Abstract
Background and purpose There is no consensus on how to predict residual equinovarus deformities after application of the Ponseti method. We assessed the prognostic value of clinical scoring systems, and also radiographic parameters that can be measured just before percutaneous Achilles tenotomy (PAT).
Method We reviewed 50 cases of clubfoot in 35 patients who were treated using the Ponseti method, including PAT, to analyze the factors that are predictive of residual equinovarus deformities. Mean age at the time of PAT was 2.4 (1.4–3.5) months, and the mean follow-up period was 23 (9–61) months. We divided these cases into 2 groups according to the need for further surgery to treat the residual deformities.
Results 40 feet with satisfactory results were included in group 1, whereas the remaining 10 feet that required further surgery for unsatisfactory residual deformities were included in group 2. We compared the initial Dimeglio and Pirani scores obtained before the first Ponseti casting, follow-up Pirani scores, and radiographic parameters determined just before PAT between these 2 groups. There was no statistically significant difference between the groups in terms of the initial Dimeglio and Pirani scores, although the follow-up Pirani scores and lateral tibiocalcaneal angle were higher and the lateral talocalcaneal angle was lower in group 2 at the time of PAT.
Interpretation We conclude that the Pirani score, lateral tibiocalcaneal angle, and talocalcaneal angle, when assessed immediately before PAT, might be predictive factors for residual equinovarus deformity following Ponseti treatment for severe idiopathic clubfoot.
There is general agreement that the initial treatment for idiopathic congenital clubfoot should be nonoperative, regardless of the severity of the deformity, and should be started as soon as possible after birth. Percutaneous Achilles tenotomy (PAT) is currently an integral part of the Ponseti technique (Morcuende et al. Citation2005). PAT can facilitate the correction of residual equinus deformity and minimize the risk of relapse (Scher et al. Citation2004). The indication for PAT is < 15° dorsiflexion of the ankle (Ponseti Citation1992). However, sometimes it is difficult to evaluate the actual dorsiflexion angle of the ankle of a small foot, especially when the patient’s condition is complicated by a midfoot break. There is a lack of objective radiographic guidelines to make the clinical decision to perform PAT. Since 2006, we have regarded a lateral tibiocalcaneal angle of > 80° to be an indicator for performing PAT after 4–6 serial Ponseti castings.
During the treatment of clubfoot, it is important to assess the severity of the deformity and to predict the clinical outcome in order to provide parents with ample predictive and prognostic information about treatments. Although the Pirani and Dimeglio scoring systems (Dimeglio et al. Citation1995, Pirani et al. Citation2008) are widely used for grading the severity of clubfoot deformities and have very good interobserver reliability (Flynn et al. Citation1998), there have been few reports on the prognostic significance of these scores (Scher et al. Citation2004, Dyer and Davis Citation2006, Uglow et al. Citation2007).
The goal of the treatment for clubfoot is to have a functional, pain-free, plantigrade foot with good mobility that does not require the patient to wear modified shoes (Hegazy et al. Citation2009). Some feet can be fully corrected to functional plantigrade feet, whereas others will still present with undercorrected residual equinovarus deformities despite the proper use of the Ponseti method. Furthermore, there is no consensus regarding which clubfeet will still have residual deformities after nonoperative treatment using the Ponseti method.
We performed a retrospective study to provide predictive and prognostic factors for clinical scoring systems, and also radiographic parameters that can be measured just before PAT, which can be used to predict residual equinovarus deformities after use of the Ponseti method.
Patients and methods
This study involved a retrospective and consecutive review of 50 clubfeet in 35 patients who had undergone PAT under general anesthesia as part of the Ponseti program, from May 2006 through June 2010. Institutional review board approval was obtained.
The medical records were reviewed in order to obtain demographic and clinical data. We only included patients with idiopathic clubfoot deformities who had undergone PAT and we excluded patients with idiopathic clubfoot deformities who had not undergone PAT and patients with syndromic or neuromuscular clubfoot. The clubfoot was graded before the first casting using the scoring systems of Dimeglio et al. (Citation1995) and Pirani et al. (Citation2008). The latter scoring system was also used at the time of PAT and at the last follow-up examination.
