Abstract
Purpose We performed two parallel systematic reviews and meta-analyses to determine the association between early migration of tibial components and late aseptic revision.
Methods One review comprised early migration data from radiostereometric analysis (RSA) studies, while the other focused on revision rates for aseptic loosening from long-term survival studies. Thresholds for acceptable and unacceptable migration were determined according to that of several national joint registries: < 5% revision at 10 years.
Results Following an elaborate literature search, 50 studies (involving 847 total knee prostheses (TKPs)) were included in the RSA review and 56 studies (20,599 TKPs) were included in the survival review. The results showed that for every mm increase in migration there was an 8% increase in revision rate, which remained after correction for age, sex, diagnosis, hospital type, continent, and study quality. Consequently, migration up to 0.5 mm was considered acceptable during the first postoperative year, while migration of 1.6 mm or more was unacceptable. TKPs with migration of between 0.5 and 1.6 mm were considered to be at risk of having revision rates higher than 5% at 10 years.
Interpretation There was a clinically relevant association between early migration of TKPs and late revision for loosening. The proposed migration thresholds can be implemented in a phased, evidence-based introduction of new types of knee prostheses, since they allow early detection of high-risk TKPs while exposing only a small number of patients.
Worldwide, several hundred thousand total knee prostheses (TKPs) are implanted each year and this number is expected to increase by a factor of 6 within the next 2 decades (Kurtz et al. Citation2005, Citation2007). Most of the new TKP designs have been introduced to the market without being shown to be safe or effective (Sheth et al. Citation2009). This has resulted in the widespread use of TKPs with failure rates exceeding 10 times the standard of national joint registries (< 5% failures at 10-year follow-up), such as the Accord, St Leger, and Journey-Deuce (Norton et al. Citation2002, Gilbert et al. Citation2009, Sheth et al. Citation2009, Palumbo et al. 2011 (personal communication)). To guarantee patient safety, several countries have developed guidelines, e.g. the NICE guidelines for total hip prostheses (2003). Furthermore, it has become increasingly evident that a phased, evidence-based introduction, as is common for pharmaceuticals, is needed to regulate the introduction of new TKPs to the market (CitationMalchau 2000, McCulloch et al. Citation2009, Schemitsch et al. Citation2010). This should include systematic assessment and early detection of the major cause of TKP failure, which is aseptic loosening of the tibial component necessitating revision surgery (2003, CitationAJR 2010).
Although it can take 10 years before loosening causes symptoms, it is possible to detect loosening early postoperatively using radiostereometric analysis (RSA) (Selvik 1989, Grewal et al. Citation1992, Karrholm et al. Citation1994, Ryd et al. Citation1995). Since RSA allows in vivo, 3D measurement of the migration of TKPs with an accuracy of 0.2 mm for translations and 0.5 degrees for rotations, only a small number of patients need be exposed to potentially unsafe TKPs (Grewal et al. Citation1992, Ryd et al. Citation1995, Nelissen et al. Citation1998). RSA could therefore play an important role in the phased, evidence-based introduction of new TKPs (Selvik Citation1989, Karrholm et al. Citation1994, Ryd et al. Citation1995). However, the evidence for the relationship between early migration and TKP revision for aseptic loosening is limited to a few studies from the 1990s (Grewal et al. Citation1992, Ryd et al. Citation1995). Furthermore, the applicability of these studies is restricted, because surgical technique, fixation methods, implant design, and polyethylene have evolved since their publication.
We hypothesized that early migration of the tibial component, measured through RSA, is associated with late revision for aseptic loosening of TKPs. We therefore systematically reviewed the association between early migration and late aseptic revision for the tibial component in TKPs. This could ultimately lead to clinical guidelines to be used in a phased introduction of new TKPs.
Material and methods
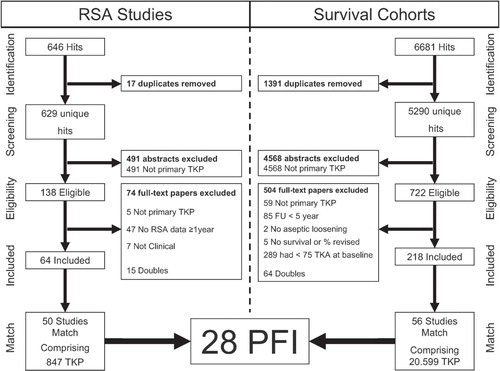
We performed two parallel systematic reviews (international registration number NTR2417; www.trialregister.nl) of studies of patients who received TKPs for end-stage osteoarthritis (OA) or rheumatoid arthritis (RA). One review comprised data on early migration of TKPs from RSA studies. From the other, we determined the long-term revision rates for aseptic loosening of TKPs from survival studies (). During all stages of the review process, a referee (RN) with over 20 years of experience in both RSA and TKR was available for consultation.
Figure 1. PRISMA flow chart of both reviews. Details of the 28 PFI combinations are given in Table 1. RSA: radiostereometric analysis; TKP: total knee prosthesis; FU: follow-up; PFI: prosthesis-fixation-insert combination.
Systematic review of RSA studies
Literature search. A thorough literature search was performed together with a medical librarian (JP), to reduce bias by increasing the likelihood of retrieving all relevant studies (Vochteloo et al. Citation2010). The following bibliographies were searched up to 2009: PubMed, Embase, Web-of-Science, and the Cochrane Library. Relevant articles were screened for additional references. Additionally, a separate search was conducted in 9 leading orthopedic and biomechanical journals (Acta Orthop, Clin Orthop Relat Res, J Arthroplasty, J Bone Joint Surg (Am and Br), Knee Surg Sports Traumatol Arthrosc, J Orthop Res, J Biomech, and Clin Biomech). Finally, Google Scholar was used. Articles in English, French, Italian, Spanish, Dutch, and German were considered. The search strategy consisted of the following components, each defined by a combination of controlled vocabulary and free text terms: (1) RSA, and (2) joint replacement. See Appendix (Supplementary data) for more details on the strategy and terms.
Inclusion and exclusion analysis. Initial screening on the basis of title and abstract of RSA studies was performed by BP to identify studies on patients treated with TKPs for OA or RA. When the information in the abstract did not suffice or where there was any doubt, the studies remained eligible. The full text of eligible studies was independently evaluated in duplicate by 2 reviewers (BP and EV). The inclusion criteria for RSA studies were: (1) primary TKP, and (2) minimal RSA follow-up of 1 year, measuring tibial component migration. Non-clinical studies (animal, phantom) were excluded.
Data extraction. BP and KN independently extracted migration data in duplicate from the RSA studies. Migration data comprised translations, rotations, and maximal total point motion (MTPM) of the tibial component in the first postoperative year. MTPM is the unit of measurement for the largest 3D migration of any point on the prosthesis surface (Ryd et al. Citation1995). Data concerning patient demographics and regional influences were also extracted to allow for confounder correction.
Quality assessment. The quality of the RSA studies was independently appraised in duplicate by BP and KN at the level of outcome using the AQUILA methodological score (Pijls et al. Citation2011). For the RSA studies, we modified the AQUILA by removing items not considered relevant for early migration: long-term follow-up and the revision assessment.
