Abstract
Background and purpose Type-II distal clavicle fractures according to the Neer classification are generally operated because of the high non-union rate after non-operative treatment. Several surgical techniques have been developed in order to reduce the non-union rate and improve functional outcome. This meta-analysis overviews the available surgical techniques for type-II distal clavicular fractures.
Methods We searched the literature systematically. No comparative studies were found. 21 studies (8 prospective and 13 retrospective cohort studies) were selected for the meta-analysis. Data were pooled for 5 surgical outcome measures: function, time to union, time to implant removal, major complications, and minor complications.
Results The 21 studies selected included 350 patients with a distal clavicular fracture. Union was achieved in 98% of the patients. Functional outcome was similar between the treatment modalities. Hook-plate fixation was associated with an 11-fold increased risk of major complications compared to intramedullary fixation and a 24-fold increased risk compared to suture anchoring.
Interpretation If surgical treatment of a distal clavicle fracture is considered, a fixation procedure with a low risk of complications and a high union rate such as plate fixation or intramedullary fixation should be used. The hook-plate fixation had an increased risk of implant-related complications.
Neer type-II fractures of the distal clavicle are unstable fractures in which the clavicle becomes separated from the underlying coracoclavicular (CC) ligament complex without damage to the most distal end of the clavicle and the acromioclavicular joint (AC joint) (Neer Citation1968). These fractures are known to have a high percentage of non-union and malunion after non-operative treatment (> 20%) (CitationNordqvist et al. 1997, Robinson and Cairns Citation2004). Neer has already recommended that these types of fractures should be treated operatively in order to reduce the non-union rate (Neer Citation1968). The distal clavicle may be osteosynthesised by a hook-plate or locking-plate fixation, double-plate fixation, transacromial fixation using Kirschner wires, cerclage wiring of the fragments, tension-band wiring, or stabilization of the medial fragment with coracoclavicular screws or slings. Hardware is usually removed after 8–12 weeks when the fracture is radiographically and clinically healed to prevent acromial osteolysis or other plate-induced complications (Bisbinas et al. Citation2010). None of the fixation techniques described has been nominated the “gold standard”; each of these treatment modalities has its advantages and disadvantages.
This study was a meta-analysis to compare functional outcome, union rates, and complications between the surgical treatment strategies for Neer type-II clavicular fractures.
Material and methods
The meta-analysis was performed following the guidelines set by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Liberati et al. Citation2009).
Search strategy
A systematic literature search was performed in PubMed, EMBASE, and Web of Science. The search included key words for fracture, clavicle, or collar bone, and lateral or distal (Table 1, see Supplementary data). The selection was not restricted regarding treatment modality, study design, publication language, or year of publication. Duplicate articles were removed.
Eligibility criteria and study selection
The title and abstract of all articles were screened to select articles on surgical treatment of distal clavicle fractures in human subjects. Subsequently, the full-text articles of the selected abstracts were retrieved for detailed evaluation. All studies that assessed surgical treatment of adult patients with acute Neer type-II distal clavicle fractures and that provided quantitative data on patient characteristics, surgical intervention, outcomes, and complications were included in the final selection. We excluded studies including only minors (< 16 years), studies including only patients with delayed union or non-union, studies including acromioclavicular joint injuries (type-III Neer classification), studies dealing with midshaft or medial clavicle fractures, studies without any data on surgical intervention and/or treatment outcomes, reviews, case series with less than 5 patients, technical reports, and expert opinions (level of evidence V). If selected studies included both eligible and non-eligible patients, these studies were only included if the data of the eligible patients could be extracted from the article. The reference lists of the articles were screened for potentially relevant studies that had not been found by the initial literature search. Study selection and data extraction were carried out by 2 independent reviewers (SAS and HN). Disagreement was resolved by consensus.
Types of outcome measures
We compared 4 types of surgical treatment (hook-plate fixation, other types of plate fixation, intramedullary fixation with pins/screws, and suture anchoring/tension bands) with respect to 5 outcome variables: function as measured by the Constant score, time to union in weeks, time to implant removal in weeks, and complications (major and minor complications separately). Union was assessed on the radiograph at the last follow-up visit.
