Abstract
Background and purpose — Although plating is considered to be the treatment of choice in distal tibia fractures, controversies abound regarding the type of plating for optimal fixation. We conducted a systematic review to evaluate and compare the outcomes of locked plating and non-locked plating in treatment of distal tibia fractures.
Patients and methods — A systematic review was conducted using PubMed to identify articles on the outcomes of plating in distal tibia fractures that were published up to June 2012. We included English language articles involving a minimum of 10 adult cases with acute fractures treated using single-plate, minimally invasive techniques. Study-level binomial regression on the pooled data was conducted to determine the effect of locking status on different outcomes, adjusted for age, sex, and other independent variables.
Results — 27 studies met the inclusion criteria and were included in the final analysis of 764 cases (499 locking, 265 non-locking). Based on descriptive analysis only, delayed union was reported in 6% of cases with locked plating and in 4% of cases with non-locked plating. Non-union was reported in 2% of cases with locked plating and 3% of cases with non-locked plating. Comparing locked and non-locked plating, the odds ratio (OR) for reoperation was 0.13 (95% CI: 0.03–0.57) and for malalignment it was 0.10 (95% CI: 0.02–0.42). Both values were statistically significant.
Interpretation — This study showed that locked plating reduces the odds of reoperation and malalignment after treatment for acute distal tibia fracture. Future studies should accurately assess causality and the clinical and economic impact of these findings.
The term distal tibia fractures encompasses a broad array of injuries involving the distal metadiaphyseal and metaphyseal region (Court-Brown and McBirnie Citation1995). Given the often diverse fracture patterns, a variety of operative strategies have evolved to treat these injuries, ranging from external fixation (El-Shazly et al. Citation2001, Babis et al. Citation2010) to locked compression plating (Bahari et al. Citation2007, Ahmad et al. Citation2012).
Plating has emerged as a common treatment for these injuries, as they are often too distal for traditional intramedullary nailing. To minimize disruption of the particularly tenuous soft-tissue envelope and periosteal blood supply, minimally invasive plate osteosynthesis (MIPO) was developed (Farouk et al. Citation1999, Hasenboehler et al. Citation2007) and then applied to locked plating (Lee et al. Citation2008).
More recently, studies have found healing complications related to the stiffness of locked plating, namely delayed union and non-union (Henderson et al. Citation2011). We conducted a systematic review to compare the outcomes and complications of locked and non-locked plating in the treatment of distal tibial fractures in adults. We hypothesized that these difficult-to-treat, often periarticular injures would have less complications when locking technology was used.
Material and methods
Search strategy
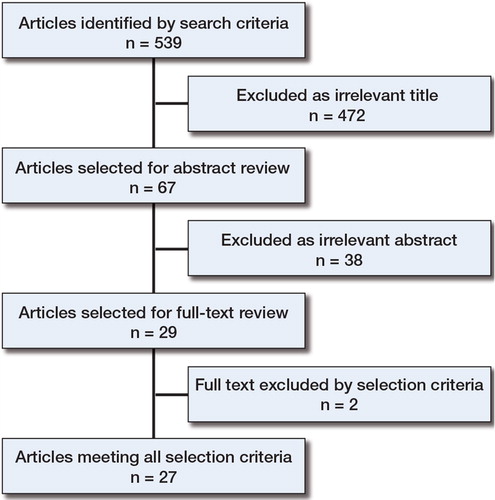
This systematic review was registered with the PROSPERO international database at the Centre for Reviews and Dissemination (registration number CRD4201400710). Our protocol consisted of a systematic literature search performed up to June 2012, using PubMed, to identify studies involving minimally invasive locked and non-locked plating of distal tibia fractures. The following keywords were used: “distal tibia fracture(s)” and “pilon fracture(s)”, with each of the following additional search terms: “minimally invasive”, “MIPO”, “MILPO”, “locking plates”, “locked plating”, or “plate fixation”. Each combination of these keywords and additional search terms on PubMed were initially screened for relevance by 2 independent observers based on title, then abstract, and finally full-text review using the following inclusion and exclusion criteria.
Selection criteria
Before initiating the search, we established proper inclusion and exclusion criteria to determine the eligibility of any article for consideration for review. The inclusion criteria were: (1) English language article; 2) study with at least 10 cases involving patients 18 years of age or older; and (3) open and closed fractures defined as “distal” AO 42A-C and all AO 43A-C (based on AO classification of fractures) (Müller et al. Citation1990). The exclusion criteria were: (1) double plating application; (2) use of a lateral approach for non-invasive plating of the distal tibia rather than a medial approach; (3) study involving combination plating and intramedullary fixation; (4) no specification of minimally invasive osteosynthesis technique; and (5) no specification of locked or non-locked plating.