Systematic review of survival studies
Literature search. The search strategy and bibliographies were the same as those in the RSA review, with the exception of the components of the search strategy. The search strategy for the survival studies consisted of the following components, each defined by a combination of controlled vocabulary and free text terms: (1) joint replacement, (2) implant failure, and (3) survival analysis. See Appendix for more details of the strategy and terms. In the search strategy, no distinction was made between total knee prostheses and total hip prostheses (THPs), because some studies reported on both TKPs and THPs (Ryd Citation1992).
Inclusion and exclusion analysis. The procedure of screening the survival studies for eligibility, and subsequent inclusion and exclusion analysis, was identical to the procedures for the RSA studies, with the exception of inclusion and exclusion criteria. The inclusion criteria for survival studies were (1) primary TKP; (2) follow-up of 5, 10, 15, 20, or 25 years; (3) endpoint revision surgery for aseptic loosening of the tibial component, or indication for revision surgery in patients with poor general health or decline; and (4) survival or percentage revised to be available for specific follow-up (see point 2). Studies with less than 75 TKPs at baseline were excluded.
Data extraction. From the survival studies, BP and KN independently determined the revision rates for aseptic loosening of the tibial component at 5-year intervals. Data concerning patient demographics and regional influences were extracted to allow for confounder correction.
Quality assessment. The quality of the survival studies was independently appraised in duplicate by BP and KN at the level of outcome using the AQUILA methodological score (Pijls et al. Citation2011).
Analysis
A detailed description of the analysis, methodology, and a worked example are available in the online Appendix (see Supplementary data). To determine the association between early migration and late revision, we matched the results from the RSA review to the results of the survival review on type of prosthesis, fixation method (e.g. cement or bone ingrowth), and articulating insert (e.g. modular or non-modular). The combination was termed PFI. Since PFI involves technical factors known to be associated with both migration and the likelihood of revision for aseptic loosening, matching on PFI prevents confounding by PFI (CitationDKAR 2009, CitationNJR 2009, CitationAJR 2010, CitationSKAR 2010). Depending on the studies available, it was possible that there would be more than 1 combination of matching RSA and survival studies for a particular PFI. For instance, if there are 3 RSA studies and 2 survival studies for the same PFI, then there are 6 possible combinations (3 times 2). All combinations were considered in the analysis. A meta-analysis for the revision rate at 5 years was performed. A model for the censoring mechanism was employed to reconstruct the data and then a generalized linear mixed model with study as a random effect was applied to estimate the survival at 5 years and its 95% confidence interval (CI) (Fiocco et al. Citation2009, 2011, Putter et al. Citation2009). Regarding the RSA studies, pooling of migration results at the level of PFI was based on weights according to study size (N).
The 10-year results for TKPs with high revision rates may not be published once the 5-year results have been published. Since 10-year revision rates in the registries are on average 1.7 times higher than 5-year revision rates, any missing 10-year results were estimated on 5-year results by applying a factor of 1.7. This method was validated by comparing the estimated 10-year results with the known 10-year results, for the complete cases (CitationDKAR 2009, CitationNJR 2009, CitationAJR 2010, CitationSKAR 2010).
Adjustment for confounding
Since migration data and revision rate data were extracted from different studies, differences between study populations might confound the observed association. In order to address this issue, we determined the degree of similarity of the population from RSA and survival study combinations, expressed by a match score, for age, sex, diagnosis, hospital type, and continent. The match score was constructed according to the results of a recent Delphi survey among an international group of 37 independent experts, and can vary between 5 (excellent) and 0 (poor) (Pijls et al. Citation2011). The RSA study and survival study combination scored 1 point for each of the following 5 criteria (up to a maximum of 5 points): (1) the difference in mean age between the patients from RSA study and those from the survival study was 5 years or less; (2) the difference in percentage of females between the RSA study and survival study was 10% or less; (3) the difference in percentage of patients diagnosed with osteoarthritis between the RSA study and the survival study was 10% or less; (4) the RSA study and the survival study were performed in similar types of hospital (e.g. both university medical centers); (5) the RSA study and the survival study were performed on the same continent. All other cases scored zero points.
We used a weighted regression model to assess the association between early migration and late aseptic revision corrected for match score, RSA study quality, survival study quality, number of TKP in the RSA studies, and number of TKP in the survival studies.
Migration thresholds
According to the principle of “primum non nocere“ (first do no harm), new implant designs should perform at least as well as the revision standard of national registries: < 3% revision at 5 years and < 5% revision at 10 years (CitationDKAR 2009, CitationNJR 2009, CitationAJR 2010, CitationSKAR 2010). Based on this revision standard, the following 3 categories were constructed for the phased introduction of new TKPs: “acceptable”, “at risk”, and “unacceptable”. The “acceptable” category was defined as the level of migration up to which all survival studies have lower revision rates than the standard. The “unacceptable” category was defined as the level of migration from which all revision rates are higher than the standard. The category “at risk” was defined as the migration interval between the “acceptable” and “unacceptable” thresholds, in which studies with revision rates lower and higher than the standard were observed.
Appraisal of publication bias
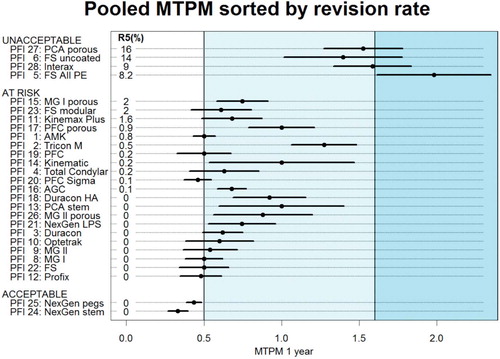
We assessed the potential effect of publication bias by comparing the results from the meta-analysis to the results from national joint registries, since they do not suffer from publication bias (CitationDKAR 2009, CitationNJR 2009, CitationAJR 2010, CitationSKAR 2010). Accordingly, the PFI combinations that perform better than average in the meta-analysis should also perform better than average in the national joint registries. The same principle also applies to PFI combinations that perform worse than average. For this purpose, the migration pooled according to the specific combination of prosthesis type, fixation method and articulating insert (PFI) and visualized in a dot chart (Jacoby Citation2006).
Results
RSA studies
The literature search yielded 629 hits for the RSA review and 50 studies were included, covering a total of 847 patients (Ryd et al. Citation1986, Citation1987, Citation1988, Citation1990, Citation1993, Albrektsson et al. Citation1990, Citation1992, Nilsson et al. Citation1991, Citation1993, Citation1998, Citation2006, Hilding et al. Citation1995, Citation2006, Citation2007, Nielsen et al. Citation1995, Nelissen et al. Citation1998, Onsten et al. Citation1998, Toksvig-Larsen et al. Citation1998, Adalberth et al. Citation1999, Citation2000, Citation2001, Citation2002, Østgaard et al. Citation1999, Li et al. Citation2000, Toksvig-Larsen et al. Citation2000, Uvehammer et al. Citation2001, Hildebrand et al. Citation2003, Catani et al. Citation2004, Kienapfel et al. Citation2004, Norgren et al. Citation2004, Dalen et al. Citation2005, Hyldahl et al. Citation2005a, Citationb, Henricson et al. Citation2006, Muller et al. Citation2006, van der Linde et al. Citation2006a,Citationb, Uvehammer et al. Citation2007, Wilson et al. Citation2007, Hansson et al. Citation2008, Henricson et al. Citation2008, Therbo et al. Citation2008, von Schewelov et al. Citation2008). Details of the study selection and flow of the review are given in . The mean quality score of the RSA studies was 3.8 (SD 1.7) on a 7-point scale. MTPM at 1 year was the most frequently and most consistently reported migration value: 44 out of 50 RSA studies reported it. Translations and rotations of the tibial component were reported infrequently and inconsistently, and did not allow a meaningful analysis. Thus, all analyses focused on MTPM at 1 year.
