Abstract
Background and purpose Humeral lengthening and deformity correction are now being done increasingly for various etiologies. Monolateral external fixators have advantages over traditional Ilizarov circular fixators; they are easy to apply, they are less bulky, and they are therefore more convenient for the patient. We assessed the effectiveness of hybrid monolateral lateral fixators in humeral lengthening and deformity correction.
Methods We retrospectively reviewed 23 patients (40 humeri) with various pathologies who underwent lengthening—with or without deformity correction using monolateral external fixator—between 2003 and 2008. Mean age at the time of the surgery was 14 (10–22) years. The mean follow-up time was 3.4 (1–7) years.
Results The average duration of external fixator use was 8.3 (6–19) months. The mean lengthening achieved was 8.8 (4–11) cm and percentage lengthening was 49% (19–73). The healing index was 28 (13–60) days/cm. The major complications were refracture in 3 humeri and varus angulation of 2 humeri. The minor complications were superficial pin tract infection (6 segments), transient radial nerve palsy (1 segment), and elbow flexion contracture (5 segments). All complications resolved.
Interpretation Hybrid monolateral fixators can be used for humeral lengthening and deformity correction. The advantage over circular fixators is that they are less bulky and patients can perform their day-to-day activities with the fixator in situ.
Distraction osteogenesis allows correction of length and various deformities of the bones. It is used extensively in lower limbs, but few reports are available for upper limbs because it is generally believed that mild-to-moderate deformities of the arm do not cause significant functional deficits. However, humeral length discrepancies can cause functional impairments when patients engage in activities that require coordinated movement such as playing musical instruments and sports (Katz et al. Citation1989, Tetsworth et al. Citation1991, Lee et al. Citation2005).
Lower-limb lengthening has become one of the standard modalities for treatment of achondroplasia (Paley Citation1988, Cai et al. Citation2007). As the results are encouraging, more and more achondroplasia patients are now opting for humeral lengthening after femoral lengthening, with a cosmetically unappealing disparity between upper and lower extremities. Short arms may also cause functional limitation. Compared with lengthening of the femur or tibia, literature regarding humeral lengthening in achondroplasia is scarce (Kashiwagi et al. Citation2001, Shadi and Koczewski Citation2007).
Gradual distraction osteogenesis using either monolateral fixators or circular fixators is the preferred treatment for humeral lengthening and correction of deformity (Cattaneo et al. Citation1990, Tanaka et al. Citation1998, Kashiwagi et al. Citation2001, Lee et al. Citation2005, Kiss et al. Citation2008). However, circular fixators are bulky and difficult to apply, especially bilaterally. Monolateral fixators are easier to apply and are less cumbersome (Shadi and Koczewski Citation2007), especially in cases with lengthening only.
We evaluated the role of hybrid monolateral external fixators in managing humeral lengthening and deformity correction for various pathologies.
Patients and methods
After receiving approval from the Institutional Review Board of our hospital, we retrospectively analyzed all patients who underwent humeral lengthening and deformity correction using monolateral external fixator at our institute between 2003 and 2008. We included 23 patients (40 humeri) with different etiology (). There were 17 genetically proven achondroplasia patients, 3 postosteomyelitis patients, and 3 traumatic physeal arrest patients. All achondroplasia patients had bilateral humeral lengthening while 6 of the other patients had unilateral lengthening and deformity correction using hybrid monolateral fixator. The mean age of the patients (15 females) at the time of the surgery was 14 (10–22) years. The mean follow-up time was 3.4 (1–7) years.
Table 1. Clinical details of the patients treated with humeral monolateral fixator
Operative technique ( and )
Figure 1. A. Case no 4. A 12-year-old girl with achondroplasia showing shortened right humerus.
B. Osteotomy and monolateral fixator application for gradual lengthening of shortened humerus.
C. Desired length achieved with use of monolateral fixator.
D. 7 months after osteotomy, full consolidation of the newly formed callus. The pixel value ratio (PVR) measured at this point was > 1 in all 4 cortices.
E. At the final follow up, 2 years after osteotomy.
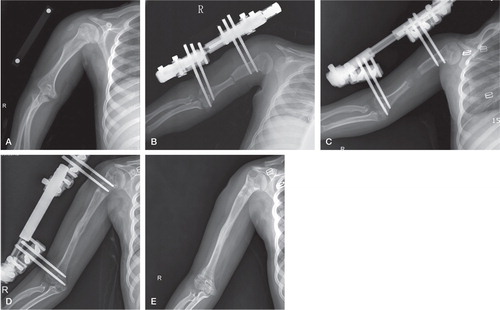
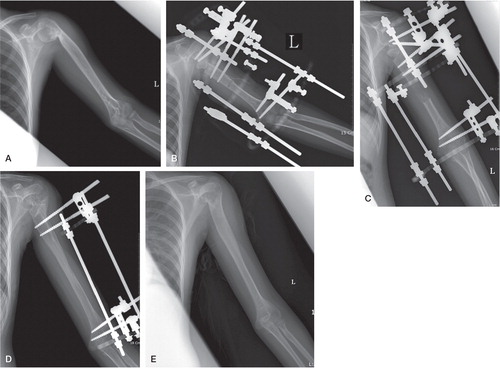
Figure 2. A. Case no 20. A 10-year-old female with shortened and deformed (varus angulation) proximal humerus due to osteomyelitis.
