Abstract
Background and purpose — The aim of short-stem total hip arthroplasty is to preserve proximal bone stock for future revisions, to improve biomechanical reconstruction, and to make minimally invasive approaches easier. It is therefore being increasingly considered to be a sound alternative to conventional total hip arthroplasty, especially for young and active patients. However, it is still unknown whether survival rates of short-stem hips match current standards. We made a systematic summary of reported overall survival after short-stem total hip arthroplasty.
Materials and methods — We conducted a systematic review of English, French, German, and Dutch literature. 2 assessors independently identified clinical studies on short-stem hip arthroplasty. After recalculating reported revision rates, we determined whether each implant had a projected revision rate of 10% or less at 10 years of follow-up or a revision rate per 100 observed component years of 1 or less. Stems were classified as “collum”, “partial collum”, or “trochanter-sparing”.
Results and Interpretation — We found 49 studies, or 51 cohorts, involving 19 different stems. There was a large increase in recent publications. The majority of studies included had a follow-up of less than 5 years. We found a large number of observational studies on “partial collum” and “trochanter-sparing” stems, demonstrating adequate survival rates at medium-term follow-up. Clinical evidence from “collum stem” studies was limited to a small number of studies with a medium-term follow-up period. These studies did not show a satisfactory overall survival rate.
In recent years, there has been an increase in uncemented total hip arthroplasty in young and more active patients (Adelani et al. Citation2013). The diaphyseal or metadiaphyseal anchorage features of uncemented stems may, however, cause proximal stress shielding. Concern about potential metaphyseal bone loss during future revision—especially in younger patients—has led to the quest for a more bone-preserving implant. Short-stemmed implants were introduced with the aim of preserving proximal bone stock for future revisions by preventing stress shielding through metaphysical bone loading. Furthermore, by following the anatomic curvature of the femoral neck, short stems may restore biomechanical proportions better than conventional stems, and tissue-sparing minimally invasive approaches may be easier with small curved stems.
Current total hip arthroplasty stems can be roughly divided into the following anchoring principles (Gulow et al. Citation2007): (1) Resurfacing endoprostheses anchoring on the epiphysis; (2) Collum endoprostheses solely anchoring on the metaphysis; (3) Short collum preserving stems anchoring on the metaphysis with short anchorage on the diaphysis; and (4) Conventional stems anchoring on the metaphysis with a long diaphyseal anchorage.
Collum endoprostheses and short stems may be combined with conventional cups and bearings, in contrast to resurfacing designs. They are increasingly being considered to be a sound alternative, especially for young and active patients. However, it is still unknown whether survival rates of short hip stems are comparable with conventional uncemented stems. With a growing number of short-stem implants being introduced to the market, we wanted to summarize in a systematic way the reported overall survival after short-stem total hip arthroplasty and to compare the survival with the current benchmark level for conventional total hip arthroplasty.
Material and methods
Inclusion criteria and study identification
To be included in this review, a study had to meet the following criteria: a clinical study publishing the complications or revision rates of short-stem total hip arthroplasty with a minimum of 3 months of follow-up.
We classified the stems that were included into the following categories (Lombardi et al. Citation2009, Jerosch 2013): (1) “collum”; conical or cylindrical ultra-short stems, with complete anchorage in the femoral neck; (2) “partial collum”; partial femoral neck-sparing curved designs; and (3) “trochanter-sparing”: trochanter-sparing but not neck-sparing, and shortened tapered stem.
Alternative extramedullary anchorage systems such as the thrust-plate prosthesis were excluded. We included randomized controlled trials, prospective and retrospective comparative studies, and observational case series (n > 1). The Medline electronic database was searched for relevant trials indexed between January 1, 1989, and January 1, 2013, limited to the English, French, German, and Dutch languages. A medical librarian was consulted to construct an appropriate search strategy. The search strategy included general short-stem total hip arthroplasty as well as more specific terms directed at specific short stems. This resulted in the following search strategy: (((femur OR femoral) AND (collum OR neck) AND (conserv* OR preserv* OR sparing OR spare*))) OR (cut type[tiab]) OR (taperloc) OR (short-stem*) OR (proxima[tiab]) OR (tri-lock[tiab]) OR (fitmore[tiab]) OR (mayo[tiab]) OR (metha[tiab]) AND (hip replacement OR hip arthroplasty[tiab]).
2 assessors independently evaluated (in 2 rounds each) the titles, abstracts, and full texts for eligibility. After the second round, remaining discrepancies were resolved by consensus between the 2 reviewers. Finally, 2 separate reviewers searched additional clinical studies by cross-referencing the studies included and by searching the internet and relevant chapters in books for additional clinical reports (Jerosch 2013). After data extraction, again 2 separate assessors confirmed the accuracy of the database by reassessment of all the studies included. Ambiguous data and duplicate publications were excluded.