Survival studies
The literature search resulted in 5,290 hits for the survival review and 56 studies were included, with a total of 20.599 patients; see (Goldberg et al. Citation1988, Laskin Citation1990, Samuelson et al. Citation1990, Wright et al. Citation1990, Moran et al. Citation1991, Grewal et al. Citation1992, Ranawat et al. Citation1993, Citation1994, Rinonapoli et al. Citation1994, Weir et al. Citation1996, Knight et al. Citation1997, Scott Citation1997, Ansari et al. Citation1998, Hsu et al. Citation1998, Ewald et al. Citation1999, Mont et al. Citation1999, Buehler et al. Citation2000, Emerson et al. Citation2000, Robertsson et al. Citation2000, Stukenborg-Colsman et al. Citation2000, Berger et al. Citation2001a,Citationb Faraj et al. Citation2001, Gill et al. Citation2001, Khaw et al. Citation2001, Schroder et al. Citation2001, Sextro et al. Citation2001, Fetzer et al. Citation2002, Forster et al. Citation2002, Khaw et al. Citation2002, Worland et al. Citation2002, Mayman et al. Citation2003, Goldberg et al. Citation2004, Arora et al. Citation2005, Bozic et al. Citation2005, Campbell et al. Citation2006, Clayton et al. Citation2006, Gioe et al. Citation2006, Lachiewicz et al. Citation2006, Vessely et al. Citation2006, Bertin Citation2007, Kim et al. Citation2007, Rodricks et al. Citation2007, Zaki et al. Citation2007, Anderson et al. Citation2008, Chana et al. Citation2008, Dalury et al. Citation2008, Parsch et al. Citation2008, Ritter et al. Citation2008, Santini et al. Citation2008, Smith et al. Citation2008). The mean quality score of the survival studies was 6.0 (SD 1.8) on an 11-point scale.
Early migration and late revision
The matching procedure resulted in 28 different PFI combinations and 89 combinations of RSA and survival studies (). There was a clear association between early migration, expressed as MTPM at 1 year, and the 5-year revision rate as expressed as prosthesis survival (). For every mm of increase in migration, 7.6% (CI: 5.7–9.5) was added to the 5-year revision rate (p < 0.001). The influence of RSA study quality, survival study quality, number of TKPs in the RSA study, number of TKPs in the survival study, and match score were small relative to the overall effect of migration on revision rate ().
Table 1. Prosthesis, Fixation and Insert (PFI) characteristics.
Figure 2. Scatter plot showing association between migration in the first postoperative year expressed as maximal total point motion (MTPM) in mm and revision rate for aseptic loosening of the tibial component at 5 years, as a percentage. The colored lines are derived from weighted regression according to match quality, survival study quality, and RSA study quality (the coefficients and 95% CI are given in Table 2).
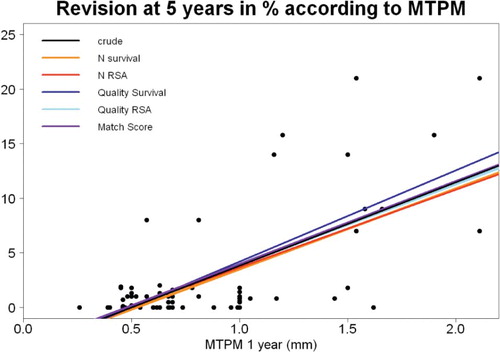
Table 2. Association between MTPM at 1 year and revision rate for aseptic loosening at 5 years
For TKPs that rely on primary fixation (cemented and uncemented with screws), 7.1% (CI: 4.7–9.5) was added to the 5-year revision rate for every 1 mm increase in MTPM (p <0.001). For TKPs that rely on secondary fixation (uncemented without screws), 10% (CI: 2.7–17) was added to the 5-year revision rate for every 1 mm increase in MTPM (p = 0.018).
Migration thresholds
shows the 3 categories for the migration of TKP. For MTPM at 1 year of between 0 mm and 0.54 mm, there was no tibial component with more than 3% revision for aseptic loosening at 5 years. With 1-year MTPM of more than 1.6 mm, no tibial components had less than 3% revision for aseptic loosening at 5 years. This indicates that acceptance of 3% revision at 5 years resulted in a threshold of 0.54 mm or acceptable MTPM at 1 year, and a threshold of 1.6 mm for unacceptable MTPM at 1 year. For the 10-year revision rates, the thresholds for acceptable and unacceptable migration were 0.45 mm and 1.6 mm, respectively ().
Figure 3. Scatter plot showing the relation between MTPM at 1 year and revision of the tibial component for aseptic loosening at 5 years. The thresholds of 0.54 mm and 1.6 mm for the three categories (acceptable, at risk, and unacceptable) are shown.
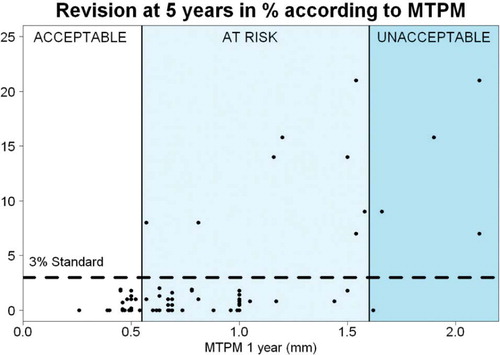
Figure 4. Scatter plot showing the relation between MTPM at 1 year and revision of the tibial component for aseptic loosening at 10 years. The thresholds of 0.45 mm and 1.6 mm for the three categories (acceptable, at risk, and unacceptable) are shown.
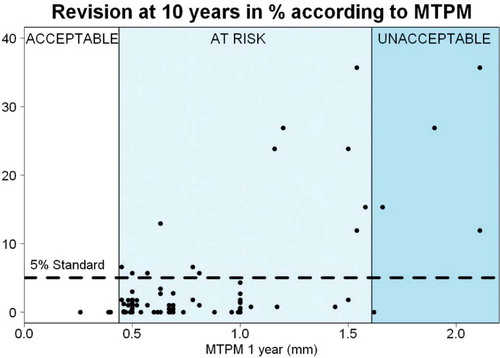
The mean difference between the estimated 10-year revision rate and the known 10-year revision rate was 0.17% (SD 2.1), indicating that there was no systematic error. The 5-year revision rates for the studies with missing 10-year revision rates were already higher than the 10-year revision rate of 5% that is considered to be acceptable. Thus, the 10-year thresholds were not influenced by any missing values.
