Abstract
Background — The mechanism of failure of metal-on-metal (MoM) total hip arthroplasty (THA) has been related to a high rate of metal wear debris, which is partly generated from the head-trunnion interface. However, it is not known whether implant fixation is affected by metal wear debris.
Patients and methods — 49 cases of MoM THA in 41 patients (10 women) with a mean age of 52 (28–68) years were followed with stereoradiographs after surgery and at 1, 2, and 5 years to analyze implant migration by radiostereometric analysis (RSA). Patients also participated in a 5- to 7-year follow-up with measurement of serum metal ions, questionnaires (Oxford hip score (OHS) and Harris hip score (HHS)), and measurement of cup and stem positions and systemic bone mineral density.
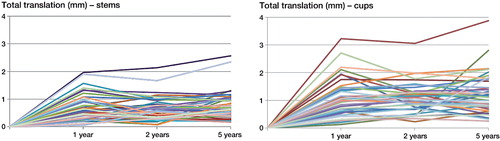
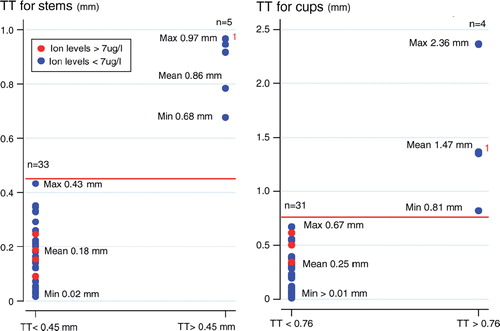
Results — At 1–2 years, mean total translation (TT) was 0.04 mm (95% CI: –0.07 to 0.14; p = 0.5) for the stems; at 2–5 years, mean TT was 0.13 mm (95% CI: –0.25 to –0.01; p = 0.03), but within the precision limit of the method. For the cups, there was no statistically significant TT or total rotation (TR) at 1–2 and 2–5 years. At 2–5 years, we found 4 cups and 5 stems with TT migrations exceeding the precision limit of the method. There was an association between cup migration and total OHS < 40 (4 patients, 4 hips; p = 0.04), but there were no statistically significant associations between cup or stem migration and T-scores < –1 (n = 10), cup and stem positions, or elevated serum metal ion levels (> 7µg/L (4 patients, 6 hips)).
Interpretation — Most cups and stems were well-fixed at 1–5 years. However, at 2–5 years, 4 cups and 5 stems had TT migrations above the precision limits, but these patients had serum metal ion levels similar to those of patients without measurable migrations, and they were pain-free. Patients with serum metal ion levels > 7 µg/L had migrations similar to those in patients with serum metal ion levels < 7 µg/L. Metal wear debris does not appear to influence the fixation of hip components in large-head MoM articulations at medium-term follow-up.
Metal-on-metal (MoM) hip articulations allow the use of larger-diameter femoral head sizes than other constrained articulation types like metal-on-polyethylene (MoP) and ceramic-on-ceramic (CoC) total hip arthroplasties (THAs), where a liner must be interpositioned between the femoral head and the metal shell. Large-diameter MoM hip articulations more closely mimic the natural human anatomy; they improve joint stability and reduce the incidence of postoperative dislocation (Krantz et al. Citation2012). Furthermore, they reduce the volume of wear particles, which has been considered advantageous from a quality and bearing perspective since wear particles from in MoP bearings are clearly associated with osteolysis and aseptic loosening in THA. MoM hip articulations have therefore been recommended worldwide in the past decade and used for younger patients with high activity levels. Although volumetric wear rates at the surfaces of MoM bearings are 20 times lower than those of conventional MoP bearings, and although the wear particles are typically smaller than 50 nm (Doorn et al. Citation1998), the number of nano-sized metal particles generated is up to 500 times higher than for MoP bearings (Sieber et al. Citation1999, Mabilleau et al. Citation2008). These nano-sized metal particles and metal ions from the MoM bearing and the trunnion of the neck junction are spread both locally and systemically. Phagocytosis of the nano-sized metal particles impairs osteoblastic activity, which may contribute to the cellular events that occur during aseptic loosening and soft tissue destruction (Lohmann et al. Citation2000).
No previous studies have investigated the implant stability of large-head MoM THAs, and only a few studies have evaluated the stability of MoM hip resurfacing articulations (RHAs) (Glyn-Jones et al. Citation2004, Itayem et al. Citation2005, Citation2007, Baad-Hansen et al. Citation2011, Penny et al. Citation2012, Lorenzen et al. Citation2013).
We hypothesized that MoM implant migration would be more extensive in patients with elevated serum metal ion levels than in patients whose serum metal ion levels were within the acceptable range (< 7 µg/L), and that MoM implants would be well-fixed in those with acceptable serum metal ion levels.
