Abbreviations
| CI | = | Confidence Interval |
| CT | = | Computer Tomography |
| MRI | = | Magnetic Resonance Imaging |
| RSA | = | Roentgen Sterephotogrammetric Analysis |
| VAS | = | Visual Analogue Scale |
| ODI | = | Oswestry Disablity Index |
| SF-36 | = | Short Form-36 |
| SIJ | = | Sacroiliac Joint |
| ME | = | Mean Error of Rigid Body Fitting |
| CN | = | Condition Number |
| MIS | = | Minimal Invasive Surgery |
| LBP | = | Low Back Pain |
| PGP | = | Pelvic Girdle Pain |
| BMS | = | Body Mass Index |
| A-P | = | Anterior - Posterior |
| ASLR | = | Active Straight Leg Raise |
| LOS | = | Limit of significansn |
Acknowledgements
This work was made possible thanks to: research grant from the Norwegian Foundation for Health and Rehabilitation (through Norges Handikapforbund) and Sophies Minde Ortopedi AS. This project was carried out at the Department of Orthopaedics, Oslo University Hospital, Norway. I am thankful for the excellent scientific environment at the Department of Orthopaedics at Oslo University Hospital, with Prof. Lars Nordsletten and Prof. Lars Engebretsen.
I will especially thank my main supervisor, Britt Stuge (PT, PhD) and my two other supervisors Prof. Olav Røise and Stephan Röhrl (MD, PhD) at the Department of Orthopaedics, Division of Surgery and Clinical Neuroscience, Oslo University Hospital, Oslo, Norway.
Thesis at a glance
Paper I
Background – Different techniques have been used to quantify the movement of SIJ’s. These include RSA, but the accuracy and precision of this method have not been properly evaluated and it is unclear how many markers are required and where they should be placed to achieve proper accuracy and precision. The purpose of this study was to test accuracy and precision of RSA, applied to the SIJ, in a phantom model and in patients.
Methods – We used a plastic phantom attached to a micrometer to obtain a true value of the movement of the SIJ and compared this value with the measured value obtained by RSA; the difference represented the accuracy. The precision of the system was measured by double examination in the phantom and in six patients, and was expressed by a limit of significance (LOS). We analyzed different marker distributions to find optimal marker placement and number of markers needed.
Results – The accuracy was high and we identified no systematic errors. The precision of the phantom was high with a LOS less than 0.25° and 0.16 mm for all directions, and in patients, the precision was less than 0.71° for rotations and 0.47 mm translations. No markers were needed in the pubic symphysis to obtain good precision.
Conclusions – The accuracy and precision are high when RSA is used to measure movement in the SI joint and support the use of RSA in research of SIJ motion.
Paper II
Background – Chamberlain’s projections (anterior-posteriorx-ray of the pubic symphysis) have been used to diagnose SIJ mobility during the single-leg stance test. This study examined the movement in the SIJ during the single-leg stance test with precise RSA.
Methods – Under general anesthesia, tantalum markers were inserted into the dorsal sacrum and the ilium of 11 patients with long-lasting and severe pelvic girdle pain. After two to three weeks, a RSA was conducted while the subjects performed a single-leg-stance.
Results – Small movements were detected in the SIJ during the single-leg stance. In both the standing- and hanging-leg sacroiliac join, a total of 0.5° rotation was observed; however, no translations were detected. There were no differences in total movement between the standing- and hangingleg SIJ.
Interpretation – The movement in the SIJ during the single-leg stance is small and almost undetectable by the precise RSA. A complex movement pattern was seen during the test, with a combination of movements in the two joints. The interpretation of the results of this study is that, the Chamberlain examination likely is inadequate in the examination of SIJ movement in patients with PGP.
Paper III
Background – The fusion of the pelvic joints in patients with severe PGP is a controversial and insufficiently studied subject. The aims of this study were to evaluate physical function and pain after SIJ fusion.
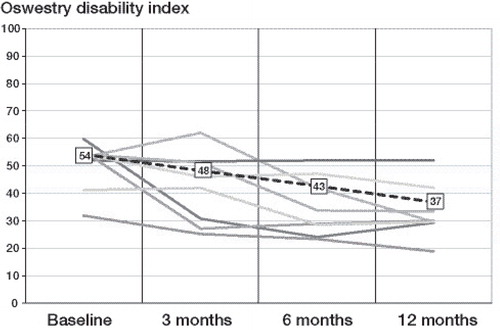
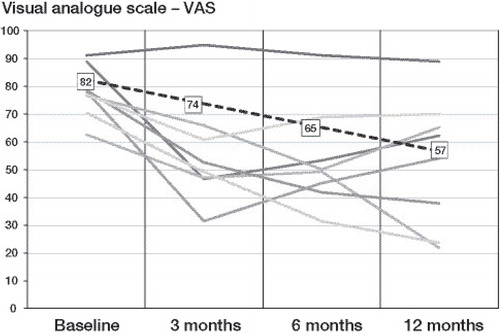
Methods – A single-subject research design study with repeated measurements was conducted; pre-operatively and 3, 6, and 12 months post-operatively. The outcome measures considered were the Oswestry disability index (ODI), visual analogue scale (VAS), and SF-36. Eight patients with severe PGP received open-accessed unilateral anterior SIJ fusion and concomitant fusion of the pubic symphysis.
Results – Seven patients reported positive results from the surgery. At 1 year post-operation, significant (p < 0.001) reductions in ODI (54 to 37) and VAS (82 to 57) were reported. The physical functioning, bodily pain, and social functioning scores in the SF-36 were also improved.