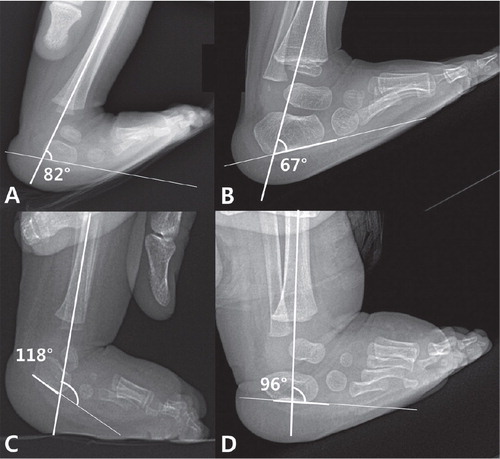
To perform the radiographic evaluation, anteroposterior (AP) and dorsiflexion lateral radiographs of the feet were taken at the time of PAT, at the last follow-up examination, and before further treatments if required. The AP view for measurement of the AP talocalcaneal angle was obtained when the foot was pressed against the radiographic plate and held in the position of maximum dorsiflexion and external rotation in order to simulate a weight-bearing anteroposterior radiograph. The lateral tibiocalcaneal and talocalcaneal angles were measured from the maximum dorsiflexion lateral view (). We performed all radiographic measurements independently.
Radiographic measurement of the lateral tibiocalcaneal angle in each group of patients. A. A lateral tibiocalcaneal angle of 82° before PAT in a 3-month-old infant. B. The same infant at 15 months of age; the lateral tibiocalcaneal angle was 67°. This child was assigned to group 1. C. A lateral tibiocalcaneal angle of 118° before percutaneous Achilles tenotomy in a 3-month-old infant. D. The same infant at 12 months of age; the lateral tibiocalcaneal angle was 96° before selective soft tissue release was performed to treat the residual equinovarus deformity. This child was assigned to group 2.
All castings were made by a pediatric orthopedic surgeon (SSP) according to the method described by Ponseti (Ponseti and Smoley Citation1963) during the first 2 months of life. After making 4–6 serial Ponseti castings during the first 2 months, forefoot adduction and hindfoot varus deformities (except ankle equinus deformities) were corrected to a neutral or overcorrected position in all patients. PAT was performed on all patients with a lateral tibiocalcaneal angle of > 80° on the dorsiflexion lateral view of the affected foot after 4–6 serial Ponseti castings. In this study, we included all patients who underwent PAT to treat a lateral tibiocalcaneal angle of > 80°. 3 weeks after long-leg castings were made, the full-time use of a Denis Browne abduction orthosis for 3 months was recommended for all patients in order to prevent relapse after PAT. After 3 months of full-time bracing, nighttime abduction orthosis and daytime massage were advised until the patient was 3 years old. All patients were scheduled to be seen regularly at the outpatient clinic in order to check for residual deformities, and we assessed bracing compliance by interviewing the parents.
After a mean follow-up period of 23 (9–61) months after PAT, we divided the 50 cases of clubfoot into 2 groups according to the requirement for further surgery—in order to treat residual deformities that were noted during the follow-up period. 40 feet, with or without minor residual deformities and > 5° of ankle dorsiflexion, were assigned to group 1. 10 feet with residual deformities and < 5° of ankle dorsiflexion, with or without apparent forefoot adduction or resting heel varus, were assigned to group 2. All feet in group 2, which were considered to have unsatisfactory results, received further operations (). For group 1, the results at the last follow-up examination were considered final, while in group 2 the results obtained just before selective soft tissue release that required further treatment for residual equinovarus deformity were considered final (Park et al. Citation2009).
Table 1. Characteristics of the 10 clubfeet in 7 patients with residual clubfoot deformities
We compared the initial Dimeglio and Pirani scores, follow-up Pirani scores obtained at the time of PAT and at the last follow-up examination, and the radiographic parameters evaluated just before PAT and at the last follow-up examination between groups 1 and 2 in order to identify predictive and prognostic factors for residual equinovarus deformities.
Statistics
We used the Kruskal-Wallis test to compare demographics between groups 1 and 2. In addition, the linear mixed model was used to consider both unilateral and bilateral observations. Intraclass correlation coefficients were used to assess the reproducibility of the radiographic evaluations of the 2 observers. Any p-value < 0.05 was considered statistically significant. SPSS version 18.0 was used to perform these analyses.