Patients and methods
A consecutive series of 41 patients who were below 65 years of age at the time of surgery and who had been diagnosed with either osteoartrosis (n = 24), sequelae of hip dysplasia (n = 6), or necrosis of the femoral head (n = 11) underwent large-head MoM THA at Aarhus University Hospital, Denmark, between August 2006 and October 2007. Exclusion criteria were fertile women and patients who were included in another ongoing research project at the department. Patients were followed with RSA postoperatively and at 1, 2 (double examinations), and 5 years—and with conventional radiographs postoperatively and at 5 years. In 2012, we completed a 5- to 7-year follow-up examination of all 41 patients with large-head MoM THA (31 men), mean age 52 (28–68) years. We considered elevated chromium and/or cobalt levels (> 7 µg/L) to be a potential risk factor for MoM implant migration.
Surgery
3 experienced orthopedic surgeons undertook the operations. A posterolateral approach was used in all patients, and all of them received an M2a-Magnum articulation. Patients were instructed to walk with weight bearing as tolerated for the first 6 weeks after surgery; thereafter, free loading and activity were allowed. 2 patients had postoperative complications: 1 had a superficial infection, which was treated with intravenous antibiotics (dicloxacillin), and the other had a temporary ischial nerve affection. 13 patients had bilateral hip articulations: 8 were bilateral M2a-Magnum articulations and the remaining 5 consisted of 3 hip resurfacing THAs (2 ReCap (Biomet) and 1 Birmingham Resurfacing Hip), 1 metal-on-ceramic (MoC) THA (DePuy), and 1 MoP THA (Biomet). 4 of the 8 bilateral M2a-Magnum articulations had only been followed with RSA on the left hip. For a correct statistical analysis, we excluded the right-hip data of those patients who had had bilateral M2a-Magnum articulations followed by RSA on both hips (4 hips) (bilateral hip-joint operations had been performed during the same operation). Right-hip data are presented in Table 1 (see Supplementary data).
Prosthesis
Cementless Bi-Metric proximal hydroxyapatite (HA)-coated stems with MoM M2a-Magnum femoral heads and ReCap acetabular solid shells (Biomet Inc., Warsaw, IN) were used in all patients. The ReCap acetabular press-fit cup and the M2a-Magnum head are made of an “as-cast” high-carbon cobalt-chromium-molybdenum (CoCrMo) alloy. The system is modular at the head-neck junction. The head size is dependent upon the cup size, with the neck length being adjusted via adaptors inserted into the femoral head. The outer diameter of the ReCap cup is fully hemispherical (180°). It has 4 rim indentations for stable attachment of the locking impaction device. It is 6 mm thick at the dome and on average 3 mm thick at the rim. The radial clearance level of the M2a-Magnum articulation is maintained at 75–150 μm (Biomet design rationale). The stem and taper are made of titanium, aluminum, and vanadium alloy (TiAlVa) and lateralized stems have an increased taper and trunnion length.
Radiostereometric analysis
3–6 intraoperative 1.0-mm tantalum markers were inserted into the greater trochanter and another 4 into the lesser trochanter, forming a rigid-body reference. 2 fixed radiographic tubes with a 40° angle between them were positioned above the patient. MB-RSA version 3.2 (RSAcore, Leiden, the Netherlands) was used to calculate the implant migration. Stereoradiographs were obtained within the first postoperative week and at the 1-, 2-, and 5-year follow-ups. Implant migration was assessed on all 5 stereoradiographs using the postoperative stereoradiograph as the reference. The point of measurement was the center of gravity of the 3-dimensional computer-aided design (3D CAD) surface model/marker model in relation to the bone markers serving as the fixed rigid-body reference. Translations (implant movement along the axes) were expressed as x-translations (medial/lateral direction), y-translations (distal/proximal direction), and z-translations (anterior/posterior direction). Rotations were expressed as rotations about the x-axis (anterior/posterior), rotations about the y-axis (external/internal rotations), and rotations about the z-axis (adduction/abduction). The total translation (TT) and the total rotation (TR) were calculated by use of the Pythagorean theorem (TT = √(x2 + y2 + z2) and TR = √(x2 + y2 + z2)). The mean error of rigid-body-fitting, which represents the stability of the markers used for migration analysis, was set to 0.50 mm. An upper limit of ≤ 150 for the condition number (CN) has been suggested (Valstar et al. Citation2005). For the cups, the mean CN was 67 (95% CI: 53–80); for the stems, it was 26 (95% CI: 20–32). The mean difference in matching of the surface cup and the stem models to the radiographic contours was 0.15 (95% CI: 0.13–0.17) for the cups and 0.24 (CI95% CI: 0.22–0.26) for the stems.
Precision and sample size of radiostereometric analysis
The precision of the RSA analyses was assessed by “double examination” of all patients (Valstar et al. Citation2005). 2 pairs of stereoradiographs from the same patient were recorded within 10–15 min at the 2-year follow-up. The postoperative stereoradiograph was used as the reference in migration analysis of the double examinations, and the expected difference in displacement between the 2 calculations represented the systematic error of the RSA system (bias); it should (optimally) be equal to zero. The mean difference between the double examinations is the systematic error of the system. The standard deviation of the difference between the 2 examinations (SD dif.) reflects the precision of the RSA results. The coefficient of repeatability (CR) (± 1.96 × SD dif.) reflects the lower limit within which it is possible to detect prosthetic migration on the individual basis of the system (Altman 2009) (Table 2, see Supplementary data). All RSA analyses of implant migrations were performed in consensus between 2 observers. Owing to the high precision of RSA, it is possible to identify an excessively migrating prosthesis, and failure can be predicted with a sample size of 15–25 patients (Valstar et al. Citation2005).