Publication bias
The pooled MTPM ranked by the pooled revision rate for each PFI combination is presented in . The PFI combinations that migrated statistically significantly less than the acceptable threshold—classified as acceptable—have had excellent track records and low revision rates in several national joint registries (CitationDKAR 2009, CitationNJR 2009, CitationAJR 2010, CitationSKAR 2010). Conversely, the PFI combinations that were classified as unacceptable on basis of their pooled migration have been abandoned and are no longer used. The possible influence of publication bias on the results was therefore small.
Figure 5. Dot chart showing the pooled MTPM ranked by the pooled revision rate for each PFI combination. The acceptable PFI combinations (based on migration) had excellent track records and low revision rates in several national registries, whereas the unacceptable PFI combinations (based on migration) have been abandoned. Thus, the potential influence of publication bias on the results is small. A detailed description of each PFI combination is given in Table 1. R5(%): pooled revision rate at 5-year follow-up, as a percentage.
Discussion
The results of this systematic review show a clinically relevant association between early migration, as measured with RSA, and long-term clinical failure resulting in revision for aseptic loosening. Each mm of migration was associated with an increase in 5-year revision rate of 8%, which remained after correction for age, sex, diagnosis, hospital type, continent, and study quality. This is more than twice the standard revision rate of several national joint registries (CitationDKAR 2009, CitationNJR 2009, CitationAJR 2010, CitationSKAR 2010). The results of this systematic review show that RSA studies can identify unsafe TKPs (in terms of aseptic loosening) as early as 1 year postoperatively. Early identification of unsafe TKPs with RSA should prevent their widespread use and save numerous patients from extensive revision surgery, possibly with postoperative complications.
Some strengths of this systematic review are the large numbers of studies included (> 100) and of patients included (> 27,000), which resulted in 28 different PFI combinations. This large variation, which reflects the diversity of TKP designs and fixation methods, ensures wide generalizability of the results. Since the migration and revision rates were from different studies, there were no migration data available in the survival studies to be incorporated into the decision to perform a revision. Thus, there is no incorporation bias in our results. We consider the risk of publication bias in this systematic review to be small, since the results from the meta-analysis are similar to those from the national joint registries, which do not suffer from publication bias. Confounders had only a small influence on the association between early migration and long-term aseptic revision.
We should also consider some limitations. The quality of the survival and RSA studies showed large variation. High methodological quality of all the studies included would have been desirable. Nevertheless, the quality of the survival studies and the RSA studies showed only very small effects on the association between migration and revision rates.
We focused on MTPM at 1 year postoperatively, but other migration parameters and follow-up beyond 1 year would also be of interest (CitationRyd et al. 1995). Unfortunately, these parameters were reported too infrequently and inconsistently to permit a meaningful analysis. Future RSA studies could therefore benefit from further standardization, particularly regarding the reporting of the results (Valstar et al. Citation2005).
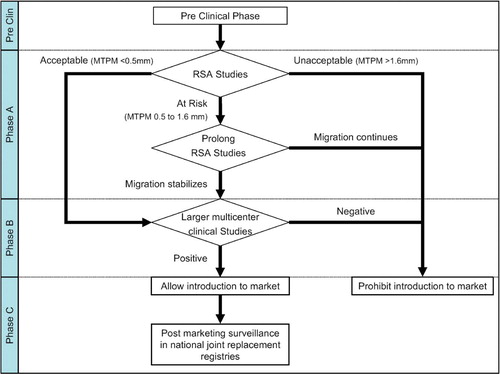
We also recognize that RSA only evaluates aseptic loosening while other failure mechanisms (e.g. infection, pain, and instability or pseudotumors in metal-on-metal total arthroplasty) cannot be evaluated by RSA. As a consequence, RSA studies are only the first step in the phased, evidence-based introduction of TKPs—as proposed by CitationMalchau (2000); see . During phase A, several single-center RSA studies should be performed to determine the safety of the TKP with regard to the risk of revision for aseptic loosening. If the TKP is considered safe, phase B studies should be conducted to evaluate the clinical performance of the TKP regarding pain relief and functioning (clinical scores and patient-reported outcome measures (PROMS)) and to determine the rate of expected or unexpected complications. Since RSA studies have already evaluated the risk of aseptic loosening, follow-up of 2 years instead of 10 years would be sufficient. This reduces the follow-up needed for a successful phased introduction by almost a decade compared to traditional cohort studies. After release on the market (phase C), the performance of the TKP must be monitored by post-marketing surveillance in national joint replacement registries (Schemitsch et al. Citation2010). This includes both the revision rate and patient evaluations using PROMS.
Figure 6. Flow chart showing the role of RSA studies in the phased evidence-based introduction of new TKPs, modified according the Malchau proposal. Stabilization is defined as migration of less than 0.2 mm in the second postoperative year (MTPM from year 1 to year 2) as described by CitationRyd et al. (1995). See discussion for details of each phase.
In this systematic review, RSA studies of 20–60 patients followed for 1 year led to the same conclusion as national joint registries with thousands of patients followed for 5–10 years. A recent publication has shown a 22–35% reduction in the number of revisions of RSA-tested total knee replacements as compared to non-RSA-tested total knee replacements in the national joint registries (Nelissen et al. Citation2011). Because inferior designs can already be detected early postoperatively, exposing only a small group of patients to potentially unsafe TKPs, RSA provides the necessary efficiency to make possible phased, evidence-based introduction. Now the observed association between early migration and long-term revision translates into practical thresholds that can lead to clinical guidelines for phased, evidence-based introduction of new TKPs.
Various authors and regulatory agencies recognize the potential of RSA (Grewal et al. Citation1992, Bulstrode et al. Citation1993, Karrholm et al. Citation1994, CitationRyd et al. 1995, CitationMalchau 2000, Hauptfleisch et al. Citation2006). The NICE guidelines of 2003 (UK) require adequate long-term clinical data for hip prostheses and indicate that RSA is an alternative to long-term follow-up studies. The Dutch Orthopaedic Society now requires a phased introduction with mandatory RSA studies before any new hip prosthesis is considered for introduction to the Dutch market (2011). Official guidelines for knee prostheses are expected to follow.
In light of the recent disasters with introduction of new orthopedic implants to the market, a phased, clinical introduction for new TKPs is mandatory to prevent patients from receiving potentially unsafe TKPs when standard TKPs with excellent long-term track records are available.
In conclusion, we found a clinically relevant association between early migration of TKPs and late revision for loosening. The proposed migration thresholds can be implemented in a phased, evidence-based introduction, since they allow early detection of TKPs with a high risk of aseptic loosening while exposing only a small number of patients.
www.actaorthop.org
Download PDF (271.4 KB)RN, BP, and EV had the idea for the study. SM provided methodological input and MF provided statistical input during the conceptual phase of the study. JP designed the search strategy for the literature search. BP and EV performed the study selection and matching procedure. KN and BP appraised the quality of the literature and performed the data extraction. MF and BP analyzed the data. BP, KN, EV, and RN wrote the initial draft manuscript. MF and SM ensured the accuracy of data and analysis. BP and MF wrote the Appendix. Critical revision of the manuscript was performed by all authors. All authors read and approved the final manuscript.