Assessment of study quality
2 reviewers (SAS, HN) independently assessed the methodological quality of each selected study by classifying the study design, and the level of evidence using the scale introduced by Wright et al. (Citation2003).
Data extraction
Data were extracted from each study using a data-extraction form. The following data were documented from each study: study characteristics (country, period), patient numbers (inclusion, follow-up), patient characteristics (age, sex, and fracture type), duration of follow-up, type of surgical intervention, and outcome measures (number of unions, time to achieve union, time to implant removal, major complications, and minor complications). For continuous outcome parameters, means and standard deviations were extracted. In cases where mean outcome measures were reported without any standard deviation, the standard deviation was estimated as range (maximum – minimum) / 4. For dichotomous outcome parameters, proportions and sample size were extracted.
Pooling of data across studies
Separate meta-analyses were performed for the 5 outcome measures: functional outcome (measured with the Constant score), time to union in weeks, time to implant removal in weeks, and major and minor complications. Complications were classified as major (reoperation, implant failure, refracture, acromial osteolysis, pseudarthrosis, and signs of impingement) or minor (wound infection and skin irritation).
Data analysis
For continuous outcome data (Constant score, time to union, time to implant removal), the standard random-effects meta-regression model ( van Houwelingen et al. Citation2002), with the surgical treatment as a categorical covariate represented by 3 dummy variables, was used to estimate the mean differences in outcome between the surgical treatments with the corresponding 95% confidence intervals (CIs). Heterogeneity between studies was modeled by a random study effect. For dichotomous outcomes (major and minor complications) the ORs and corresponding CIs were calculated using a logistic regression model with a random intercept to account for heterogeneity between studies (Stijnen et al. Citation2010). Heterogeneity between studies was tested by comparing a model with and without the random study effect using the likelihood ratio test. To test differences between treatments, first an overall test was performed. If the overall test resulted in a small p-value (< 0.1), differences were tested pairwise. All analyses were performed using SAS/STAT statistical software. Any p-values < 0.05 were considered to be statistically significant.
Results
Study selection
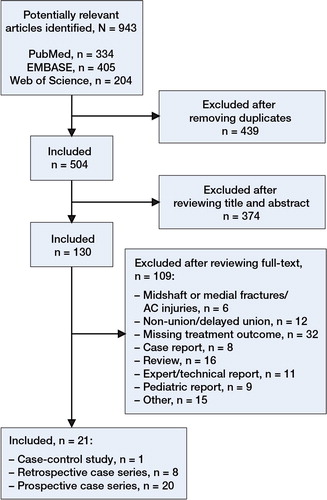
In the initial search, we identified 943 abstracts (). After removing duplicates, 504 articles remained. We selected 130 articles for detailed evaluation based on content after reading the titles and abstracts. Of these 130 articles, 21 remained after applying the inclusion and exclusion criteria (Webber and Haines Citation2000, Othman Citation2002, Rokito et al. Citation2002, Fann et al. Citation2004, Bezer et al. Citation2005, Scadden and Richards Citation2005, Bhangal et al. Citation2006, Kashii et al. Citation2006, Meda et al. Citation2006, Badhe et al. Citation2007, Fazal et al. Citation2007, Muramatsu et al. Citation2007, Kalamaras et al. Citation2008, Wang and Wong Citation2008, Herrmann et al. Citation2009, Renger et al. Citation2009, Shin et al. Citation2009, Yu et al. Citation2009, Jou et al. Citation2011, Kaipel et al. Citation2010, Lee et al. Citation2010). No randomized or non-randomized controlled trials comparing surgical modalities for distal clavicle fractures were found. Of the 21 studies finally selected, only 1 was a retrospective case-control (level-III) study comparing non-operative treatment to open reduction with coracoclavicular stabilization with suture bands, whereas all other 20 articles were prospective or retrospective case series (level-IV).