Data extraction ()
2 observers (ASK and NT) reviewed all the identified titles and abstracts independently. For inclusion of an article, there had to be agreement between the observers. The full texts of the articles selected were then reviewed. The following independent variables and outcomes were retrieved and extracted to a spreadsheet: demographic data (sex, age); average follow-up; number of cases in each study; number of open fractures; number of intra- and extra-articular fractures; incidence of superficial and deep infection, malalignment, non-union, delayed union, bone graft application, wound healing problems, hardware removal, implant failure, and reoperation for reasons other than bone grafting or hardware removal or debridement. Malalignment was defined as any angular deformity of more than 5 degrees in the frontal plane or more than 10 degrees in the sagittal plane, unless otherwise mentioned in the article. If the authors of an article did not define “delayed union” or “non-union”, we considered “delayed union” to mean that the healing time exceeded 6 months and we considered “non-union” to be failure to heal by 9 months. Implant failure was defined as any instance of screw cutout, plate/screw breakage, or implant displacement (Farouk et al. Citation1999).
Statistics
Several outcomes were compared across the selected studies; these included: non-union, delayed union, bone graft application, superficial infection, deep infection, wound healing difficulties, implant failure, reoperation, malalignment, and implant removal. Study-level binomial regression was used on the pooled data across the included studies. To carry out this regression, the glm function was used in the R software package (R Core Team Citation2012), where each regression was weighted using the number of cases. Because there was suspected heterogeneity among the chosen studies, the regression model assumed the quasi-binomial distribution rather than the binomial distribution. The quasi-binomial distribution is similar to the binomial one, with the exception that the dispersion parameter is no longer fixed to 1 and allows for the estimation of over-dispersion. 2 models were systematically investigated. Model 1 was a simple model that examined only the effect of locking status—which was the primary study characteristic of interest—on each outcome. Model 2 extended model 1 such that it not only included locking status but also adjusted for various study characteristics of interest, which included: mean age of study participants, average follow-up time, number of female study participants, number of open fractures, and number of intra- and extra-articular fractures.
Risk of bias
As with any systematic review, several forms of bias are introduced and must be considered when collecting and analyzing source data. Database bias is present, however small, when using an expansive collection of literature such as PubMed. Source selection bias, again small, is present when only making use of published data. Finally, publication bias may exist in any systematic review in which conclusions are drawn from pooled studies, as there is always potential for under- or over-reporting of certain outcomes.
Results
29 studies met our eligibility criteria. 17 of them involved patients with locked plating and 11 of them involved patients with non-locked plates. 1 study (Ozkaya et al. Citation2009) included patients in both groups (). 2 other studies did not report thoroughly on the data necessary for analysis, so only 27 studies contributed to the analysis (). None of the studies included was a truly randomized clinical trial. There were 764 cases altogether, with 499 cases involving locked plating and 265 cases involving non-locked plating. The average age of the study participants was 44 (31–53) years. In the studies selected, there were approximately 10 females per study with 1 study (Krackhardt et al. Citation2005) involving 26 females. The mean follow-up time was 20 (8.8–36) months. The number of open fractures varied among studies, and there were as few as 0 open fractures in 12 studies, while Krackhardt et al. (Citation2005) had as many as 21 open fractures. The number of intra- and extra-articular fractures in each study varied, with an average of 10 intra-articular fractures and 18 extra-articular fractures.
Table 1. Characteristics of the studies
Based on descriptive analysis, locked plating showed a higher rate of delayed union (6%) and implant removal (21%) than non-locked plating (4% and 7%, respectively). Locked plating showed a lower rate of non-union (2%), malalignment (2%), and reoperation (1%) than non-locked plating (3% non-union, 12% malalignment, and 5% reoperation) ().
Quasi-binomial regression model 1 examined the effect of locking status on each outcome. When we pooled all studies and carried out regression analysis, the estimated odds ratio (OR) for non-unions of locked plating compared to non-locked plating was 0.40 (95% CI: 0.20–0.81; p = 0.02) (). Using model 1, removal of a locked plate was more likely to occur, with an OR of 6 (95% CI: 1.8–19; p = 0.007). Reoperation (OR = 0.14; p = 0.01) and malalignment (OR = 0.09; p < 0.001) were also less likely to occur when locked plating was used.