B. Bifocal humeral osteotomy with use of hybrid monolateral fixator for correction of deformity and lengthening simultaneously.
C. Desired lengthening of the humerus at the distal osteotomy site.
D. Full consolidation of the lengthening site, 7 months after osteotomy. Proximal pins and assembly were removed after healing of proximal osteotomy, thereby converting it to a simple monolateral fixator.
E. Final follow-up 5 years after osteotomy, showing excellent remodeling.
All surgery was performed by the senior author (HRS). In all achondroplasia patients, both sides were lengthened simultaneo-usly using monolateral external fixators (U & I Co. Ltd., Seoul, Korea). Surgery was performed under general anesthesia. First, 2 or 3 Schanz screws (depending on the length of the bone) were passed in the proximal metaphyseal region and distal humerus perpendicular to their anatomical axis using an image intensifier. The external fixator was then connected between these Schanz screws. An oblique skin incision was made in the anterolateral region of the mid-arm and muscles were split down to the bone. Periosteum was incised longitudinally and retracted with a periosteal elevator. Using a drill bit in a drill sleeve, multiple transverse drill holes were made in the mid-diaphyseal region of the bone. Through these drill holes, an osteotomy was performed with an osteotome.
For varus deformities of the proximal humerus along with shortening after physeal arrest or osteomyelitis, bifocal osteotomy of the humerus was performed. At the proximal osteotomy, correction of deformity was done and at the distal osteotomy, gradual lengthening was performed. Pins in different planes were connected using arches, rings, and rods. The advantage of this assembly was that we could adjust the magnitude of the correction post operatively. Once deformity correction was achieved, we waited for the consolidation of the osteotomy site. Then the assembly was converted from the hybrid to the simple monolateral fixator and the desired lengthening was achieved.
Postoperatively, lengthening was started after 7 days at a rate of 1 mm/day (0.25 mm every 6 h). The rate was subsequently adjusted according to the morphology of the callus, as described by Li et al. (Citation2006). Physiotherapy was given 2 or 3 times per week to prevent development of elbow contracture. Our protocol for removal of the external fixator after completion of the lengthening was changed in 2005. Initially it was based on radiographically adequate consolidation, but later it was based on pixel value ratio (PVR) as previously described by us (Singh et al. Citation2010). The value of 1 indicates adequate corticalization of the regenerate for safe removal of the fixator. With this method, patients were not braced/splinted after fixator removal.
We followed patients on a weekly basis for the first month, bi-weekly during the lengthening period. After lengthening period—usually 2–3 months after the surgery—then monthly basis visit during consolidation period. At every visit, we clinically evaluated pain, range of movement at the elbow and shoulder, condition of the pin tract, and angulation or translation of the osteotomy site. Muscle functions were checked to detect nerve injuries.
Ranges of shoulder and elbow motion were recorded at each visit. Patients and/or parents were interviewed to determine functional outcome, specific changes in conducting activities of daily living or sports participation, and whether the patient would opt for this surgical intervention again if given the choice. We completed 2 validated quality-of-life (QOL) questionnaires, the Short Form 36 (SF-36) and the Rosenberg self-esteem questionnaire. The QOL scores were analyzed preoperatively and postoperatively.
Radiographic evaluation
At the final follow-up, the external fixator index (EFI), healing index (HI), amount of lengthening, and percentage of initial length gained were recorded. EFI was calculated by dividing the entire duration of external fixation in days by the total length of regenerate in cm (Paley et al. Citation1997). The healing index is defined as the time required for 1 cm of newly formed callus to consolidate, and is calculated by dividing the total length of time in days—from the time of stopping the distraction to the time when the external fixator is removed—by the total increase in length of the bone (Devmurari et al. Citation2010).
We classified the complications as minor or major according to Paley (Citation1990). The major complications interfered with the original goals of the treatment and the minor ones did not.
Results
The mean gain in length of the humerus was 8.8 (4–11) cm. The mean lengthening percentage (LP) was 49% (19–73). The mean healing index (HI) was 28 (13–60) days/cm. The mean external fixator index (EFI) was 30 (15–60) days per cm ().