Study characteristics
All articles included were published in English. 8 studies were conducted in Asia, 11 in Europe, 1 study in North America, and 1 study in Australia (Table 2, see Supplementary data). The surgical procedures described in the studies were performed between 1989 and 2007. In total, 405 patients with a distal clavicle fracture were included in the 21 selected studies. Excluded from the analysis were 13 patients with non-union at inclusion in the study (Meda et al. Citation2006, Kalamaras et al. Citation2008, Kaipel et al. Citation2010), 16 patients with non-operative treatment, 7 patients with a Neer type-III fracture (Meda et al. Citation2006), 17 patients who were lost to follow-up, and 2 minors (Webber and Haines Citation2000, Kalamaras et al. Citation2008, Jou et al. Citation2011), leaving the data on 350 patients for analysis. The mean number of patients with a complete follow-up was 17 (6–44) per study. Fracture fixation was performed using hook plates in 143 patients (Bhangal et al. Citation2006, Kashii et al. Citation2006, Meda et al. Citation2006, Muramatsu et al. Citation2007, Renger et al. Citation2009, Lee et al. Citation2010) (Table 2A, see Supplementary data). In the group using different types of plate fixation, distal radial locking plates were used in 20 patients (Kalamaras et al. Citation2008, Herrmann et al. Citation2009, Yu et al. Citation2009) and double plates in 9 patients (Kaipel et al. Citation2010) (Table 2B, see Supplementary data). As intramedullary fixation, Knowles pins were used in 68 patients (Fann et al. Citation2004, Wang and Wong Citation2008, Jou et al. Citation2011), coracoclavicular screws in 30 patients (Fazal et al. Citation2007), and malleolar screws in 10 patients (Scadden and Richards Citation2005) (Table 2C, see Supplementary data). For the group with suture anchoring or tension bands, K-wires with suture anchoring were used in 10 patients (Bezer et al. Citation2005), tension-band suturing in 43 patients (Rokito et al. Citation2002, Badhe et al. Citation2007, Shin et al. Citation2009), vicryl tape in 6 patients (Othman Citation2002), and a Dacron arterial graft in 11 patients (Webber and Haines Citation2000) (Table 2D, see Supplementary data). The studies included 238 men and 101 women and mean age was 38 (17–86) years at the time of trauma. In 1 study, sex ratio was not reported (n = 11) (Bhangal et al. Citation2006).
Study quality
None of the 21 articles included pertained to a randomized controlled trial (RCT). One retrospective case-control study (Rokito et al. Citation2002) was identified, comparing suture bands with non-operative treatment, and only the surgically treated patients were included in the present meta-analysis. All other studies were prospective (n = 8) or retrospective case series (n = 12) (Webber and Haines Citation2000, Othman Citation2002, Fann et al. Citation2004, Bezer et al. Citation2005, Scadden and Richards Citation2005, Bhangal et al. Citation2006, Kashii et al. Citation2006, Meda et al. Citation2006, Badhe et al. Citation2007, Fazal et al. Citation2007, Muramatsu et al. Citation2007, Kalamaras et al. Citation2008, Wang and Wong Citation2008, Herrmann et al. Citation2009, Renger et al. Citation2009, Shin et al. Citation2009, Yu et al. Citation2009, Jou et al. Citation2011, Kaipel et al. Citation2010, Lee et al. Citation2010). The primary outcome in all studies was the incidence of union and non-union, as determined on radiographs or by clinical evaluation (withstanding pressure on fracture side without pain). Evaluation of the outcome was not done blind in any of the studies.