Serum metal ion measurements
At the 5- to 7-year follow-up, blood samples were collected from all patients according to recent guidelines (MacDonald et al. Citation2004). The first 3 samples in each case were used for other blood examinations to avoid chromium contamination from the steel needle (Penny and Overgaard Citation2010, Papageorgiou et al. Citation2007). The blood was collected in 6.0-mL Trace Element Serum (13 × 100 mm KFK359 tubes; 368380; BectonDickinson, Franklin Lakes, NJ) (BD 2013) and centrifuged to separate the serum. All serum samples were examined by inductively coupled plasma mass spectrometry (ICP-MS) at Vejle Hospital, Denmark. We considered elevated levels of chromium and cobalt in the serum to be > 7 µg/L (CitationMHRA 2010). Serum levels of leukocytes, CRP, creatinine, and GFR were also analyzed to screen for infection and renal impairment. All patients returned a questionnaire about possible work- or leisure-related chromium or cobalt exposure. We enquired about the patients’ oral intake of minerals, if they had any tattoos, their profession, and about pastime activities involving cement, pottery glaze, or metal.
Dual-energy X-ray absorptiometry scans
Dual-energy X-ray absorptiometry (DXA) scans were performed at the 5- to 7-year follow-up with a GE Lunar Prodigy Advance 2005 DXA scanner; analyses were performed using enCORE software version 11.40. Bone mineral density (BMD) was measured in the lumbar spine and, if possible, in the femoral neck to assess the skeletal status of all patients. T-scores were interprented as recommended by the World Health Organization; T-scores of between –1 and –2.5 were classified as osteopenia, and T-scores below –2.5 were classified as osteoporosis. In the data analysis, osteopenia and osteoporosis were combined into one group designated “low BMD”; and T-scores between –1 and 4 in all anatomical areas were designated “normal BMD”.
Radiography and clinical outcome measures
At the 5- to 7-year follow-up, conventional radiographs and stereoradiographs of the pelvis and hip were assessed. During all stereoradiographs, the patients assumed standard positions: supine, body parallel to the examination table, and the big toes pointing straight up. Cup and stem positions were read from the model-based (MB) RSA software (RSAcore, Leiden, the Netherlands) using the positions of the fitted models on the 5-year stereoradiographs. The Harris hip score (HHS) (Harris Citation1969) (range 0–100) and the Oxford hip score (OHS) (range 0–48) were recorded at the 5- to 7-year follow-up. HHS scores from 90–100 and OHS scores from 40–48 were categorized as an excellent outcome, and scores below these levels were considered to be a risk factor for MoM implant migration.
Statistics
All continuous variables were tested for normality (Shapiro-Wilk test). When data were not normally distributed, non-parametric tests (Mann-Whitney U-test and Wilcoxon rank-sum test) were used. When data were normally distributed, Satterthwaite’s t-test was used. Calculations of the correlation coefficient (r) of independent variables were assessed using Spearman correlation analysis. Any p-value below 0.05 was considered statistically significant. All analyses were performed using STATA software version 11.
Ethics
All patients gave their informed consent regarding participation in this investigation. Data were kept anonymous and were treated confidentially. The follow-up was performed in accordance with the Helsinki Declaration II. The study was reported to the local ethics committee who accepted it as a quality study of the M2a THA, and it was approved by the Danish Data Protection Agency (June 27, 2012, journal no. 2007-58-0010).
Results
Radiostereometric analysis
2 patients had no tantalum markers in the femur (1 bilateral), 7 cups (2 bilateral cases) could not be analyzed due to inadequate visualization of the tantalum markers (n = 3) or due to marker instability (n = 4), and 1 patient did not turn up for the 2-year RSA examination. This left 39 stems (36 cups) available for the 1- and 5-year RSA analyses and 38 stems (35 cups) for the 2-year double RSA analyses. Results of the 5-year RSA migrations are presented in .
Table 3. Translations (mm) and rotations (°) for cups and stems at 5-year follow-up
Stem migration (TT) was not significant (p = 0.5) between the first year and the second year. However, between the second and the fifth year, mean stem migration (TT) was 0.13 mm (95% CI: –0.25 to 0.01), which was a significant (p = 0.03) but clinically very small migration (, 2, and ). 5 male patients had stem migration above the detection limit (0.45 mm) from the second to the fifth year. These 5 patients had a mean TT of 0.86 (range 0.68–0.97) mm, which was different from that of patients without any measurable migration (n = 33; p < 0.001) (). However, all 5 patients had serum metal ion levels below the recommended threshold level (7 µg/L), and serum metal ion levels were similar in patients with (n = 5) and without (n = 33) measurable stem migrations (p=0.65). There was no statistically significant subsidence (p = 0.1) or anteversion (p = 0.9) for the stems from the first to the fifth year. The cups had no measurable TT or TR during any of the time intervals (p > 0.06) (, 2, and ). Between the second and the fifth year, 4 patients had cup migrations above the TT detection limit (0.76 mm), with a mean of 1.47 (range 0.81–2.36) mm, and these cup migrations (n = 4) were significantly different from the migrations of cups (n = 31) that migrated below the detection limit (p < 0.001) (). However, there was no difference in serum metal ion levels were similar in patients with and without measurable cup migrations (p = 0.61). At 5 years, the mean proximal cup migration was 0.46 mm (95% CI: 0.30–0.62), which was similar to the 1-year (p = 0.91) and the 2-year (p = 0.80) levels of cup migrations. There was an association between total OHS below 40 (n = 4) and cup migration (p = 0.04).