Table 2. Comparison of various series using different modalities for humeral lengthening for various etiologies
Complications
11 minor and 6 major complications were encountered in 40 segments. The minor complications were 6 pin tract infections, 5 of which healed with pin tract dressing and oral antibiotic. In 1 case, a pin loosened. Elbow flexion contractures of 20–35° occurred in 3 patients (5 segments) but they resolved following physiotherapy, with a return to full motion. Radial nerve neuropraxia occurred in 1 segment during distraction phase (1 mm per day). There was spontaneous recovery after 2 months.
Refracture of the humerus occurred in 3 patients through newly generated bone at the diaphyseal region. All refractures occurred in patients prior to using PVR for removal of the fixator. All refractures were treated with a sugar-tong splint, and all united (). No patients had fracture through a pin site. There was no non-union in any of the patients. 2 patients developed varus angulation (20º and 30º) after removal of the fixator. No surgery was done for this deformity, and there was no functional limitation at final follow-up.
Functional outcome
At the final follow-up, all patients carried out their normal activities and engaged in sports. When the patients or their parents were asked whether they would opt for this surgical intervention again if given the choice, all of them said that they would be happy to do it.
The quality-of-life scores were calculated to measure improvement after surgery. Rosenberg self-esteem questionnaire score was higher after lengthening (mean 25, SD 0.7) than before lengthening (mean 21, SD 0.4) (p < 0.001). The SF-36 score also improved (p = 0.04 for the physical component summary, p = 0.002 for the mental component summary, and p = 0.007 for the total score).
Discussion
Humerus lengthening was first reported by Dick and Tietjen (Citation1978) using a Wagner lengthening device, plating, and autogenous bone graft. Since then, many authors have had success in treating humeral deformities with the Ilizarov frame, the monolateral fixator, and recently the Taylor spatial frame. The hybrid external fixator combines the versatility and modularity of the Ilizarov frame with the compactness of the monolateral fixator.
Humeral lengthening in achondroplasia is indicated when the lower extremities have been lengthened extensively in order to improve stature and proportion, with increased self-esteem of the patients. In other cases, humeral lengthening has been done when there was upper limb length discrepancy of ≥ 5 cm, giving a cosmetic problem (Lee et al. Citation2005), but recent reports indicate that in patients with highly demanding activities such as sports and playing of musical instruments, lengthening can be considered for even lower degrees of discrepancy (McLawhorn et al. Citation2011).
Traditionally, humeral lengthening has been done using circular external fixators. Cattaneo et al. (Citation1990) lengthened 29 patients with various etiologies; 14 had achondroplasia with a mean gain in length of 9 cm and a mean duration of treatment of 8 months. Kashiwagi et al. (Citation2001) performed bilateral lengthening in 10 achondroplasia patients using Ilizarov circular rings, with a mean gain in length of 8 cm and a mean healing index of 30 days/cm. Our results are comparable to these results. However, it is cumbersome to apply Ilizarov frames bilaterally in the small arms of achondroplasia patients. The monolateral fixator is easy to apply and is less cumbersome, and patients can perform their daily activities with the external fixator (Figure 4). Shadi and Koczewski (Citation2007) treated 5 patients with achondroplasia using monolateral fixators and achieved more than 50% of the primary segmental length.
Complications using monolateral fixators in humeral lengthening are less than for other long bones (Tanaka et al. Citation1998, Hosny Citation2005, Shadi and Koczewski Citation2007, Kim et al. Citation2012). Also, when compared with other lengthening devices, the complication rates appear to be lower with monolateral fixators. The incidence of pin tract infection and elbow flexion contracture in the series of Kashiwagi et al. (Citation2001) was almost double that in our series. Kashiwagi et al. used transosseous wires that pass through muscles—which may cause pain and difficulty in dressing, with increased risk of infection. Also, elbow stiffness may occur because of pain during motion, impeding physiotherapy.
A serious complication is refracture and angulation deformities after excessive lengthening. However, the incidence is less than with lengthening in lower limbs (Kim et al. Citation2012). We had 3 refractures (of 40) in the newly generated bone after removal of the fixator. The risk of refracture can be minimized by analyzing the regenerate during healing. If there is a concave, lateral, or central type of callus in regenerate bone, temporary cessation of distraction and gradual compression is recommended. Timing of the removal of a fixator is very crucial; we have previously reported that PVR is a reliable method of showing corticalization (Singh et al. Citation2010). In all the refractures that we analyzed retrospectively, PVR was < 1 although radiographs showed adequate bridging of the bone. None of the previous reports have mentioned the incidence of varus angulation after lengthening of the humeri, which occurred in 3 out of 40 segments in our patients.
The healing index of humerus is lower than that in the bones of the lower extremity, and we have observed that functional recovery is much faster in upper limbs than in lower limbs. Tanaka et al. (Citation1998) reported that the humerus showed faster bony reconstruction than the tibia .The healing index in our series was 28 days, which is comparable to that in other series.