Conclusion – Positive and significant changes in disability and pain at 1 year after SIJ fusion were observed. Despite these positive results, open accessed anterior fusion of the SIJ was associated with adverse events and complications such as infection and nerve damages.
Paper IV
Purpose – Fusion of the SIJ has been a treatment option for patients with severe PGP. The primary aims were to evaluate the long-term outcomes in patients who underwent SIJ fusion and to compare 1-year outcomes with long-term outcomes. The secondary aim was to compare patients who underwent SIJ fusion with a comparable group who did not.
Methods – This study includes 50 patients that underwent SIJ fusion between 1977 and 1998. Function (ODI), pain intensity (VAS) and health-related quality of life (SF-36) were determined according to a patient-reported questionnaire. The questionnaire scores were compared with previously recorded 1-year outcomes and with questionnaire scores from a group of 28 patients who did not undergo SIJ fusion.
Results – The patients who underwent SIJ fusion reported a mean ODI of 33 (95% CI 24–42) and a mean VAS score of 54 (95% CI 46–63) 23 years (range 19–34) after surgery. Regarding quality of life, the patients reported reduced physical function, but mental health was not affected in the same manner. The patients with successful 1-year outcomes (48%) retained significantly improved function and reduced pain levels compared with the subgroup of patients with unsuccessful 1-year outcomes (28%). The patients who underwent surgery did not differ from the non-surgery group in any outcome at the long term follow-up.
Conclusions – Patients treated with SIJ fusion had moderate disability and pain 23 years after surgery, and the 1-year outcomes were sustained 23 years after surgery. Although many fused patients reported good outcome, this group did not differ from the comparable non-surgical group.
Introduction
Pelvic girdle pain
The sacroiliac joint (SIJ) can be a source of pain for 13-30% of patients with low back pain (LBP) (CitationVleeming et al. 2008) and for possibly an even greater proportion of patients suffering from “failed back surgery” (CitationDePalma et al. 2011, CitationKatz et al. 2003). This pain may be caused by a specific pathology of the joint (CitationBellamy et al. 1983), but the specific role of the SIJ in unspecific pelvic girdle pain (PGP) disorder remains unknown. PGP is a common complaint in pregnancy that can cause disability, and in some women, the complaint continues after delivery (CitationAlbert et al. 2002, CitationVleeming et al. 2008). The origin and diagnosis of PGP are also unclear because radiological findings are often absent, and the diagnostic criteria lack sufficient evidence. It has, however, become increasingly clear that the clinical presentation and disability level in patients with PGP differ from those in patients suffering from LBP (CitationO’Sullivan and Beales 2007, CitationRobinson et al. 2010).
Terminology
Many different terms have been used to describe pelvic pain (CitationWu et al. 2004), and some of these terms describe possible etiologies, such as “relaxation”, “instability” and “arthropathy”. Because the origin of pain in PGP is uncertain, these terms might be incorrect or misleading. To obtain a single term, the authors of the European guidelines for the diagnosis and treatment of pelvic girdle pain proposed the term PGP, together with the following definition (CitationVleeming et al. 2008).
“Pelvic girdle pain generally arises in relation to pregnancy, trauma, arthritis and osteoarthritis. Pain is experienced between the posterior iliac crest and the gluteal fold, particularly in the vicinity of the SIJ. The pain may radiate in the posterior thigh and can also occur in conjunction with/or separately in the symphysis. The endurance capacity for standing, walking, and sitting is diminished. The diagnosis of PGP can be reached after exclusion of lumbar causes. The pain or functional disturbances in relation to PGP must be reproducible by specific clinical tests.”
This definition has been proposed for pelvic musculoskeletal pain to exclude gynecological and/or urological disorders and to promote consistent use of terminology.
Epidemiology
PGP is most commonly reported in pregnancy, but some patients also develop PGP after minor trauma or without any specific reason. The prevalence of PGP during pregnancy has been estimated to be approximately 20% (CitationVleeming et al. 2008), and approximately 50% of patients report LBP during pregnancy (CitationBerg et al. 1988, CitationWu et al. 2004, CitationRobinson et al. 2006, CitationOstgaard et al. 1991). Most women recover, but approximately 10-25% of women continue to have complaints after delivery (CitationAlbert et al. 2001, CitationWu et al. 2004, CitationLarsen et al. 1999, CitationVleeming et al. 2008, CitationBjelland et al. 2013b), and approximately 5% suffer from pain that is sufficiently severe to require medical assistance (CitationWu et al. 2004). Furthermore, it seems that patients with symptoms in all three pelvic joints during pregnancy have an increased risk of suffering from disabling PGP 2 years after delivery compared to patients with pain in one or two joints (CitationAlbert et al. 2001). PGP occurs frequently during pregnancy and has a good prognosis of rapid regression of symptoms, but in some cases, the pain becomes long-lasting and debilitating.
The SIJ has also been suggested to be a possible source of pain in non-pregnant patients, such as patients with non-specific LBP. The prevalence reported has varied greatly and has been estimated to be somewhere between 10% and 62% (CitationSimopoulos et al. 2012). Without a gold standard to diagnose the SIJ pain, the prevalence has been difficult to establish. Intra-articular SIJ injections have been used as a gold standard to estimate the prevalence of SIJ pain in patients with LBP. The effects of these injections have been reported to be positive or negative, however, with different cut-off values defining a positive test result. Some investigators used a single injection as the cut-off, whereas others did not define the test as positive if the test was not replicated with a control block (CitationSimopoulos et al. 2012). The selection of patients is another factor that has had a large influence on prevalence. The lowest prevalence has been observed in unselected groups of patients with unspecific LBP, and in studies including patients with a probability of SIJ pain, the prevalence has increased. Although the prevalence varies, it is highly possible that the SIJ is a source of pain in patients with non-specific LBP, but without a gold standard, these numbers are uncertain.