Figure 1. Box plots of total translations (mm) in cups and stems at the 1-, 2-, and 5-year follow-up. The line in each box marks the median, the box shows the interquartile range, and the whiskers show the tenth and ninetieth percentiles.
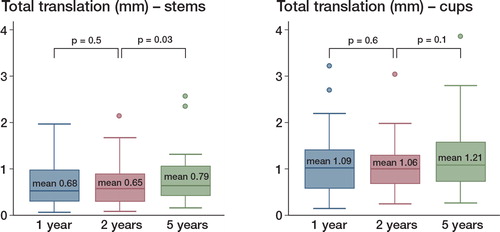
Figure 4. Dichotomized total translation (TT) for stems and cups between the second and the fifth year. Patients who had migrations above the precision limit of the method are represented on the right side of the plots, and patients with elevated serum metal ion concentrations are marked with red dots. The TT precision limit was 0.45 mm for stems and 0.76 mm for cups. 1 patient had both cup and stem migrations with TT above the precision limits (denoted 1)
Serum metal ion measurements
At the 5- to 7-year follow-up, serum ion concentrations were obtained from 41 patients. The mean cobalt level was 2.64 (0.57–21.5) µg/L and the mean chromium level was 3.79 (0.57–28.37) µg/L. In total, 4 patients (6 hips) had elevated serum metal ion concentrations (> 7 µg/L). Of these, 2 patients reported a clicking or squeaking hip. According to the questionnaires on possible chromium or cobalt exposure, 2 patients had a tattoo and 1 patient worked with cement, but none of these patients had chromium or cobalt levels above 2.5 µg/l. The mean femoral head size in women was 46 (SD 3, range 42–52) and in men it was 50 (SD 3, range 46–54). The mean cup inclination angle was 45° (35–59), the mean cup anteversion angle was 17° (1–29), and the mean stem anteversion angle was 19° (2–35). Component positions between the sexes were similar (p > 0.09). Cup inclination angles > 50° were associated with higher levels of both chromium and cobalt (p = 0.004 and p = 0.006); the same was the case for female gender (p = 0.02 and p = 0.03) and for patients with femoral head sizes < 50 and higher levels of chromium (p = 0.03) but not of cobalt (p = 0.25).
DXA scans
The mean T-score in the low-BMD group (n = 10) was –1.92 (–2.40 to –1.40) and the mean T- score in the normal-BMD group (n = 29) was 0.44 (–0.01 to 0.90). Low BMD did not affect the magnitude of stem migration (TT) (p = 0.2), and there was no significant association between low BMD and elevated levels of serum chromium (p = 0.3) or cobalt (p = 0.2).
Radiography and clinical outcome measures
The conventional radiographs revealed that in the period between the postoperative radiographs and the 5-year radiographs, 3 radiolucent lines (RLLs) and 2 small osteolyses in DeLee zones I and II around the cup had appeared, but they were not associated with elevated serum chromium and/or cobalt levels. There were no RLLs or osteolyses around the stem.
The mean OHS was 43 (8–48) and mean HHS was 89 (12–96). 2 patients had poor OHS and HHS outcome scores. One of these patients had been in a motorcycle accident prior to his hip surgery, and his low scores (HHS of 12 and OHS of 8) were related to neuropathic pain and a prolapsed disc, and at the 5-year follow-up he had almost no walking ability. His serum chromium and cobalt levels were 1.64 µg/L and 0.88 µg/L, respectively, and magnetic resonance imaging (MRI) and computed tomography (CT) scans were normal. Another male patient with an HHS of 62 and an OHS of 12 had experienced hip pain since undergoing MoM THA. His serum chromium and cobalt levels were 0.70 µg/L and 1.53 µg/L, respectively, and MRI and ultrasonography scans were normal. The patient was revised to a traditional MoP THA upon request, due to pain. During revision, the surgeon observed metallosis around the hip joint, but no cystic or solid masses. Both cup and stem were well-fixed. Septic lymphocyte-dominated vasculitis-associated lesion (ALVAL) scores were low (1–2). So far, the patient has been without pain since revision.
