continent. The match score is constructed according to the results of a recent Delphi survey among an international group of 37 independent experts and can vary between 0 (poor) and 5 (excellent) (Pijls et al. Citation2011). The RSA study and the survival study combination scored 1 point for each of the following criteria (up to a maximum of 5 points): (1) the difference in mean age between patients from the RSA study and those from the survival study was 5 years or less; (2) the difference in percentage of females between the RSA study and the survival study was 10% or less; (3) the difference in percentage of patients diagnosed with primary osteoarthritis between the RSA study and the survival study was 10% or less; (4) the RSA study and the survival study were performed in a similar type of hospital (e.g. both in university medical centers); and (5) the RSA study and the survival study were performed on the same continent.
All other cases scored zero points.
We used a weighted regression model to assess the association between early migration and late aseptic revision, corrected for the influence of match score, RSA study quality, survival study quality, number of THPs in the RSA studies and number of THPs in the survival studies.
Migration thresholds
According to the principle of “primum non nocere“ (first do no harm), new implant designs should perform at least as well as the revision standard of national registries: 3% revision at 5 years and 5% revision at 10 years according to the Swedish Hip Arthroplasty Register and the Australian National Joint Replacement Registry (SHAR 2009, AJR 2010). Based on this revision standard, the following 3 categories were constructed for the phased introduction of new THP: “acceptable”, “at risk”, and “unacceptable”. The category “acceptable” was defined as the level of migration up to which all survival studies have lower revision rates than the standard. The category “unacceptable” was defined as the level of migration from which all revision rates are higher than the standard. The category “at risk” was defined as the migration interval between the “acceptable” and “unacceptable” thresholds, in which studies with revision rates lower and higher than the standard were observed.
Appraisal of publication bias
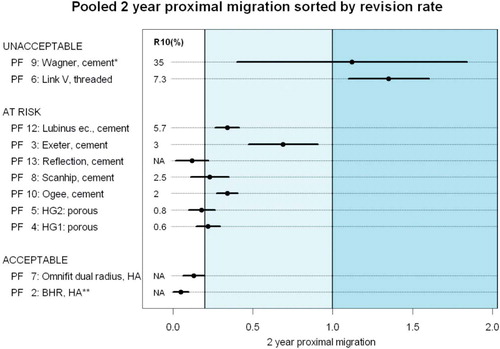
We assessed the potential effect of publication bias by comparing the results from the meta-analysis to the results from national joint registries, since they do not suffer from publication bias (NJR 2009, SHAR 2009, AJR 2010). Accordingly, the PFs that perform better than average in the meta-analysis should also perform better than average in the national joint registries. The same principle also applies to PFs that perform worse than average. For this purpose, the migration pooled by PF was sorted according to revision rate pooled according to the specific combination of prosthesis type and fixation method and visualized in a dot chart (Jacoby Citation2006).
Results
RSA studies
The literature search yielded 629 hits and 26 studies were included, with a total of 700 acetabular cups (Mogensen et al. Citation1982, Mjoberg et al. Citation1990, Snorrason et al. Citation1990, Citation1993, Önsten et al. Citation1993, Citation1994a, Citationb, Citation1995, Citation1996, Thanner et al. Citation1995, Citation1996, Digas et al. Citation2004, von Schewelov et al. Citation2004, 2005, Itayem et al. Citation2005, 2007, Nelissen et al. Citation2005, Rohrl et al. Citation2005, Palm et al. Citation2007, Thien et al. Citation2007). Details of study selection and flow of the review are shown in . On a 7-point scale, the mean AQUILA methodological quality score of the RSA studies was 4.9 (SD 0.8). Proximal migration at 2 years was the most frequently and most consistently reported migration value: 23 out of 26 RSA studies reported it. Change in inclination (rotation around the z-axis) was reported infrequently and inconsistently, and did not allow a meaningful analysis. For the analyses, we will therefore focus on proximal migration at 2 years.