The authors thank the Atlantic Innovation Fund (Atlantic Canada Opportunities Agency) for providing funding for this study (contract no. 191933). The Atlantic Innovation Fund did not take part in the design or conduct of the study; in the collection, management, analysis, or interpretation of the data; or in the preparation, review, or approval of the manuscript.
- Adalberth G, Nilsson KG, Bystrom S, Kolstad K, Mallmin H, Milbrink J. Stability assessment of a moderately conforming all-polyethylene tibial component in total knee arthroplasty: a prospective RSA study with 2 years of follow-up of the Kinemax Plus design. Am J Knee Surg 1999; 12 (4): 233-40.
- Adalberth G, Nilsson KG, Bystrom S, Kolstad K, Milbrink J. Low-conforming all-polyethylene tibial component not inferior to metal-backed component in cemented total knee arthroplasty: prospective, randomized radiostereometric analysis study of the AGC total knee prosthesis. J Arthroplasty 2000; 15 (6): 783-92.
- Adalberth G, Nilsson KG, Bystrom S, Kolstad K, Milbrink J. All-polyethylene versus metal-backed and stemmed tibial components in cemented total knee arthroplasty. A prospective, randomised RSA study. J Bone Joint Surg (Br) 2001; 83 (6): 825-31.
- Adalberth G, Nilsson KG, Karrholm J, Hassander H. Fixation of the tibial component using CMW-1 or Palacos bone cement with gentamicin: similar outcome in a randomized radiostereometric study of 51 total knee arthroplasties. Acta Orthop Scand 2002; 73 (5): 531-8.
- AJR.Australian Orthopaedic Association National Joint Replacement Registry Annual Report 2010 http://wwwdmacadelaideeduau/aoanjrr/publicationsjsp?section=reports2010. 2010:accessed 12-05-2011.
- Albrektsson BE, Ryd L, Carlsson LV, Freeman MA, Herberts P, Regner L, . The effect of a stem on the tibial component of knee arthroplasty. A roentgen stereophotogrammetric study of uncemented tibial components in the Freeman-Samuelson knee arthroplasty. J Bone Joint Surg (Br) 1990; 72 (2): 252-8.
- Albrektsson B EJ, Carlsson LV, Freeman M AR, Herberts P, Ryd L. Proximally cemented versus uncemented Freeman-Samuelson knee arthroplasty. A prospective randomised study. J Bone Joint Surg (Br) 1992; 74 (2) :233-8.
- Anderson JA, Baldini A, Sculco TP. Patellofemoral function after total knee arthroplasty: a comparison of 2 posterior-stabilized designs. J Knee Surg 2008; 21: 91-6.
- Ansari S, Ackroyd CE, Newman JH. Kinematic posterior cruciate ligament-retaining total knee replacements. A 10-year survivorship study of 445 arthroplasties. Am J Knee Surg 1998; 11 (1): 9-14.
- Arora J, Ogden AC. Osteolysis in a surface-cemented, primary, modular Freeman-Samuelson total knee replacement. J Bone Joint Surg (Br) 2005; 87 (11): 1502-6.
- Berger R, Lyon JH, Jacobs JJ, Barden RM, Berkson EM, Sheinkop MB, . Problems with cementless total knee arthroplasty at 11 years follow-up. Clin Orthop 2001a; (392): 196-207.
- Berger RA, Rosenberg AG, Barden RM, Sheinkop MB, Jacobs JJ, Galante JO. Long-term followup of the Miller-Galante total knee replacement. Clin Orthop 2001b; (388): 58-67.
- Bertin KC. Tibial component fixation in total knee arthroplasty: a comparison of pegged and stemmed designs. J Arthroplasty 2007; 22 (5): 670-8.
- Bozic KJ, Kinder J, Menegini M, Zurakowski D, Rosenberg AG, Galante JO. Implant survivorship and complication rates after total knee arthroplasty with a third-generation cemented system. Clin Orthop 2005; (430): 117-24.
- Buehler KO, Venn-Watson E, D’Lima DD, Colwell CW, Jr. The press-fit condylar total knee system: 8- to 10-year results with a posterior cruciate-retaining design. J Arthroplasty 2000; 15 (6): 698-701.
- Bulstrode CJ, Murray DW, Carr AJ, Pynsent PB, Carter SR. Designer hips. Bmj 1993; 306 (6880): 732-3.
- Campbell DG, Duncan WW, Ashworth M, Mintz A, Stirling J, Wakefield L, . Patellar resurfacing in total knee replacement. A ten year randomised prospective trial. J Bone Joint Surg (Br) 2006; 88: 734-9.
- Catani F, Leardini A, Ensini A, Cucca G, Bragonzoni L, Toksvig-Larsen S, . The stability of the cemented tibial component of total knee arthroplasty: posterior cruciate-retaining versus posterior-stabilized design. J Arthroplasty 2004; 19 (6): 775-82.
- Chana R, Shenava Y, Nicholl AP, Lusted FJ, Skinner PW, Gibb PA. Five to 8 year results of the uncemented Duracon total knee arthroplasty system. J Arthroplasty 2008; 23 (5): 677-82.
- Clayton R A , Amin A, Gaston MS, Brenkel IJ. Five year results of the Sigma total knee arthroplasty. The Knee 2006; 13: 359-64.
- Dalen T, Nilsson KG. VersaBond bone cement prospective randomized study of the clinical properties of a new bone cement in total knee replacement. Knee 2005; 12 (4): 311-7.
- Dalury DF, Barrett WP, Mason JB, Goldstein WM, Murphy J, Roche MW. Midterm survival of a contemporary modular total knee replacement. J Bone Joint Surg (Br) 2008; 90: 1594-6.
- Dutch Orthopaedic Society (NOV) guideline total hip prosthesis 2011: http://www.kwaliteitskoepel.nl/assets/structured-files/2011/Richtlijn+Totale+Heupprothese+2010+zonder+watermerk.pdf
- DKAR.Danish Knee Arthroplasty Registry Report 2009. http://wwwkneedk/groups/dkr/pdf/DKRreportEnglish2010pdf. 2009:accessed 12-05-2011.
- Emerson RH, Higgins LL, Head WC. The AGC total knee prosthesis at average 11 years. J Arthroplasty 2000; 15 (4): 418-23.
- Ewald FC, Wright RJ, Poss R, Thomas WH, Mason MD, Sledge CB. Kinematic total knee arthroplasty: a 10- to 14-year prospective follow-up review. J Arthroplasty 1999; 14 (4): 473-80.
- Faraj AA, Nevelos AB, Nair A. A 4- to 10-year follow-up study of the Tricon-M noncemented total knee replacement. Orthopedics 2001; 24 (12): 1151-4.
- Fetzer GB, Callaghan JF, Templeton JE, Goetz D, Sullivan PM, Kelly SS. Posterior cruciate-retaining modular total knee arthroplasty. A 9- to 12 year follow-up investigation. J Arthroplasty 2002; 17 (8): 961-6.