Discussion
The aim of this 5- to 7-year longitudinal cohort study was to assess the stability of large-head MoM THA implants (ReCap Shell/M2a-Magnum head/Bi-Metric stem) and to investigate whether migration was more extensive in patients with elevated serum metal ion levels than in patients with acceptable serum metal ion levels. The mean migration of cups and stems indicated that, in general, the implants were well-fixed, and we found no association between MoM implant migration and elevated serum metal ions. Between the second and the fifth year, 5 stems and 4 cups (in 8 patients) had migrations above the TT detection limit, yet no stem migrated more than 1 mm TT and no cup migrated more than 2.36 mm TT, and these 8 patients were asymptomatic. We found no association between MoM implant migration and elevated serum chromium or cobalt levels.
Migration of the ReCap cup
The cups showed no statistically significant migration (TT or TR) during any of the time intervals. However, between the second and fifth year, 4 patients had measurable TT, i.e. migration above the detection limit of 0.76 mm TT. For acetabular cups, Nieuwenhuijse et al. (Citation2012) suggested that the risk of aseptic loosening is increased in the presence of a sagittal rotation of 2.53° and a proximal migration of 1.76 mm within the first 2 postoperative years (Nieuwenhuijse et al. Citation2012). In a systemic review and meta-analysis of 26 RSA studies and 49 survival studies, Pjils et al. (2012) found that cups with a 2-year proximal migration of between 0.2 and 1.0 mm were “at risk” of having revision rates above 5% at the 10-year postoperative check-up, and a proximal migration above 1 mm was “unacceptable”, as revision rates were above 5% at 10 years postoperatively (Pijls et al. Citation2012). Comparing our results with those of Nieuwenhuijse et al. (Citation2012), we did not find any cups with a 2-year proximal cup migration above 1.76 mm, but 2 cups had sagittal cup rotations above 2.53° (i.e. 3.28° and 3.34°). When comparing the proximal cup migrations that we found reported here to the classification by Pijls et al. (Citation2012), we identified 17 cups “at risk” of revision (range 0.24–0.77) and 7 cups with “unacceptable” migrations (range 1.01–1.34). However, since our detection limit for proximal migration was 0.31 mm, any individual cup migration below this limit may be regarded as estimation uncertainty—not cup migration. Patients with cup migrations above the recommendations by Nieuwenhuijse et al. (Citation2012) and Pjils et al. (2012) were asymptomatic and had low serum metal ion levels.
Some RSA studies have evaluated the fixation in different brands of MoM hip resurfacing arthroplasties (HRAs): 2 of the ReCap (Biomet) (Baad-Hansen et al. Citation2011, Lorenzen et al. Citation2013), 2 of the Birmingham Hip Component (BHR) (Smith & Nephew) (Glyn-Jones et al. Citation2004, Itayem et al. Citation2005, Citation2007), and 1 of the ASR (DePuy) (Penny et al. Citation2012). They all reported small total migrations of the resurfacing femoral component compared to those of conventional stems. Only the study of the BHR components also analyzed migration of the acetabular cup. The BHR cup and the ReCap cup have some similarities, as they are both made of as-cast material, they are fully hemispheric (180°), and they have a similar wall thickness at the rim; however, the coating in the bone-implant interface is different with a porous titanium plasma-spray hydroxyapatite-coated surface for the ReCap cups and a single layer of integrally cast CoCr-alloy bead-surface coated with hydroxyapatite for the BHR cups. At 5 years, the mean micromovement of the BHR acetabular cup was reported to be less than 0.11 mm (SD 0.26) for translations and less than 0.52° (SD 0.86) for rotations. These micromovements were smaller than those observed for the ReCap cup in our study, which indicates that the BHR acetabular cup is more stable than the ReCap cup. However, migrations of the BHR cup were measured by marker-based RSA and we used model-based RSA; thus, the size and shape of models used for analysis of implant migration were not alike. The precision of marker-based RSA depends on the configuration and the number of tantalum beads added to the shell and polyethylene, whereas the precision of model-based RSA depends on the geometry of the outer contour of an implant. Model-based RSA has a slightly lower precision than marker-based RSA, especially for the rotations (Kaptein et al. Citation2006, Lorenzen et al. Citation2013). We used model-based RSA for all analyses, and the symmetrical design of the hemispheric ReCap cup hampered the fitting of the cup model to the implant counter on the stereoradiographs—as there are only a few benchmarks (4 small flanches) on the outer surface of the cup, and these may not be visible in all patient-individual serial stereoradiographs. Furthermore, the large M2a-Magnum head made it difficult to differentiate between the contour of the head and the edge of the ReCap cup. Model-based and marker-based RSA methods have different precisions for different prosthetic designs and possible marker configurations, and comparison between studies using different models is therefore problematic (Baad-Hansen et al. Citation2007, Lorenzen et al. Citation2013). We found the ReCap cup to be stable until the 5-year follow-up, although migrations were more extensive than those observed in a slightly different MoM hip arthroplasty acetabular cup (Itayem et al. Citation2007).