Results
The study included 26 boys and 9 girls. Clubfoot deformities were bilateral in 15 patients and unilateral in the remaining 20 patients. 28 right feet and 22 left feet were involved. Mean gestational age and mean weight at birth were 39 (27–41) weeks and 3.1 (1.2–3.8) kg, respectively. The mean initial Dimeglio and Pirani scores before the first casting were 13 (10–19) points (of 20 points) and 4.4 (3.5–6.0) points (of 6 points), respectively. Mean age at the time of PAT was 2.4 (1.4–3.5) months.
All radiographic parameters were measured twice by each observer just before PAT. The mean overall AP talocalcaneal angle was 7.9° (–9 to 20). The mean overall lateral tibiocalcaneal angle was 97° (80–137) and the mean lateral talocalcaneal angle was 25° (–5 to 57).
40 clubfeet were included in group 1, and the remaining 10 clubfeet were included in group 2. There were no statistically significant differences between groups 1 and 2 in terms of demographic factors ().
Table 2. Demographics of groups 1 and 2. Values are mean (SD)
The mean time of nighttime bracing per day after 3 months of full-time bracing was similar between the 2 groups. Group 1 wore the brace for 6.9 (4–9) hours/day and group 2 wore the brace for 7.5 (4–9) hours/day (p = 0.6).
For group 1, the mean Pirani score improved to 2.2 (1.0–5.0) points at the time of PAT and was 1.5 (0.5–3.0) points after a mean follow-up of 24 (15–61) months (p < 0.001). For group 2, the mean Pirani score improved to 3.1 (2.0–3.5) points at the time of PAT and was 2.7 (1.5–3.0) points after a mean follow-up of 19 (9–57) months (p = 0.005) (). Differences in initial Dimeglio and Pirani scores between the 2 groups were not statistically significant. However, at the time of PAT and at the last follow-up examination, the Pirani scores in group 2 were significantly higher than those in group 1.
Table 3. Clinical scores of groups 1 and 2. Values are least-squares mean (SE) [95% CI]
In group 1, the mean AP talocalcaneal angle was 8° (–3 to 20), the mean lateral tibiocalcaneal angle was 95° (80–137), and the mean lateral talocalcaneal angle was 28° (1–55) at the time of PAT; for group 2, these angles were 7° (–7 to 18), 107° (86–126), and 13° (–5 to 55), respectively (). The differences in the lateral tibiocalcaneal angles and lateral talocalcaneal angles between these 2 groups were statistically significant. At the last follow-up examination, the mean AP talocalcaneal angle was 22° (12–33), the mean lateral tibiocalcaneal angle was 72° (51–104), and the mean lateral talocalcaneal angle was 24° (8–50) in group 1; in group 2, these angles were 23° (15–31), 99° (65–111), and 19° (8–37), respectively. At the last follow-up examination, the mean degree of ankle dorsiflexion in group 1 was 23° (10–40) and in group 2 it was 4° (0–30).
Table 4. Radiographic data for groups 1 and 2 at the time of PAT. Values are least-squares means (SE) [95% CI]
Regarding tests for correlation between the Pirani score at the last follow-up examination and the radiographic parameters measured at the time of PAT in all 50 clubfeet, there was a positive Spearman correlation coefficient (r = 0.61) between the Pirani score and the lateral tibiocalcaneal angle and a negative correlation (r = –0.42) between the Pirani score and the lateral talocalcaneal angle, both of which were statistically significant at the 5% level. The correlation coefficients for the Pirani score at the last follow-up examination and the radiographic parameters before PAT are shown in .
Table 5. Degree of correlation between Pirani score at the last follow-up examination and the radiographic parameters measured at the time of PAT. All values are correlation coefficient (p-value)
The measurements by the 2 observers showed a high level of reproducibility ().
