Abstract
Background — Arthroscopic meniscal surgery is the most common orthopedic procedure, and the incidence has increased in Denmark over the last 10 years. Concomitantly, several randomized controlled trials have shown no benefit of arthroscopic procedures including arthroscopic partial meniscectomy in middle-aged and older individuals suffering from knee pain with or without knee osteoarthritis. We examined the annual incidence of meniscal procedures together with age, sex, and diagnosis for patients who underwent meniscal procedures in the period 2000–2011 in Denmark.
Methods — Data on age, sex, diagnosis, and surgical procedures were extracted from the Danish National Patient Register for the years 2000–2011, for all records containing meniscal surgery as a primary or secondary procedure.
Results — The overall annual incidence of meniscal procedures per 100,000 persons in Denmark doubled from 164 in 2000 to 312 in 2011 (i.e. 8,750 procedures to 17,368 procedures). A 2-fold increase was found for patients aged between 35 and 55, and a 3-fold increase was found for those older than 55. Middle-aged and older patients accounted for 75% of all 151,228 meniscal procedures carried out between 2000 and 2011.
Interpretation — The incidence of meniscal procedures performed in Denmark doubled from 2000 to 2011, with the largest increase in middle-aged and older patients. This increase contrasts with the mounting evidence showing no added benefit of arthroscopic partial meniscectomy over non-surgical treatments. Our observations illustrate the long delay in the dissemination, acceptance, and implementation of research evidence into the practice of arthroscopic surgery.
About 1 million arthroscopic knee procedures were performed in 2006 in the USA, of which at least 700,000 were meniscal resections (Cullen et al. Citation2009). Numbers from Sweden confirm that meniscal procedures are the most common arthroscopic knee procedures (Roos and Lohmander Citation2009). The Danish media have reported an increased frequency of meniscal procedures over recent years in Denmark, but the precise numbers, sex, and age distribution of the patients and underlying diagnoses have not been reported. In the same time period, several large, high-quality randomized controlled trials (Moseley et al. Citation2002, Herrlin et al. Citation2007, Kirkley et al. Citation2008) have failed to show any benefit of arthroscopic procedures including arthroscopic partial meniscectomy (APM) for middle-aged and older patients suffering from knee pain with or without concomitant features of radiographic knee osteoarthritis (OA) ().
Table 1. Randomized controlled trials comparing arthroscopy including arthroscopic partial meniscectomy with non-surgical interventions
Previous reports on the frequency of meniscal procedures have either been based on estimation from a number of hospitals (Cullen et al. Citation2009) or from insurance databases (Abrams et al. Citation2013). In Denmark, on the other hand, there is a national database on all healthcare procedures performed in public and private hospitals and clinics (Lynge et al. Citation2011). In addition, all Dasnish residents are registered in the Civil Registration System (Pedersen Citation2011) and population demographics are publicly available on the internet through Danish Statistics. This allows calculation of annual incidence rates for meniscal procedures based on the entire Danish population.
We examined the number of meniscal procedures performed in Denmark in the years between 2000 and 2011. We also examined age and sex distribution and the diagnosis registered for the patients undergoing these procedures, using data from the Danish National Patient Register.
Patients and methods
The Danish National Patient Register
All patient contacts with public and private hospitals and clinics in Denmark are registered in the Danish National Patient Register (DNPR) (Lynge et al. Citation2011). Administrative data include the unique personal identification number (the Central Person Register (CPR) number (Pedersen Citation2011), given to all residents of Denmark and registered in the Civil Registration System), hospital identification, date and time of activity, and patient’s municipality (among other characteristics). Clinical data include types of surgical procedures (according to the Nordic Classification of Surgical Procedures (NCSP)) and diagnosis (International Classification of Diseases (ICD-10)). A unique record number can be used to identify each patient contact with the hospital. This record number can be combined with the CPR number to track individual patient contacts within the hospital system.
