Abstract
Background and purpose High age is associated with increased postoperative mortality, but the factors that predict mortality in older hip and knee replacement recipients are not known.
Methods Preoperative clinical and operative data on 1,998 primary total hip and knee replacements performed for osteoarthritis in patients aged ≥ 75 years in a single institution were collected from a joint replacement database and compoared with mortality data. Average follow-up was 4.2 (2.2–7.6) years for the patients who survived. Factors associated with mortality were analyzed using Cox regression analysis, with adjustment for age, sex, operated joint, laterality, and anesthesiological risk score.
Results Mortality was 0.15% at 30 days, 0.35% at 90 days, 1.60% at 1 year, 7.6% at 3 years, and 16% at 5 years, and was similar following hip and knee replacement. Higher age, male sex, American Society of Anesthesiologists risk score of > 2, use of walking aids, preoperative walking restriction (inability to walk or ability to walk indoors only, compared to ability to walk > 1 km), poor clinical condition preoperatively (based on clinical hip and knee scores or clinical severity of osteoarthritis), preoperative anemia, severe renal insufficiency, and use of blood transfusions were associated with higher mortality. High body mass index had a protective effect in patients after hip replacement.
Interpretation Postoperative mortality is low in healthy old joint replacement recipients. Comorbidities and functional limitations preoperatively are associated with higher mortality and warrant careful consideration before proceeding with joint replacement surgery.
Ability to walk is critical for maintaining independence in daily activities. Difficulties in walking and impaired function are also strong predictors of mortality in the elderly (Keeler et al. Citation2010, Hardy et al. Citation2011). Arthritis is one of most frequent reasons for disability in older age (Spiers et al. Citation2005, Song et al. Citation2006), and recently, osteoarthritis has been associated with higher mortality in the general population (Nüesch et al. Citation2011).
Joint replacement is an effective treatment in late-stage arthritis of the hip and knee and leads to improvement in function, pain, performance in activities of daily living, and quality of life in the oldest patients (Brander et al. Citation1997, Jones et al. Citation2001, Ethgen et al. Citation2004, Hamel et al. Citation2008). The demand for joint replacement surgery is increasing (Birrell et al. Citation1999, Robertsson et al. Citation2000). On the other hand, joint replacements are associated with higher mortality than in the general population (Lie et al. Citation2010), particularly in patients over 75 years of age (Hosick et al. Citation1994, Gill et al. Citation2003, Aynardi et al. Citation2009, Lie et al. Citation2010, Pedersen et al. Citation2011). Thus, in the elderly the benefits of joint replacement must be weighted against the higher risk of postoperative complications (SooHoo et al. Citation2006, Parvizi et al. Citation2007, Memtsoudis et al. Citation2010, SooHoo et al. Citation2010) including death, and limited life expectancy.
Although the demand for joint replacements can be expected to increase considerably in the near future as the average age of the population increases, there has been limited research on the outcomes of hip and knee replacements in the elderly. Furthermore, the results obtained in younger patients cannot be extrapolated to older patients due to specific characteristics of these patients, such as neurodegenerative diseases, frailty, and reduced functional reserve and ability to recover.
We analyzed mortality and predictors of mortality following primary hip and knee replacement in patients aged ≥ 75 years in a large population-based sample. We hypothesized that comorbidities and physical condition preoperatively rather than chronological age in itself would be predictive of patient survival after primary joint replacement.
Materials and methods
From September 1, 2002 through January 31, 2009, 2,559 primary hip and knee replacements were performed at our institution in patients aged 75 years or more at the time of surgery.
We included only the first operations for each patient during the observation period (simultaneous replacement of both hips or knees were, however, included and are referred to as bilateral operations), leading to exclusion of 306 subsequent primary joint replacements. We also excluded operations performed for reasons other than primary osteoarthritis (acute hip fracture or revision of failed osteosynthesis, n = 74; inflammatory arthritis, n = 70; secondary OA, n = 23; osteonecrosis, n = 19; bone tumor or metastasis, n = 10; or other miscellaneous diagnoses, n = 6), unicondylar knee replacement (n = 47), and resurfacing hip replacement (n = 6). Thus, the present series consisted of 756 primary total hip replacements and 1,242 primary total knee replacements performed for primary osteoarthritis (OA). Altogether, patients aged ≥ 75 years accounted for 31–41% of all primary joint replacements performed annually at our institution, for primary OA. There were no statistically significant differences between the observation years.
Our institution is responsible for publicly-funded joint replacement surgery in the local hospital district (with about 470,000 inhabitants). Most patients are referred for surgery by general practitioners and private specialists. Referrals are based on uniform national criteria for access to non-emergency treatment, introduced in 2005, and local clinical pathways for treatment of hip and knee osteoarthritis. According to these criteria, referral is considered appropriate when the total score exceeds a specific cutoff value, corresponding to the presence of continuous pain and/or severe disability in usual activities together with radiographic confirmation of joint destruction.
