Hemicortical resection was first described by Campanacci et al. (Citation1982). Several studies have shown the technique to be a safe alternative to larger segmental resections for low-grade chondrosarcoma (Deijkers et al. Citation2002), pareostal osteosarcoma (Lewis et al. Citation2000, Pezzillo et al. Citation2008), and adamantinoma (Agarwal et al. Citation2007). However, several complications have been reported with this resection and reconstruction, the most important being fractures of the host bone, inadequate margins, and infection.
The resections and reconstructions are usually done without objective 3D measurements. Computer-assisted surgery (CAS) offers objective measurements in 3D with high accuracy. It can be used to produce an exact copy of the resected part of the host bone by using the same resection planes in both tumor and allograft resection. In this technical note we describe the technique, report results, and identify shortcomings and possibilities.
Surgical technique
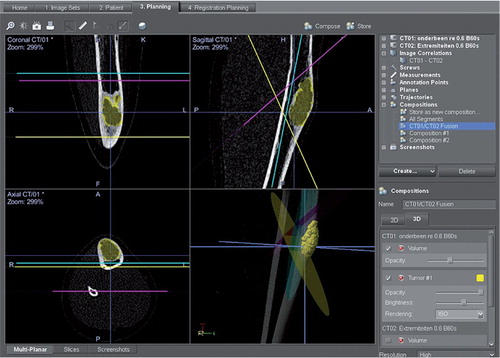
We used a fresh frozen donor tibia with similar dimensions to those of the host tibia. A preoperative CT scan was performed on both the patient and the donor bone. These scans were imported into the CAS system (Orthomap software; Stryker, Mahwah, NY) and manually matched to find the optimum overlay. Special care was given to matching of the cortices of the host and donor bone. The resection was planned with both resection planes and annotation points. The planned resection planes () from the CAS setup of the host bone are now also usable in the allograft dataset because the two datasets are linked and matched in the CAS system.
Figure 1. Preoperative planning screen. The tumor has been colored, to discern it more easily during the operation. The resection planes have been planned using the coronal, axial, and sagittal view. These planes are copied to the pre-matched CT of the donor bone.
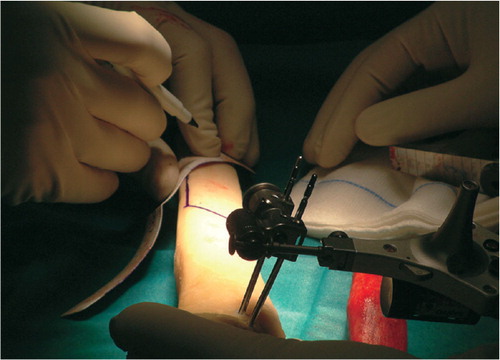
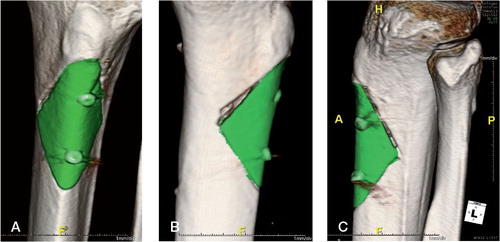
Normal CAS setup was performed using a patient tracker placed on the tibia. A system-calculated deviation, between the CT and spatial data, of under 1.0 mm was accepted as in our normal image-based setup. The pointer tool was then used to identify and mark the edges and entry points of the planned trapezoid or wedge-like shape. The excision planes were marked with a pen and checked with the pointer tool for accuracy. The corners of the resection shape were marked with annotation points (as special interest points) for extra feedback. We used an oscillating bone saw to perform the pre-planned trapezoid or wedge-shaped resection. Angulation of the saw was checked at intervals using the pointer tool. Resection planes were checked again for margins after resection. Exactly the same procedure was followed in the allograft bone (). 2 screws were used for fixation of the grafts.
Patients
4 patients were selected for hemicortical resection using CAS. All had a diagnosis of adamantinoma, reported by a specialized musculoskeletal pathologist. Mean patient age was 22 (8–54) years. In 3 of the 4 cases, 50% or more of the bone circumference was affected by the tumor. The average length of the resection and allograft was 7.5 (6–9) cm. The surgical margin was marginal in 3 patients and wide in 1, depending on adamantinoma subtype.
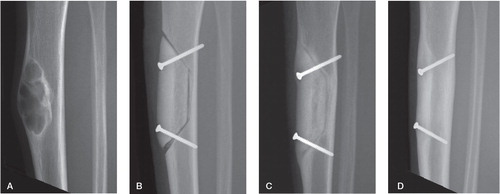
All grafts were reported by the radiologist as being well-aligned and with good bone contact. Postoperative and follow-up radiographs from the first patient are shown in . All patients are currently able to walk unassisted, and function is excellent. All of them are free of disease. There have been no complications.
Figure 3. Radiographic series of the first patient. A. OFD-like AD lesion in situ. B. Immediately postoperatively. The graft and the host resection planes are both smooth and in close proximity. The distal point of the host bone has a small defect, most probably created by the vibrations of the saw blade. The remaining gap is filled with Vitoss (Orthovita Inc., Malvern, PA). C. Progressive ingrowth after 5 months. Cortical hypertrophy is clearly visible. D. Full integration and almost entirely faded boundary line at 16 months.