We used the orthopedic pyramid proposed by Schemitsch et al. (Citation2010) to classify each study according to its level of evidence and development phase The pyramid is a proposal for an evidence-based approach to implant development and assessment of their safety prior to their widespread implementation. As with drug development, the development of orthopedic devices has 4 phases. Phase 1 is a laboratory phase consisting of biomechanical studies, basic science investigations, and expert opinions. This review did not include phase-1 studies. Phase 2 consists of case series and case-control studies. Phase 3 provides comparative evidence through comparative cohort studies. The development of a new device is concluded by randomized clinical trials in phase 4, thereby providing decisive evidence prior to widespread clinical use. Randomized controlled trials were only classified as such if they randomly investigated 2 or more different types of prosthesis. If they investigated other factors, such as the surgical approach, by using identical implants in both groups, the study was classified as a case series.
Outcome measurement
The primary outcome measure was stem revision for any reason as the failure endpoint for the stem, the neck in case of a modular neck system, or both the cup and stem. We recalculated revision rates based on the number of revisions provided in the article. Cup revisions alone were not included in the calculation. We determined whether each implant showed a revision rate consistent with the National Institute of Clinical Excellence (NICE) benchmark of 10% or less at 10 years of follow-up (Dillon 2013). If follow-up was less than 10 years, we determined whether the stem was on target to meet the 10-year benchmark. We calculated the revision per 100 observed component years for each study, stem type, and stem category. This method was previously used by the Quality of Literature in Arthroplasty (QoLA) project, initiated by the EFORT and the European Arthroplasty Registry (EAR), to compare clinical and arthroplasty registry datasets for hips and knees (Labek et al. Citation2011). The formula for the calculation is: number of cases of revision surgery for any reason divided by the number of component years observed and multiplied by 100. The advantage of this method is that it allows comparison of datasets adjusted for the 2 main factors influencing the value of individual cohorts: number of cases and follow-up period. A value of 1 represents a 1% revision rate at 1 year and a 10% revision rate at 10 years. Thus, a value of 1 or less is required to meet the NICE benchmark.
The mean follow-up of each stem category and stem type was calculated relative to the number of patients (n) in each study, as follows: (follow-upstudy A × nstudy A) + (follow-upstudy B × nstudy B) / nstudy A + nstudy B.
We calculated the mean revision rate per 100 observed component years of each stem category and stem type as well as the corresponding standard deviation (σ) and 95% confidence interval (CI) using Microsoft Excel version 14.1.3. When assuming an α of 0.05, the corresponding 95% CI was calculated as: mean ± 1.96 (σ/√n). Where there were inconsistent results, we calculated revision rates and the mean revision rate per 100 observed component years of the group with and without the outlier.
Results
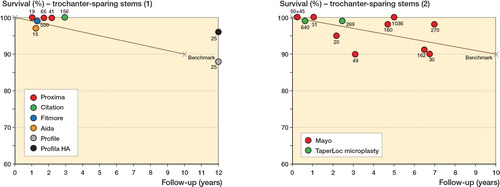
We included 49 studies involving 19 different stem types and 6,495 patients. 2 studies compared 2 different short stems, which for clarity will be presented as individual studies, resulting in a total of 51 individual short-stem cohorts (Hallan et al. Citation2006, Logroscino et al. Citation2011). There were 39 studies with a follow-up period of 5 years or less, 9 studies with a follow-up of between 5 and 10 years, and 3 studies with a follow-up of more than 10 years. 25 studies included 50 patients or less, 9 studies between 50 and 100 patients, 10 studies between 100 and 200 patients, and 7 studies included more than 200 patients. The majority of studies were level-4, phase-2 studies (n = 46). 3 studies were classified as a comparative case series (level-2, phase-3) and 2 studies were classified as randomized clinical trials (RCTs) (level-1, phase-4). We found a large increase in recent short-stem hip publications. While only 12 studies had been published before 2007, 13 studies appeared between 2007 and 2010 and 26 studies appeared between 2010 and 2013. The reported survival rate for each individual study in relation to the number of cases, follow-up period, and the projected deviation from the NICE benchmark of at least 90% survival at 10 years of follow-up is shown graphically in –.
Collum stems
We found 7 collum stem studies, reporting on 3 stem types in 540 patients (). Mean follow-up of collum stems was 4.4 (2.0–6.0) years. The mean follow-up of the CUT (ESKA Implants AG, Lubeck, Germany) was 4.4 (3.1–6.0) years. We only found 2 other collum stem type case series, with the Gothenburg Osseointegrated Titanium Mk. II (GOT) stem and the Spiron stem (K-Implant GmbH, Garbsen, Germany), both with a small number of patients (20 and 34) and a short follow-up period of 2 years. Although the follow-up was short and the sample size small, the GOT stem study reported no stem revisions when compared with a cemented Spectron femoral stem (Smith and Nephew, London, UK) in an RCT (Carlsson et al. Citation2006).
Table 1. Summary of included studies
For collum stems, shows large differences of reported survival of the CUT stem between studies. The mean revision rate per 100 observed component years for collum stems was 2.0 (CI: 1.8–2.2) (). 3 out of 5 CUT studies showed a survival rate below the projected 90% survival at 10 years of follow-up. 1 series with 82 patients had survival as low as 62% (31 revisions) at 6 years of follow-up (Ishaque et al. Citation2009). Both the CUT and the Spiron showed a revision rate per 100 observed component years of > 1. When excluding the outlier with a survival rate of 62% at 6 years of follow-up, the revision rate per 100 observed component years of the CUT stem was 1.6 ().