Pre- and perioperative data, including Knee Society score (KSS; Insall et al. Citation1989) and Harris hip score (HHS; Harris Citation1969), were recorded prospectively in a specific joint replacement database by an orthopedic surgeon or a physiotherapist. This database (Tekoset; Advanced Medical Vision, Tampere, Finland) was developed in the early 2000s, and has been used in our unit since the hospital was founded in September 2002. Hospitalization data and supplementary perioperative information were collected from the hospital administration database (which is shared with the adjacent university hospital). Operation-related data (anesthesiological risk score, duration of surgery, blood loss, and use of blood products) were recorded in the operating room, and hospitalization data were recorded upon discharge. The hospitalization data were also reported to the Finnish Hospital Discharge Register.
Eventual revision surgeries and later primary operations were identified from the joint replacement database. Data on preoperative laboratory routines were collected from the databases of the adjacent university hospital laboratory. 387 patients (19%) had preoperative hemoglobin values missing and 892 patients (45%) had preoperative creatinine values missing, because laboratory tests were done in outside laboratories. These patients were omitted from respective analyses. Date of death was retrieved from the hospital administration database, which is linked to national census data. Data from different sources could be combined using the unique personal identification number of each Finnish resident and the date of surgery as matching criteria.
Statistics
All data were analyzed using patients (i.e. joint replacement operations) as the statistical unit. The patients were followed until March 31, 2010 unless death occurred before that. Patients who underwent subsequent joint replacements after the one being followed-up were censored at the time of that operation. The minimum follow-up for surviving patients was 26 months.
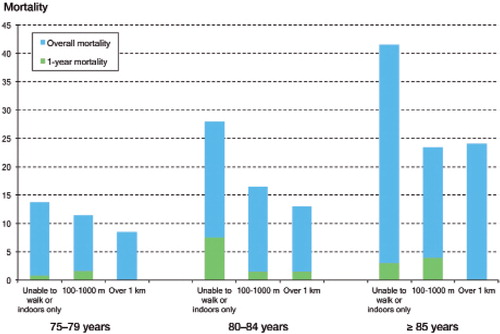
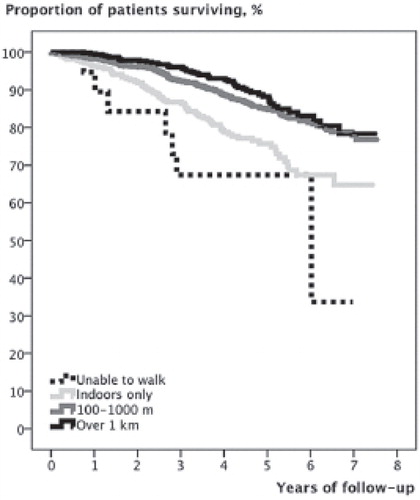
The main outcome was overall mortality. Postoperative mortality was analyzed at 7, 30, and 90 days and at 1 year, but due to the low number of deaths, predictors of mortality at these time points could not be analyzed. Mortality at 1, 3, and 5 years was estimated using Kaplan-Meier survival analysis, which was also used to produce the survival curves presented in and . All mortality data are presented as case numbers and percentages.
Figure 1. Kaplan-Meier survival curves with death as endpoint for patients aged 75–79 years, 80–84 years, and ≥ 85 years at the time of primary hip or knee replacement.
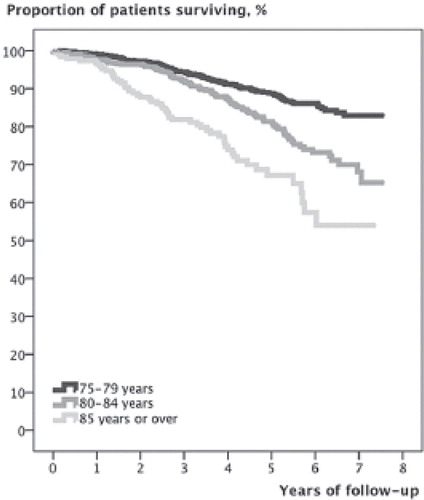
Figure 2. Kaplan-Meier survival curves with death as endpoint following primary hip or knee replacement, with respect to preoperative walking ability.
Mortality and its predictors were calculated for the whole series, to achieve maximal statistical power. Even so, the results of subgroup analyses for patients aged 75–79 years, 80–84 years, and ≥ 85 years, and for hip and knee replacements, are reported when they provide information that differs from the results of the main analyses.