Etiology
The etiology of PGP is poorly understood, but there is agreement that the cause is multi-factorial, and it must be viewed in a bio-psycho-social framework (CitationO’Sullivan and Beales 2007). Many attempts have been undertaken to understand the origin of PGP, and the factors that are believed to be of importance include hormonal, genetic, psychological, neurophysiological, biomechanical, pathoanatomical and social factors (CitationO’Sullivan and Beales 2007, CitationKanakaris et al. 2011).
All of these different factors can contribute to PGP, but the extent to which each factor contributes is likely different in each patient. The hormonal influence of relaxin and progesterone on the ligaments, with smoothening and relaxing effects, has been well established (CitationAlbert et al. 1997), but the association between hormone levels and PGP has been debated (CitationAlbert et al. 1997, CitationVollestad et al. 2012, CitationBjelland et al. 2013a). The sacropelvic ligaments have been of interest because many patients with PGP report tenderness in these ligaments (CitationTorstensson et al. 2009, CitationPalsson and Graven-Nielsen 2012). The relaxing effects of hormones on the ligaments during pregnancy have contributed to the biomechanical understanding or misunderstanding of pelvic relaxation and instability. Separation of the pubic symphysis has been used as an objective measurement of pelvic joint movement, and pubic movement has been reported to be greater in patients with PGP than in controls (CitationMens et al. 2009). However, the variations in the movements and the overlap in range between patients with and without PGP are too large to use these measurements as diagnostic tools. Although increased movement can be observed during and shortly after pregnancy, there has been no documentation of a correlation between sacroiliac mobility and symptoms in patients with long-term PGP (CitationSturesson et al. 1989, CitationVleeming et al. 2012). However, a correlation has been found between asymmetrical laxity of the SIJ and the intensity of symptoms (CitationDamen et al. 2001). Because pelvic relaxation during pregnancy is a normal physiological response, and the majority of pregnant women do not experience pain, the importance of this minimal increase in pelvic joint movement is uncertain. Although many factors have been proposed to be important when PGP develops and persists, it has been suggested that pain caused by dysfunction in the SIJ is a plausible explanation (CitationOstgaard et al. 1991).
Altered muscle activation has been observed in patients with PGP (CitationMens et al. 2009, CitationO’Sullivan and Beales 2007, CitationWu et al. 2008, CitationBeales et al. 2009, CitationStuge et al. 2012, CitationStuge et al. 2013). Optimal muscular control is important for stabilizing the SIJ as well as the entire pelvic girdle (CitationSnijders et al. 1993), and a treatment program, including training in motor control, has been shown to reduce PGP (CitationStuge et al 2004a,. CitationO’Sullivan and Beales 2007, CitationStuge et al. 2004b).
When researching PGP, the bio-psycho-social model should be applied because psychological and social factors also seem to contribute when a patient develops chronic pain syndrome. Psychological factors, such as emotional distress and catastrophizing during pregnancy, have been shown to increase the risk of PGP (Beales et al. 2009, CitationBjelland et al. 2013b, CitationOlsson et al. 2012), and social factors, such as physically demanding work and inconvenient work hours, have also been found to increase the risk of PGP (CitationJuhl et al. 2005). These findings are in contrast to the strict reductionist biological model of medicine, in which the disease can be explained by an underlying pathological process or a developmental abnormality.
Diagnostics
Medical history
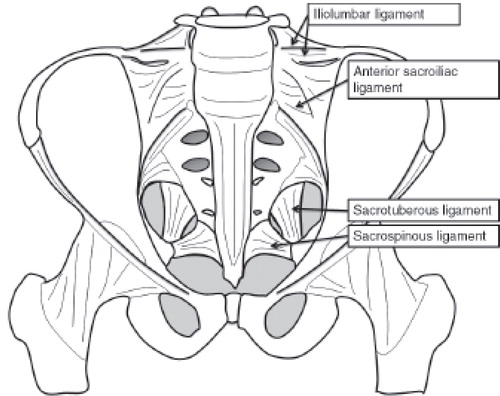
The clinical presentation of patients with PGP varies, but there are certain common characteristics. Often, the pain is located over the SIJ region and extends below the posterior spine, along the long dorsal ligament (), deep into the gluteal region and into the pubic symphysis. The pain worsens with standing, sitting and walking (CitationVleeming et al. 2008, CitationWu et al. 2004), and many patients report “catching” of the leg (CitationSturesson et al. 1997). Although many patients have reported these clinical symptoms, the medical history alone has been reported to have limited value compared to an SIJ injection as the gold standard (CitationDreyfuss et al. 1996).
Clinical tests
There have been many reports with very different results regarding the reliability and validity of clinical tests in the diagnosis of PGP. The main reason for this variation has been the lack of a gold standard with which to compare the tests (CitationVleeming et al. 2008). Dreyfuss et al. (1996) did not find any reasonable value of medical history or clinical testing compared to diagnostic SIJ block, but other researchers have found adequate sensitivity and specificity with clinical testing, particularly if multiple tests were used (CitationLaslett et al. 2005a). In two systematic reviews (Citationvan der Wurff et al. 2000b, Citationvan der Wurff et al. 2000a), the authors reported both the reliability and validity of clinical tests to be poor; however, later studies of higher quality reported more promising results (CitationLaslett et al. 2006). These tests can be divided into provocation tests and functional tests (CitationVleeming et al. 2008).