Since 2000, the DNPR has formed the basis of payment of public and private hospital services via the Diagnostic Related Group (DRG) system (Lynge et al. Citation2011). It is assumed that registration is complete for public hospitals since 2000. For private hospitals and clinics, however, it is known that reporting is not complete, even though this has been mandatory since 2003. In 2008, it was estimated by the Danish National Board of Health that 5% of all private operations were missing in the DNPR (Lynge et al. Citation2011). Registration of orthopedic procedures has been reported to be correct in 92% of a sample of cases (inpatients and outpatients), and even better for outpatients alone, whereas numbers were lower for registration of diagnoses (primary diagnoses 83% and secondary diagnoses 77%), but again with better numbers for outpatients (Lass et al. Citation2006).
Study sample
Data were extracted from the DNPR on all record numbers containing a procedure code(s) for meniscal surgery (KNGD and all sub-codes) as the primary procedure or as part of other surgery in the twelve-year period 2000–2011. For each record, information was extracted on age, sex, diagnosis (primary and secondary), and surgical procedures in addition to meniscal surgery. The CPR number was used to track patients with several meniscal operations (defined as surgery on separate dates) during the study period. For patients with several surgery dates, it could not be determined whether surgery was carried out on the same knee—as left or right side is not registered systematically in the DNPR.
Definitions
Primary surgical procedure: meniscal surgery was considered the primary surgical procedure if the procedure was coded as “V” (V = most important surgical procedure in a finished contact) or “P” (P = most important procedure during a given surgery). Secondary surgical procedure: meniscal surgery was considered a secondary surgical procedure if it was coded as “D” (D = secondary procedure, part of a surgery without being the primary procedure). Thus, several surgical procedures could be conducted at the same surgery. Primary diagnosis: diagnosis coded as “A” (A = action diagnosis, the diagnosis that best describes the condition of a finalized contact) was considered the primary diagnosis. Secondary diagnosis: diagnosis coded as “B” (B = secondary diagnosis, diagnosis that supplements the description of an ended contact).
Incidence rates
Information on numbers of registered inhabitants in Denmark was retrieved from Danish Statistics (www.statistikbanken.dk). As mid-year data was not available, we estimated the mid-year population from numbers at the beginning and the end of each year in the period from 2000 to 2011. These numbers were used to calculate annual incidence rates per 100,000 persons in the age groups: 0–34 years, 35–55 years, and older than 55 years.
Statistics
We used chi-square test to assess differences in proportions of meniscal procedures performed on men and women as well as the defined age groups in 2000 as compared to 2011. A 2-sided unpaired Student’s t-test, assuming equal variances, was used to assess differences in mean age (with 95% confidence intervals (CIs)) of individuals undergoing meniscal procedures in 2000 as compared to 2011.
Ethics
Data were extracted from the DNPR with approval from Statens Serum Institut (study ID: FSEID 00000526), which is the Danish authority responsible for the DNPR. In addition, the study was approved by the Danish Data Protection Agency (study ID: 2013-41-1792), which must approve all extractions of personal data for research purposes from the DNPR. As the study only pertained to registry-based data, it could be conducted without permission from the Ethics Committee according to Danish legislation (Committee Act § 1, paragraph 1).
Results
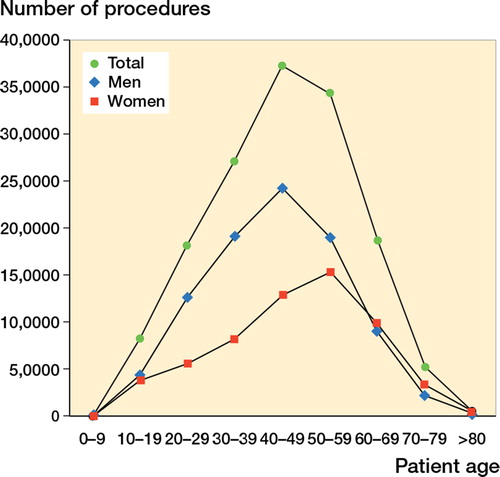
The incidence of meniscal procedures per 100,000 persons almost doubled between 2000 and 2011, with a particularly large increase (26%) observed from 2008 to 2009. While the incidence rate was stable in patients younger than 35 years, a doubling was observed for the middle-aged patients between 35 and 55 years of age. For those older than 55, we found a 3-fold increase in incidence rate between 2000 and 2011 (). This was reflected in a lower proportion of younger patients and a higher proportion of older patients in 2011 compared to 2000 (p < 0.001), which also showed in the increase in mean age of patients who underwent meniscal procedures—from 41 (CI: 41–42) in 2000 to 47 (CI: 46–47) in 2011 (). Middle-aged patients accounted for 50% of the total number of meniscal procedures in the years 2000–2011; the remaining procedures were equally divided between younger (25%) and older patients (25%). Meniscal procedures were carried out in men more frequently than in women (Figure), but the proportion of women increased from 2000 to 2011 (p < 0.001) ().