Migration of the Bi-metric stem
We observed 2 statistically significant movements of the Bi-Metric stem; between the second and the fifth year, the mean TT for the stems was 0.13 mm (p = 0.03); and between the first and the second year, the mean TR was 0.32° (p = 0.04). However, both movements were clinically very small and within the detection limits of the method, and they may therefore be regarded as instances of estimation uncertainty. Patients with stem migration (TT) above the precision limits (n = 5) were all asymptomatic and had serum chromium and cobalt concentrations below 7 µg/L.
Within the first year, the mean Bi-Metric stem migration (TT) was 0.68 mm, and at the 5-year follow-up it had increased to 0.79mm, which indicates that the stems mainly migrated during the first year. Previous short-term RSA studies on uncemented stems have likewise identified maximum migration within the first year (Soballe et al. Citation1993, Bottner et al. Citation2005, Grant et al. Citation2005, Strom et al. Citation2007, Campbell et al. Citation2011, Lazarinis et al. Citation2013). After this period, most successful stems migrate at low rates for the following 5–10 years. Stems that fail prematurely will show continuous migration; thus, it is essential to assess the individual implant migration. Subsidence is a clinically important measure of stem fixation. A subsidence level of 1.2 mm at 2-year follow-up has been found to be a strong indicator of early or medium-term revision for the cemented cobalt-chromium Lubinus SP 1 prosthesis (LINK) (Karrholm et al. Citation1994). At 2 years, the Bi-Metric stems analyzed in our study had moved proximally by a mean distance of 0.10 mm, which is below the suggested risk limit and also below the detection limit for the y-axis of 0.43mm. The individual subsidence patterns revealed 1 stem with a 1-year subsidence of 1.7 mm, which is above the suggested limit of 1.2 mm; but between the first and the fifth year, this stem remained stable. However, the quantity of subsidence may be an indicator of later failure; it may not be the failure mechanism for all stem types, and different stems may have different migration patterns that can be deemed safe for good outcome (Gruen et al. Citation1979). The Bi-Metric stem has previously given excellent results, with a 10-year survival rate of 100% in patients with juvenile chronic arthritis (Lyback et al. Citation2004), and the Finnish Arthroplasty Register reported a 15-year survival rate of 95% (Eskelinen et al. Citation2006). We found 5 asymptomatic patients with stem migrations (TT) above the detection limit (range 0.68–0.97 mm), and these patients will be followed more closely in the future. No stems were revised and, apart from the 5 patients with measurable stem migrations, the individual migration patterns were in general not progressive or suggestive of loosening.
Serum metal ion measurements and DXA scans
We found that elevated serum metal ion levels were significantly associated with cup inclination angles above 50°, femoral head sizes below 50, and female sex. Previous studies have made similar observations, and it has been suggested that these factors may influence serum metal ion levels (Vendittoli et al. Citation2007, De et al. Citation2008, Hart et al. Citation2008, Citation2009, Langton et al. Citation2008, Desy et al. Citation2011). Even though we examined these associations from a relatively small number of patients, we judge them to be valid as they are comparable with and supportive of those found in previous studies of MoM hip articulations. We found no association between low systemic BMD and cup or stem migration. In patients with cemented THAs, low systemic BMD and bone reduction in Gruen zones 1 and 7 have been found to be predictive of late stem loosening (Nixon et al. Citation2007), but no association between periprosthetic bone loss and stem migration has been shown, as evaluated by RSA (li et al. Citation2007).
Conclusion
The majority of all cups and stems were well-fixed between 1 and 5 years after surgery. Between the second and the fifth year, 4 cups and 5 stems had migrations (TT) above the detection limit, but these measurable migrations were clinically small, the patients were asymptomatic, and they had serum metal ion levels similar to those in patients without MoM implant migration. Furthermore, patients with elevated serum metal ion levels had migration patterns comparable to those of patients with acceptable serum metal ion levels. Migration of the ReCap cup or the Bi-Metric stem of M2a-Magnum components is apparently not associated with elevated serum metal ion levels—and vice versa, elevated serum metal ion levels are not associated with more extensive migration of the cup and stem components at medium-term follow-up.
The RSA results of this study suggest that in future, good long-term fixation of the Bi-Metric stem and the ReCap acetabular cup of the M2a Magnum components can be expected. Although aseptic loosening and wear are 2 important reasons for implant failure, which can both be predicted by RSA, implant failure may also have other causes, and the absence of implant migration in RSA studies does not guarantee good long-term results. In agreement with the guidelines on RSA of implants and the guidelines for follow-up of MoM hip articulations, we will continue to follow this patient group with serum metal ion measurements, clinical observations, and radiological measurements including stereoradiography to evaluate the longer-term results.
Supplementary data
Figure 2 and Tables 1 and 2, are available at Acta’s website (www.actaorthop.org), identification number 6563.
Supplementary Material
Download PDF (165.6 KB)KS, MS, IM, NDL, JSS, and MHH were involved in the follow-up examinations. MH, MS, and IM performed the statistical analyses and the interpretation. MH wrote the initial manuscript and MS, IM, KS, JSS, and NDL helped revise it. All authors approved the final manuscript.
We thank Lone L(please check)vgren, Rikke M(please check)rup, and Inger Krog-Mikkelsen for their help in arranging the follow-up, and especially Rikke M(please check)rup for her supervision and help in analyzing the stereoradiographs.