Provocation tests aim to stress the SIJ and the surrounding ligaments and to trigger actual pain. Laslett (2005) emphasized that the test should be regarded as positive if it reproduces familiar pain. The use of multiple tests strengthens the probability of the diagnosis (CitationLaslett et al. 2003, CitationLaslett et al. 2005b, CitationSlipman et al. 1998, CitationStanford and Burnham 2010, Citationvan der Wurff 2006, Citationvan der Wurff et al. 2006, CitationVleeming et al. 2008). The above-mentioned studies used 3 of 5-6 positive provocation tests as a cut-off and SIJ injection as the gold standard. The studies reported sensitivity of 82-94% and specificity ranging from 57% to 78%. As shown in , if only 1 positive test was chosen, the sensitivity was high because a patient with PGP most likely tested positive on one test. Because these tests loaded the SIJ in different ways, the patients most likely did not respond to all tests; consequently, the sensitivity decreased, together with an increased cut-off for positive clinical tests (). The specificity was low if only 1 test of 5 was positive, but if 5 of 5 tests were positive, the specificity was 88–100%.
Table 1. Sensitivity and specificity of combinations of tests
To provoke the pubic symphysis pain, two tests have been used: the modified Trendelenburg test and palpation of the pubic symphysis (CitationAlbert et al. 2000, CitationVleeming et al. 2008). The modified Trendelenburg test is considered positive if the patient experiences pain in the symphysis when standing on one leg with the other hip in 90° of flexion (CitationAlbert et al. 2000). The sensitivity has been reported to be 40–62% and the specificity to be 99% (CitationVleeming et al. 2008). Gentle palpation of the symphysis, with pain 5 seconds after removal of the hand, has been shown to have sensitivity of 60–81% and specificity of 85–99% and to have good inter-examiner agreement (kappa = 0.89) (CitationAlbert et al. 2000, CitationKristiansson and Svardsudd 1996).
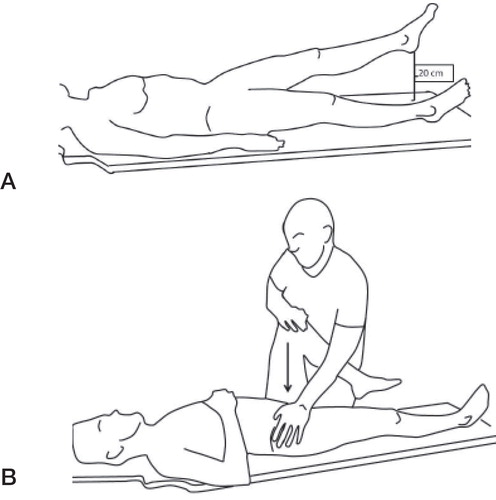
The most widely used functional test is the active straight leg raise (ASLR) () (CitationMens et al. 1999). When Mens et al. (1999) applied this test in 200 patients with suspected PGP and compared these patients to 50 healthy controls, they found, when a cut-off score between 0 and 1 was chosen, sensitivity of 0.87 and specificity of 0.94. The same test proved to be well-correlated with the severity of symptoms (CitationMens et al. 2002).
Figure 1. A. Active straight leg raise (ASLR). The patient lifts the leg 20 cm from the bench and grades the difficulty of performing this action between 0 (no problem) and 5 (impossible). B. Posterior pelvic pain provocation test (P4). A gentle press is made on the flexed leg, and the test is positive if a familiar pain is reproduced in the posterior gluteal region.
Radiological examinations
Computer tomography is the best examination for visualizing the bony anatomy of the SIJ, but one challenge is that radiological findings of degeneration can be observed in normal subjects as well as in patients with SIJ pain. In a study of 45 asymptomatic subjects, Vogler et al. (1984) reported symmetrical and normal CT scans in subjects younger than 30 years old, but with increasing age, the radiological findings changed. The joint space became less uniform, and subchondral sclerosis was observed. In the oldest participants (older than 59 years old), the investigators discovered high percentages of osteophytes, cysts, erosions and ankylosis. These findings were verified by Shibata et al. (2002), who reported joint space narrowing (87%), sclerosis (52%) and osteophytes (68%) in 190 patients who were asymptomatic for SIJ, with a higher prevalence with increasing age. Subsequently, Elgafy et al. (2001) compared degenerative CT findings with SIJ injections to examine the relationship between radiological findings and symptoms. Of 62 patients with positive SIJ injections, 42.5% had normal CT findings, and when these cases were compared to a control group of asymptomatic patients, the authors found sensitivity of 58% and specificity of 69% for CT. In summary, these CT findings could be found in patients with PGP and suspected SIJ pain, as well as in asymptomatic subjects, which limited the diagnostic value of CT scans for the diagnosis of PGP (CitationVogler, III et al. 1984, CitationElgafy et al. 2001, CitationShibata et al. 2002).
Magnetic resonance imaging has been reported to play an important role in diagnosing inflammatory SIJ pathology and particularly in diagnosing early changes in SIJ spondyloarthropathies (CitationPuhakka et al. 2004a, CitationPuhakka et al. 2004b, CitationVleeming et al. 2008). The use of MRI can be used to identify these changes, but it has primarily been used to exclude serious pathology.