Table 2. Number of meniscal procedures (all codes) and incidence rate of meniscal procedures per year from 2000 through 2011, gender distribution, and mean age at surgery per year
Number of meniscal procedures in Denmark (all codes) divided into age groups for the years 2000–2011. Blue: men; red: women; and green: men + women.
The 151,228 meniscal procedures registered between 2000 and 2011 were performed on 148,819 individual patients. Most patients had 1 surgery with 1 meniscal procedure performed, while 1,863 patients had 2 or more meniscal procedures performed at the same operation. Furthermore, 520 patients had more than 1 operation involving procedures to the meniscus within the period 2000–2011. The majority of meniscal procedures (124,363, or 82%) were performed as the primary surgical procedure.
2 NCSP procedure codes accounted for 99% of all 151,228 meniscal procedures. These were KNGD11 (i.e. arthroscopic partial resection of meniscus in knee joint) and KNGD21 (i.e. arthroscopic re-insertion of meniscus in knee joint)—accounting for 92% and 7%, respectively. For those patients with meniscal procedures performed as a secondary surgical procedure (26,865 patients) the most common primary procedures (accounting for 87%) were: anterior cruciate ligament reconstruction (30%: KNGE45*, KNGE51, KNGE55), arthroscopic exploration (28%: KNGA11), synovectomy (18%: KNGF01, KNGF11), and cartilage resection (11%: KNGF31).
Five common diagnoses (i.e. old meniscal tear, traumatic meniscal tear, unspecific knee problems, osteoarthritis, and lesion/rupture of cruciate ligament) represented 80% of all primary diagnoses. Notably, the numbers of diagnoses of “old meniscus tear” and “traumatic meniscus tear” were similar in 2000 (i.e. 2,070 and 2,252, respectively), whereas the diagnosis “old meniscus tear” (n = 5,563) predominated over the diagnosis “traumatic meniscus tear” (n = 3,035) as the primary diagnosis in 2011. Six diagnoses represented 74% of all the secondary diagnoses ().
Table 3. Most common primary and secondary diagnoses for patients undergoing procedures to the meniscus in the period 2000–2011 in Denmark
Discussion
The incidence of arthroscopic meniscal procedures in Denmark almost doubled between 2000 and 2011. The largest relative increase in meniscal procedures (i.e. a 3-fold increase in incidence rate) was observed in patients older than 55, whereas the largest absolute increase (i.e. 4,481 procedures) occurred in the middle-aged population between 35 and 55 years of age. In contrast, the incidence rate of meniscal procedures in young patients under 35 was stable. These data suggest that the increased incidence of arthroscopic meniscal surgery mainly involved patients with degenerative meniscal tears, a condition known to be associated with an increased risk of knee osteoarthritis.
Coverage and validity is an important issue for all registries. The validity of registration of orthopedic procedure codes in Denmark has been reported to be good (correct in more than 92% of cases for outpatients), whereas numbers are less precise for diagnosis codes (Lass et al. Citation2006). It is generally assumed that registration has been complete for public hospitals since 2000, but it is known that reporting is not complete for private hospitals (5% of operations have been estimated to be missing in the DNPR by the Danish National Board of Health) even though this has been mandatory since 2003 (Lynge et al. Citation2011). In 2005, it was estimated that private payments accounted for around 15% of all healthcare expenses in Denmark (Folketinget Citation2007). Thus, the numbers in our study may have been underestimated, and some of the changes observed may have been due to variable completeness of reporting. Nevertheless, in comparison to other studies that have reported incidence rates of surgical procedures (Cullen et al. Citation2009, Abrams et al. Citation2013), the unique registration of all hospital contacts and concomitantly performed procedures in Denmark, along with the Danish population data, enable reliable estimation of time-related trends in surgical procedures.