Assessment of study quality
The studies included differed regarding the timing of radiography, type of surgical treatment, duration, and follow-up occasions. Loss to follow-up occurred in 7 studies (Fann et al. Citation2004, Bezer et al. Citation2005, Bhangal et al. Citation2006, Kalamaras et al. Citation2008, Herrmann et al. Citation2009, Renger et al. Citation2009, Kaipel et al. Citation2010). None of the researchers were blinded regarding evaluation of the radiograph, or regarding functional outcome. No inconsistency was found in percentage union and functional outcome across the surgical methods. No differences in the directness were expected in effect sizes across the studies, and the study population, interventions, and outcome measures in each study were comparable. Functional outcome was measured using the Constant score in 16 of the studies, the UCLA score in 2 studies, the Oxford Shoulder Score in 1 study, the simple shoulder test questionnaire in 1 study, and the Japanese Orthopaedic Association score in 1 study. Since the results of these instruments could not be compared directly, only the studies using the Constant score or those that could be converted to a percentage score were included in the analysis of functional outcome. There appeared to be a relationship between age and risk of major complications. However, no confounders were identified to influence the outcomes of each study, because the data did not allow it.
Treatment outcomes
Function. Function according to the Constant score was similar after hook-plate fixation and after the other surgical approaches in general (p = 0.9) (). All patients had good to excellent scores in the tests for functional outcome at final follow-up. Heterogeneity between studies was highly significant (p < 0.001).
Figure 2. Mean differences in Constant scores, weeks to union, and weeks to implant removal for plate fixation, pins, and sutures compared to hook-plate fixation. Df: degrees of freedom.
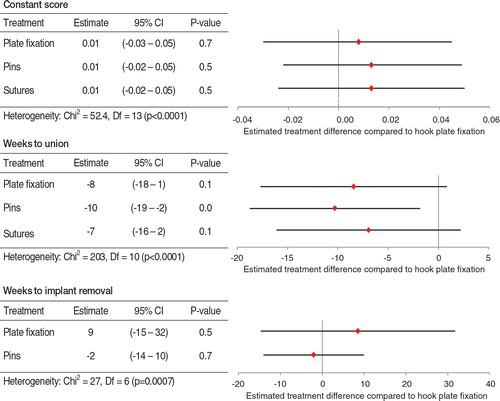
Union. Overall union was achieved in 342 of 350 patients (98%). Of the 21 studies, 16 reported a union rate of 100%. The average time to union ranged from less than 6 weeks to more than 33 weeks (Table 2, see Supplementary data). 8 of 350 patients (2%) developed non-union (n = 6) or delayed union (n = 2). Of those, 3 patients had been treated with a hook plate, 2 with intramedullary fixation, and 3 with sutures. The 2 delayed unions achieved union after 9 and 10 months. No non-unions were found in the plate-fixation group. There was a tendency to significant differences in time to fracture union between treatments (overall p = 0.08). After hook-plate fixation, it took on average 10 weeks longer to obtain fracture union than with pin fixation (p = 0.02) (). Time to union after hook-plate fixation was not statistically significantly different to that after plate fixation and suture fixation, although there was a longer consolidation period after hook-plate fixation (p = 0.07; p = 0.1). The heterogeneity between studies was highly significant (p < 0.001).
Implant removal. The occurrence of implant removal after hook-plate fixation was compared to that after plate fixation and intramedullary fixation. In some studies, implant removal was standard practice for prevention of skin irritation or pin/screw protrusion after bony union had been achieved (Fann et al. Citation2004, Bezer et al. Citation2005, Scadden and Richards Citation2005, Bhangal et al. Citation2006, Kashii et al. Citation2006, Fazal et al. Citation2007, Wang and Wong Citation2008, Renger et al. Citation2009, Jou et al. Citation2011, Lee et al. Citation2010). In 5 other studies, the implant was only removed if major complications occurred (Webber and Haines Citation2000, Meda et al. Citation2006, Muramatsu et al. Citation2007, Herrmann et al. Citation2009, Kaipel et al. Citation2010). In the studies reporting on sutures and tension bands, patients did not require a second operation for removal of the implants (Othman Citation2002, Rokito et al. Citation2002, Badhe et al. Citation2007, Kalamaras et al. Citation2008, Shin et al. Citation2009, Yu et al. Citation2009). No statistically significant difference was found when comparing treatment for weeks to implant removal (p = 0.7). On average, intramedullary fixation was removed earlier (–2 weeks) than hook-plate fixation, whereas plate fixation was left in situ longer (8.6 weeks) (). Heterogeneity between studies was highly significant (p < 0.001).