No competing interests declared.
- Baad-Hansen T, Kold S, Kaptein BL, Soballe K. High-precision measurements of cementless acetabular components using model-based RSA: an experimental study. Acta Orthop 2007; 78 (4): 463-9.
- Baad-Hansen T, Storgaard JS, Soballe K. Two-year migration results of the ReCap hip resurfacing system-a radiostereometric follow-up study of 23 hips. Int Orthop 2011; 35 (4): 497-502.
- BD. http://www.bd.com/resource.aspx?IDX=10155. 2013.
- Biomet. M2a-Magnum large metal articulation: design rationale, 2009. http://www.biomet.com/campaign/trueAlternativeBearings/BOI03400MagnumDesignRationale.pdf. 2013.
- Bottner F, Zawadsky M, Su EP, Bostrom M, Palm L, Ryd L, Sculco TP. Implant migration after early weightbearing in cementless hip replacement. Clin Orthop 2005; (436): 132-7.
- Campbell D, Mercer G, Nilsson KG, Wells V, Field JR, Callary SA. Early migration characteristics of a hydroxyapatite-coated femoral stem: an RSA study. Int Orthop 2011; 35 (4): 483-8.
- De HR, Pattyn C, Gill HS, Murray DW, Campbell PA, De SK. Correlation between inclination of the acetabular component and metal ion levels in metal-on-metal hip resurfacing replacement. J Bone Joint Surg (Br) 2008; 90 (10): 1291-7.
- Desy NM, Bergeron SG, Petit A, Huk OL, Antoniou J. Surgical variables influence metal ion levels after hip resurfacing. Clin Orthop 2011; (469) (6): 1635-41.
- Doorn PF, Campbell PA, Worrall J, Benya PD, McKellop HA, Amstutz HC. Metal wear particle characterization from metal on metal total hip replacements: transmission electron microscopy study of periprosthetic tissues and isolated particles. J Biomed Mater Res 1998; 42 (1): 103-11.
- Eskelinen A, Remes V, Helenius I, Pulkkinen P, Nevalainen J, Paavolainen P. Uncemented total hip arthroplasty for primary osteoarthritis in young patients: a mid-to long-term follow-up study from the Finnish Arthroplasty Register. Acta Orthop 2006; 77 (1): 57-70.
- Glyn-Jones S, Gill HS, McLardy-Smith P, Murray DW. Roentgen stereophotogrammetric analysis of the Birmingham hip resurfacing arthroplasty. A two-year study. J Bone Joint Surg (Br) 2004; 86 (2): 172-6.
- Grant P, Aamodt A, Falch JA, Nordsletten L. Differences in stability and bone remodeling between a customized uncemented hydroxyapatite coated and a standard cemented femoral stem A randomized study with use of radiostereometry and bone densitometry. J Orthop Res 2005; 23 (6): 1280-5.
- Gruen TA, McNeice GM, Amstutz HC. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop 1979; (141): 17-27.
- Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg (Am) 1969; 51 (4): 737-55.
- Hart AJ, Buddhdev P, Winship P, Faria N, Powell JJ, Skinner JA. Cup inclination angle of greater than 50 degrees increases whole blood concentrations of cobalt and chromium ions after metal-on-metal hip resurfacing. Hip Int 2008; 18 (3): 212-9.
- Hart AJ, Sabah S, Henckel J, Lewis A, Cobb J, Sampson B, Mitchell A, Skinner JA. The painful metal-on-metal hip resurfacing. J Bone Joint Surg (Br) 2009; 91 (6): 738-44.
- Itayem R, Arndt A, Nistor L, McMinn D, Lundberg A. Stability of the Birmingham hip resurfacing arthroplasty at two years. A radiostereophotogrammetric analysis study. J Bone Joint Surg (Br) 2005; 87 (2): 158-62.
- Itayem R, Arndt A, McMinn DJ, Daniel J, Lundberg A. A five-year radiostereometric follow-up of the Birmingham Hip Resurfacing arthroplasty. J Bone Joint Surg (Br) 2007; 89 (9): 1140-3.
- Kaptein BL, Valstar ER, Spoor CW, Stoel BC, Rozing PM. Model-based RSA of a femoral hip stem using surface and geometrical shape models. Clin Orthop 2006; (448): 92-7.
- Karrholm J, Borssen B, Lowenhielm G, Snorrason F. Does early micromotion of femoral stem prostheses matter? 4-7-year stereoradiographic follow-up of 84 cemented prostheses. J Bone Joint Surg (Br) 1994; 76 (6): 912-7.
- Krantz N, Miletic B, Migaud H, Girard J. Hip resurfacing in patients under thirty years old: an attractive option for young and active patients. Int Orthop 2012; 36 (9): 1789-94.
- Langton DJ, Jameson SS, Joyce TJ, Webb J, Nargol AV. The effect of component size and orientation on the concentrations of metal ions after resurfacing arthroplasty of the hip. J Bone Joint Surg (Br) 2008; 90 (9): 1143-51.