The allografts have fully integrated in 3 patients. In the fourth patient, there was progressive consolidation and proximal incorporation at the 3-month follow-up. Mean time until full integration, measured by the fading of the boundary line, was 6 (5–8) months.
A 1-day postoperative CT scan, with 1.0 mm slice thickness, of the fourth patient was analyzed using advanced visualization software (iNtution; TeraRecon, and Photoshop CS5; Adobe). It showed an average gap of 0.9 (0–5.4) mm. In these 60 slices, 76 gap measurements of 120 were below 1.0 mm. This was with 2 measurements per slice, the lateral and medial gap between host and donor bone. A gap of more than 5 mm was only measured once.
Discussion
Deijkers et al. (Citation2002) described 22 patients with low-grade malignant bone tumors who underwent hemicortical resections. A fracture of the remaining hemicortex occurred in 6 patients: in 3 patients during the operation and in 3 others shortly afterwards. The authors speculated that optimal matching of the allograft precisely to the host bone defect, i.e. a larger graft-bone contact area, would lead to fewer complications such as fractures.
Our preliminary results indicate that CAS makes it possible to both resect and reconstruct more precisely. This may lead to fewer intraoperative and postoperative fractures due to better allograft fit. Furthermore, earlier integration can be expected if the gap between host bone and allograft is smaller.
The proximal resection plane in shows an increasingly larger gap, especially for the medial cortex. We believe that this is due to an angulation error of the oscillating saw. Due to increasing distance from the entry point, the error accumulates. The correction to the planned angle can be seen in the CT scan, as there is a small fragment of bone between the resection plane that is too wide and the correct one (). We consider that this finding supports the need for a navigated means of resection, as the system can check the angulation of the saw at any point in the resection.
Figure 4. Graph of the post operative CT scan of the fourth patient. Average gap was 0.9 mm (range 0–5.4). The sharp increase of the medial gap is due to an angulation error during resection.
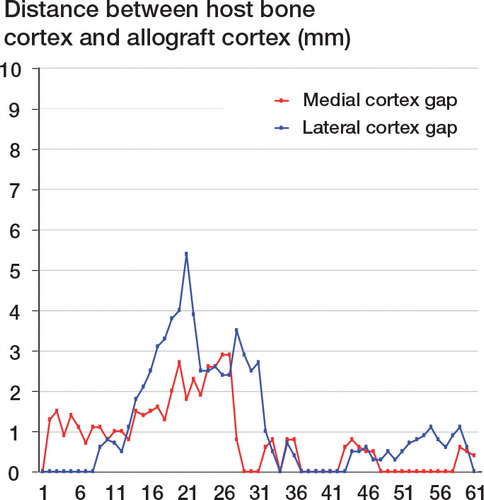
Figure 5. 3D rendered images made with iNtution (TeraRecon). The allograft is auto-segmented and colored green. The medial view shows the defect caused by an angulation misalignment in the last stage of the proximal resection plane. A. Medial view. 2 distinct resection cuts are visible. B. Anterior-posterior view. C. Lateral view.
We tried to attach a tracker to a bone saw and to use it with navigation in the first procedure, in order to excise the tumor and cut the graft, but this proved to be inaccurate. The tracker was attached to the saw and calibrated in a universal calibration tool, but the blade was too flexible for reliable calibration.
Pre-planned saw blocks for both the patient bone and allograft bone could be alternatives. CAS has the advantage that the resection planes can be adjusted during surgery and there is no placement inaccuracy. Another alternative is prefabrication by 3D printing of a filler material. Accurate resection must be performed for the filler to fit, and we feel that navigation is again required. Furthermore, a non-biological solution is more likely to fail in the long run.
The CAS system makes the creation of the allograft easier. The technique can be applied to any bone tumor eligible for hemicortical resection, and also to other defects requiring bony reconstructions.
Conception and design: J-G and P-J. Analysis and interpretation: all authors. Drafting, revision, and final approval of manuscript: all authors.
No competing interests declared.
- Agarwal M, Puri A, Anchan C, Shah M, Jambhekar N. Hemicortical excision for low-grade selected surface sarcomas of bone. Clin Orthop 2007; (459): 161-6.
- Campanacci M, Capanna R, Stilli S. Posterior hemiresection of the distal femur in parosteal osteosarcoma. Ital J Orthop Traumatol 1982; 8 (1): 23-8.
- Deijkers RL, Bloem RM, Hogendoorn PC, Verlaan JJ, Kroon HM, Taminiau AH. Hemicortical allograft reconstruction after resection of low-grade malignant bone tumours. J Bone Joint Surg (Br) 2002; 84 (7): 1009-14.
- Lewis VO, Gebhardt MC, Springfield DS. Parosteal osteosarcoma of the posterior aspect of the distal part of the femur. Oncological and functional results following a new resection technique. J Bone Joint Surg (Am) 2000; 82 (8): 1083-8.
- Pezzillo F, Maccauro G, Nizegorodcew T, Rossi B, Gosheger G. Resection of parosteal osteosarcoma of the distal part of the femur: An original reconstruction technique with cement and plate. Sarcoma 2008; 2008: 763056.