Figure 1. Reported survival of collum stems by each individual study, follow-up period, and the projected deviation from the NICE benchmark of 90% survival at 10 years of follow-up. The number of included patients is displayed next to each study.
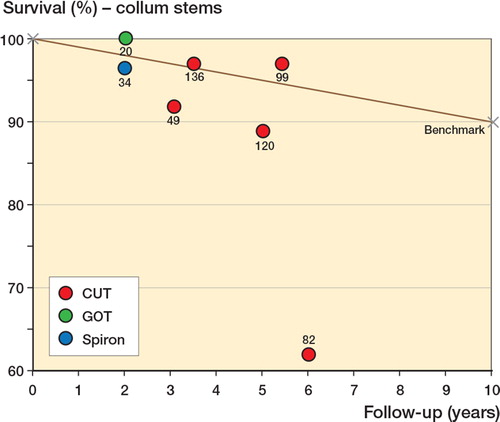
Table 2. Mean revisions per 100 observed component years for each stem category and stem type individually
Partial collum stems
We found 24 partial collum stem studies, reporting on 8 stem types in 2,357 patients (). Mean follow-up was 4.0 (0.5–15) years. The CFP (Waldemar Link GmbH & Co. KG, Hamburg, Germany) had the longest reported mean follow-up of 5.1 (3.0–11) years in 9 studies, and the Optimys (Mathys Medical, Bettlach, Switzerland) had the shortest follow-up of 0.5 years in a single case series. 1 Biodynamic stem study with a follow-up of 15 years was excluded due to ambiguous data (Pipino Citation2000). In this study, only 44 out of the initial 56 consecutive hips were evaluated. Whether the remaining 12 hips were revised or lost to follow-up, or whether the patient had died, is unclear. The Biodynamic stem is no longer available.
panels I and II show a survival rate above the benchmark for most partial collum stems, with a mean revision rate per 100 observed component years of 0.64 (CI: 0.60–0.68) (). However, in a small single case series of 15 patients the Delphi-M (ESKA Implants) showed a survival of 87% after 3.1 years ( panel I and ). In 2009, production of the Dephi-M ceased for economic reasons (Budde et al. Citation2012). There was an Optimys stem revision in a single case series of 63 patients with a short follow-up period of 6 months (Pfeil et al. Citation2013). This stem revision was due to a periprosthetic fracture after a fall by an elderly patient with dementia. This single revision resulted in a revision rate per 100 observed component years of 3.2.
Figure 2. Panels I and II. Reported survival of partial collum stems by each individual study, follow-up period, and the projected deviation from the NICE benchmark of 90% survival at 10 years of follow-up. The number of included patients is displayed next to each study.
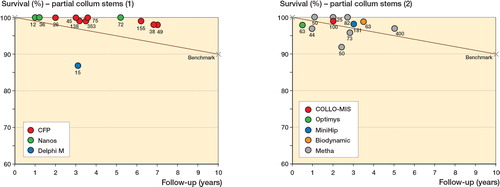
Figure 3. Panels I and II. Reported survival of trochanter-sparing stems by each individual study, follow-up period, and the projected deviation from the NICE benchmark of 90% survival at 10 years of follow-up. The number of included patients is displayed next to each study.
panels I and II show survival rates above the benchmark for the CFP, the Nanos (Smith and Nephew, London, UK), the COLLO-MIS (Lima, Udine, Italy), and the MiniHip (Corin, Cirencester, UK). We found only 1 small case series with the Delphi-M stem, which had a survival rate below the benchmark ( panel I) (Budde et al. Citation2012). The survival of the Metha stem (B. Braun, Melsungen, Germany) varied greatly between studies, with some reporting survival rates below and others above the benchmark ( panel II). The revision rate per 100 observed component years for all 7 Metha stem studies combined was 1.2 (CI: 1.1–1.4) ().
Trochanter-sparing stems
We found 20 trochanter-sparing studies reporting on 8 stem types in 3,628 patients (). The mean follow-up was 3.4 (0.3–12) years (). Both the Profile and the Profile hydroxyapatite- (HA-) coated stem (DePuy, Warsaw, IN) showed the longest reported mean follow-up of 12 years in the same study (Hallan et al. Citation2006). Clinical reports on both of these stems were limited to this single case study, and both groups in this study consisted of only 25 patients. Although the survival of both stems was adequate, the addition of the HA coating appeared to be more favorable (, panel I).
We found 10 studies on the Mayo stem (Zimmer) involving 1,853 patients (), with a mean follow-up of 5 (0.3–7) years. 1 study compared the Mayo stem with an uncemented ABG stem (Stryker Howmedica Inc., Rutherford, NJ) in an RCT and found 100% survival of 45 hips after a short follow-up period of 3 months (Hube et al. Citation2004). The remaining studies were all case series. Although survival varied among Mayo stem studies, the majority of the larger case series had a survival rate exceeding the benchmark ( panel II), reflected by a mean revision rate per 100 observed component years of 0.8 ().