Patient age at lengthening using monolateral fixator was 12–14 years. At this age, soft tissues are elastic and osteogenic potential is good. Lee et al. (Citation2005) recommended that if lengthening of more than about 10 cm is needed, it should be done in 2 stages. We also agree with their suggestions. However, in some of our patients we have lengthened by approximately 10–11 cm without any complications. So the decision could be discussed with the patients and their parents if a massive amount of lengthening was needed.
In conclusion, hybrid monolateral fixators can be used as a modality for lengthening and deformity correction in various pathologies of the humerus. The assembly is less cumbersome than with circular fixators, and patients can carry out their daily activities with the fixator in place. Our patients reported improved performance in daily activities and improved self-image.
RM: literature review, implementation, manuscript preparation, and editing. HRS: Study design, literature review, manuscript preparation, and editing. KWP: implementation, manuscript preparation, and editing. SHS: study design, data analysis, and implementation. HNK: collection of data and manuscript preparation.
This study was supported by a grant from the Korea Healthcare Technology R&D Project of the Ministry of Health, Welfare, and Family Affairs, Republic of Korea (A110416).
No competing interests declared.
- Cai G, Yang L, Saleh M, Coulton L. The effect of tibial diaphyseal lengthening on the longitudinal growth of the tibia. J Pediatr Orthop B 2007; 16: 403-7.
- Cattaneo R, Villa A, Catagni MA, Bell D. Lengthening of the humerus using the Ilizarov technique. Description of the method and report of 43 cases. Clin Orthop 1990; (250): 117-24.
- Devmurari KN, Song HR, Modi HN, Venkatesh KP, Ju KS, Song SH. Callus features of regenerate fracture cases in femoral lengthening in achondroplasia. Skeletal Radiol 2010; 39: 897-903.
- Dick HM, Tietjen R. Humeral lengthening for septic neonatal growth arrest. Case report. J Bone Joint Surg (Am) 1978; 60: 1138-9.
- Hosny GA. Unilateral humeral lengthening in children and adolescents. J Pediatr Orthop B 2005; 14: 439-43.
- Kashiwagi N, Suzuki S, Seto Y, Futami T. Bilateral humeral lengthening in achondroplasia. Clin Orthop 2001; (391): 251-7.
- Katz K, Goldberg I, Bahar A, Yosipovitch Z. Humeral lengthening for septic neonatal growth arrest. J Hand Surg Am 1989; 14: 903-7.
- Kim SJ, Agashe MV, Song SH, Choi HJ, Lee H, Song HR. Comparison between upper and lower limb lengthening in patients with achondroplasia: a retrospective study. J Bone Joint Surg (Br) 2012; 94: 128-33.
- Kiss S, Pap K, Vizkelety T, Terebessy T, Balla M, Szoke G. The humerus is the best place for bone lengthening. Int Orthop 2008; 32: 385-8.
- Lee FY, Schoeb JS, Yu J, Christiansen BD, Dick HM. Operative lengthening of the humerus: indications, benefits, and complications. J Pediatr Orthop 2005; 25: 613-6.
- Li R, Saleh M, Yang L, Coulton L. Radiographic classification of osteogenesis during bone distraction. J Orthop Res 2006; 24: 339-47.
- McLawhorn AS, Sherman SL, Blyakher A, Widmann RF. Humeral lengthening and deformity correction with the multiaxial correction system. J Pediatr Orthop B 2011; 20: 111-6.
- Paley D. Current techniques of limb lengthening. J Pediatr Orthop 1988; 8: 73-92.
- Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop 1990; (250): 81-104.
- Paley D, Herzenberg JE, Paremain G, Bhave A. Femoral lengthening over an intramedullary nail. A matched-case comparison with Ilizarov femoral lengthening. J Bone Joint Surg (Am) 1997; 79: 1464-80.
- Shadi M, Koczewski P. Humeral lengthening with a monolateral external fixator in achondroplasia. Pediatr Endocrinol Diabetes Metab 2007; 13: 121-4.
- Singh S, Song HR, Venkatesh KP, Modi HN, Park MS, Jang KM, et al.. Analysis of callus pattern of tibia lengthening in achondroplasia and a novel method of regeneration assessment using pixel values. Skeletal Radiol 2010; 39: 261-6.
- Tanaka K, Nakamura K, Matsushita T, Horinaka S, Kusaba I, Kurokawa T. Callus formation in the humerus compared with the femur and tibia during limb lengthening. Arch Orthop Trauma Surg 1998; 117: 262-4.
- Tetsworth K, Krome J, Paley D. Lengthening and deformity correction of the upper extremity by the Ilizarov technique. Orthop Clin North Am 1991; 22: 689-713.