Table 2. Quasi-binomial regression results for the effect of locking status on various outcomes (i.e. model 1)
With adjustment for all independent variables, quasi-binomial regression model 2 showed no statistically significant relationship between locked plating and non-unions (OR = 0.44; p = 0.2) or delayed unions (OR = 1.5; p = 0.5) (). The estimated odds ratio for reoperation of a locked plate vs. a non-locked plate was 0.13 (95% CI: 0.03–0.57; p = 0.01), while that for malalignment was 0.10 (95% CI: 0.02–0.42; p = 0.005).
Table 3. Quasi-binomial regression results for the effect of locking status on various outcomes adjusted for all of the independent variables (i.e. model 2)
Discussion
To our knowledge, this is the first systematic review to directly compare outcomes of locked and non-locked plating in distal tibia fractures treated using the MIPO and MILPO techniques. In response to the high rates of infection, delayed union, and non-union with traditional extensile approaches in the distal tibia region, MIPO techniques were developed (Helfet et al. Citation1997, Cole and Stephen Citation1999) and later adapted to locked compression plating (LCP), i.e. MILPO (Hazarika et al. Citation2006, Bahari et al. Citation2007). Employing both indirect and direct reduction maneuvers, this technique allows for an extra-periosteal, subcutaneous tunnel to run between 2 or more small incisions, allowing the plate to span the fracture site while minimizing soft-tissue disruption (Redfern et al. Citation2004).
More recently, plate selection has become a topic of debate, with high rates of healing difficulties reported with the use of locked plates in other anatomical regions (Henderson et al. Citation2011). Previously, Newman et al. (Citation2011) had looked at all the fixation techniques for non-articular distal tibia fractures, including plating using a minimally invasive approach. Their review of locked and non-locked plating revealed low rates of infection, malunion, and non-union with both plating systems when using this technique.
In contrast, when using quantitative analysis alone, we found locked plating to have a 50% increase in the rate of delayed union and a 3-fold increase in the rate of implant removal while the rate of malalignment was 6 times less prevalent with locked plating. The rate of superficial infection was similar in both plating groups studied.
When examining the effect of locked plating on each variable via model 1, non-union, reoperation, and malalignment are seemingly less likely to occur with the use of locked plating (). Conversely, locked plating was more likely to result in implant removal. Although a higher rate of delayed union was observed with locked plating, this was not found to be significant when applying the regression model (OR = 1.5; p = 0.4).
When adjusted for all independent variables, model 2 demonstrated that the relative probabilities for delayed union (OR = 1.5; p = 0.5) or non-union (OR = 0.44; p = 0.2) were no different with locked plating. In addition, the odds ratio of implant removal was no longer significant (p = 0.06). Conversely, the significantly lower relative probability of reoperation (p = 0.01) and malalignment (p = 0.005) remained when locked plating was used. These findings should call for consideration of the statistical method used when outcomes of locked and non-locked plating are reported.
We attempted to determine the relative chances of complications among heterogeneous studies. However, a thorough meta-analysis was not possible as there has not been a sufficient number of prospective, comparative, and randomized clinical trials. Variability in the reporting of fracture location (articular vs. non-articular involvement; metaphyseal vs. meta-diaphyseal) and degree of comminution was difficult to standardize for the review, and may have affected the findings. Additionally, the lack of a standardized method for evaluation and reporting of complications may have affected the results. For instance, the reporting of wound complications (superficial vs. deep) was not standardized, and therefore difficult to categorize—thereby possibly skewing outcomes. Other factors, such as smoking history, diabetes, and other chronic medical diseases, may have adversely affected outcomes. However, such data were not adjusted for, as they were either under-reported or not reported at all in the studies selected.
The confounding potential of some variables must be considered in the comparison of locked and non-locked plating in this study. Locking plates are more recent technology, so most of the studies included were more recent than the non-locked studies. This could represent a trend in the use of “newer” technology in the treatment of distal tibia fractures rather than a true effect of the locking mechanism on treatment outcomes. Furthermore, surgeon preference may also be a factor in the choice of plate fixation: more conservative surgeons may be less likely to use locking plates. Another potential confounder is severity of injury and subsequent choice of fixation. Degree of comminution is often difficult to quantify and report in a standardized format. However, this factor does often dictate the choice of surgical fixation and may skew certain fracture patterns with the choice of locked or non-locked plating. Finally, in an attempt to control for different surgical techniques, we included only studies that used a minimally invasive surgical approach by the medial side of tibia. This technique minimizes soft-tissue dissection in an attempt to promote vascularity around the fracture site. This may unintentionally increase the inclusion of either more severe injuries or a more “at-risk” patient population, and therefore prevent generalization of the current results to all patients.