Survival studies
The literature search yielded 5,290 hits, and 49 studies were included, involving a total of 38,013 acetabular cups; see (Howie et al. Citation1990, Partio et al. 1994, Latimer et al. 1996, Woolson et al. 1996, Chiu et al. Citation1997, Furnes et al. Citation1997, Tompkins et al. Citation1997, Bohm and Bosche Citation1998, D’Lima et al. Citation1998, Kesteris et al. Citation1998, Callaghan et al. Citation1999, Petersen et al. Citation1999, Ragab et al. Citation1999, Thanner et al. Citation1999, Garellick et al. Citation2000, Ricci et al. Citation2000, Archibeck et al. Citation2001, Oosterbos et al. Citation2001, Espehaug et al. Citation2002, Rogers et al. Citation2003, Duffy et al. Citation2004, Fink et al. Citation2004, Herrera et al. Citation2004, Parvizi et al. Citation2004, Sinha et al. Citation2004, Ender et al. Citation2005, Min et al. Citation2005, Badhe and Livesley 2006, Eskelinen et al. Citation2006, Castoldi et al. Citation2007, Firestone et al. Citation2007, Gjengedal et al. Citation2007, Hing et al. Citation2007, Ince et al. Citation2007, Surdam et al. Citation2007, D’Angelo et al. Citation2008, Gallo et al. Citation2008, Garcia-Rey et al. 2008, Heilpern et al. Citation2008, Makela et al. Citation2008, McBryde et al. Citation2008, Steffen et al. Citation2008, Williams et al. Citation2008). The mean AQUILA methodological quality score of the survival studies was 7.3 (SD 1.1) on an 11-point scale.
Early migration and late revision
The matching procedure resulted in 13 different PFs and 94 combinations of RSA and survival studies (). There was a clear association between 2-year proximal migration and the 10-year revision rate expressed as prosthesis survival (). For every 1-mm increase in proximal migration (at 2 years), 10% (95% CI: 5.5–14.2; p < 0.05) was added to the 10-year revision rate. Although there was some influence (on the results) of RSA study quality, survival study quality, number of acetabular cups in the RSA study, number of acetabular cups in the survival study, and match score, the association remained significant (with all p-values < 0.05) (). There was no clear association between proximal migration rate (i.e. 2-year proximal migration minus 1-year proximal migration) and the 10-year revision rate.
Table 1. Breakdown of prosthesis types and fixation methods
Figure 2. Scatter plot showing association between 2-year proximal migration in mm and revision rate for aseptic loosening of the acetabular cup at 10 years, as a percentage. The colored lines were derived from weighted regression according to match quality, survival study quality, and RSA study quality (the coefficients and 95% CIs are given in Table 2).
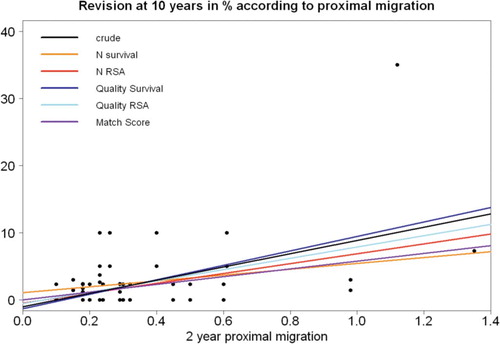
Table 2. Association between 2-year proximal migration and revision rate for aseptic loosening at 10 years a
Migration thresholds
shows the 3 categories of THPs. For proximal migration at 2 years of between 0 and 0.2 mm, there was no cup with more than 5% revision for aseptic loosening at 10 years. Where there was 2-year proximal migration of more than 1.0 mm, there was no cup with less than 5% revision for aseptic loosening at 10 years. This indicates that accepting 5% revision at 10 years resulted in a threshold of 0.2 mm for acceptable proximal migration at 2 years and a threshold of 1.0 mm for unacceptable proximal migration at 2 years.
Publication bias
The pooled 2-year migration ranked by the pooled 10-year revision rate for each PF is presented in . The Wagner cup and threaded Link V cup were classified as unacceptable based of their pooled migration. These cups have been discontinued and are no longer used. Moreover, the Wagner cup had the worst (overall) survival ever recorded in the history of the Swedish Register: 28% at 10 years (Ahnfelt et al. Citation1990). The potential influence of publication bias on the unacceptable threshold is therefore small. The 10-year revision rate for the acceptable PFs were lacking (NA), so longer follow-up of these PFs is necessary to determine whether their 10-year revision rate for aseptic loosening of the cup is lower than 5%.
Figure 4. Dot chart showing the pooled 2-year proximal migration ranked by the pooled 10-year revision rate for each PF: combination of prosthesis type and fixation method. The unacceptable PFs (based on their migration pattern) have been abandoned, with the Wagner cup having the worst recorded survival in the Swedish Register (Ahnfelt et al. Citation1990). A detailed description of each PF is given in Table 1. R10(%) is the pooled revision rate at 10-year follow-up, in percent; NA: not available.
*This a best-case scenario for the Wagner cup, since the reference scene was not made directly postoperatively. Thus, the actual 2-year proximal migration is more than the observed value presented here.
** The Birmingham Hip Resurface (BHR) prostheses of the RSA study were implanted by the developer, so the migration results (and “acceptable” classification) may not apply to non-developers.