The associations of the available patient-related, clinical, and operative variables with overall patient survival were analyzed by Cox regression analysis. Age, body mass index (BMI), duration of operation, blood loss, and renal function were analyzed as continuous variables and also categorized as follows. Age was analyzed in groups of 75–79 years, 80–84 years, and ≥ 85 years. BMI was categorized into 4 groups: underweight (< 20 kg/m2), normal (20–24 kg/m2), overweight (25–29 kg/m2), and obese (≥ 30 kg/m2). For duration of operation and blood loss, quartiles were used as cutoff points. Renal function was categorized based on estimated glomerular filtration rate (GFR), calculated using the Cockcroft and Gault formula (Cockcroft and Gault Citation1976), as normal (≥ 90 mL/min) or as mild (60–89 mL/min), moderate (30–59 mL/min), or severe (< 30 mL/min) renal insufficiency. Patients with hemoglobin below the normal range of the local reference values (134–167 g/L for men and 117–155 g/L for women) were considered to have anemia.
Walking distance and use of walking aids were analyzed separately from KSS and HHS because mobility level is an important predictor of mortality in the general population (Keeler et al. Citation2010, Nüesch et al. Citation2011). As a modification of the original block-based categorization of walking ability, walking distance both for HHS and KSS was recorded in our joint replacement database as follows: unable to walk/bed or chair only, indoors only/housebound, 100–500 m, 500–1,000 m, 1-1.5 km, over 1.5 km/unlimited. For the present analyses, the 100–500 m and 500–1,000 m groups were combined (100–1,000 m) and the groups 1–1.5 km and over 1.5 km/unlimited were combined (over 1 km).
In addition, KSS and HHS were used to create a composite marker “severe OA”, defined as (1) the presence of axial deformity of > 10 degrees, severe anteroposterior or mediolateral instability, range of motion of < 80 degrees before knee replacement; or (2) the presence of severe limp, total range of motion of < 100 degrees, or positive Trendelenburg sign (recorded routinely in the joint replacement database in addition to the components of HHS) before hip replacement. The criteria for this composite marker are based on the clinical experience of two joint replacement surgeons (TP and AE) and they were used in this study as an objective marker of severity of OA because radiographic data were lacking.
The comparisons were first performed without adjustment (univariate analysis) and then with adjustment for age, sex, American Society of Anesthesiologists (ASA) risk score, operated joint, and laterality (unilateral, bilateral). No significant violations of the proportional hazards assumption were observed in visual assessment of log-minus-log curves in the Cox regression analyses. Finally, variables that were associated with overall mortality in adjusted analyses were included in the same multivariate model to analyze their independent effects. As sensitivity analysis, the adjusted models were also re-run after exclusion (one at at time) of (1) prostheses with cementless or hybrid fixation, (2) patients who had undergone subsequent primary hip or knee replacement or revision surgery, (3) bilateral operations.
The results of the regression analyses are presented as hazard ratios (HRs) with 95% confidence intervals (CIs) (corresponding to statistical significance at the p < 0.05 level).
Results
Patients and operative data
Patient demographics, preoperative data, and operative data are given in . Knee replacement recipients were more likely to have both sides involved, but they used walking aids less frequently and had less restriction of mobility.
Table 1. Patient demographics and preoperative clinical situation in primary hip and knee replacements
In the majority of cases, a cemented total joint replacement was performed. Of the total knee replacements, 399 (32%) were cruciate-retaining, 766 (62%) were cruciate-substituting, 58 (5%) were constrained condylar, and 19 (1%) were hinged (or tumor prosthesis) designs. The patella was resurfaced in 530 knees (42%).
Most patients (93%) arrived at hospital on the day of operation. 1,987 operations (99%) were performed under spinal anesthesia. Intravenous antibiotic prophylaxis (3 g of cefuroxime as a single bolus unless contraindicated) was given before the operation in all cases. Low-molecular-weight heparin for 4 weeks was used as thromboprophylaxis in 1,875 cases (94%). Most patients (64%) were discharged to other healthcare units for rehabilitation, and the rest were discharged directly home. 347 patients (17.4% and 17.3% of hip and knee replacement recipients) underwent another joint replacement during the observation period. 20 hip replacements (2.6%) and 24 knee replacements (1.9%) were later revised.
Postoperative mortality and overall patient survival
278 patients (14%) died during their follow-up (median 4.2 (0–7.6) years). For surviving patients, median follow-up was 4.4 (2.2–7.6) years. Mortality was 0.10% (n = 2) at 7 days, 0.15% (n = 3) at 30 days, 0.35% (n = 7) at 90 days, and 1.60% (n = 32) at 1 year.
Mortality at 1, 3, and 5 years after surgery was 1.6% (CI: 1.0–2.2), 7.6% (CI: 6.4–8.8), and 16% (CI: 13.7–17.7), respectively, and there was no difference between hip and knee replacements (adjusted HR = 1.0, CI: 0.8-1.3, for hip replacements compared to knee replacements).