The Aida stem (Implantcast, Buxtehude, Germany) was the only trochanter-sparing stem with a survival below the benchmark in 35 hips with a mean follow-up of 15 months. The survival rate of 97% was the result of a single stem revision due to a periprosthetic fracture after a fall on the seventh postoperative day (Mumme Citation2013). Due to the short follow-up and small sample size, this single revision resulted in a revision rate per 100 observed component years of 2.3. All remaining trochanter-sparing stems had excellent survival rates with revision rate per 100 observed component years at or below the benchmark of 1, resulting in a mean revision rate per 100 observed component years of 0.8 (CI: 0.77–0.83) ().
Discussion
We found a large number of partial collum and trochanter-sparing stem observational case series showing adequate survival rates at medium-term follow-up. Considering the large number of collum stems currently on the market, we expected to find more studies on collum stems. Clinical evidence for collum stem studies was limited to a small number of studies with a medium-term follow-up period. These studies did not show a satisfactory overall survival rate. We found a large increase in publications on short-stem hip arthroplasty in recent years. This recent trend illustrates the evolution of today’s market towards bone- and tissue-sparing total hip arthroplasty. We therefore suspect that several short-stem studies were published after January 1, 2013, which were not included in this review.
There is no clear definition of what a short stem is. After roughly classifying the stem-anchoring principles in 4 groups, Gulow et al. (Citation2007) provided a rather arbitrary distinction between group 3 (short stems) and group 4 (conventional stems): short stems are (in today’s language) hip implants that are anchored in the metaphysis and the proximal part of the diaphysis and are shorter than the classic standard stems. In the absence of a clear definition of “short”, some trochanter-sparing type stems included in this review, such as the Citation, may be on the borderline of being short. The exclusion of other conventional stems with a short diaphyseal anchorage was somewhat arbitrary.
We classified the short stems in 3 categories, despite possible overlap. For example, the Mayo stem requires preservation of a small intact cortical ring in which cancellous bone is impacted for its stability (Falez et al. Citation2008). Since this ring is fairly small, we did not consider that femoral neck preservation is its main feature. In addition, design features of stems within the same category may differ as well, such as coatings, three-dimensional shapes, modular necks, curvatures, and integrated anteversion angles.
The geometrical differences result in different levels of resection and variations in the restoration of offset and leg length between short stems, especially in coxa valga or coxa vara patients. By templating 19 different short stems on the anteroposterior pelvic radiographs of 3 patients with markedly different caput-collum-diaphyseal angles, Babisch (Citation2013) demonstrated large offset and leg length differences between stems. Few stems achieved good reconstruction of leg length and offset in all 3 patients. All these stems were partial collum or trochanter-sparing stems: Fitmore, CFP, MiniHip, Optimys, and Global tissue-sparing stems (Biomet, Warsaw, IN).
To our knowledge, our study is the first to summarize the clinical results of all 3 categories of short-stem hip arthroplasty stems. Our results agree with a previous systematic review by Rometsch et al. (Citation2012), which summarized the survival of all short-hip stems with a “modern” trochanter-sparing design and included both partial collum and trochanter-sparing stems. The authors included 14 studies with a total rate of revision for any reason per 100 observed component years of 0.38, while we included 44 partial collum and trochanter-sparing stem studies with a total revision rate per 100 observed component years of 0.70. They included a thorough assessment of the study quality and found high variability, with no apparent association between study quality and survival. The authors concluded that even though the early survival rates of these types of stems appeared to be comparable to those of other uncemented stems, most of the publications that were included presented only short-term data. Similarly to Rometsch et al. (Citation2012), virtually all studies in our review were observational case series, few of which had a follow-up of more than 5 years. The majority of short-stem hip arthroplasty studies consisted of level-4 case series, with only 2 small-sized randomized clinical studies with a short follow-up period. In observational studies, there is the inherent risk of selection bias if the ideal patients are selected for these procedures. Furthermore, most of these studies were performed by hip surgeons with special interest in total hip arthroplasty, resulting in expertise bias. This emphasizes the need for well-constructed RCTs to evaluate hip implant innovations.
Consistent with Rometsch et al. (Citation2012), we used the revision rate per 100 observed component years to summarize revision data based on several studies with different numbers of cases and follow-up periods. This method allows comparison of datasets adjusted for the 2 main factors influencing the value of individual cohorts: number of cases and follow-up period (Labek et al. Citation2011). However, this indicator does not completely correspond to revision rates from hip arthroplasty registries. It assumes a linear distribution of revision over time, although arthroplasty data show relatively more revisions within the first year. However, the small differences between back-calculated values based on the revision rate per 100 observed component years and the registry data actually measured had no effect on the overall result, especially when more significant confounders were taken into consideration. These confounders include population demographics, surgical expertise, or the influence of a national public healthcare system. This may cause differences in survival of up to a factor 3 between individual departments and individual implants, and even between national registries when comparing the survival rates of the same implant. The large effect of confounders on survival complicates drawing conclusions from small deviations from the benchmark, since they may be caused by factors other than the type of implant. Moreover, a systematic review of reports from worldwide registry datasets showed a mean revision rate per 100 observed component years of 1.29 after primary total hip arthroplasty, which corresponds to a revision rate of 12.9% after 10 years (Labek et al. Citation2011). Thus, strict adherence to the benchmark of less than 1 revision per 100 observed component years when evaluating innovative hip implants is debatable.