- Fiocco M, Putter H, Houwelingen JC. Meta-analysis of pairs of survival curves under heterogeneity: a Poisson correlated gamma frailty approach” Statistics in Medicine. Stat Med 2009; 28 (30): 3782-97.
- Fiocco M, Stijnen T, Putter H. Meta-analysis of time-to-event outcomes using a hazard-based approach: Comparison with other models, robustness and meta-regression. Computational Statistics and Data Analysis. 2011: doi:10.1016/j.csda.2011.05.009
- Forster MC, Kothari P, Howard PW. Minimum 5-year follow-up and radiologic analysis of the all-polyethylene tibial component of the Kinemax Plus system. J Arthroplasty 2002; 17 (2): 196-200.
- Gilbert RE, Carrothers AD, Gregory JJ, Oakley MJ. The St. Leger total knee replacement: a 10-year clinical and radiological assessment. Knee 2009; 16 (5): 322-5.
- Gill GS, Joshi AB. Long-term results of Kinematic Condylar knee replacement. An analysis of 404 knees. J Bone Joint Surg (Br) 2001; 83 (3): 355-8.
- Gioe TJ, Stroemer ES, Santos ER. All-polyethylene and metal-backed tibias have similar outcomes at 10 years: a randomized level I [corrected] evidence study. Clin Orthop 2006; (455): 12-8.
- Goldberg VM, Figgie MP, Figgie HE, III, Heiple KG, Sobel M. Use of a total condylar knee prosthesis for treatment of osteoarthritis and rheumatoid arthritis. Long-term results. J Bone Joint Surg (Am) 1988; 70 (6): 802-11.
- Goldberg VM, Kraay M. The outcome of the cementless tibial component. A minimum 14 year clinical evaluation. Clin Orthop 2004; (428): 214-20.
- Grewal R, Rimmer MG, Freeman MA. Early migration of prostheses related to long-term survivorship. Comparison of tibial components in knee replacement. J Bone Joint Surg (Br) 1992; 74 (2): 239-42.
- Hansson U, Ryd L, Toksvig-Larsen S. A randomised RSA study of Peri-Apatite HA coating of a total knee prosthesis. Knee 2008; 15 (3): 211-6.
- Hauptfleisch J, Glyn-Jones S, Beard DJ, Gill HS, Murray DW. The premature failure of the Charnley Elite-Plus stem: a confirmation of RSA predictions. J Bone Joint Surg (Br) 2006; 88 (2): 179-83.
- Henricson A, Dalen T, Nilsson KG. Mobile bearings do not improve fixation in cemented total knee arthroplasty. Clin Orthop 2006; (448): 114-21.
- Henricson A, Linder L, Nilsson KG. A trabecular metal tibial component in total knee replacement in patients younger than 60 years: A two-year radiostereophotogrammetric analysis. J Bone Joint Surg (Br) 2008; 90 (12): 1585-93.
- Hildebrand R, Trappmann D, Georg C, Muller HH, Koller M, Klose KJ, . What effect does the hydroxyapatite coating have in cementless knee arthroplasty? Orthopade 2003; 32 (4): 323-30.
- Hilding MB, Yuan X, Ryd L. The stability of three different cementless tibial components. A randomized radiostereometric study in 45 knee arthroplasty patients. Acta Orthop Scand 1995; 66 (1): 21-7.
- Hilding M, Aspenberg P. Postoperative clodronate decreases prosthetic migration: 4-year follow-up of a randomized radiostereometric study of 50 total knee patients. Acta Orthop 2006; 77 (6): 912-6.
- Hilding M, Aspenberg P. Local peroperative treatment with a bisphosphonate improves the fixation of total knee prostheses: a randomized, double-blind radiostereometric study of 50 patients. Acta Orthop 2007; 78 (6): 795-9.
- Hsu R WW, Tsai YH, Huang TJ, Chang J CC. Hybrid total knee arthroplasty: A 3- to 6-year outcome analysis. J Formos Med Assoc 1998; 97 (6): 410-5.
- Hyldahl H, Regner L, Carlsson L, Karrholm J, Weidenhielm L. All-polyethylene vs. metal-backed tibial component in total knee arthroplasty-a randomized RSA study comparing early fixation of horizontally and completely cemented tibial components: part 1. Horizontally cemented components: AP better fixated than MB. Acta Orthop 2005a; 76 (6): 769-77.
- Hyldahl H, Regner L, Carlsson L, Karrholm J, Weidenhielm L. All-polyethylene vs. metal-backed tibial component in total knee arthroplasty-a randomized RSA study comparing early fixation of horizontally and completely cemented tibial components: part 2. Completely cemented components: MB not superior to AP components. Acta Orthop 2005b; 76 (6): 778-84.
- Jacoby WG. The Dot Plot: A Graphical Display for Labeled Quantitative Values. The Political Methodologist 2006; 14 (1): 6-14.
- Karrholm J, Borssen B, Lowenhielm G, Snorrason F. Does early micromotion of femoral stem prostheses matter? 4-7-year stereoradiographic follow-up of 84 cemented prostheses. J Bone Joint Surg (Br) 1994; 76 (6): 912-7.
- Khaw FM, Kirk LM, Gregg PJ. Survival analysis of cemented Press-Fit Condylar total knee arthroplasty. J Arthroplasty 2001; 16 (2): 161-7.
- Khaw FM, Kirk LM, Morris RW, Gregg PJ. A randomised, controlled trial of cemented versus cementless press-fit condylar total knee replacement. J Bone Joint Surg (Br) 2002; 84: 658-66.
- Kienapfel H, Hildebrand R, Neumann T, Specht R, Koller M, Celik I, . The effect of Palamed G bone cement on early migration of tibial components in total knee arthroplasty. Inflamm Res (Suppl 2) 2004; 53: S159-S63.
- Kim YH, Yoon SH, Kim JS. The long-term results of simultaneous fixed-bearing and mobile-bearing total knee replacements performed in the same patient. J Bone Joint Surg (Br) 2007; 89 (10): 1317-23.
- Knight JL, Atwater RD, Grothaus L. Clinical results of the modular porous-coated anatomic (PCA) total knee arthroplasty with cement: a 5-year prospective study. Orthopedics 1997; 20 (11): 1025-33.
- Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg (Am) 2005; 87 (7): 1487-97.
- Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg (Am) 2007; 89 (4): 780-5.
- Lachiewicz PF, Soileau ES. Patella maltracking in posterior-stabilized total knee arthroplasty. Clin Orthop 2006; (452): 155-8.
- Laskin RS. Total condylar knee replacement in patients who have rheumatoid arthritis. A ten-year follow-up study. J Bone Joint Surg (Am) 1990; 72 (4): 529-35.
- Li MG, Nilsson KG. The effect of the preoperative bone quality on the fixation of the tibial component in total knee arthroplasty. J Arthroplasty 2000; (15): 744-53
- Malchau H. Introducing new technology: a stepwise algorithm. Spine (Phila Pa 1976) 2000; 25 (3): 285.
- Mayman D, Bourne RB, Rorabeck CH, Vaz M, Kramer J. Resurfacing versus not resurfacing the patella in total knee arthroplasty: 8- to 10-year results. J Arthroplasty 2003; 18 (5): 541-5.