Although this systematic review found a strong correlation between the use of locked plating and reduction of the odds of malalignment and reoperations, we are careful not to endorse its use in all distal tibia fractures. Additional, well-designed observational studies and randomized controlled trials are necessary to show causality, given the potential for confounding as previously discussed. Other clinical and cost-benefit factors must also be considered. While the use of internal fixed-angle devices has grown exponentially, resulting in three-quarters of all plates sold in the USA, indications for locked plating rather than non-locked plating in distal tibia fractures remain nebulous, often being left to the discretion of the surgeon (S Citation2012). As locking screws alone can cost up to 6 times more than non-locking screws, locked plating constructs come at a substantially greater cost to the patient and the healthcare system (S Citation2011). To better understand the indications and benefits of locked plating for these injuries, future studies should carefully scrutinize the cost-benefit of such devices in light of the reported outcomes.
ASK and NT did the literature search, data retrieval and manuscript preparation. LPT did statistical analysis. NHA designed the study. KWD did the initial search and writing. DLC edited the manuscript and developed the idea.
No competing interests declared.
- Ahmad MA, Sivaraman A, Zia A, Rai A, Patel AD. Percutaneous locking plates for fractures of the distal tibia: our experience and a review of the literature. J Trauma Acute Care Surg 2012; 72 (2): E81-7.
- Aksekili MA, Celik I, Arslan AK, Kalkan T, Ugurlu M. The results of minimally invasive percutaneous plate osteosynthesis (MIPPO) in distal and diaphyseal tibial fractures. Acta Orthop Traumatol Turc 2012; 46 (3): 161-7.
- Babis GC, Kontovazenitis P, Evangelopoulos DS, Tsailas P, Nikolopoulos K, Soucacos PN. Distal tibial fractures treated with hybrid external fixation. Injury 2010; 41 (3): 253-8.
- Bahari S, Lenehan B, Khan H, McElwain JP. Minimally invasive percutaneous plate fixation of distal tibia fractures. Acta Orthop Belg 2007; 73 (5): 635-40.
- Borens O, Kloen P, Richmond J, Roederer G, Levine DS, Helfet DL. Minimally invasive treatment of pilon fractures with a low profile plate: preliminary results in 17 cases. Arch Orthop Trauma Surg 2009; 129 (5): 649-59.
- Borg T, Larsson S, Lindsjo U. Percutaneous plating of distal tibial fractures. Preliminary results in 21 patients. Injury 2004; 35 (6): 608-14.
- Cheng W, Li Y, Manyi W. Comparison study of two surgical options for distal tibia fracture-minimally invasive plate osteosynthesis vs. open reduction and internal fixation. Int Orthop 2011; 35 (5): 737-42.
- Cole PAB, Stephen K. Minimally invasive surgery for the pilon fracture: The percutaneous-submuscular plating technique. Tech Orthop 1999; 14 (3): 8.
- Collinge C, Protzman R. Outcomes of minimally invasive plate osteosynthesis for metaphyseal distal tibia fractures. J Orthop Trauma 2010; 24 (1): 24-9.
- Court-Brown CM, McBirnie J. The epidemiology of tibial fractures. J Bone Joint Surg (Br) 1995; 77 (3): 417-21.
- El-Shazly M, Dalby-Ball J, Burton M, Saleh M. The use of trans-articular and extra-articular external fixation for management of distal tibial intra-articular fractures. Injury (Suppl 4) 2001; 32: SD99-106.
- Farouk O, Krettek C, Miclau T, Schandelmaier P, Guy P, Tscherne H. Minimally invasive plate osteosynthesis: does percutaneous plating disrupt femoral blood supply less than the traditional technique? J Orthop Trauma 1999; 13 (6): 401-6.
- Francois J, Vandeputte G, Verheyden F, Nelen G. Percutaneous plate fixation of fractures of the distal tibia. Acta Orthop Belg 2004; 70 (2): 148-54.
- Guo JJ, Tang N, Yang HL, Tang TS. A prospective, randomised trial comparing closed intramedullary nailing with percutaneous plating in the treatment of distal metaphyseal fractures of the tibia. J Bone Joint Surg (Br) 2010; 92 (7): 984-8.
- Gupta RK, Rohilla RK, Sangwan K, Singh V, Walia S. Locking plate fixation in distal metaphyseal tibial fractures: series of 79 patients. Int Orthop 2010; 34 (8): 1285-90.
- Hasenboehler E, Rikli D, Babst R. Locking compression plate with minimally invasive plate osteosynthesis in diaphyseal and distal tibial fracture: a retrospective study of 32 patients. Injury 2007; 38 (3): 365-70.