In addition, while revision rate per 100 observed component years may be a suitable indicator in large series with long-term follow-up, its use is of limited value in small case series or studies with a short follow-up period. In these case series the denominator is small, with a resultant large effect of a single revision on the numerator. Although most likely unrelated to the type of implant, the single revision for a periprosthetic fracture resulted in a high revision rate per 100 observed component years for both the Optimys and the Aida stem series (Mumme Citation2013, Pfeil et al. Citation2013). Nonetheless, the consistently good survival rates in several larger and smaller case series of other stems, such as the CFP, the Metha, and the Mayo, indicate that the medium-term survival of these stems is likely to be comparable to that of conventional uncemented stems ( panels I and II, and panel II).
Our study only provides information on the durability of these implants, but not their potential clinical benefits. Smaller curved stems should more easily enable minimally invasive hip approaches. Therefore, with the increased popularity of minimally invasive hip approaches, the use of smaller curved stems is becoming more widespread. In a systematic review of published results of short and standard-length stems inserted though a minimally invasive approach, McElroy et al. (Citation2011) determined whether 1 type of implant was preferable. Although some authors used a short stem with a minimally invasive approach, the majority of studies used a conventional stem. Successful functional outcomes and adequate survival were reported for both stem types.
Retaining the femoral neck by using collum and partial collum short stems potentially improves biomechanical reconstruction. An increase in horizontal offset correlates positively with abductor strength, although too much offset may cause trochanteric bursitis and possibly a higher stem failure rate (Kamada et al. Citation2011, Schmidutz et al. Citation2012a). Previous studies have shown an increase in horizontal femoral offset, within the beneficial range, when using partial collum stems (Jerosch et al. Citation2012, Schmidutz et al. Citation2012a). However, due to the higher femoral resection, restoration of limb length was more difficult with a tendency for leg lengthening (Confalonieri et al. Citation2008, Schmidutz et al. Citation2012a, Van Oldenrijk et al. Citation2013).
The load of short stems on proximal metaphyseal bone should prevent proximal stress shielding and long-term osteolysis. However, several studies using periprosthetic CT osteodensitometry and DXA have shown progressive loss of metaphyseal cortical and cancellous bone density loss with use of a short stem. Furthermore, bone density loss in Gruen zones 3, 4, and 5, below the trochanter minor, was significantly lower or absent, thereby suggesting diaphyseal fixation (Roth et al. Citation2005, Logroscino et al. Citation2011, Schmidt et al. Citation2011, Kress et al. Citation2012, Lazarinis et al. Citation2013).
In conclusion, despite favorable medium-term revision rates suggested by observational studies, there remains a need for long-term RCTs, registry data, biomechanical analyses, and bone density measurement to affirm the benefits of short-stem hip arthroplasty.
JVO and DH: preparation of protocol, search for and selection of articles, data extraction and analysis, and writing and editing of manuscript. JM and MK: search for and selection of articles, and data extraction. RWP: preparation of protocol, and writing and editing of manuscript.
No competing interests declared.
- Adelani MA, Keeney JA, Palisch A, Fowler SA, Clohisy JC. Has total hip arthroplasty in patients 30 years or younger improved? A systematic review. Clin Orthop 2013; (471) (8): 2595-601.
- Babisch J. Möglichkeiten der patientenindividuellen Hüftgelenkrekonstruktion und Knochenresection bei Kurzschaftprothesen. In: Kurzschaftendoprothesen. Wo liegen die Unterschiede ( ed. Jerosch J). Cologne: Deutscher Ärzte-Verlag GmbH; 2013: 193-227.
- Birkenhauer B, Kistmacher H, Ries J. Conception and first results of the Spiron cementless femoral neck screw prosthesis. Orthopade 2004; 33 (11): 1259-66.
- Braun A, Sabah A. Two-year results of a modular short hip stem prosthesis--a prospective study. Z Orthop Unfall 2009; 147 (6): 700-6.
- Briem D, Schneider M, Bogner N, Botha N, Gebauer M, Gehrke T, Schwantes B. Mid-term results of 155 patients treated with a collum femoris preserving (CFP) short stem prosthesis. Int Orthop 2011; 35 (5): 655-60.
- Bücking P, Wittenberg RH. Metha. In: Kurzschaftendoprothesen. Wo liegen die Unterschiede ( ed. Jerosch J). Cologne: Deutscher Ärzte-Verlag GmbH; 2013: 66-9.