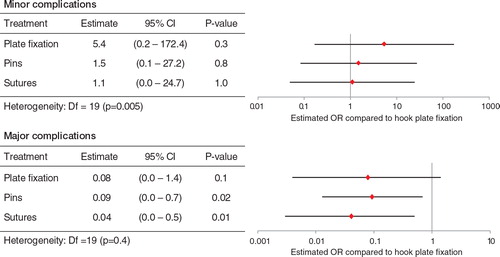
Complications. In all but 4 studies, complications of treatment were observed (Othman Citation2002, Scadden and Richards Citation2005, Badhe et al. Citation2007, Yu et al. Citation2009). Some complications, such as pin or screw migration, led to a second operation. Regarding minor complications, no differences were found between the treatment modalities (p = 0.9) (). In contrast, the overall test for differences in the incidence of major complications was statistically significant (p = 0.01). Acromial osteolysis, refracture, and implant failure occurred 11 times more frequently after hook-plate fixation than after intramedullary fixation (p = 0.02) and 24 times more frequently after suturing (p = 0.01) (). The number of major complications after plate fixation was not significantly different from that after hook-plate fixation (p = 0.08). For both complication variables, significant heterogeneity between studies was found.
Discussion
There is little evidence available for the preferred operative treatment of distal clavicle fractures regarding radiographic union, function, and complications associated with the treatment. In general and independent of the type of fixation, in our meta-analysis we found union rates of over 90% after operative treatment of distal clavicle fractures. The function outcomes ranged from good to excellent; all patients regained full functional range of motion. Both union rate and functional outcome were not significantly different with hook-plate fixation, plate fixation, pins, or sutures. Time to union, however, was shortest after fixation with pins and longest after hook-plate fixation, with only pins showing a statistically significantly shorter time to union than with hook-plate fixation. Weeks to implant removal were not significantly different between the surgical treatment modalities. Hook-plate fixation was associated with a higher risk of major complications such as reoperation and implant failure, compared to intramedullary fixation and sutures.
One systematic review of type-II distal clavicle fractures, identifying union and complication rates according to the different treatment methods, has been published previously (Oh et al. Citation2011). These authors found a non-union rate of 33% for non-operative treatment, but with similar functional scores as for the surgically treated groups in most of the studies. The authors noted that the functional outcome after non-operative treatment remained controversial, and that a well-designed RCT was therefore needed. We did not include non-operative treatment in our analysis, because only a very small number of non-operatively treated patients were analyzed in one of the comparative studies (Rokito et al. Citation2002) and no other eligible studies with non-operatively treated patients were identified. In accordance with our results, Oh et al. (Citation2011) found similar satisfactory functional outcome results for all surgical modalities. The decision for surgical treatment should not be based on functional outcomes, because despite the high percentages of non-union, no similar function was found for non-operative or surgical treatment (Oh et al. Citation2011). The complication rate for the non-operatively treated patients was, however, low compared to that for the surgical group, again despite the high non-union rate (Rokito et al. Citation2002, Oh et al. Citation2011). Non-operative treatment has been considered by some authors to be a treatment for Neer type-II fractures (Deafenbaugh et al. Citation1990, Nordqvist et al. Citation1993, Robinson and Cairns Citation2004), but these data were not compared to an operative method.
The data we present in this meta-analysis are clinically relevant. Hook-plate fixation is the most frequently used method for fixating type-II clavicular fractures. However, although the performance of the hook plate is comparable to that for other surgical types of fixation, its complication rate is higher and the fracture healing takes longer than for intramedullary fixation. When choosing which method to use for fixation of a type-II clavicular fracture, the benefit to the patient is the first priority. This is mostly associated with optimal functional outcome and a low complication risk. Merely due to the relatively high complication risk, hook-plate fixation is therefore not the method of choice and its use should be reserved for very specific indications, e.g. when no alternative adequate methods are available and the operation can be performed by a surgeon who has extensive experience with hook-plate fixation.