Discussion
This systematic review showed a clinically relevant association between early proximal migration of acetabular cups, as measured with RSA, and clinical failure (i.e. revision surgery) at medium- and long-term follow-up and corrected for age, sex, diagnosis, type of hospital, region, study size, and study quality. Each mm of proximal migration increased the 10-year revision rate by 10% on average, which is more than twice the standard revision rates of several national joint registries (NJR Citation2009, SHAR Citation2009, AJR Citation2010).
We also found that RSA studies can identify unsafe acetabular cups as early as 2 years postoperatively. Early identification of these less optimal performing THPs with RSA prevents their widespread use. Compared to the present policy of introduction of new prostheses, such a policy would safeguard numerous patients from revision surgery.
The strengths of this systematic review are the large number of studies included (75) and patients included (> 38,000), which resulted in 13 different Prosthesis and Fixations (PFs). This large variation, which reflects the diversity in THP designs and fixation methods, ensures wide applicability of the results. Since the migration and revision rates are from different studies, the RSA data could not have been used (incorporated) for the decision to perform a revision; this means that there is no incorporation bias.
One limitation is that the migration of the BHR (Birmingham Hip Resurface) and Omnifit acetabular cups was classified as “acceptable”. This means that we would expect their 10-year revision rate for aseptic loosening to be lower than 5%. However, since their 10-year revision rate was not available in this review, longer follow-up of the BHR and Omnifit is required. Regarding the BHR, it should also be noted that the surgery in the RSA study was performed by the developer (Itayem et al. Citation2005). Thus, the observed migration (and “acceptable” classification) does not necessarily apply to non-developers. Regarding the Omnifit dual-radius cup, it should be noted that although the early migration (primary fixation) is classified as “acceptable”, the problem is secondary loosening due to excessive wear and osteolysis (von Schewelov et al. Citation2004). A phased introduction should therefore also focus on wear measurements, where RSA plays an important role.
We are also aware that RSA only evaluates aseptic loosening while other failure mechanisms (e.g. osteolysis and pseudotumors in BHR resurfacing) are not evaluated by RSA. Thus, RSA studies are only the first step in the phased introduction as proposed by Malchau (Malchau 2000, Pandit et al. Citation2008).
Even more than a decade ago, several authors pleaded for a phased, evidence-based introduction of new prostheses (Murray et al. 1995, Liow et al. 1997, Muirhead-Allwood Citation1998, Malchau 2000). The association we have found between early migration and long-term revision of acetabular cups translates into practical threshold values of migration (i.e. RSA) for such a phased evidence-based introduction policy. During phase A, multiple single-center RSA studies should be performed to determine the safety of the THP with regard to the risk of revision for aseptic loosening and wear. Once the THP is considered safe, phase B studies must be conducted to evaluate the clinical performance of the THP regarding pain relief and functioning (clinical scores and patient-reported outcome measures (PROMS)) and to determine the rate of other complications (e.g. pseudotumors) (Pandit et al. Citation2008). After release on the market, phase C starts, where the performance of the THP must be monitored by post-marketing surveillance in national joint replacement registries (Schemitsch et al. Citation2010). This includes both the revision rate and patient evaluations using PROMS.
In this systematic review, RSA studies of 10–60 patients followed for only 2 years identified the same unsafe cups (the Wagner cup and the Link V threaded cup) as did national joint registries where thousands of patients were followed for 10 years. A recent publication has shown a 22–35% reduction in the number of revisions of RSA-tested total knee replacements as compared to non-RSA-tested total knee replacements in the national joint registries (Nelissen et al. Citation2011).
The Wagner cup is of special interest. It has had the worst survival ever recorded in the history of the Swedish Register: 28% at 10 years (Ahnfelt et al. Citation1990). If the threshold of unacceptable migration (1.0 mm) had been known at the time the Wagner cup was introduced, it would have been classified as “unacceptable” after 2 years of RSA follow-up with only 11 patients. The latter would have suggested a closer follow-up of this prosthesis. The Link V cup would also have been classified as “unacceptable” after only 2 years of follow-up with RSA. Both examples illustrate the clinical value of the migration thresholds for the early identification of THPs with a high likelihood of failure at long-term follow-up.
Various authors and regulatory agencies have recognized the potential of RSA (Bulstrode et al. Citation1993, Kärrholm et al. Citation1994, Ryd et al. 1995, Malchau 2000, Hauptfleisch et al. Citation2006). The NICE guidelines (2003) (UK) required adequate long-term clinical data for hip prostheses and indicated that RSA was a promising technique that might be an early warning indicator of poor long-term revision rates. The Dutch Orthopaedic Society now requires a phased introduction with mandatory RSA studies before any new hip prosthesis is considered for introduction to the Dutch market (2011).