Radionuclide bone scanning has also been used to diagnose SIJ pathology, but when scintigraphy is compared to SIJ injections, the sensitivity of the former has proven to be low. When scans were considered either positive or negative, Slipman et al. (1996) reported sensitivity of 13%, indicating that 87% of the patients with positive SIJ injections had negative bone scans. Subsequently, CitationMaigne et al. (1998) used quantitative radionuclide bone scans and found higher uptake in joints with positive SIJ injections, and they reported sensitivity of 46% and specificity of 89%. The radionuclide bone scan is therefore an inadequate tool for screening the SIJ as the origin of pain (CitationSlipman et al. 1996, CitationMaigne et al. 1998).
The sacroiliac joint
The SIJ has been considered one of many etiologies of PGP and LBP. Before herniated discs were discovered to be a cause of LBP, the SIJ was believed to play a central role as a pain generator. Subsequently, however, focus moved away from the SIJ toward the herniated disc. More recent injection studies have discovered that a significant proportion of LBP patients have SIJ pain (CitationSchwarzer et al. 1995, CitationSimopoulos et al. 2012), and the SIJ has also been suggested to be a significant contributor to failed back surgery (CitationKatz et al. 2003, CitationMaigne and Planchon 2005). Hence, the SIJ might play a role in the development of PGP, as well as having a potentially important role in patients with LBP.
The sacroiliac joint in historical perspective
There has been great interest in the SIJ in the medical literature, and according to several authors (CitationBuchowski et al. 2005, CitationWeisl 1955, CitationLynch 1920, CitationVleeming et al. 2012), the SIJ was first described by Hippocrates as a source of pain. Hippocrates () described the “disjunctio pelvica” as a reason for pain during pregnancy, but it was originally believed that the SIJ only became mobile during pregnancy. Since the time of Hippocrates, debate has persisted regarding the degree of mobility of the SIJ. According to Weisl (1955), Dimerbroeck stated in 1689 that the SIJ was likely also mobile also in men and in women apart from pregnancy, and this fact was later confirmed by multiple cadaver studies (CitationWeisl 1955). From these cadaver studies, evidence emerged that the SIJ is a synovial joint and therefore must move. Subsequent measurements of the true conjugate distance showed differences between different postures, indicating movement of the sacrum relative to the innominate bone (CitationVon Schubert 1929, CitationWeisl 1955). Later authors concluded that the movement of the SIJ was mostly rotational around an axis perpendicular to the joint surface.
In 1930, Chamberlain described an radiographic method for indirectly measuring SIJ movement. Because SIJ movements were assumed to be mostly rotational, the movement measured in the pubic symphysis was interpreted as an indirect measurement of SIJ movement (CitationChamberlain 1930). Chamberlain also found that the movement observed in the pubic symphysis, and indirectly in the SIJ, could be correlated with pain. This relationship between Chamberlain’s radiographic studies and pain was also reported by other researchers, but the findings were not consistent (Anderson and Peterson 1944, CitationMens et al. 1999). During this time period, the SIJ was a well-established cause of ischialgia and LBP, but it lost attention when Mixter and Barr (CitationMixter and Barr 1934) first described a ruptured intervertebral disc as a source of ischialgia. Despite Anderson’s (1944) statement, “There seems to be no question at the present time that the SIJ is a movable joint,” and the convincing results of Weisl (1955) showing SIJ movement, interest in the SIJ declined. Subsequently, Solonen (1957) stated that because of the strong ligaments and irregular shape of the SIJ, the joint is immobile, and this observation was more or less considered to be true for a long period of time. In the 1980s, interest in the SIJ returned, and there were several studies during this period that attempted to establish and understand the biomechanical properties of the SIJ (CitationWeisl 1955, CitationSolonen 1957, CitationSmidt et al. 1995, CitationSmidt et al. 1997, CitationSturesson 1999, CitationSturesson et al. 1989, CitationSturesson et al. 1999, CitationSturesson et al. 2000a, CitationSturesson et al. 2000b).
Anatomy
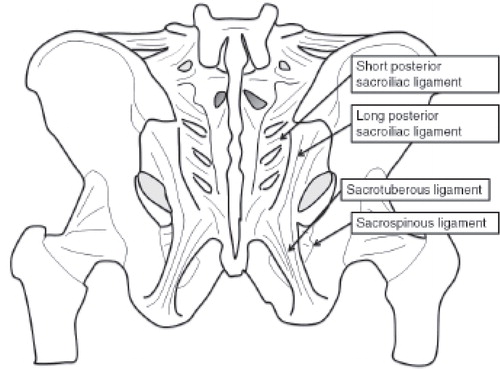
The SIJ is a diarthrodial joint, but it is unique because the sacral surface has hyaline cartilage, and the ilial surface has fibrocartilage (CitationFoley and Buschbacher 2006, CitationForst et al. 2006, Vleeming et al. 2012). The joint’s anatomy is variable between subjects with regard to its size and shape, and the joint changes over one’s lifetime (CitationVleeming et al. 1990, CitationVogler, III et al. 1984). The joint is L-shaped and is formed from the sacral bodies from S1 to S3. The joint line is smooth in childhood but becomes more irregular in adulthood, which minimizes movement (CitationVleeming et al. 2012). In addition to the irregular joint surface, primary stabilization of the joint is accomplished by different strong ligaments ( and ). The anterior ligament is more or less a thickening of the anterior capsule, and it is not as strong as the dorsal ligaments. The dorsal ligaments consist of different defined ligaments, of which the interosseous ligament is the strongest. This ligament is multidirectional and is an important stabilizer, allowing great forces to be transferred from the spine to the lower extremities. The other ligaments that stabilize this joint include the long and short dorsal sacroiliac ligament, the sacrotuberous ligament and the iliolumbar ligament ( and ). The bony anatomy and these ligaments ensure that the pelvic girdle is not a rigid ring but instead works as a suspension mechanism that allows forces to be transferred without causing a fracture to the pelvis (CitationVleeming et al. 2012).