Mortality rates at 1, 3, and 5 years for different patient subgroups and adjusted HRs for overall mortality are given in . The results of respective univariate analyses are given in the Appendix (see Supplementary data).
Table 2. Mortality at 1, 3, and 5 years following primary hip or knee replacement, and the factors associated with mortality. The results concerning factors predicting mortality are presented as hazard ratios (HRs) and their 95% confidence intervals (CIs), calculated using Cox regression analysis, with adjustment for age, sex, ASA risk score, joint (hip, knee), and laterality (unilateral, bilateral)
Patient characteristics
During the first postoperative year, mortality was higher in the age groups 80–84 years (2.3%, adjusted HR = 2.4, CI: 1.1–5.3) and ≥ 85 years (3.2%, adjusted HR = 3.2, CI: 1.2–8.8) than in patients aged 75–79 years (0.9%) but in general, 1-year mortality was low (). The differences between the age groups persisted as the follow-up progressed. Men had higher mortality than women ().
Lowest 1-year mortality was observed in overweight patients and lowest overall mortality was observed in obese patients, and altogether high BMI showed a protective effect against mortality, even after adjustment (). This effect was particularly apparent in hip replacements (adjusted HR per increase of 1 kg/m2 = 0.91, CI: 0.86–0.96) whereas following knee replacement BMI had no effect on mortality (adjusted HR per increase of 1 kg/m2 = 0.99, CI: 0.96–1.03).
ASA risk score was strongly associated with overall mortality (), whereas there was no statistically significant effect on 1-year mortality (data not shown). Preoperative anemia (see below) and severe renal insufficiency were associated with higher mortality, independent of ASA score ().
Preoperative clinical state
Preoperative functional limitations () and poorer preoperative clinical state, approximated with HHS and KSS, and “severe OA” were associated with higher mortality (). The association between walking distance and mortality was essentially similar for hip and knee replacements (data not shown) and in the 3 age groups (). After adjustment, a statistically significant association with mortality was only observed for the category “inability to walk/indoors only” (combined due to small case numbers) compared to “over 1 km” in the age groups 80–84 years and ≥ 85 years (adjusted HR = 2.1, CI: 1.1–3.8, and adjusted HR = 2.5, CI: 1.1–6.0, respectively).
Surgery-related factors
Except for blood transfusions, none of the operation-related variables tested had any effect on mortality in the adjusted analyses ().
Anemia, blood loss, and use of blood transfusions
Patients with anemia and those who received blood transfusions had increased mortality whereas blood loss did not affect mortality in the adjusted analyses (). Preoperatively, anemic patients both with and without blood transfusion had higher overall mortality (adjusted HR = 1.7, CI: 1.2–2.7, and adjusted HR = 1.5, CI: 0.98–2.2) than patients with normal hemoglobin and not receiving blood products. When patients were stratified according to the amount of blood loss, blood transfusions were not associated with mortality in the adjusted analyses (data not shown). In the absence of blood transfusion, blood loss did not affect mortality. Exclusion of patients with anemia did not change these results.
Sensitivity analyses
The key findings remained essentially unchanged in the previously defined subgroup analyses that were performed as sensitivity analyses.
Discussion
The major strength of our study is the large, regionally representative sample with detailed prospectively and systematically collected clinical data, which allowed more comprehensive analysis and control over numerous confounding factors than the health registers used in most previous studies. Inevitably, postoperative mortality increases with age, but the present study shows that alone, its predictive power is poor. Male sex, comorbidities, anemia, severity of arthritis, and particularly functional limitations preoperatively were predictive of increased mortality following primary hip and knee replacement, independently of age, whereas the operation-related variables analyzed had little or no effect on long-term prognosis.
In general, early postoperative mortality was low. The mortality of 0.18% at 30 days and 0.51% at 90 days is comparable or only slightly higher than has been reported in earlier series (Parvizi et al. Citation2001a, Citationb, SooHoo et al. Citation2006, Aynardi et al. Citation2009, Lie et al. Citation2010, SooHoo et al. Citation2010), although we included only patients over 75 years of age. In patients aged ≥ 80–85 years, reported in-hospital and 90-day mortality rates range from 1% to 4.7% (Gill et al. Citation2003, Kreder et al. Citation2005, Pedersen et al. Citation2011). The materials in these studies were from much earlier series (Gill et al. Citation2003, Kreder et al. Citation2005) or were collected from several different institutions (Kreder et al. Citation2005, Pedersen et al. Citation2011) whereas our series was operated on in a high-volume tertiary-care center concentrating solely on joint replacement. Lower postoperative mortality has been reported in specialty hospitals than in general hospitals (Cram et al. Citation2007), and in association with higher procedure volume (Shervin et al. Citation2007). Moreover, almost all the patients in this study received effective thromboprophylaxis and were operated on under spinal anesthesia.