Meniscal tears are often associated—by both healthcare professionals and lay-persons—with traumatic sports injuries in young, active individuals (Englund et al. Citation2012). However, reports from Sweden and the USA show that APM is most often performed in individuals between 45 and 64 years of age (Cullen et al. Citation2009, Roos and Lohmander Citation2009, Abrams et al. Citation2013) Other reports have shown that meniscal tears are also common in asymptomatic knees (Zanetti et al. Citation2003, Boks et al. Citation2006, Englund et al. Citation2007, Citation2008). Thus, meniscal tears as well as other structural abnormalities characteristic of knee OA (i.e. osteophytes, bone marrow lesions, cartilage damage, etc.) are common incidental findings at MRI examination of both asymptomatic and painful knees of middle-aged and older patients (Englund et al. Citation2008, Guermazi et al. Citation2012). Incidental meniscal lesions in these age groups are often of the “degenerative” type and frequently occur in the absence of a distinct trauma but in the presence of other structural joint changes characteristic of knee OA (Englund et al. Citation2008, Citation2009).
Taken together, these reports suggest that in the middle-aged and older population, any association between meniscal damage and the development of frequent knee pain exists because both pain and meniscal damage are related to knee OA and not because of a direct link between meniscal tears and pain (Englund et al. Citation2007, Citation2008). In our study, only about 17% of those treated with APM had knee OA as the primary or secondary diagnosis. However, the validity of this proportion is limited by the lack of clear diagnostic criteria for OA in the DNPR database, and perhaps also in clinical practice. It is notable that the most frequent primary diagnosis was “old meniscus tear”, which commonly occurs in the presence of osteoarthritic joint changes. This primary diagnosis increased 2.7 fold between 2000 and 2011, while the diagnosis of traumatic meniscal tear increased only by a factor of 1.3 in the same time period. Only 1 in 4 of the primary diagnoses were represented by “traumatic meniscus tear” or “anterior cruciate ligament tear”.
Consistent with the results from Sweden and the USA (Cullen et al. Citation2009, Roos and Lohmander Citation2009), we observed that middle-aged and older individuals accounted for 75% of all meniscal procedures in Denmark between 2000 and 2011. Of the 8,618 additional procedures performed in 2011 compared to 2000, essentially the entire increase was in those aged 35–55 years (4,481 procedures) and in those older than 55 (3,600 procedures). The increasing incidence of APM in the middle-aged and older groups between 2000 and 2011 is surprising, in light of the 3 high-quality randomized controlled trials (RCT) published in the same time period that failed to show any benefit of arthroscopic interventions including APM over and above that of placebo surgery, physiotherapy alone, or physiotherapy in combination with other medical treatments for patients in the same age groups, with or without features of knee osteoarthritis (Moseley et al. Citation2002, Herrlin et al. Citation2007, Kirkley et al. Citation2008) (). Further consolidating these results, 3 more recent RCTs and an extended follow-up of a previous RCT (Herrlin et al. Citation2013) showed no additional benefit of APM in combination with physiotherapy compared to physiotherapy alone for patients with meniscal tears and knee osteoarthritis (Katz et al. Citation2013), no superior effect of APM in comparison to 3 weeks of supervised exercise for middle-aged patients with meniscal tears (Yim et al. Citation2013), and no difference between APM and placebo surgery in middle-aged patients with meniscal tears and no features of knee OA (Sihvonen et al. Citation2013) (). The recent study by Sihvonen et al. (Citation2013) extended previous findings by showing that there was no benefit of APM for middle-aged or older patients with “degenerative” meniscal tears even in the absence of radiographic signs of osteoarthritis. Other studies comparing APM to placebo surgery (Hare et al. Citation2013) and APM to exercise (ClinicalTrials.gov Identifier: NCT01002794) are under way and may provide further information.