No muscles directly cross the SIJ, but the interactions of adjacent muscles and fascial structures are dynamic stabilizers of the SIJ. The biceps femoris, the gluteus maximus and the piriformis are connected to the ligaments around the SIJ and contribute to the functional stability of the joint (CitationSnijders et al. 1993). Additionally, the pelvic floor muscles have been reported to add stiffness to the pelvic ring (Snijders et al. 1993, CitationPool-Goudzwaard et al. 2004). Furthermore, the deep abdominal muscles connecting to the thoracolumbar fascia are believed to contribute to the stability of the SIJ (CitationVleeming et al. 1995).
Stability of the SIJ
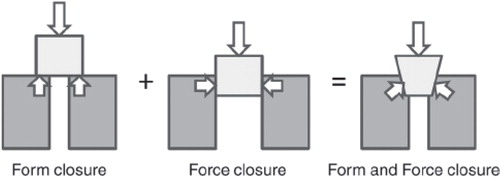
A biomechanical model has been created to describe the forces that contribute to the stability of the SIJ. Snijders et al. (1993) described a model based on the theory of form and force closure. Form closure refers to a situation in which the joint is stable, without any need for additional stabilizing forces, and form closure is a situation in which the joint is stabilized by friction and compression forces. The SIJ is believed to be stabilized by a combination of form closure (ridges and grooves in the SIJ) and force closure (ligaments and muscles) (CitationSnijders et al. 1993, CitationVleeming et al. 1990) ().
The range of motion in the SIJ is small, both in patients with PGP and in asymptomatic individuals (CitationGoode et al. 2008, CitationVleeming et al. 2008, CitationVleeming et al. 2012). Hence, the stability of the SIJ is more closely related to how a load can be smoothly and effortlessly transferred across the SIJ than it is related to the degree of mobility. Non-optimal joint stability is defined in the European guidelines (CitationVleeming et al. 2008) as an “altered laxity or stiffness leading to new joint positioning and/or exaggerated/reduced joint compression, with a disturbed performance/effort ratio.”
Figure 5. Form closure refers to a situation where the joint is stable without any need for extra stabilizing forces, and force closure refers to a situation where the joint is stabilized by friction and compression forces. The combination of form and force closure is known as a selflocking mechanism.
Innervation
The innervation of the SIJ has been reported in many studies, but there is no agreement regarding the exact innervation of the SIJ (CitationCohen 2005, CitationVleeming et al. 2013). In two systematic reviews (CitationCohen 2005, CitationVleeming et al. 2013), the innervation of the dorsal part of the joint was suggested to arise primarily from the lateral branches of L4–S3, although different authors have suggested that different levels are involved. The anterior part is assumed to be innervated by the ventral rami, varying from L2 to S4. Further immunohistochemical analyses have been performed on the ventral capsule, interosseous ligaments, cartilage and bone, and there has been evidence of sensory nerves in all of these structures (CitationSzadek et al. 2008, CitationSzadek et al. 2010). The presence of calcitonin gene-related peptide and substance P immunoreactive fibers has been believed to provide morphological and physiological bases for pain signals originating from these structures (Szadek et al. 2008, Szadek et al. 2010), which could be why SIJ injections have effects and might also be why fusion to the joint can be effective for alleviating PGP.
Referred pain
Referred pain has been reported to coexist with SIJ pain, and in a study of 25 patients with PGP, verified by positive SIJ injections, as many as 60% had either thigh or leg pain (CitationLaplante et al. 2012). In another study of 50 patients, the authors found buttock pain in 94% of the patients and referred pain to the leg in more than 50% of the cases but with 18 different pain distributions (CitationSlipman et al. 2000). Before the herniated disc was discovered, the SIJ was regarded as an important etiology of sciatica, and it has been questioned whether nerves can be affected by disturbances in the SIJ (CitationFortin et al. 1994). Using arthrography, extravasation of contrast agent has been observed in many subjects, and different pathways between the SIJ and neural structures have been identified. Fortin et al. (1994) reported 61% SIJ extravasation in 76 injections, and these cases followed 5 patterns; ventral (16%), dorsal to the first sacral foramen (8%), dorsal sub-ligamentous (24%), superior (3%) and inferior (12%) to the sacral ala. Ventral extravasation of inflammatory agent could theoretically affect the lumbosacral plexus and S1 foramen all the way up to the L5 foramen. The neurotransmitter substance P has been identified as a possible cause of “neurogenic inflammation”. The SIJ is innervated and can therefore be a pain generator. Different referred pain patterns have been observed and can be explained by individual variations in innervation, direct nerve involvement or different sclerotomes (Fortin et al. 1994, CitationSlipman et al. 2000).
Biomechanical considerations of SIJ movement
“Interestingly, studies that demonstrated the highest levels of quality and that offered the lowest levels of error in measurement also reported the lowest values [of movement] available at the SIJ.”