In the longer term, the decline in patient survival ( and ) most likely represents the natural process of aging, as the excess mortality related to the surgery lasts only a month (Lie et al. Citation2010, Pedersen et al. Citation2011). The 5-year mortality exceeded one fifth in certain patient subgroups (e.g. in those who were housebound before surgery), but on the other hand, it was only below 10% in patients who were healthy and physically fit before surgery. In Finland, life expectancy at the age of 80 is 8.5 years for women and 7.0 years for men (Official Statistics of Finland 2003), and in general, the survival of joint replacement recipients is better than that of general population (Robertsson et al. Citation2007, Pedersen et al. Citation2011). Thus, thoughts about compromised life expectancy should not prevent performance of hip or knee replacement in older patients if a satisfactory outcome can otherwise be expected.
As expected in the light of previous literature (SooHoo et al. Citation2006, Gaston et al. Citation2007, Lie et al. Citation2010, Memtsoudis et al. Citation2010, Pedersen et al. Citation2011), male sex and comorbidity were predictive of mortality—particularly in long-term follow-up. Unfortunately, the effects of different conditions on mortality could not be analyzed because no data on specific comorbid conditions or medication were registered in our data sources and such data could not be gathered retrospectively because of the size of the material. Considering comorbidity would have been important, because in the presence of comorbidity the criteria for performing joint replacement are probably stricter and thus surgery may be delayed in order to gain greater improvement to compensate the increased risks. It has, however, been reported that the patients with the worst preoperative clinical state do not reach as good an outcome as those who are operated earlier in the course of OA (Lingard et al. Citation2004). Furthermore, our results strongly suggest that poor preoperative clinical state is associated with increased mortality, although it remains unclear to what extent this is attributable to comorbidities or to the degree of OA.
In-hospital mortality after hip and knee replacement has been linked to dementia, renal disease, cerebrovascular disease, and diabetes (Memtsoudis et al. Citation2010). Accordingly, patients with severe renal insufficiency appeared as one of the subgroups with the highest mortality in our study. History of coronary heart disease, but not hypertension or obesity, has been associated with higher mortality (Gaston et al. Citation2007), but in another study hip replacement recipients had lower mortality than age- and sex-matched population-based controls—even in the presence of cardiovascular disease, diabetes, or cancer (Pedersen et al. Citation2011).
Supporting earlier observations in the general population (Keeler et al. Citation2010, Hardy et al. Citation2011), in patients with osteoarthritis (Nüesch et al. Citation2011) and in hip fracture patients (Pioli et al. Citation2006, Paksima et al. Citation2008), impaired functional status, and—specifically—mobility disability appeared to be a strong independent predictor of postoperative mortality, both during the first postoperative year and in long-term follow-up. We acknowledge that patients who were housebound or unable to walk at all were a minority in this study, but even so their prognosis appeared to be particularly poor, and the differences compared to patients with a greater level of mobility persisted after multiple adjustments, which underscores the importance of this observation.
Although arthritis is a clear reason for walking difficulties preoperatively in hip and knee replacement patients, it should be kept in mind that in the aged, mobility disability may also relate to comorbid diseases and to conditions such as anemia (Lipschitz Citation2003), malnutrition (Timpini et al. Citation2011), vitamin D deficiency (Nawabi et al. Citation2010), cognitive decline and depression (Qiu et al. Citation2010), or frailty in the absence of specific, previously diagnosed diseases (Landi et al. Citation2010). Obviously, such conditions impair patient survival, but they may also adversely affect recovery and clinical outcome (Bischoff-Ferrari et al. Citation2004, Nawabi et al. Citation2010). Higher BMI was found to have a protective effect in our study—as has also been reported in the general population (Heiat et al. Citation2001) and, for example, in cardiothoracic surgery (Thourani et al. Citation2011). So, in some instances higher BMI could be considered a mark of well-being in older individuals—at least as far as it is not associated with increased comorbidity.
Preoperative anemia is common in older hip and knee replacement recipients, and it can predict the need for blood transfusions, occurrence of postoperative complications, and short-term mortality (Wu et al. Citation2007, Spahn Citation2010). Our study confirmed that anemia also increases mortality with longer follow-up, as it does in the general geriatric population (Lipschitz Citation2003). Given the adverse consequences of anemia, identification of its causes (such as renal insufficiency, malignancies, and the geriatric conditions mentioned above) and initiation of appropriate treatment preoperatively is advised in order to prevent its progression—and to improve patients’ prognosis (Lipschitz Citation2003).