Arthroscopic surgery of the knee is considered to be low-risk surgery. However, the procedures discussed here have been reported to be associated with a 2–3% frequency of adverse events, including deep venous thrombosis, infections, surgical complications, cardiovascular events, pulmonary embolism, and death within 3 months (Noble et al. Citation1998, Wai et al. Citation2002, Salzler et al. Citation2013, Valdes et al. Citation2013). Some of these adverse events may represent avoidable harm.
In conclusion, a large increase in the incidence of arthroscopic meniscal procedures in middle-aged and older individuals occurred between 2000 and 2011 in Denmark. This increase took place in spite of increasing high-level evidence for a lack of added benefit provided by APM over other treatments in middle-aged and older individuals with and without features of knee OA. Our observations emphasize the long delay in the dissemination, acceptance, and implementation of high-level clinical evidence into the practice of arthroscopic surgery.
JBT and LSL conceived the study. JBT and KBH were responsible for the collection and analysis of data, and all the authors contributed to the interpretation of the data. JBT drafted the manuscript, which was critically revised by KBH and LSL. All the authors approved the final version of the manuscript.
The authors have no competing interests to declare. The study was supported by grants from the Danish Council for Independent Research | Medical Sciences (#12-125457).
- Abrams GD, Frank RM, Gupta AK, Harris JD, McCormick FM, Cole BJ. Trends in meniscus repair and meniscectomy in the United States, 2005-2011. Am J Sports Med 2013; 41 (10): 2333-9.
- Boks SS, Vroegindeweij D, Koes BW, Hunink MM, Bierma-Zeinstra SM. Magnetic resonance imaging abnormalities in symptomatic and contralateral knees: Prevalence and associations with tTraumatic history in general practice. Am J Sports Med 2006; 34 (12): 1984-91.
- Cullen KA, Hall MJ, Golosinskiy A. Ambulatory surgery in the United States, 2006. National Health Statistics Reports, National Center for Health Statistics 2009; 11: 1-28.
- Englund M, Niu J, Guermazi A, Roemer FW, Hunter DJ, Lynch JA, Lewis CE, Torner J, Nevitt MC, Zhang YQ, Felson DT. Effect of meniscal damage on the development of frequent knee pain, aching, or stiffness. Arthritis Rheum 2007; 56 (12): 4048-54.
- Englund M, Guermazi A, Gale D, Hunter DJ, Aliabadi P, Clancy M, Felson DT. Incidental meniscal findings on knee MRI in middle-aged and elderly persons. N Engl J Med 2008; 359 (11): 1108-15.
- Englund M, Guermazi A, Roemer FW, Aliabadi P, Yang M, Lewis CE, Torner J, Nevitt MC, Sack B, Felson DT. Meniscal tear in knees without surgery and the development of radiographic osteoarthritis among middle-aged and elderly persons: The Multicenter Osteoarthritis Study. Arthritis Rheum 2009; 60 (3): 831-9.
- Englund M, Roemer FW, Hayashi D, Crema MD, Guermazi A. Meniscus pathology, osteoarthritis and the treatment controversy. Nat Rev Rheumatol 2012; 8 (7): 412-9.
- Folketinget EU-Oplysningen (Økonomigruppen og 3. Udvalgssekretariat). Minianalyse: Sundhedssektoren i Danmark: Hvor stor er den, og hvad får vi for pengene? 2007.
- Guermazi A, Niu J, Hayashi D, Roemer FW, Englund M, Neogi T, Aliabadi P, McLennan CE, Felson DT. Prevalence of abnormalities in knees detected by MRI in adults without knee osteoarthritis: population based observational study (Framingham Osteoarthritis Study). BMJ 2012; 345: e5339.
- Hare KB, Lohmander LS, Christensen R, Roos EM. Arthroscopic partial meniscectomy in middle-aged patients with mild or no knee osteoarthritis: a protocol for a double-blind, randomized sham-controlled multi-centre trial. BMC Musculoskelet Disord 2013; 14: 71.