As mentioned in the historical overview, several attempts have been undertaken to establish movement in the SIJ, both in healthy subjects and in patients with PGP. Many different techniques have been used, such as cadaver studies, studies using different markers (skin markers, palpation of the bony landmarks and k-wires) and radiological studies (radiography, CT, RSA) (CitationLavignolle et al. 1983, Sturesson et al. 1989, CitationBrunner et al. 1991, CitationVleeming et al. 1992a, CitationJacob and Kissling 1995, CitationSmidt et al. 1995, CitationSmidt et al. 1997, Sturesson 1999, Sturesson et al. 1999, Sturesson et al. 2000a, Sturesson et al. 2000b, CitationHungerford et al. 2004, CitationHungerford et al. 2007). All of these techniques have obvious advantages and disadvantages. The cadaver studies lacked muscular influence on stabilization, and the sample tended to come from an older population. The different experimental settings have different levels of precision and accuracy, and it seems that the methods with the best precision have the lowest measured SIJ motion (CitationGoode et al. 2008). Although the literature regarding analysis of movement has reported various results, there are some points on which these reports have generally agreed.
Most of the movement in the SIJ is rotational, occurring around all 3 axes but predominantly in the sagittal plane (Sturesson et al. 1989, CitationBrunner et al. 1991, CitationWalker 1992, CitationMens et al. 1999, Goode et al. 2008).
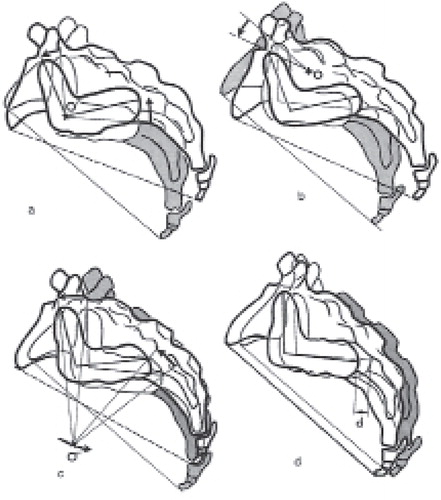
There are different theories regarding the motion of the sacrum relative to the innominate bone and the center of rotation. Because the sacrum is L-shaped and has an irregular surface, and because there is a large variation among subjects, a fixed center of rotation has been difficult to find (CitationWalker 1992). In , different theories that have been proposed are presented: (a) sacral tilt with the center of rotation inside the SIJ; (b) sacral rotation with the center of rotation located immediately dorsal to the SIJ; (c) rotation with the center of rotation in front of the SIJ; and finally, (d) translation with no rotation (CitationAlderink 1990). The evidence is not in agreement regarding this subject, but the strongest evidence has supported that the center of rotation is most likely located dorsal to the SIJ as a transverse axis and in close proximity to the iliac tuberosity (Figure 6b) (CitationEgund et al. 1978, CitationBrunner et al. 1991, CitationVleeming et al. 1992b, CitationJacob and Kissling 1995), although there are likely large individual differences.
The movements in the SIJ are small, and the total rotation has varied in different studies but has seldom exceeded a mean value of 2° (CitationJacob and Kissling 1995, CitationEgund et al. 1978, CitationVleeming et al. 1992a, CitationGoode et al. 2008, CitationVleeming et al. 2012). This movement has seemed to be greater in an unloaded pelvis than in a loaded pelvis (Sturesson et al. 1989, Sturesson et al. 2000a, Sturesson et al. 2000b, CitationGoode et al. 2008).
There do not seem to be differences in movement between symptomatic and asymptomatic SIJs (Sturesson et al. 1989).
There is evidence that women tend to have greater mobility than men. In healthy volunteers, Jacobs (1990) did not find any differences in SIJ movement with regard to age, sex or parturition. Other studies have reported less movement in men than in women (CitationBrunner et al. 1991, CitationBussey et al. 2009, Sturesson et al. 1989). It also seems that multiparous women have greater movement of the pelvic joints than nulliparous and men (CitationGarras et al. 2008, CitationMens et al. 2009).
Figure 6. Different theories of the location of the axis of rotation. Alderink 1991. Reproduced with permission from CitationAlderink G J. The sacroiliac joint: review of anatomy, mechanics, and function. J Orthop Sports Phys Ther 1990; 13(2): 71-84. doi:10.2519/jospt.1991.13.2.71 Copyright © Journal of Orthopaedic & Sports Physical Therapy®.
To measure SIJ movement accurately, the RSA technique has been applied to the SIJ. One-millimeter markers were implanted in patients, and with a specialized x-ray set-up and a computer program, the in vivo movement could be measured with high precision (Sturesson et al. 1989). These markers were attached to a segment in each ilium and to one in the sacrum, and the movement between these segments was then measured (for a more detailed description, see section 4.5). The RSA studies have, in general, reported less movement than other studies using methods with questionable precision (CitationGoode et al. 2008), and because the RSA showed less motion than other methods, the RSA method has been questioned. The RSA studies have measured movement between the sacrum and the ilium with dorsally placed RSA markers, and the markers were placed near the joint line. Because of the flat anatomy of the bones, the markers became collinear (in the same plane, which is not necessarily the optimal 3D distribution of the markers (CitationCibulka 2001).