In conclusion, we found a clinically relevant association between early migration of THPs and late revision for loosening. The proposed migration thresholds can be implemented in a phased, evidence-based introduction, since they allow early detection of high-risk THPs while exposing a small number of patients.
Supplementary Material
Download PDF (209.3 KB)RGN, BGP, and ERV conceived the study. SM provided methodological input and MF provided statistical input during the conceptual phase of the study. JWP designed the search strategy for the literature search. BGP and MJN performed the study selection and matching procedure, appraised the quality of the literature, and performed the data extraction. MF and BGP analyzed the data. BGP, MJN, ERV, and RGN wrote the initial draft manuscript. MF and SM ensured the accuracy of the data and analysis. BGP and MF wrote the Appendix. Critical revision of the manuscript was done by all authors. All the authors read and approved the final manuscript.
We thank the Atlantic Innovation Fund (Atlantic Canada Opportunities Agency) for providing funding for this study (Contract no. 191933). The Atlantic Innovation Fund did not take part in the design or performance of the study; in the collection, management, analysis, or interpretation of the data; or in preparation, review, or approval of the manuscript.
- Ahnfelt L, Herberts P, Malchau H, Andersson G BJ. Prognosis of total hip replacement. Acta Orthop Scand (Suppl 238) 1990; 61: 2-25.
- AJR. Australian Orthopaedic Association National Joint Replacement Registry Annual Report 2010 http://wwwdmacadelaideeduau/aoanjrr/publicationsjsp?section=reports2010. 2010: accessed 12-05-2011.
- Archibeck MJ, Berger RA, Jacobs JJ, Quigley LR, Gitelis S, Rosenberg AG, Second-generation cementless total hip arthroplasty. Eight to eleven-year results. J Bone Joint Surg (Am) 2001; 83 (11): 1666-73.
- Badhe S, Livesley P. Early polyethylene wear and osteolysis with ABG acetabular cups (7-to 12-year follow-up). Int Orthop 2006; 30 (1): 31-4.
- Bohm P, Bosche R. Survival analysis of the Harris-Galante I acetabular cup. J Bone Joint Surg (Br) 1998; (3): 396-403.
- Bulstrode CJ, Murray DW, Carr AJ, Pynsent PB, Carter SR. Designer hips. Bmj 1993; 306 (6880): 732-3.
- Callaghan JJ, Johnston RC, Pedersen DR. The John Charnley Award. Practice surveillance: a practical method to assess outcome and to perform clinical research. Clin Orthop 1999; (369): 25-38.
- Castoldi F, Rossi R, La RM, Sibelli P, Rossi P, Ranawat AS. Ten-year survivorship of the anatomique Benoist Girard I total hip arthroplasty. J Arthroplasty 2007; 22 (3): 363-8.
- Chiu KH, Shen WY, Tsui HF, Chan KM. Experience with primary exeter total hip arthroplasty in patients with small femurs. Review at average follow-up period of 6 years. J Arthroplasty 1997; 12 (3): 267-72.
- Clarius M, Jung AW, Streit MR, Merle C, Raiss P, Aldinger PR. Long-term results of the threaded Mecron cup in primary total hip arthroplasty : A 15-20-year follow-up study. Int Orthop 2010; 34 (8): 1093-8.
- D’Angelo F, Molina M, Riva G, Zatti G, Cherubino P. Failure of dual radius hydroxyapatite-coated acetabular cups. J Orthop Surg Res 2008; 3: 35.
- D’Lima DD, Oishi CS, Petersilge WJ, Colwell CW, Walker RH. 100 cemented versus 100 noncemented stems with comparison of 25 matched pairs. Clin Orthop 1998; (348): 140-8.
- Digas G, Thanner J, Anderberg C, Kärrholm J. Bioactive cement or ceramic/porous coating vs. conventional cement to obtain early stability of the acetabular cup. Randomised study of 96 hips followed with radiostereometry. J Orthop Res 2004; 22 (5): 1035-43.
- Duffy P, Sher JL, Partington PF. Premature wear and osteolysis in an HA-coated, uncemented total hip arthroplasty. J Bone Joint Surg (Br) 2004; 1: 34-8.
- Dutch Orthopaedic Society (NOV) guideline total hip prosthesis 2011: http://www.kwaliteitskoepel.nl/assets/structured-files/2011/Richtlijn+Totale+Heupprothese+2010+zonder+watermerk.pdf
- Ender SA, Machner A, Pap G, Grasshoff H, Neumann HW. Long-term results with the Harris-Galante press-fit-cup. Z Orthop Ihre Grenzgeb 2005; 143 (3): 348-54.