Limitations
Several studies (Fann et al. Citation2004, Bezer et al. Citation2005, Bhangal et al. Citation2006, Kalamaras et al. Citation2008, Herrmann et al. Citation2009, Renger et al. Citation2009, Kaipel et al. Citation2010) suffered from loss to follow-up for different reasons, which led to incomplete data on functional outcome and union and possibly gave rise to bias in cases of selective dropout. The sample sizes in these studies became relatively small, thus contributing to a relatively small total sample size in this meta-analysis and possibly leading to a lack of power.
The level of evidence in the studies was low and heterogeneity of the outcome parameters was high. Heterogeneity was accounted for by using random-effects modeling. The definition, by which non-union was confirmed, was not uniform across studies, which may affect union rates to a lesser extent. Functional outcomes were defined using different methods, and they were therefore difficult to compare. This was solved by selecting only the studies that provided Constant scores—or those convertible to percentages comparable with the Constant score—for data analysis. Heterogeneity between the studies was high. In this meta-analysis, we applied correction for heterogeneity. A well-designed RCT comparing operative treatment and non-operative treatment or another operative method should bypass these kinds of flaws.
In conclusion, if surgical treatment of a distal clavicle fracture is indicated, a fixation procedure with a low risk of complications and a high union rate should be used. The number and severity of hook plate-related complications seems to disqualify this implant. However, due to the limited quality of the studies included and the relatively small number of patients involved, no definite conclusion can be drawn regarding the most preferred treatment. Evidence from RCTs is lacking.
www.actaorthop.org
Download PDF (40.1 KB)SAS, HN, PK, and IS designed the study protocol. SAS and HN selected the articles and gathered the data. Statistical analysis was performed by KHJH and TS. All the authors contributed to writing and presentation of the manuscript.
No competing interests declared.
- Badhe SP, Lawrence TM, Clark DI. Tension band suturing for the treatment of displaced type 2 lateral end clavicle fractures. Arch Orthop Trauma Surg 2007; 127 (1): 25-8.
- Bezer M, Aydin N, Guven O. The treatment of distal clavicle fractures with coracoclavicular ligament disruption: a report of 10 cases. J Orthop Trauma 2005; 19 (8): 524-8.
- Bhangal KK, Evans SC, Gibbons CE. Treatment of displaced lateral clavicle fractures with the AO hook plate. European Journal of Trauma 2006; 32 (5): 468-70.
- Bisbinas I, Mikalef P, Gigis I, Beslikas T, Panou N, Christoforidis I. Management of distal clavicle fractures. Acta Orthop Belg 2010; 76 (2): 145-9.
- Deafenbaugh MK, Dugdale TW, Staeheli JW, Nielsen R. Nonoperative treatment of Neer type II distal clavicle fractures: a prospective study. Contemp Orthop 1990; 20 (4): 405-13.
- Fann CY, Chiu FY, Chuang TY, Chen CM, Chen TH. Transacromial Knowles pin in the treatment of Neer type 2 distal clavicle fracturesA prospective evaluation of 32 cases. J Trauma 2004; 56 (5): 1102-5.
- Fazal MA, Saksena J, Haddad FS. Temporary coracoclavicular screw fixation for displaced distal clavicle fractures. J Orthop Surg (Hong Kong) 2007; 15 (1): 9-11.
- Herrmann S, Schmidmaier G, Greiner S. Stabilisation of vertical unstable distal clavicular fractures (Neer 2b) using locking T-plates and suture anchors. Injury 2009; 4 (3): 236-9.
- Jou IM, Chiang EP, Lin CJ, Lin CL, Wang PH, Su WR. Treatment of unstable distal clavicle fractures with Knowles pin. J Shoulder Elbow Surg 2011; 20 (3): 414-9.
- Kaipel M, Majewski M, Regazzoni P. Double-plate fixation in lateral clavicle fractures-a new strategy. J Trauma 2010; 69 (4): 896-900.
- Kalamaras M, Cutbush K, Robinson M. A method for internal fixation of unstable distal clavicle fractures: early observations using a new technique. J Shoulder Elbow Surg 2008; 17 (1): 60-2.