- Lazarinis S, Mattsson P, Milbrink J, Mallmin H, Hailer NP. A prospective cohort study on the short collum femoris-preserving (CFP) stem using RSA and DXA. Acta Orthop 2013; 84 (1): 32-9.
- Li MG, Rohrl SM, Wood DJ, Nivbrant B. Periprosthetic changes in bone mineral density in 5 stem designs 5 years after cemented total hip arthroplasty. No relation to stem migration. J Arthroplasty 2007; 22 (5): 689-91.
- Lohmann CH, Schwartz Z, Koster G, Jahn U, Buchhorn GH, MacDougall MJ, Casasola D, Liu Y, Sylvia VL, Dean DD, Boyan BD. Phagocytosis of wear debris by osteoblasts affects differentiation and local factor production in a manner dependent on particle composition. Biomaterials 2000; 21 (6): 551-61.
- Lorenzen ND, Stilling M, Jakobsen SS, Gustafson K, Soballe K, Baad-Hansen T. Marker-based or Model-based RSA for Evaluation of Hip Resurfacing Arthroplasty? A Clinical Validation and 5-year Follow-up. Arch Orthop Trauma Surg 2013; 133 (11): 1613-21.
- Lyback CC, Lyback CO, Kyro A, Kautiainen HJ, Belt EA. Survival of Bi-Metric femoral stems in 77 total hip arthroplasties for juvenile chronic arthritis. Int Orthop 2004; 28 (6): 357-61.
- Mabilleau G, Kwon YM, Pandit H, Murray DW, Sabokbar A. Metal-on-metal hip resurfacing arthroplasty: a review of periprosthetic biological reactions. Acta Orthop 2008; 79 (6): 734-47.
- MacDonald SJ, Brodner W, Jacobs JJ. A consensus paper on metal ions in metal-on-metal hip arthroplasties. J Arthroplasty (Suppl 3) 2004; 19 (8): 12-6.
- MHRA, Medicines and Healthcare products Regulatory Agency. Medical device alert: all metal-on-metal (MoM) hip replacements, 2010 (MDA/2010/03). http://www.mhra.gov.uk/home/groups/dts-bs/documents/medicaldevicealert/con079162.pdf
- Nieuwenhuijse MJ, Valstar ER, Kaptein BL, Nelissen RG. Good diagnostic performance of early migration as a predictor of late aseptic loosening of acetabular cups: results from ten years of follow-up with Roentgen stereophotogrammetric analysis (RSA). J Bone Joint Surg (Am) 2012; 94 (10): 874-80.
- Nixon M, Taylor G, Sheldon P, Iqbal SJ, Harper W. Does bone quality predict loosening of cemented total hip replacements? J Bone Joint Surg (Br) 2007; 89 (10): 1303-8.
- Papageorgiou I, Yin Z, Ladon D, Baird D, Lewis AC, Sood A, Newson R, Learmonth ID, Case CP. Genotoxic effects of particles of surgical cobalt chrome alloy on human cells of different age in vitro. Mutat Res 2007; 619 (1-2): 45-58.
- Penny JO, Overgaard S. Serum chromium levels sampled with steel needle versus plastic IV cannula. Does method matter? J Biomed Mater Res B Appl Biomater 2010; 92 (1): 1-4.
- Penny JO, Ding M, Varmarken JE, Ovesen O, Overgaard S. Early micromovement of the Articular Surface Replacement (ASR) femoral component: two-year radiostereometry results. J Bone Joint Surg (Br) 2012; 94 (10): 1344-50.
- Pijls BG, Nieuwenhuijse MJ, Fiocco M, Plevier JW, Middeldorp S, Nelissen RG, Valstar ER. Early proximal migration of cups is associated with late revision in THA: a systematic review and meta-analysis of 26 RSA studies and 49 survivalstudies. Acta Orthop 2012; 83 (6): 583-91.
- Sieber HP, Rieker CB, Kottig P. Analysis of 118 second-generation metal-on-metal retrieved hip implants. J Bone Joint Surg (Br) 1999; 81 (1): 46-50.
- Soballe K, Toksvig-Larsen S, Gelineck J, Fruensgaard S, Hansen ES, Ryd L, Lucht U, Bunger C. Migration of hydroxyapatite coated femoral prostheses. A Roentgen Stereophotogrammetric study. J Bone Joint Surg (Br) 1993; 75 (5): 681-7.
- Strom H, Nilsson O, Milbrink J, Mallmin H, Larsson S. Early migration pattern of the uncemented CLS stem in total hip arthroplasties. Clin Orthop 2007; (454): 127-32.
- Valstar ER, Gill R, Ryd L, Flivik G, Borlin N, Karrholm J. Guidelines for standardization of radiostereometry (RSA) of implants. Acta Orthop 2005; 76 (4): 563-72.
- Vendittoli PA, Mottard S, Roy AG, Dupont C, Lavigne M. Chromium and cobalt ion release following the Durom high carbon content, forged metal-on-metal surface replacement of the hip. J Bone Joint Surg (Br) 2007; 89 (4): 441-8.