- Eskelinen A, Remes V, Helenius I, Pulkkinen P, Nevalainen J, Paavolainen P. Uncemented total hip arthroplasty for primary osteoarthritis in young patients: a mid-to long-term follow-up study from the Finnish Arthroplasty Register. Acta Orthop 2006; 77 (1): 57-70.
- Espehaug B, Furnes O, Havelin LI, Engesaeter LB, Vollset SE. The type of cement and failure of total hip replacements. J Bone Joint Surg (Br) 2002; 84 (6): 832-8.
- Fink B, Protzen M, Hansen-Algenstaedt N, Berger J, Ruther W. High migration rate of two types of threaded acetabular cups. Arch Orthop Trauma Surg 2004; 124 (1): 17-25.
- Fiocco M, Putter H, van Houwelingen JC. Meta-analysis of pairs of survival curves under heterogeneity: a Poisson correlated gamma-frailty approach. Stat Med 2009a; 28 (30): 3782-97.
- Fiocco M, Putter H, Van Houwelingen JC. A new serially correlated gamma-frailty process for longitudinal count data. Biostatistics 2009b; 10 (2): 245-57.
- Fiocco M, Stijnen T, Putter H. Meta-analysis of time-to-event outcomes using a hazard-based approach: Comparison with other models, robustness and meta-regression. Computational Statistics and Data Analysis. 2011: doi:10.1016/j.csda.2011.05.009
- Firestone DE, Callaghan JJ, Liu SS, Goetz DD, Sullivan PM, Vittetoe DA, . Total hip arthroplasty with a cemented, polished, collared femoral stem and a cementless acetabular component. A follow-up study at a minimum of ten years. J Bone Joint Surg (Am) 2007; 89 (1): 126-32.
- Furnes O, Lie SA, Havelin LI, Vollset SE, Engesaeter LB. Exeter and charnley arthroplasties with Boneloc or high viscosity cement. Comparison of 1,127 arthroplasties followed for 5 years in the Norwegian Arthroplasty Register. Acta Orthop Scand 1997; 68 (6): 515-20.
- Gallo J, Langova K, Havranek V, Cechova I. Poor survival of ABG I hip prosthesis in younger patients. BiomedPapMedFacUniv PalackyOlomoucCzechRepub 2008; 152 (1): 163-8.
- Garcia-Rey E, Garcia-Cimbrelo E. Clinical and radiographic results and wear performance in different generations of a cementless porous-coated acetabular cup. Int Orthop 2008; 32 (2): 181-7.
- Garellick G, Malchau H, Herberts P. Survival of hip replacements: A comparison of a randomized trial and a registry. Clin Orthop 2000; (375): 157-67.
- Gjengedal E, Uppheim G, Bjerkholt H, Hovik O, Reikeras O. Excellent results of a femoral press-fit stem cemented with a thin mantle: 116 hips followed for 11-18 years. Eur J Orthop Surg Traumatol 2007; 17: 279-84.
- Hauptfleisch J, Glyn-Jones S, Beard DJ, Gill HS, Murray DW. The premature failure of the Charnley Elite-Plus stem: a confirmation of RSA predictions. J Bone Joint Surg (Br) 2006; 88 (2): 179-83.
- Heilpern GN, Shah NN, Fordyce MJ. Birmingham hip resurfacing arthroplasty: a series of 110 consecutive hips with a minimum five-year clinical and radiological follow-up. J Bone Joint Surg (Br) 2008; 90 (9): 1137-42.
- Herrera A, Canales V, Anderson J, Garcia-Araujo C, Murcia-Mazon A, Tonino AJ. Seven to 10 years followup of an anatomic hip prosthesis: an international study. Clin Orthop 2004; (423): 129-37.
- Hing CB, Back DL, Bailey M, Young DA, Dalziel RE, Shimmin AJ. The results of primary Birmingham hip resurfacings at a mean of five years. An independent prospective review of the first 230 hips. J Bone Joint Surg (Br) 2007; 89 (11): 1431-8.
- Howie DW, Campbell D, McGee M, Cornish BL. Wagner resurfacing hip arthroplasty. The results of one hundred consecutive arthroplasties after eight to ten years. J Bone Joint Surg (Am) 1990; 72 (5): 708-14.
- Ince A, Sauer U, Wollmerstedt N, Hendrich C. No migration of acetabular cups after prophylaxis for heterotopic ossification. Clin Orthop 2007; (461): 125-9.