- Budde S, Windhagen H, Lerch M, Broese M, Gotze P, Thorey F. Clinical and radiological results after implantation of the femoral neck preserving Delfi M hip prosthesis: a case series. Technol Health Care 2012; 20 (2): 85-93.
- Carlsson LV, Albrektsson T, Albrektsson BE, Jacobsson CM, Macdonald W, Regner L, Weidenhielm LR. Stepwise introduction of a bone-conserving osseointegrated hip arthroplasty using RSA and a randomized study: II. Clinical proof of concept–40 patients followed for 2 years. Acta Orthop 2006; 77 (4): 559-66.
- Confalonieri N, Manzotti A, Montironi F, Pullen C. Leg length discrepancy, dislocation rate, and offset in total hip replacement using a short modular stem: navigation vs conventional freehand. Orthopedics (10 Suppl 1) 2008; 31.
- Dillon A. Hip disease– replacement prostheses (TA2). Technology appraisal Manchester: National Institute for Health and Clinical Excellence Level 1A, City Tower, Piccadilly Plaza, Manchester M1 4BT; 2003 (updated 04-01-201315-08-2013); Available from: http://guidance.nice.org.uk/TA2/Guidance/pdf/English.
- Ender SA, Machner A, Pap G, Hubbe J, Grashoff H, Neumann HW. Cementless CUT femoral neck prosthesis: increased rate of aseptic loosening after 5 years. Acta Orthop 2007; 78 (5): 616-21.
- Ettinger M, Ettinger P, Lerch M, Radtke K, Budde S, Ezechieli M, Becher C, Thorey F. The NANOS short stem in total hip arthroplasty: a mid term follow-up. Hip Int 2011; 21 (5): 583-6.
- Falez F, Casella F, Panegrossi G, Favetti F, Barresi C. Perspectives on metaphyseal conservative stems. J Orthop Traumatol 2008; 9 (1): 49-54.
- Floerkemeier T, Tscheuschner N, Calliess T, Ezechieli M, Floerkemeier S, Budde S, Windhagen H, von Lewinski G. Cementless short stem hip arthroplasty METHA (R) as an encouraging option in adults with osteonecrosis of the femoral head. Arch Orthop Trauma Surg 2012; 132 (8): 1125-31.
- Ghera S, Pavan L. The DePuy Proxima hip: a short stem for total hip arthroplasty. Early experience and technical considerations. Hip Int 2009; 19 (3): 215-20.
- Gilbert RE, Salehi-Bird S, Gallacher PD, Shaylor P. The Mayo Conservative Hip: experience from a district general hospital. Hip Int 2009; 19 (3): 211-4.
- Gill IR, Gill K, Jayasekera N, Miller J. Medium term results of the collum femoris preserving hydroxyapatite coated total hip replacement. Hip Int 2008; 18 (2): 75-80.
- Goebel D, Schultz W. The Mayo cementless femoral component in active patients with osteoarthritis. Hip Int 2009; 19 (3): 206-10.
- Gotze C, Ehrenbrink J, Ehrenbrink H. Is there a bone-preserving bone remodelling in short-stem prosthesis? DEXA analysis with the Nanos total hip arthroplasty. Z Orthop Unfall 2010; 148 (4): 398-405.
- Gulow J, Scholz R, Freiherr von Salis-Soglio G. Short-stemmed endoprostheses in total hip arthroplasty. Orthopade 2007; 36 (4): 353-9.
- Gustke K. Short stems for total hip arthroplasty: initial experience with the Fitmore stem. J Bone Joint Surg (Br) (11 Suppl A) 2012; 94: 47-51.
- Hagel A, Hein W, Wohlrab D. Experience with the Mayo conservative hip system. Acta Chir Orthop Traumatol Cech 2008; 75 (4): 288-92.
- Hallan G, Lie SA, Havelin LI. High wear rates and extensive osteolysis in 3 types of uncemented total hip arthroplasty: a review of the PCA, the Harris Galante and the Profile/Tri-Lock Plus arthroplasties with a minimum of 12 years median follow-up in 96 hips. Acta Orthop 2006; 77 (4): 575-84.
- Hube R, Zaage M, Hein W, Reichel H. Early functional results with the Mayo-hip, a short stem system with metaphyseal-intertrochanteric fixation. Orthopade 2004; 33 (11): 1249-58.
- Ishaque BA, Gils J, Wienbeck S, Donle E, Basad E, Sturz H. Results after replacement of femoral neck prostheses - thrust plate prosthesis (TPP) versus ESKA cut prosthesis. Z Orthop Unfall 2009; 147 (1): 79-88.
- Jerosch J. Kurzschaftendoprothesen. Wo liegen die Unterschiede. Cologne: Deutscher Ärzte-Verlag GmbH; 2013a: 234.
- Jerosch J. MiniHip. In: Kurzschaftendoprothesen. Wo liegen die Unterschiede ( ed. Jerosch J). Cologne: Deutscher Ärzte-Verlag GmbH; 2013b: 164-6.
- Jerosch J, Grasselli C, Kothny PC, Litzkow D, Hennecke T. Reproduction of the anatomy (offset, CCD, leg length) with a modern short stem hip design–a radiological study. Z Orthop Unfall 2012; 150 (1): 20-6.