Table 6. Radiographic results of the 50 clubfeet that were evaluated by 2 observers at the time of PAT
Discussion
In 1950, Ponseti developed a method for treating congenital idiopathic clubfoot that uses manipulation and casting followed by PAT if pes equinovarus deformity remains (Ponseti Citation1992). This method is successful in almost 90% of cases (Herzenberg et al. Citation2002, Hegazy et al. Citation2009), and PAT should be the treatment for almost 85% of clubfeet (Morcuende et al. Citation2005). Indication for PAT is when the patient can only perform < 15° dorsiflexion of the ankle (Ponseti Citation1992). Sometimes it is difficult to determine the range of motion of a small foot, especially when complicated by a midfoot break and presents with pseudodorsiflexion. Since 2006, we have started to consider the dorsiflexion lateral view of the affected foot after 4–6 serial Ponseti castings in order to obtain more objective radiographic data and evaluate the necessity of performing PAT. We usually regard a lateral tibiocalcaneal angle of > 80° to be an indicator of PAT.
Simons (Citation1978) described the absence or small size of ossification centers in young children. Radler et al. (Citation2007) also noted that radiographic measurements of infant feet are not fully reliable. They stated that there is a bias when drawing lines to represent the axes of the ossific nuclei, which often appear almost circular at very young ages. The mean age of the patients in their report was 9 weeks when the angle was measured. We believe that the tarsal bones of our patients were actually more ossified and that radiographic measurements would be more accurate and reliable because the mean age of the patients at the time of PAT was around 10 weeks. All of the intraclass correlation coefficients for the 3 radiographic parameters were also > 0.9. Also, because the most predictive factor in our study was the lateral tibiocalcaneal angle, for which the axes were drawn in a constant and obvious line, the measurements were considered to be sufficiently reliable.
In infants with normal feet, the maximum dorsiflexion lateral tibiocalcaneal angle is typically 25–65° (Vanderwilde et al. Citation1988). In clubfoot, a tight heel cord restricts calcaneal movement during dorsiflexion, thus resulting in an increased angle. The lateral tibiocalcaneal angle is influenced by the relationship between the tibia and the calcaneus (de Gheldere and Docquier Citation2008), and an increased angle indicates severe contracture of the soft tissue around the posterior ankle joint, including the Achilles tendon, posterior capsule of the ankle joint, tibialis posterior, peroneal tendon sheath, and other soft tissues. Soft tissue contracture around the posterior ankle joint may also have an effect on the parallel relationship between the talus and the calcaneus, as seen on lateral radiographs, thus reducing the lateral talocalcaneal angle. Because PAT affects the release of only the contracted Achilles tendon, the other remaining contracted soft tissues will continue to be risk factors for residual equinovarus deformities. Based on our results, we believe that clubfeet that present with an increased lateral tibiocalcaneal angle and a reduced talocalcaneal angle prior to PAT are at a higher risk of residual equinovarus deformities than those with a reduced lateral tibiocalcaneal angle and increased talocalcaneal angle.
We have found no studies in the English-based literature on the relationship between the radiographic parameters of clubfoot and the tendency for residual equinovarus deformities. We observed an increased lateral tibiocalcaneal angle and a reduced talocalcaneal angle in group 2. As shown in , there was a correlation between the lateral tibiocalcaneal angle and the degree of ankle dorsiflexion seen at the last follow-up examination. This indicates that a high initial lateral tibiocalcaneal angle reduces the degree of ankle dorsiflexion seen on physical examination; therefore, further treatment may be required.
We divided the 50 clubfeet into 2 groups according to whether further surgery (e.g. selective soft tissue release) would be needed, which was mainly determined by the degree of dorsiflexion at the ankle as measured on physical examination. Scher et al. (Citation2004) reported that an initial score of > 5.0 on the Pirani scale and grade IV feet according to the Dimeglio system would indicate that the patient will very likely need PAT. In addition, Uglow et al. (Citation2007) reported that a higher grade according to the Dimeglio system indicates a high rate of relapse. This indicates that clubfeet with higher scores, according to these 2 scoring systems, are at risk of having residual equinus deformities even after Ponseti manipulation. However, some authors have reported that there is no significant relationship between the initial Pirani or Dimeglio scores and the rate of relapse (Dobbs et al. Citation2004, Haft et al. Citation2007). The initial Dimeglio and Pirani scores were not significantly different in groups 1 and 2, which is in agreement with the studies by Dobbs et al. (Citation2004) and Haft et al. (Citation2007).
Although the initial Pirani scores were not statistically significantly different in groups 1 and 2, follow-up Pirani scores at the time of PAT and at the last follow-up examination were significantly higher in group 2—and they also showed a highly positive correlation with the lateral tibiocalcaneal angle. These results indicate that patients with a high lateral tibiocalcaneal angle tended to have a high Pirani score and a low degree of ankle dorsiflexion at the last follow-up examination; thus, these patients required further treatment.