- Itayem R, Arndt A, Nistor L, McMinn D, Lundberg A. Stability of the Birmingham hip resurfacing arthroplasty at two years. A radiostereophotogrammetric analysis study. J Bone Joint Surg (Br) 2005; 87 (2): 158-62.
- Itayem R, Arndt A, McMinn DJ, Daniel J, Lundberg A. A five-year radiostereometric follow-up of the Birmingham Hip Resurfacing arthroplasty. J Bone Joint Surg (Br) 2007; 89 (9): 1140-3.
- Jacoby WG. The Dot Plot: A Graphical Display for Labeled Quantitative Values. The Political Methodologist 2006; 14 (1): 6-14.
- Kärrholm J, Borssen B, Lowenhielm G, Snorrason F. Does early micromotion of femoral stem prostheses matter? 4-7-year stereoradiographic follow-up of 84 cemented prostheses. J Bone Joint Surg (Br) 1994; 76 (6): 912-7.
- Kesteris U, Robertsson O, Wingstrand H, Onnerfalt R. Cumulative revision rate with the Scan Hip Classic I total hip prosthesis. 1,660 cases followed for 2-12 years. Acta Orthop Scand 1998; 69 (2): 133-7.
- Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg (Am) 2005; 87 (7): 1487-97.
- Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg (Am) 2007; 89 (4): 780-5.
- Latimer HA, Lachiewicz PF. Porous-coated acetabular components with screw fixation. Five to ten-year results. J Bone Joint Surg (Am) 1996; 78 (7): 975-81.
- Liow RY, Murray DW. Which primary total knee replacement? A review of currently available TKR in the United Kingdom. Ann R Coll Surg Engl 1997; 79 (5): 335-40.
- Makela K, Eskelinen A, Pulkkinen P, Paavolainen P, Remes V. Cemented total hip replacement for primary osteoarthritis in patients aged 55 years or older: results of the 12 most common cemented implants followed for 25 years in the Finnish Arthroplasty Register. J Bone Joint Surg (Br) 2008; 90 (12): 1562-9.
- Malchau H. Introducing new technology: a stepwise algorithm. Spine (Phila Pa 1976) 2000; 25 (3): 285.
- McBryde CW, Revell MP, Thomas AM, Treacy RB, Pynsent PB. The influence of surgical approach on outcome in Birmingham hip resurfacing. Clin Orthop 2008; (466) (4): 920-6.
- McCulloch P, Altman DG, Campbell WB, Flum DR, Glasziou P, Marshall JC, . No surgical innovation without evaluation: the IDEAL recommendations. Lancet 2009; 374 (9695): 1105-12.
- Min BW, Song KS, Kang CH, Won YY, Koo KH. Polyethylene liner failure in second-generation harris-galante acetabular components. J Arthroplasty 2005; (6): 717-22.
- Mjoberg B, Franzen H, Selvik G. Early detection of prosthetic-hip loosening. Comparison of low- and high-viscosity bone cement. Acta Orthop Scand 1990; 61 (3): 273-4.
- Mogensen B, Ekelund L, Hansson LI, Lidgren L, Selvik G. Surface replacement of the hip in chronic arthritis. A clinical, radiographic and roentgen stereophotogrammetric evaluation. Acta Orthop Scand 1982; 53 (6): 929-36.
- Muirhead-Allwood SK. Lessons of a hip failure. Bmj 1998; 316 (7132): 644.
- Murray DW, Carr AJ, Bulstrode CJ. Which primary total hip replacement? J Bone Joint Surg (Br) 1995; 77 (4): 520-7.
- Nelissen R G HH, Garling EH, Valstar ER. Influence of cement viscosity and cement mantle thickness on migration of the Exeter total hip prosthesis. J Arthroplasty 2005; (4) 521-58.
- Nelissen RG, Pijls BG, Kärrholm J, Malchau H, Nieuwenhuijse MJ, Valstar ER. RSA and registries: the quest for phased introduction of new implants. J Bone Joint Surg (Am) (Suppl 3) 2011; 93: 62-5.
- NHS National Institute for Clinical Excellence. Guidance on the selection of prostheses for primary total hip replacement. 2003;(http://www.nice.org.uk/nicemedia/pdf/Guidance_on_the_selection_of_hip_prostheses.pdf).
- NJR. New Zealand National Joint Registry Annual Report 2009 (eleven year report) http://wwwcdhbgovtnz/NJR/. 2009: accessed 12-05-2011.
- Önsten I, Bengner U, Besjakov J. Socket migration after Charnley arthroplasty in rheumatoid arthritis and osteoarthritis. A roentgen stereophotogrammetric study. J Bone Joint Surg (Br) 1993; 75 (5): 677-80.