- Kamada S, Naito M, Nakamura Y, Kiyama T. Hip abductor muscle strength after total hip arthroplasty with short stems. Arch Orthop Trauma Surg 2011; 131 (12): 1723-9.
- Kendoff D, Egidy C, Gehrke T. C.F.P. In: Kurzschaftendoprothesen. Wo liegen die Unterschiede ( ed. Jerosch J). Cologne: Deutscher Ärzte-Verlag GmbH; 2013: 48.
- Kress AM, Schmidt R, Nowak TE, Nowak M, Haeberle L, Forst R, Mueller LA. Stress-related femoral cortical and cancellous bone density loss after collum femoris preserving uncemented total hip arthroplasty: a prospective 7-year follow-up with quantitative computed tomography. Arch Orthop Trauma Surg 2012; 132 (8): 1111-9.
- Krieger M. COLLO-MIS. In: Kurzschaftendoprothesen. Wo liegen die Unterschiede ( ed. Jerosch J). Cologne: Deutscher Ärzte-Verlag GmbH; 2013: 134-8.
- Labek G, Abel J, Agreiter M, Alegre DN, Arrich F, Asparouhov A, Atilla B, Caceres-Palou E, Berger C, Böhler N, Brabec V, Delaunay V, da Conceição Diogo NM, Dorninger R, Frischhut S, Haderer B, Haselsteiner F, Forster Horváth C, Hassenpflug J, Hochgatterer R, Hoffmeyer P, Hois I, Hübl M, Iovanescu L, Janda W, Kandel L, Kendoff D, Keurentjes C, Kjaersgaard-Andersen P, Klaus H, Krismer M, Krivanek S, Labek G, Lair J, Leonhardt J, Liebensteiner M, Liebs T, Lübbeke-Wolff A, Matamalas Adrover A, Mattan Y, Mroz R, Necas L, Nelissen R, Neumann D, Pabinger C, Pawelka W, Pfeiffer KP, Pijls B, Rauf R, Ribeiro C, Schlichtherle R, Schuh R, Sekyra K, Specht K, Stoica CI, Stöckl B, Szendroi M, Tarnau A, Thaler M, Thelu C, Todorov S, Williams V, Zagra V, Zahár A, Ziernhöld G. Final Report of EFORT-EAR’s QoLA Project on the Quality of Publications regarding the Outcome of Revision Rate after Arthroplasty. published at the 2011 EFORT Congress in Copenhagen. 2011.
- Labek G, Thaler M, Janda W, Agreiter M, Stockl B. Revision rates after total joint replacement: cumulative results from worldwide joint register datasets. J Bone Joint Surg (Br) 2011; 93 (3): 293-7.
- Lazarinis S, Mattsson P, Milbrink J, Mallmin H, Hailer NP. A prospective cohort study on the short collum femoris-preserving (CFP) stem using RSA and DXA. Primary stability but no prevention of proximal bone loss in 27 patients followed for 2 years. Acta Orthop 2013; 84 (1): 32-9.
- Lerch M, von der Haar-Tran A, Windhagen H, Behrens BA, Wefstaedt P, Stukenborg-Colsman CM. Bone remodelling around the Metha short stem in total hip arthroplasty: a prospective dual-energy X-ray absorptiometry study. Int Orthop 2012; 36 (3): 533-8.
- Logroscino G, Ciriello V, D’Antonio E, De Tullio V, Piciocco P, Magliocchetti Lombi G, Santori FS, Albanese CV. Bone integration of new stemless hip implants (proxima vs. nanos). A DXA study: preliminary results. Int J Immunopathol Pharmacol (1 Suppl 2) 2011; 24: 113-6.
- Lombardi AV, Jr., Berend KR, Adams JB. A short stem solution: through small portals. Orthopedics 2009; 32 (9): pii: orthosupersite.com/view.asp?rID=42833.
- McElroy MJ, Johnson AJ, Mont MA, Bonutti PM. Short and standard stem prostheses are both viable options for minimally invasive total hip arthroplasty. Bull NYU Hosp Jt Dis (Suppl 1) 2011; 69: S68-76.
- Molfetta L, Capozzi M, Caldo D. Medium term follow up of the Biodynamic neck sparing prosthesis. Hip Int 2011; 21 (1): 76-80.
- Molli RG, Lombardi AV, Jr., Berend KR, Adams JB, Sneller MA. A short tapered stem reduces intraoperative complications in primary total hip arthroplasty. Clin Orthop 2012; (470) (2): 450-61.
- Morrey BF. Short-stemmed uncemented femoral component for primary hip arthroplasty. Clin Orthop 1989; (249): 169-75.
- Morrey BF, Adams RA, Kessler M. A conservative femoral replacement for total hip arthroplasty. A prospective study. J Bone Joint Surg (Br) 2000; 82 (7): 952-8.
- Mumme T. AIDA. In: Kurzschaftendoprothesen. Wo liegen die Unterschiede ( ed. Jerosch J). Cologne: Deutscher Ärzte-Verlag GmbH; 2013: 109-11.