- McCulloch P, Altman DG, Campbell WB, Flum DR, Glasziou P, Marshall JC, . No surgical innovation without evaluation: the IDEAL recommendations. Lancet 2009; 374 (9695): 1105-12.
- Mont MA, Yoon TR, Krackow KA, Hungerford DS. Eliminating patellofemoral complications in total knee arthroplasty: clinical and radiographic results of 121 consecutive cases using the Duracon system. J Arthroplasty 1999; 14 (4): 446-55.
- Moran CG, Pinder IM, Lees TA, Midwinter MJ. Survivorship analysis of the uncemented porous-coated anatomic knee replacement. J Bone Joint Surg (Am) 1991; 73 (6): 848-57.
- Muller SD, Deehan DJ, Holland JP, Outterside SE, Kirk LM, Gregg PJ, . Should we reconsider all-polyethylene tibial implants in total knee replacement? J Bone Joint Surg (Br) 2006; 88 (12): 1596-602.
- Nelissen RG, Valstar ER, Rozing PM. The effect of hydroxyapatite on the micromotion of total knee prostheses. A prospective, randomized, double-blind study. J Bone Joint Surg (Am) 1998; 80 (11): 1665-72.
- Nelissen RG, Pijls BG, Karrholm J, Malchau H, Nieuwenhuijse MJ, Valstar ER. RSA and registries: the quest for phased introduction of new implants. J Bone Joint Surg (Am) (Suppl 3) 2011; 93: 62-5.
- NHS National Institute for Clinical Excellence. Guidance on the selection of prostheses for primary total hip replacement. 2003;(http://www.nice.org.uk/nicemedia/pdf/Guidance_on_the_selection_of_hip_prostheses.pdf).
- Nielsen PT, Berg-Hansen E, Toksvig LS, Ryd L, Rechnagel K, Schroder HM, . AGC 2000 tibial components with hydroxyapatite coating - a randomized series followed 5 years with RSA. Acta Orthop Scand (Suppl 265) 1995; 66: 77.
- Nilsson KG, Karrholm J. Increased varus-valgus tilting of screw-fixated knee prostheses. Stereoradiographic study of uncemented versus cemented tibial components. J Arthroplasty 1993; 8 (5): 529-40.
- Nilsson KG, Dalen T. Inferior performance of Boneloc bone cement in total knee arthroplasty: a prospective randomized study comparing Boneloc with Palacos using radiostereometry (RSA) in 19 patients. Acta OrthopScand 1998; 69 (5): 479-83.
- Nilsson KG, Karrholm J, Ekelund L, Magnusson P. Evaluation of micromotion in cemented vs uncemented knee arthroplasty in osteoarthrosis and rheumatoid arthritis. Randomized study using roentgen stereophotogrammetric analysis. J Arthroplasty 1991; 6 (3): 265-78.
- Nilsson KG, Henricson A, Norgren B, Dalen T. Uncemented HA-coated implant is the optimum fixation for TKA in the young patient. Clin Orthop 2006; (448): 129-39.
- NJR. New Zealand National Joint Registry Annual Report 2009 (eleven year report) http://wwwcdhbgovtnz/NJR/. 2009:accessed 12-05-2011.
- Norgren B, Dalen T, Nilsson KG. All-poly tibial component better than metal-backed: a randomized RSA study. Knee 2004; 11 (3): 189-96.
- Norton MR, Vhadra RK, Timperley AJ. The Johnson-Elloy (Accord) total knee replacement. Poor results at 8 to 12 years. J Bone Joint Surg (Br) 2002; 84 (6): 852-5.
- Onsten I, Nordqvist A, Carlsson AS, Besjakov J, Shott S. Hydroxyapatite augmentation of the porous coating improves fixation of tibial components. A randomised RSA study in 116 patients. J Bone Joint Surg (Br) 1998; 80 (3): 417-25.
- Østgaard SE, Dirksen KL, Lund B. Hydroxyapatite coating in total knee arthroplasty - a randomised RSA study of tibial components. Acta Orthop (Suppl 289) 1999; 70: 4.
- Palumbo B, Henderson E, Edwards PK, Burris B, Gutierrez S, Ancha A, . Initial experience of the Journey-Deuce Bicompartimental Knee Prosthesis. Personal communication.
- Parsch D, Kruger M, Moser MT, Geiger F. Follow-up of 11-16 years after modular fixed-bearing TKA. Int Orthop 2008; 33 (2): 431-5.
- Pijls BG, Dekkers OM, Middeldorp S, Valstar ER, Van der Heide HJ, Van der Linden-Van der Zwaag HM, . AQUILA: Assessment of QUality In Lower limb Arthroplasty: An expert Delphi consensus for total knee and total hip arthroplasty. BMC Musculoskelet Disord 2011; 12 (1): 173.
- Putter H, Fiocco M, Stijnen T. Meta-analysis of diagnostic test accuracy studies with multiple thresholds using survival methods. Biom J 2009; 52 (1): 95-110.
- Ranawat CS, Flynn WF, Jr., Saddler S, Hansraj KK, Maynard MJ. Long-term results of the total condylar knee arthroplasty. A 15-year survivorship study. Clin Orthop 1993; (286): 94-102.
- Ranawat CS, Flynn WF, Deshmukh RG. Impact of modern technique on long-term results of total condylar knee arthroplasty. Clin Orthop 1994; (309): 131-5.
- Rinonapoli E, Mancini GB, Pucci G, Pazzaglia G, Aglietti P. Arthroplasty of the knee using total condylar prosthesis. Long term results (10 to 17 years) and survival analysis. Rev Chir Orthop Reparatrice Appar Mot 1994; 80 (3): 223-9.
- Ritter MA, Wing JT, Berend ME, Davis KE, Meding JB. The clinical effect of gender on outcome of total knee arthroplasty. J Arthroplasty 2008; 23 (3): 331-6.
- Robertsson O, Scott G, Freeman M AR. Ten-year survival of the cemented Freeman-Samuelson primary knee arthroplasty - Data from the Swedish Knee Arthroplasty Register and the Royal London Hospital. J Bone Joint Surg (Br) 2000; 8 (4): 506-7.
- Rodricks DJ, Patil S, Pulido P, Colwell CW, Jr. Press-fit condylar design total knee arthroplasty. Fourteen to seventeen-year follow-up. J Bone Joint Surg (Am) 2007; 89 (1): 89-95.
- Ryd L. Roentgen stereophotogrammetric analysis of prosthetic fixation in the hip and knee joint. Clin Orthop 1992; (276): 56-65.
- Ryd L, Albrektsson BE, Herberts P, Lindstrand A, Selvik G. Micromotion of noncemented Freeman-Samuelson knee prostheses in gonarthrosis. A roentgen-stereophotogrammetric analysis of eight successful cases. Clin Orthop 1988; (229): 205-12.
- Ryd L, Lindstrand A, Rosenquist R, Selvik G. Tibial component fixation in knee arthroplasty. Clin Orthop 1986; (213): 141-9.