- Kashii M, Inui H, Yamamoto K. Surgical treatment of distal clavicle fractures using the clavicular hook plate. Clin Orthop 2006; (447): 158-64.
- Lee KW, Lee SK, Kim KJ, Kim YI, Kwon WC, Choy WS. Arthroscopic-assisted locking compression plate clavicular hook fixation for unstable fractures of the lateral end of the clavicle: a prospective study. Int Orthop 2010; 34 (6): 839-45.
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med 2009; 151 (4): W65-W94.
- Meda PV, Machani B, Sinopidis C, Braithwaite I, Brownson P, Frostick SP. Clavicular hook plate for lateral end fractures:– a prospective study. Injury 2006; 37 (3): 277-83.
- Muramatsu K, Shigetomi M, Matsunaga T, Murata Y, Taguchi T. Use of the AO hook-plate for treatment of unstable fractures of the distal clavicle. Arch Orthop Trauma Surg 2007; 127 (3): 191-4.
- Neer CS. Fractures of the distal third of the clavicle. Clin Orthop 1968; (58): 43-50.
- Nordqvist A, Petersson C, Redlund-Johnell I. The natural course of lateral clavicle fracture. 15 (11-21) year follow-up of 110 cases. Acta Orthop Scand 1993; 64 (1): 87-91.
- Nordqvist A, Redlund-Johnell I, von SA, Petersson CJ. Shortening of clavicle after fracture. Incidence and clinical significance, a 5-year follow-up of 85 patients. Acta Orthop Scand 1997; 68 (4): 349-51.
- Oh JH, Kim SH, Lee JH, Shin SH, Gong HS. Treatment of distal clavicle fracture: a systematic review of treatment modalities in 425 fractures. Arch Orthop Trauma Surg 2011; 131 (4): 525-33.
- Othman AY. Internal fixation of lateral clavicle fractures with vicryl tape. European Journal of Orthopaedic Surgery and Traumatology 2002; 12 (3): 129-31.
- Renger RJ, Roukema GR, Reurings JC, Raams PM, Font J, Verleisdonk EJ. The clavicle hook plate for Neer type II lateral clavicle fractures. J Orthop Trauma 2009; 23 (8): 570-4.
- Robinson CM, Cairns DA. Primary nonoperative treatment of displaced lateral fractures of the clavicle. J Bone Joint Surg (Am) 2004; 86 (4): 778-82.
- Rokito AS, Zuckerman JD, Shaari JM, Eisenberg DP, Cuomo F, Gallagher MA. A comparison of nonoperative and operative treatment of type II distal clavicle fractures. Bull Hosp Jt Dis 2002; 61 (1-2): 32-9.
- Scadden JE, Richards R. Intramedullary fixation of Neer type 2 fractures of the distal clavicle with an AO/ASIF screw. Injury 2005; 36 (10): 1172-5.
- Shin SJ, Roh KJ, Kim JO, Sohn HS. Treatment of unstable distal clavicle fractures using two suture anchors and suture tension bands. Injury 2009; 40 (12): 1308-12.
- Stijnen T, Hamza TH, Ozdemir P. Random effects meta-analysis of event outcome in the framework of the generalized linear mixed model with applications in sparse data. Stat Med 2010; 29 (29): 3046-67.
- van Houwelingen HC, Arends LR, Stijnen T. Advanced methods in meta-analysis: multivariate approach and meta-regression. Stat Med 2002; 21 (4): 589-624.
- Wang SJ, Wong CS. Extra-articular knowles pin fixation for unstable distal clavicle fractures. J Trauma 2008; 64 (6): 1522-7.
- Webber MC, Haines JF. The treatment of lateral clavicle fractures. Injury 2000; 31 (3): 175-9.
- Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg (Am) 2003; 85 (1): 1-3.
- Yu C, Sun YH, Zhao CQ, Shi DW, Wang Y. Treatment of distal clavicle fracture with distal radius volar locking compression plate. Chin J Traumatol 2009; 12 (5): 299-301.