Perioperative blood transfusions are associated with an increased risk of postoperative complications and short-term mortality in non-cardiac surgery (Glance et al. Citation2011), including total hip replacement (Pedersen et al. Citation2009). In the present study, blood transfusion did not increase mortality in anemic patients, which is in accordance with the results of a previous large study of hip fracture patients (Carson et al. Citation1998). In the absence of anemia, instead, blood transfusions appeared to increase mortality. Accordingly, Pedersen et al. (Citation2009) reported a higher risk of adverse postoperative outcome in patients with postoperative hemoglobin levels > 105 g/L who received blood transfusion than in those who did not receive allogenous blood. The authors suggested that this could be related to perioperative factors (e.g. blood loss) that could not be identified in their registry-based study. Another explanation might be that the patients who received blood transfusions had comorbidities that increased the need for blood transfusion and impaired patient survival but that could not be taken into account in the present study. This could explain why mortality first started to decline in longer-term follow-up.
Our study had certain limitations. Firstly, although it consisted of a population-based sample, the results cannot be generalized to all patients suffering from late-stage arthritis in this age group. This is because it is likely that patients with poorer physical condition and more comorbidity are referred for surgery less often, which introduces healthy-patient bias. Moreover, in our area, patients aged ≥ 80 years have more severe OA and poorer overall clinical state at the time of primary knee replacement than patients aged 75–79 years (Jämsen et al. in press), suggesting that the threshold for referring for and performing surgery is higher in the oldest age group. Furthermore, the mortality rates obtained in a single specialized unit cannot be generalized to other settings where somewhat higher mortality rates could be expected (Cram et al. Citation2007, Shervin et al. Citation2007).
Secondly, we had to rely on ASA score as a measure of comorbidity because data on the type and severity of comorbid conditions were not available. At the group level, ASA score can be used for adjustments in statistical analyses but at the level of an individual patient, it has little value, because the effects of different conditions on mortality and risk of complications may vary even though they might give the same ASA score. The effects of depression, dementia, malnutrition, and frailty on the outcomes of joint replacement are of interest in future research, because in the aged, they may contribute to arthritis-related disability and also impair clinical outcomes and patient survival.
A related issue that could not be resolved is the role of postoperative complications. Both age and comorbidity increase the risk of postoperative complications, which—again—have been cited as strong predictors of in-hospital mortality (Memtsoudis et al. Citation2010) and could partly explain the excess mortality observed with longer follow-up.
Finally, data on clinical state preoperatively were missing for a number of patients, partly because it was not (for one reason or another) recorded in daily clinical practice. Moreover, laboratory data were available only for those patients who used the services of the local university hospital. Because of these missing data, we could not run multivariate analyses to test which factors were independent predictors of mortality. Otherwise, the data can be considered to be reliable because of the prospective and systematic registration. Importantly, there is no reason to believe that missing data would have led to systematic bias in our results, but instead, it would more likely have led to false negative results.
Our results indicate that hip and knee replacement can be considered safe, regarding postoperative mortality, in selected older patients. Some of the factors associated with mortality are potentially modifiable. In particular, factors that may underlie poor mobility in an older patient with arthritis should be worked out carefully before joint replacement. Otherwise, the factors associated with poor prognosis should be acknowledged before surgery and weighed against the expected benefits of joint replacement. When indicated, joint replacement should be performed without unnecessary delay to avoid worsening of patient’s clinical condition.
Supplementary data.
Appendix is available at our website (www.actaorthop.org), identification number 5608.
Supplementary Material
Download PDF (41.1 KB)EJ collected and analyzed the materials, wrote the first draft of the manuscript, and took care of revisions. TP, AR, PJ, JK, JN, and JV contributed to interpretation of the results and preparation of the manuscript.
The authors are grateful for the financial support given to one of the authors (EJ) by the Competitive Research Funds of Tampere University Hospital, Tampere, Finland (grant 9L031) and the Pirkanmaa Regional Fund of the Finnish Cultural Foundation.
No competing interests declared.
- Aynardi M, Pulido L, Parvizi J, Sharkey PF, Rothman RH. Early mortality after modern total hip arthroplasty. Clin Orthop 2009; (467) (1): 213-8.
- Birrell F, Johnell O, Silman A. Projecting the need for hip replacement over the next three decades: influence of changing demography and threshold for surgery. Ann Rheum Dis 1999; 58 (9): 569-72.
- Bischoff-Ferrari HA, Lingard EA, Losina E, Baron JA, Roos EM, Phillips CB, Mahomed NN, Barrett J, Katz JN. Psychosocial and geriatric correlates of functional status after total hip replacement. Arthritis Rheum 2004; 51 (5): 829-35.
- Brander VA, Malhotra S, Jet J, Heinemann AW, Stulberg SD. Outcome of hip and knee arthroplasty in persons aged 80 years and older. Clin Orthop 1997; (345): 67-78.
- Carson JL, Duff A, Berlin JA, Lawrence VA, Poses RM, Huber EC, O’Hara DA, Noveck H, Sotrm BL. Perioperative blood transfusion and postoperative mortality. JAMA 1998; 279 (3): 199-205.
- Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron 1976; 16 (1): 31-41.
- Cram P, Vaughan-Sarrazin MS, Wolf B, Katz JN, Rosenthal GE. A comparison of total hip and knee replacement in specialty and general hospitals. J Bone Joint Surg (Am) 2007; 89 (8): 1675-84.
- Ethgen O, Bruyère O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg (Am) 2004; 86 (5): 963-74.
- Gaston MS, Amin AK, Clayton RA, Brenkel IJ. Does a history of cardiac disease or hypertension increase mortality following primary elective total hip arthroplasty? Surgeon 2007; 5 (5): 260-5.
- Gill GS, Mills D, Joshi AB. Mortality following primary total knee arthroplasty. J Bone Joint Surg (Am) 2003; 85 (3): 432-5.
- Glance LG, Dick AW, Mukamel DB, Fleming FJ, Zollo RA, Wissler R, Salloum R, Meredith UW, Osler TM. Association between intraoperative blood transfusion and mortality and morbidity in patients undergoing non-cardiac surgery. Anesthesiology 2011; 114 (2): 283-92.
- Hamel MB, Toth M, Legedza A, Rosen MP. Joint replacement surgery in elderly patients with severe osteoarthritis of the hip or knee. Decision making, postoperative recovery, and clinical outcomes. Arch Intern Med 2008; 168 (13): 1430-40.
- Hardy SE, Kang Y, Studenski SA, Degenholtz HB. Ability to walk ¼ mile predicts subsequent disability, mortality and health care costs. J Gen Intern Med 2011; 26 (2): 130-5.
- Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg (Am) 1969; 51 (4): 737-55.
- Heiat A, Vaccarino V, Krumholz HM. An evidence-based assessment of federal guidelines for overweight and obesity as they apply to elderly persons. Arch Intern Med. 2001; 161 (9): 1194-203.
- Hosick WB, Lotke PA, Baldwin A. Total knee arthroplasty in patients 80 years of age and older. Clin Orthop 1994; (299): 77-80.
- Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop 1989; (248): 13-4.
- Jones CA, Voaklander DC, Johnston DW, Suarez-Almazor ME. The effect of age on pain, function, and quality of life after total hip and knee arthroplasty. Arch Intern Med 2001; 161 (3): 454-60.
- Jämsen E, Jäntti P, Puolakka T, Eskelinen A. Primary knee replacement for primary osteoarthritis in the aged: gender differences in epidemiology and preoperative clinical state. Aging Clin Exp Res 2012. [Epub ahead of print] PubMed PMID: 22968368.
- Keeler E, Guralnik JM, Tian H, Wallace RB, Reuben DB. The impact of functional status on life expectancy in older persons. J Gerontol A Biol Sci Med Sci 2010; 65 (7): 727-33.
- Kreder HJ, Berry GK, McMurtry IA, Halman SI. Arthroplasty in the octogenarian: quantifying the risks. J Arthroplasty 2005; 20 (3): 289-93.
- Landi F, Abbatecola AM, Provinciali M, Corsonello A, Bustacchini S, Manigrasso L, Cherubini A, Bernabei R, Lattanzio F. Moving against frailty: does physical activity matter? Biogerontology 2010; 11 (5): 537-45.
- Lie SA, Pratt N, Ryan P, Engesaeter LB, Havelin LI, Furnes O, Graves S. Duration of increase in early postoperative mortality after elective hip and knee replacement. J Bone Joint Surg (Am) 2010; 92 (1): 619-28.
- Lingard EA, Katz JN, Wright EA, Sledge CB, The Kinemax Outcomes Group. Predicting the outcome of total knee arthroplasty. J Bone Joint Surg (Am) 2004; 86: 2179-86.
- Lipschitz D. Medical and functional consequences of anemia in the elderly. J Am Ger Soc (Suppl 1) 2003; 51: S10-3.
- Memtsoudis SG, Della Valle AG, Besculides MC, Esposito M, Koulouvaris P, Salvati EA. Risk factors for perioperative mortality after lower extremity arthroplasty: a population-based study of 6,901,324 patient discharges. J Arthroplasty 2010; 25 (1): 19-26.
- Nawabi DH, Chin KF, Keen RW, Haddad FS. Vitamin D deficiency in patients with osteoarthritis undergoing total hip replacement. A cause for concern? J Bone Joint Surg (Br) 2010; 92 (4): 496-9.
- Nüesch E, Dieppe P, Reichenbach S, Williams S, Iff S, Jüni P. All cause and disease specific mortality in patients with knee or hip osteoarthritis: population based cohort study. BMJ 2011; 342: d1165.
- Official Statistics of Finland (OSF): Causes of death. Life expectancy in 1983 and 2003. Helsinki: Statistics Finland, 2003. (cited 2011 Aug 22). Available from http://www.stat.fi/til/ksyyt/2003/ksyyt_2003_2005-05-31_tau_001_en.html.