- Hazarika S, Chakravarthy J, Cooper J. Minimally invasive locking plate osteosynthesis for fractures of the distal tibia—results in 20 patients. Injury 2006; 37 (9): 877-87.
- Helfet DL, Shonnard PY, Levine D, Borrelli J, Jr. Minimally invasive plate osteosynthesis of distal fractures of the tibia. Injury (Suppl 1) 1997; 28: A42-7; discussion A7-8.
- Henderson CE, Kuhl LL, Fitzpatrick DC, Marsh JL. Locking plates for distal femur fractures: is there a problem with fracture healing? J Orthop Trauma (Suppl 1) 2011; 25: S8-14.
- Khoury A, Liebergall M, London E, Mosheiff R. Percutaneous plating of distal tibial fractures. Foot Ankle Int 2002; 23 (9): 818-24.
- Krackhardt T, Dilger J, Flesch I, Hontzsch D, Eingartner C, Weise K. Fractures of the distal tibia treated with closed reduction and minimally invasive plating. Arch Orthop Trauma Surg 2005; 125 (2): 87-94.
- Lau TW, Leung F, Chan CF, Chow SP. Wound complication of minimally invasive plate osteosynthesis in distal tibia fractures. Int Orthop 2008; 32 (5): 697-703.
- Lee T, Blitz NM, Rush SM. Percutaneous contoured locking plate fixation of the pilon fracture: surgical technique. J Foot Ankle Surg 2008; 47 (6): 598-602.
- Leonard M, Magill P, Khayyat G. Minimally-invasive treatment of high velocity intra-articular fractures of the distal tibia. Int Orthop 2009; 33 (4): 1149-53.
- Ma CH, Yu SW, Tu YK, Yen CY, Yeh JJ, Wu CH. Staged external and internal locked plating for open distal tibial fractures. Acta Orthop 2010; 81 (3): 382-6.
- Maffulli N, Toms AD, McMurtie A, Oliva F. Percutaneous plating of distal tibial fractures. Int Orthop 2004; 28 (3): 159-62.
- Müller MENS, Koch P, Schatzker J. The comprehensive classification of fractures of long bones. 1st. ed. Springer-Verlag, Berlin, Heidelberg, New York 1990.
- Newman SD, Mauffrey CP, Krikler S. Distal metadiaphyseal tibial fractures. Injury 2011; 42 (10): 975-84.
- Oh CW, Park BC, Kyung HS, Kim SJ, Kim HS, Lee SM, et al. Percutaneous plating for unstable tibial fractures. J Orthop Sci 2003; 8 (2): 166-9.
- Ozkaya U, Parmaksizoglu AS, Gul M, Sokucu S, Kabukcuoglu Y. Minimally invasive treatment of distal tibial fractures with locking and non-locking plates. Foot Ankle Int 2009; 30 (12): 1161-7.
- Pai V, Coulter G, Pai V. Minimally invasive plate fixation of the tibia. Int Orthop 2007; 31 (4): 491-6.
- R Core Team (2012). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. ISBN 3-900051-07-0, URL http://www.R-project.org/.
- Redfern DJ, Syed SU, Davies SJ. Fractures of the distal tibia: minimally invasive plate osteosynthesis. Injury 2004; 35 (6): 615-20.
- Ronga M, Longo UG, Maffulli N. Minimally invasive locked plating of distal tibia fractures is safe and effective. Clin Orthop 2010; (468) (4): 975-82.
- Salton HL, Rush S, Schuberth J. Tibial plafond fractures: limited incision reduction with percutaneous fixation. J Foot Ankle Surg 2007; 46 (4): 261-9.
- Shon OJ, Park CH. Minimally invasive plate osteosynthesis of distal tibial fractures: a comparison of medial and lateral plating. J Orthop Sci 2012; 17 (5): 562-6.
- Shrestha D, Acharya BM, Shrestha PM. Minimally invasive plate osteosynthesis with locking compression plate for distal diametaphyseal tibia fracture. Kathmandu Univ Med J (KUMJ) 2011; 9 (34): 60-6.
- S M. 2011 Trauma Update. Orthopedic Network News 2011; 22 (2): 20.
- S M. 2012 Trauma Update. Orthopedic Network News 2012; 23 (2): 20.
- Tong D, Ji F, Zhang H, Ding W, Wang Y, Cheng P, et al. Two-stage procedure protocol for minimally invasive plate osteosynthesis technique in the treatment of the complex pilon fracture. Int Orthop 2012; 36 (4): 833-7.