- Ryd L, Lindstrand A, Rosenquist R, Selvik G. Micromotion of conventionally cemented all-polyethylene tibial components in total knee replacements. A roentgen stereophotogrammetric analysis of migration and inducible displacement. Arch Orthop Trauma Surg 1987; 106 (2): 82-8.
- Ryd L, Lindstrand A, Stenstrom A, Selvik G. Porous coated anatomic tricompartmental tibial components. The relationship between prosthetic position and micromotion. Clin Orthop 1990; (251): 189-97.
- Ryd L, Carlsson L, Herberts P. Micromotion of a noncemented tibial component with screw fixation. An in vivo roentgen stereophotogrammetric study of the Miller-Galante prosthesis. Clin Orthop 1993; (295): 218-25.
- Ryd L, Albrektsson BE, Carlsson L, Dansgard F, Herberts P, Lindstrand A, . Roentgen stereophotogrammetric analysis as a predictor of mechanical loosening of knee prostheses. J Bone Joint Surg (Br) 1995; 77 (3): 377-83.
- Samuelson K, Nelson L. An all-polyethylene cementless tibial component. A five- to nine-year follow-up study. Clin Orthop 1990; (260): 93-7.
- Santini AJ, Raut V. Ten-year survival analysis of the PFC total knee arthroplasty–a surgeon’s first 99 replacements. Int Orthop 2008; 32 (4): 459-65.
- Schemitsch EH, Bhandari M, Boden SD, Bourne RB, Bozic KJ, Jacobs JJ, . The evidence-based approach in bringing new orthopaedic devices to market. J Bone Joint Surg (Am) 2010; 92 (4): 1030-7.
- Schroder HM, Berthelsen A, Hassani G, Hansen EB, Solgaard S. Cementless porous-coated total knee arthroplasty. J Arthroplasty 2001; 16 (5): 559-67.
- Scott RD. The incidence and causes of re-operation after press-fit condylar (PFC) total knee arthroplasty. J Orthop Science 1997; 2: 46-52.
- Selvik G. Roentgen stereophotogrammetry. A method for the study of the kinematics of the skeletal system. Acta Orthop Scand (Suppl 232) 1989: 1-51.
- Sextro GS, Berry DJ, Rand JA. Total knee arthroplasty using cruciate-retaining kinematic condylar prosthesis. Clin Orthop 2001; (388): 33-40.
- Sheth U, Nguyen NA, Gaines S, Bhandari M, Mehlman CT, Klein G. New orthopedic devices and the FDA. J Long Term Eff Med Implants 2009; 19 (3): 173-84.
- SKAR. Swedish Knee Arthroplasty Registry Report 2010 V1.0. http://wwwkneenkose/english/online/thePages/contactphp. 2010:accessed 12-05-2011.
- Smith AJ, Wood DJ, Li MG. Total knee replacement with and without patellar resurfacing: a prospective, randomised trial using the profix total knee system. J Bone Joint Surg (Br) 2008; 90: 43-9.
- Stukenborg-Colsman C, Wirth CJ. Knee endoprosthesis: clinical aspects. Orthopade 2000; 29 (8): 732-8.
- Therbo M, Lund B, Jensen KE, Schroder HM. Effect of bioactive coating of the tibial component on migration pattern in uncemented total knee arthroplasty: A randomized RSA study of 14 knees presented according to new RSA-guidelines. J Orthop Trauma 2008; 2: 63-7.
- Toksvig-Larsen S, Jorn LP, Ryd L, Lindstrand A. Hydroxyapatite-enhanced tibial prosthetic fixation. Clin Orthop 2000; (370): 192-200.
- Toksvig-Larsen S, Ryd L, Lindstrand A. Early inducible displacement of tibial components in total knee prostheses inserted with and without cement: a randomized study with roentgen stereophotogrammetric analysis. J Bone Joint Surg (Am) 1998; 80 (1): 83-9.
- Uvehammer J, Karrholm J, Carlsson L. Influence of joint area design on tibial component migration: comparison among a fixed symmetrical, asymmetrical, and moveable bearing. J Knee Surg 2007; 20 (1): 20-6.
- Uvehammer J, Regner L, Karrholm J. Flat vs. concave tibial joint surface in total knee arthroplasty: randomized evaluation of 39 cases using radiostereometry. Acta Orthop Scand 2001; 72 (3): 257-65.
- Valstar ER, Gill R, Ryd L, Flivik G, Borlin N, Karrholm J. Guidelines for standardization of radiostereometry (RSA) of implants. Acta Orthop 2005; 76 (4): 563-72.
- van der Linde MJ, Garling EH, Valstar ER, Tonino AJ, Nelissen RG. Periapatite may not improve micromotion of knee prostheses in rheumatoid arthritis. Clin Orthop 2006a; (448): 122-8.
- Van der Linde MJ, Grimm B, Garling EH, Valstar ER, Tonino AJ, Heyligers IC. Comparative study of the migration of the tibial tray in total knee arthroplasty for cemented, uncoated and periapatite coated components using roentgenstereogrammetric analysis (RSA). J Bone Joint Surg (Br) (Suppl I) 2006b; 88: 96-7.
- Vessely MB, Whaley AL, Harmsen WS, Schleck CD, Berry DJ. The Chitranjan Ranawat Award - Long-term survivorship and failure modes of 1000 cemented condylar total knee arthroplasties. Clin Orthop 2006; (452): 28-34.
- Vochteloo AJ, Pijls BG, van der Heide HJ. Sutures v staples. Let’s add three other studies. Bmj 2010; 340: c2627.
- von Schewelov T, Besjakov J, Sanzen L, Carlsson A. A clinical and radiostereometric study of the cemented PFC-sigma prosthesis: a 5-year study of 29 cases with a fixed bearing. J Knee Surg 2008; 22 (3): 231-6.
- Weir DJ, Moran CG, Pinder IM. Kinematic condylar total knee arthroplasty. 14-year survivorship analysis of 208 consecutive cases. J Bone Joint Surg (Br) 1996; 78 (6): 907-11.
- Wilson D, Dunbar MJ. A prospective randomized controlled trial using roentgen stereophotogrammetric analysis of a trabecular metal tibial monoblock knee arthroplasty component - 2 year results. J Biomech 2007; 40 (S2): S182.
- Worland RL, Johnson GV, Alemparte J, Jessup DE, Keenan J, Norambuena N. Ten to fourteen year survival and functional analysis of the AGC total knee replacement system. Knee 2002; 9 (2): 133-7.
- Wright J, Ewald FC, Walker PS, Thomas WH, Poss R, Sledge CB. Total knee arthroplasty with the kinematic prosthesis. Results after five to nine years: a follow-up note. J Bone Joint Surg (Am) 1990; 72 (7): 1003-9.
- Zaki SH, Rafiq I, Kapoor A, Raut V, Gambhir AK, Porter ML. Medium term results with the Press Fit Condylar (PFC) sigma knee prosthesis the wrightington experience. Acta Orthop Belgica 2007; 73 (1): 55-9.
Data sharing
The statistical code and dataset are available upon request from the corresponding author at [email protected]. R code for the analysis described in the Appendix is available from one of the authors ([email protected]).Supplementary data