- Nowak M, Nowak TE, Schmidt R, Forst R, Kress AM, Mueller LA. Prospective study of a cementless total hip arthroplasty with a collum femoris preserving stem and a trabeculae oriented pressfit cup: minimun 6-year follow-up. Arch Orthop Trauma Surg 2011; 131 (4): 549-55.
- Oehme S. MAYO. In: Kurzschaftendoprothesen. Wo liegen die Unterschiede ( ed. Jerosch J). Cologne: Deutscher Ärzte-Verlag GmbH; 2013: 57-8.
- Patel RM, Smith MC, Woodward CC, Stulberg SD. Stable fixation of short-stem femoral implants in patients 70 years and older. Clin Orthop 2012; (470) (2): 442-9.
- Pfeil J, Siebert W, Grieshaber HM. Optimys. In: Kurzschaftendoprothesen. Wo liegen die Unterschiede ( ed. Jerosch J). Cologne: Deutscher Ärzte-Verlag GmbH; 2013: 38-40.
- Pipino F. Preservation of the femoral neck in hip arthroplasty: results of a 13-17 year follow-up. J Orthop Trauma 2000; 1: 31-9.
- Pipino F. CFP prosthetic stem in mini-invasive total hip arthroplasty. Journal of Orthopedics and Traumatology. 2004; 5 (3 ): 165-71.
- Pons M. Learning curve and short-term results with a short-stem CFP system. Hip Int (Suppl 7) 2010; 20: 52-7.
- Rohrl SM, Li MG, Pedersen E, Ullmark G, Nivbrant B. Migration pattern of a short femoral neck preserving stem. Clin Orthop 2006; (448): 73-8.
- Rometsch E, Bos PK, Koes BW. Survival of short hip stems with a “modern”, trochanter-sparing design–a systematic literature review. Hip Int 2012; 22 (4): 344-54.
- Roth A, Richartz G, Sander K, Sachse A, Fuhrmann R, Wagner A, Venbrocks RA. Periprosthetic bone loss after total hip endoprosthesis. Dependence on the type of prosthesis and preoperative bone configuration. Orthopade 2005; 34 (4): 334-44.
- Rudert M, Leichtle U, Leichtle C, Thomas W. Implantation technique for the CUT-type femoral neck endoprosthesis. Oper Orthop Traumatol 2007; 19 (5-6): 458-72.
- Schemitsch EH, Bhandari M, Boden SD, Bourne RB, Bozic KJ, Jacobs JJ, Zdero R. The evidence-based approach in bringing new orthopaedic devices to market. J Bone Joint Surg (Am) 2010; 92 (4): 1030-7.
- Schmidt R, Gollwitzer S, Nowak TE, Nowak M, Haberle L, Kress A, Forst R, Muller LA. Periprosthetic femoral bone reaction after total hip arthroplasty with preservation of the collum femoris: CT-assisted osteodensitometry 1 and 3 years postoperatively. Orthopade 2011; 40 (7): 591-8.
- Schmidutz F, Beirer M, Weber P, Mazoochian F, Fottner A, Jansson V. Biomechanical reconstruction of the hip: comparison between modular short-stem hip arthroplasty and conventional total hip arthroplasty. Int Orthop 2012a; 36 (7): 1341-7.
- Schmidutz F, Graf T, Mazoochian F, Fottner A, Bauer-Melnyk A, Jansson V. Migration analysis of a metaphyseal anchored short-stem hip prosthesis. Acta Orthop 2012b; 83 (4): 360-5.
- Steens W, Skripitz R, Schneeberger AG, Petzing I, Simon U, Goetze C. Cementless femoral neck prosthesis CUT–clinical and radiological results after 5 years. Z Orthop Unfall 2010; 148 (4): 413-9.
- Synder M, Drobniewski M, Pruszczynski B, Sibinski M. Initial experience with short Metha stem implantation. Ortop Traumatol Rehabil 2009; 11 (4): 317-23.
- Thomas W, Lucente L, Mantegna N, Grundei H. ESKA (CUT) endoprosthesis. Orthopade 2004; 33 (11): 1243-8.
- Toth K, Mecs L, Kellermann P. Early experience with the Depuy Proxima short stem in total hip arthroplasty. Acta Orthop Belg 2010; 76 (5): 613-8.
- Tsao A, Pesut T, Peacock C, Tucci M, Buckhalter RA. Bone sparing surgical options for total hip replacement. Biomed Sci Instrum 2003; 39: 284-8.
- Van Oldenrijk J, Schafroth MU, Rijk E, Runne WC, Verheyen CC, van Egmond C, Bhandari M, Poolman RW. Learning curve analysis of the Collum Femoris Preserving total hip surgical technique. Hip Int 2013; 23 (2): 154-61.
- Wohlrab D, Hagel A, Hein W. Advantages of minimal invasive total hip replacement in the early phase of rehabilitation. Z Orthop Ihre Grenzgeb 2004; 142 (6): 685-90.