- Önsten I, Carlsson AS. Cemented versus uncemented socket in hip arthroplasty. A radiostereometric study of 60 randomized hips followed for 2 years. Acta Orthop Scand 1994a; 65 (5): 517-21.
- Önsten I, Carlsson AS, Ohlin A, Nilsson JA. Migration of acetabular components, inserted with and without cement, in one-stage bilateral hip arthroplasty. A controlled, randomized study using roentgenstereophotogrammetric analysis. J Bone Joint Surg (Am) 1994b; 76 (2): 185-94.
- Önsten I, Akesson K, Obrant KJ. Micromotion of the acetabular component and periacetabular bone morphology. Clin Orthop 1995; (310): 103-10.
- Önsten I, Carlsson AS, Sanzen L, Besjakov J. Migration and wear of a hydroxyapatite-coated hip prosthesis. A controlled roentgen stereophotogrammetric study. J Bone Joint Surg (Br) 1996; 78 (1): 85-91.
- Oosterbos CJ, Rahmy AI, Tonino AJ. Hydroxyapatite coated hip prosthesis followed up for 5 years. Int Orthop 2001; 25 (1): 17-21.
- Palm L, Olofsson J, Astrom SE, Ivarsson I. No difference in migration or wear between cemented low-profile cups and standard cups : a randomized radiostereographic study of 53 patients over 3 years. Acta Orthop 2007; 78 (4): 479-84.
- Pandit H, Glyn-Jones S, McLardy-Smith P, Gundle R, Whitwell D, Gibbons CL, . Pseudotumours associated with metal-on-metal hip resurfacings. J Bone Joint Surg (Br) 2008; 90 (7): 847-51.
- Partio E, von BH, Wirta J, Avikainen V. Survival of the Lubinus hip prosthesis. An eight- to 12-year follow-up evaluation of 444 cases. Clin Orthop 1994; (303): 140-6.
- Parvizi J, Sullivan T, Duffy G, Cabanela ME. Fifteen-year clinical survivorship of Harris-Galante total hip arthroplasty. J Arthroplasty 2004; 19 (6): 672-7.
- Petersen MB, Poulsen IH, Thomsen J, Solgaard S. The hemispherical Harris-Galante acetabular cup, inserted without cement. The results of an eight to eleven-year follow-up of one hundred and sixty-eight hips. J Bone Joint Surg (Am) 1999; 81 (2): 219-24.
- Pijls BG, Dekkers OM, Middeldorp S, Valstar ER, Van der Heide HJ, Van der Linden-Van der Zwaag HM, . AQUILA: Assessment of QUality In Lower limb Arthroplasty: An expert Delphi consensus for total knee and total hip arthroplasty. BMC Musculoskelet Disord. 2011; 12 (1): 173.
- Putter H, Fiocco M, Stijnen T. Meta-analysis of diagnostic test accuracy studies with multiple thresholds using survival methods. Biom J 2009; 52 (1): 95-110.
- Ragab AA, Kraay MJ, Goldberg VM. Clinical and radiographic outcomes of total hip arthroplasty with insertion of an anatomically designed femoral component without cement for the treatment of primary osteoarthritis - A study with a minimum of six years of follow-up. J Bone Joint Surg (Am) 1999; 81 (2): 210-8.
- Ricci WM, Westrich GH, Lorei M, Cazzarelli JF, Pellicci PM, Sculco TP, . Primary total hip replacement with a noncemented acetabular component: minimum 5-year clinical follow-up. J Arthroplasty 2000; 15 (2): 146-52.
- Rogers A, Kulkarni R, Downes EM. The ABG hydroxyapatite-coated hip prosthesis: one hundred consecutive operations with average 6-year follow-up. J Arthroplasty 2003; 18 (5): 619-25.
- Rohrl S, Nivbrant B, Mingguo L, Hewitt B. In vivo wear and migration of highly cross-linked polyethylene cups a radiostereometry analysis study. J Arthroplasty 2005; 20 (4): 409-13.
- Ryd L. Roentgen stereophotogrammetric analysis of prosthetic fixation in the hip and knee joint. Clin Orthop 1992; (276): 56-65.
- Ryd L, Albrektsson BE, Carlsson L, Dansgard F, Herberts P, Lindstrand A, . Roentgen stereophotogrammetric analysis as a predictor of mechanical loosening of knee prostheses. J Bone Joint Surg (Br) 1995; 77 (3): 377-83.