- Herrlin S, Hallander M, Wange P, Weidenhielm L, Werner S. Arthroscopic or conservative treatment of degenerative medial meniscal tears: a prospective randomised trial. Knee Surg Sports Traumatol Arthrosc 2007; 15 (4): 393-401.
- Herrlin SV, Wange PO, Lapidus G, Hallander M, Werner S, Weidenhielm L. Is arthroscopic surgery beneficial in treating non-traumatic, degenerative medial meniscal tears? A five year follow-up. Knee Surg Sports Traumatol Arthrosc 2013; 21 (2): 358-64.
- Katz JN, Brophy RH, Chaisson CE, de Chaves L, Cole BJ, Dahm DL, Donnell-Fink LA, Guermazi A, Haas AK, Jones MH, Levy BA, Mandl LA, Martin SD, Marx RG, Miniaci A, Matava MJ, Palmisano J, Reinke EK, Richardson BE, Rome BN, Safran-Norton CE, Skoniecki DJ, Solomon DH, Smith MV, Spindler KP, Stuart MJ, Wright J, Wright RW, Losina E. Surgery versus physical therapy for a meniscal tear and osteoarthritis. N Engl J Med 2013; 368 (18): 1675-84.
- Kirkley A, Birmingham TB, Litchfield RB, Giffin JR, Willits KR, Wong CJ, Feagan BG, Donner A, Griffin SH, D’Ascanio LM, Pope JE, Fowler PJ. A randomized trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med 2008; 359 (11): 1097-107.
- Lass P, Lilholt J, Thomsen L, Lundbye-Christensen S, Enevoldsen H, Simonsen OH. The quality of diagnosis and procedure coding in Orthopaedic surgery Northern Jutland. Ugeskrift for læger 2006; 168 (48): 4212-5.
- Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Public Health (7 Suppl) 2011; 39: 30-3.
- Moseley JB, O’Malley K, Petersen NJ, Menke TJ, Brody BA, Kuykendall DH, Hollingsworth JC, Ashton CM, Wray NP. A Controlled Trial of Arthroscopic Surgery for Osteoarthritis of the Knee. N Engl J Med 2002; 347 (2): 81-8.
- Noble J, Ilango B, Obeid M. Complications of arthroscopy of the knee. The Knee 1998; 5: 1-8.
- Pedersen CB. The Danish Civil Registration System. Scand J Public Health (7 Suppl) 2011; 39: 22-5.
- Roos E, Lohmander S. Young patients—old knees. Knee problems in the middle age often osteoarthritis. Läkartidningen 2009; 106 (24-25): 1645-8.
- Salzler MJ, Lin A, Miller CD, Herold S, Irrgang JJ, Harner CD. Complications after arthroscopic knee surgery. Am J Sports Med 2013; 42(2): 292-6.
- Sihvonen R, Paavola M, Malmivaara A, Itala A, Joukainen A, Nurmi H, Kalske J, Jarvinen T LN. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. New Engl J Med 2013; 369 (26): 2515-24.
- Valdes AM, Suokas AK, Doherty SA, Jenkins W, Doherty M. History of knee surgery is associated with higher prevalence of neuropathic pain-like symptoms in patients with severe osteoarthritis of the knee. Semin Arthritis Rheum 2013: [Epub ahead of print]
- Wai EK, Kreder HJ, Williams JI. Arthroscopic debridement of the knee for osteoarthritis in patients fifty years of age or older: Utilization and outcomes in the province of Ontario. J Bone Joint Surg (Am) 2002; 84 (1): 17-22.
- http://www.statistikbanken.dk - accessed Nov 13. Danish Statistics (Danmarks Statistik).
- Yim JH, Seon JK, Song EK, Choi JI, Kim MC, Lee KB, Seo HY. A Comparative study of meniscectomy and nonoperative treatment for degenerative horizontal tears of the medial meniscus. Am J Sports Med 2013; 41 (7): 1565-70.
- Zanetti M, Pfirrmann CW, Schmid MR, Romero J, Seifert B, Hodler J. Patients with suspected meniscal tears: Prevalence of abnormalities seen on MRI of 100 symptomatic and 100 contralateral asymptomatic knees. AJR Am J Roentgenol 2003; 181 (3): 635-41.