- Paksima N, Koval KJ, Aharanoff G, Walsh M, Kubiak EN, Zuckerman JD, Egol KA. Predictors of mortality after hip fracture: a 10-year prospective study. Bull NYU Hosp Jt Dis 2008; 66 (2): 111-7.
- Parvizi J, Johnson BG, Rowland C, Ereth M, Lewallen DG. Thirty-day mortality after elective total hip arthroplasty. J Bone Joint Surg (Am) 2001a; 83 (10): 1524-8.
- Parvizi J, Sullivan TA, Trousdale RT, Lewallen DG. Thirty-day mortality after total knee arthroplasty. J Bone Joint Surg (Am) 2001b; 83 (8): 1157-61.
- Parvizi J, Mui A, Purtill JJ, Sharkey PF, Hozack WJ, Rothman RH. Total joint arthroplasty: When do fatal or near-fatal complications occur? J Bone Joint Surg (Am) 2007; 89 (1): 27-32.
- Pedersen AB, Mehnert F, Overgaard S, Johnsen SP. Allogeneic blood transfusion and prognosis following total hip replacement: a population-based follow up study. BMC Musculoskelet Disord 2009; 10: 167.
- Pedersen AB, Baron JA, Overgaard S, Johnsen SP. Short- and long-term mortality following primary total hip replacement for osteoarthritis: a Danish nationwide epidemiological study. J Bone Joint Surg (Br) 2011; 93 (2): 172-7.
- Pioli G, Barone A, Giusti A, Oliveri M, Pizzonia M, Razzano M, Palummeri E. Predictors of mortality after hip fracture: results from 1-year follow-up. Aging Clin Exp Res 2006; 18(5): 381-7.
- Qiu WQ, Dean M, Liu T, George L, Gann M, Cohen J, Bruce ML. Physical and mental health of housebound older adults: an overlooked population. J Am Ger Soc 2010; 58 (12): 2423-8.
- Robertsson O, Dunbar MJ, Knutson K, Lidgren L. Past incidence and future demand for knee arthroplasty in Sweden: a report from the Swedish Knee Arthroplasty Register regarding the effect of past and future population changes on the number of arthroplasties performed. Acta Orthop Scand 2000; 71 (4): 376-80.
- Robertsson O, Stefánsdóttir A, Lidgren L, Ranstam J. Increased long-term mortality in patients less than 55 years old who have undergone knee replacement for osteoarthritis: results from the Swedish Knee Arthroplasty Register. J Bone Joint Surg (Br) 2007; 89 (5): 599-603.
- Shervin N, Rubash HE, Katz JN. Orthopaedic procedure volume and patient outcomes: a systematic literature review. Clin Orthop 2007; (457): 35-41.
- Song J, Chang RW, Dunlop DD. Population impact of arthritis on disability in older adults. Arthritis Rheum 2006; 55 (2): 248-55.
- SooHoo NF, Lieberman JR, Ko CY, Zingmond DS. Factors predicting complication rates following total knee replacement. J Bone Joint Surg (Am) 2006; 88 (3): 480-5.
- SooHoo NF, Farng E, Lieberman JR, Chambers L, Zingmond DS. Factors that predict short-term complication rates after total hip arthroplasty. Clin Orthop 2010; 468 (9): 2263-71.
- Spahn DR. Anemia and patient blood management in hip and knee surgery. A systematic review of literature. Anesthesiology 2010; 113 (2): 482-95.
- Spiers NA, Matthews RJ, Jagger C, Matthews FE, Boult C, Robinson TG, Brayne C. Diseases and impairments as risk factors for onset of disability in the older population in England and Wales: findings from the Medical Research Council Cognitive Function and Ageing Study. J Gerontol A Biol Sci Med Sci 2005; 60 (2): 248-54.
- Thourani VH, Keeling WB, Kilgo PD, Puskas JD, Lattouf OM, Chen EP, Guyton RA. The impact of body mass index on morbidity and short- and long-term mortality in cardiac valvular surgery. J Thorac Cardiovasc Surg 2011; 142 (5): 1052-61.
- Timpini A, Facchhi E, Cossi S, Ghisla MK, Romanelli G, Marengoni A. Self-reported socio-economic status, social, physical and leisure activities and risk for malnutrition in late life: a cross-sectional population-based study. J Nutr Health Aging 2011; 15 (3): 233-8.
- Wu WC, Schifftner TL, Henderson WG, Eaton CB, Poses RM, Uttley G, Sharma SC, Vezeridis M, Khuri SF, Friedmann PD. Preoperative hematocrit levels and postoperative outcomes in older patients undergoing non-cardiac surgery. JAMA 2007; 297 (22): 2481-8.