- Schemitsch EH, Bhandari M, Boden SD, Bourne RB, Bozic KJ, Jacobs JJ, . The evidence-based approach in bringing new orthopaedic devices to market. J Bone Joint Surg (Am) 2010; 92 (4): 1030-7.
- SHAR. Swedish Hip Arthroplasty Registry Report 2009. http://wwwshprse/Libraries/Documents/AnnualReport-2009-ENsflbashx. 2009: accessed 16-1-2011.
- Sheth U, Nguyen NA, Gaines S, Bhandari M, Mehlman CT, Klein G. New orthopedic devices and the FDA. J Long Term Eff Med Implants 2009; 19 (3): 173-84.
- Sinha RK, Dungy DS, Yeon HB. Primary total hip arthroplasty with a proximally porous-coated femoral stem. J Bone Joint Surg (Am) 2004; 86 (6): 1254-61.
- Snorrason F, Kärrholm J. Primary migration of fully-threaded acetabular prostheses. A roentgen stereophotogrammetric analysis. J Bone Joint Surg (Br) 1990; 72 (4): 647-52.
- Snorrason F, Kärrholm J, Holmgren C. Fixation of cemented acetabular prostheses. The influence of preoperative diagnosis. J Arthroplasty 1993; 8 (1): 83-90.
- Steffen RT, Pandit HP, Palan J, Beard DJ, Gundle R, Lardy-Smith P, . The five-year results of the Birmingham Hip Resurfacing arthroplasty: an independent series. J Bone Joint Surg (Br) 2008; 90 (4): 436-41.
- Stocks GW, Freeman MA, Evans SJ. Acetabular cup migration. Prediction of aseptic loosening. J Bone Joint Surg (Br) 1995; 77 (6): 853-61.
- Surdam JW, Archibeck MJ, Schultz SC, Jr., Junick DW, White RE, Jr. A second-generation cementless total hip arthroplasty mean 9-year results. J Arthroplasty 2007; 22 (2): 204-9.
- Thanner J, Freij-Larsson C, Kärrholm J, Malchau H, Wesslen B. Evaluation of Boneloc. Chemical and mechanical properties, and a randomized clinical study of 30 total hip arthroplasties. Acta Orthop Scand 1995; 66 (3): 207-14.
- Thanner J, Kärrholm J, Malchau H, Wallinder L, Herberts P. Migration of press-fit cups fixed with poly-L-lactic acid or titanium screws: a randomized study using radiostereometry. J Orthop Res 1996; 14 (6): 895-900.
- Thanner J, Kärrholm J, Malchau H, Herberts P. Poor outcome of the PCA and Harris-Galante hip prostheses. Randomized study of 171 arthroplasties with 9-year follow-up. Acta Orthop Scand 1999; 70 (2): 155-62.
- Thien TM, Ahnfelt L, Eriksson M, Stromberg C, Kärrholm J. Immediate weight bearing after uncemented total hip arthroplasty with an anteverted stem: a prospective randomized comparison using radiostereometry. Acta Orthop 2007; 78 (6): 730-8.
- Tompkins GS, Jacobs JJ, Kull LR, Rosenberg AG, Galante JO. Primary total hip arthroplasty with a porous-coated acetabular component. Seven-to-ten-year results. J Bone Joint Surg (Am) 1997; 79 (2): 169-76.
- Vochteloo AJ, Pijls BG, van der Heide HJ. Sutures v staples. Let’s add three other studies. Bmj 2010; 340: c2627.
- von Schewelov T, Sanzen L, Önsten I, Carlsson A. Catastrophic failure of an uncemented acetabular component due to high wear and osteolysis - An analysis of 154 Omnifit prostheses with mean 6-year follow-up. Acta Orthop Scand 2004; 75 (3): 283-94.
- von Schewelov T, Sanzen L, Önsten I, Carlsson A, Besjakov J. Total hip replacement with a zirconium oxide ceramic femoral head: a randomised roentgen stereophotogrammetric study. J Bone Joint Surg (Br) 2005; 87 (12): 1631-5.
- Williams S, Isaac G, Porter N, Fisher J, Older J. Long-term radiographic assessment of cemented polyethylene acetabular cups. Clin Orthop 2008; 466 (2): 366-72.
- Woolson ST, Haber DF. Primary total hip replacement with insertion of an acetabular component without cement and a femoral component with cement - Follow-up study at an average of six years. J Bone Joint Surg (Am) 1996; 78 (5): 698-705.
Data sharing
Statistical code and dataset are available upon request from the corresponding author. R code for the analysis described in the Appendix is available from one of the authors (e-mail [email protected]). Supplementary data
Appendix is available at our website (www.actaorthop.org), identification number 5482.