In conclusion, we suggest that the clinical Pirani score, lateral tibiocalcaneal angle, and lateral talocalcaneal angle should be measured at the time of PAT because they may predict residual equinovarus deformities that might show even after Ponseti treatment of severe idiopathic clubfoot.
We thank Min-Joo Kim, PhD, of the Department of Clinical Epidemiology and Biostatistics, College of Medicine, University of Ulsan, Seoul, Korea for advice regarding the statistical analyses performed in this study.
No competing interests declared.
- de Gheldere A, Docquier PL. Analytical radiography of clubfoot after tenotomy. J Pediatr Orthop 2008; 28 (6): 691-4.
- Dimeglio A, Bensahel H, Souchet P, Mazeau P, Bonnet F. Classification of clubfoot. J Pediatr Orthop B 1995; 4 (2): 129-36.
- Dobbs MB, Rudzki JR, Purcell DB, Walton T, Porter KR, Gurnett CA. Factors predictive of outcome after use of the Ponseti method for the treatment of idiopathic clubfeet. J Bone Joint Surg (Am) 2004; 86 (1): 22-7.
- Dyer PJ, Davis N. The role of the Pirani scoring system in the management of club foot by the Ponseti method. J Bone Joint Surg (Br) 2006; 88 (8): 1082-4.
- Flynn JM, Donohoe M, Mackenzie WG. An independent assessment of two clubfoot-classification systems. J Pediatr Orthop 1998; 18 (3): 323-7.
- Haft GF, Walker CG, Crawford HA. Early clubfoot recurrence after use of the Ponseti method in a New Zealand population. J Bone Joint Surg (Am) 2007; 89 (3): 487-93.
- Hegazy M, Nasef NM, Abdel-Ghani H. Results of treatment of idiopathic clubfoot in older infants using the Ponseti method: a preliminary report. J Pediatr Orthop B 2009; 18 (2): 76-8.
- Herzenberg JE, Radler C, Bor N. Ponseti versus traditional methods of casting for idiopathic clubfoot. J Pediatr Orthop 2002; 22 (4): 517-21.
- Morcuende JA, Abbasi D, Dolan LA, Ponseti IV. Results of an accelerated Ponseti protocol for clubfoot. J Pediatr Orthop 2005; 25 (5): 623-6.
- Park SS, Kim SW, Jung BS, Lee HS, Kim JS. Selective soft-tissue release for recurrent or residual deformity after conservative treatment of idiopathic clubfoot. J Bone Joint Surg (Br) 2009; 91 (11): 1526-30.
- Pirani S, Hodges D, Sekeramyi F. A reliable and valid method of assessing the amount of deformity in the congentital clubfoot deformity. J Bone Joint Surg (Br) (Suppl) 2008; 90: 53.
- Ponseti IV. Treatment of congenital club foot. J Bone Joint Surg (Am) 1992; 74 (3): 448-54.
- Ponseti IV, Smoley EN. Congenital clubfoot: the results of treatment. J Bone Joint Surg (Am) 1963; 45: 261-75.
- Radler C, Manner HM, Suda R, Burghardt R, Herzenberg JE, Ganger R, Grill F. Radiographic evaluation of idiopathic clubfeet undergoing Ponseti treatment. J Bone Joint Surg (Am) 2007; 89 (6): 1177-83.
- Scher DM, Feldman DS, van Bosse HJ, Sala DA, Lehman WB. Predicting the need for tenotomy in the Ponseti method for correction of clubfeet. J Pediatr Orthop 2004; 24 (4): 349-52.
- Simons GW. A standardized method for the radiographic evaluation of clubfeet. Clin Orthop 1978; (135): 107-18.
- Uglow MG, Senbaga N, Pickard R, Clarke NM. Relapse rates following staged surgery in the treatment of recalcitrant talipes equinovarus: 9- to 16-year outcome study. J Child Orthop 2007; 1 (2): 115-9.
- Vanderwilde R, Staheli LT, Chew DE, Malagon V. Measurements on radiographs of the foot in normal infants and children. J Bone Joint Surg (Am) 1988; 70 (3): 407-15.