Guidelines for the standardization of RSA of implants have recommended at least three non-collinear RSA markers in each segment (rigid body), which should be compared to one another (CitationValstar et al. 2005). A good 3D configuration of the segments relies on the distance between the markers and the distribution of the markers on all three axes; a condition number (CN) expresses the quality of a marker segment (CitationMakinen et al. 2004). The CN is a mathematical expression of how the markers relate to a straight line that passes through the segment (Ryd et al. 2000). A low CN represents a good scatter of markers in the segment. A CN below 110 is considered a reliable distribution (Valstar et al. 2005), and an upper limit of 150 is suggested. This CN will consequently influence the precision and accuracy. Additionally, another factor of importance is how well the RSA computer identifies and calculates the placement of each individual marker. The precision of each marker can be influenced by soft tissue disturbances and by the stability of the markers. If the markers are not thoroughly inserted into the bone and end up in the soft tissue, the markers can become unstable. This instability can occur in the sacrum because of the thick and strong dorsal ligaments covering the bone, particularly in the cranial portion. To ensure including only stable markers in the analysis, unstable markers should be excluded if they move more than 0.35 mm between two examinations (ME; mean error of rigid body fitting) (Valstar et al. 2005). Uncertainties with the RSA method, when applied to the pelvic joints, were addressed in a letter to the editor by CitationCibulka (2001), in which he asked:
“I question whether using this sort of marker arrangement can accurately define the fixed segments (especially the innominate bones) and therefore truly describe sacroiliac joint motion.”
“Would a different configuration (e.g., wider distribution) of pelvic markers show different results?”
These questions formed the basis for our first research question: What are the accuracy and precision of RSA when applied to the SIJ, and was the marker distribution used in the available RSA studies useful?
The Chamberlain technique
“The place to look for evidence of sacroiliac joint motion is at the symphysis pubis, where it is magnified and measurable.”
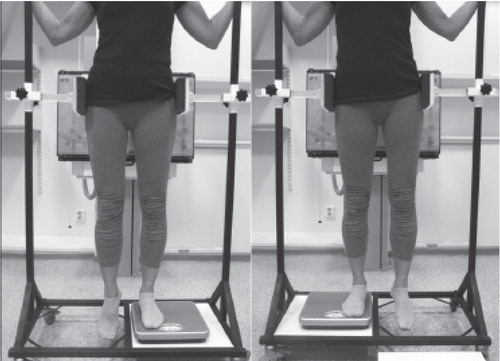
All of the experimental techniques used to quantify SIJ movement have been impractical in clinical practice. In 1930, Chamberlain described an easy and practical method for measuring pubic movement on anterior-posterior (AP) pelvic radiographs while the patient stood on one leg with the other leg hanging down (single-leg stance) (Chamberlain 1930) (). In patients with SIJ pain, Chamberlain found that weight bearing caused cranial displacement of the pubic bone to the side of the painful joint. This displacement was explained by rotation around the axis that was perpendicular to the SIJ surface. The Chamberlain technique has since been used to examine pubic bone movement and, indirectly, SIJ hyper-mobility (CitationMens et al. 1999).
Since the Chamberlain technique was first described, researchers have attempted to correlate pubic movement with SIJ pain (CitationAnderson and Peterson 1944, CitationMens et al. 1999, CitationSiegel et al. 2008). Chamberlain found a clear pattern in his patients, but Mens et al. (2009) subsequently found the exact opposite pattern, in which the hanging leg caused downward displacement of the pubic bone on the side of the painful joint. These differences have made it difficult for clinicians to use the results of this test in the diagnosis of PGP, particularly when normal variations in the movement of the pubic symphysis have proved to be large (CitationGarras et al. 2008). Measurements of the movement of the SIJ with the subject in the single-leg stance have been obtained using k-wires; however, those authors only measured healthy subjects without SIJ pain (CitationJacob and Kissling 1995). Because the Chamberlain technique is an indirect measurement of SIJ movement, what really occurs in the SIJ during the single-leg stance test in patients with PGP remains unknown.
Figure 7. The Chamberlain technique. Radiographs are obtained with the patient standing on one leg with the other leg hanging down.
This uncertainty formed the basis for our second research question: What is the movement in the SIJ during the single-leg stance in patients with severe PGP?
SIJ fusion as a treatment for SIJ pain
“Cases of relaxation of the sacroiliac joint which have had the above type of arthrodesis performed have been uniformly successful.”
The role of the SIJ as a pain generator has interested orthopedic surgeons for almost a century. Smith-Petersen described a method for SIJ fusion in 1921 (CitationSmith-Peterson MN 1921), and since then, several different attempts have been made to select and operate on patients with suspected SIJ pain. In the beginning, a large proportion of the patients had joint infections (especially tuberculosis), and many of the first surgical techniques were developed to treat these infections, but patients with “pelvic relaxation” during pregnancy have also comprised a large proportion of the patients receiving SIJ fusion (CitationSmith-Peterson 1921, CitationSmith-Petersen and Rogers 1926, CitationHagen 1974) (). SIJ fusion followed the same popularity curve as the knowledge of SIJ movement, most likely because movement, pain and fusion are closely related in an orthopedic surgeon’s mind. If there is mobility that causes pain, fusion can cure the pain. Before the herniated disc was discovered, SIJ fusion was a novel treatment for low back pain and disruption after pregnancy, and the treatment was described in several case series in the period from 1921 to the 1940s (). After the 1940s, there were no papers in the literature until the 1970s, when new reports of SIJ fusion started to appear. In the last few years, the role of the SIJ in orthopedic surgery has again been gaining popularity.
Table. Former studies reporting surgical outcomes after sacroiliac joint fusion.
Almost a century has passed since Smith-Petersen published his experiences with SIJ fusion in 1921. Despite this long history, only a few papers can be found in the literature, and to locate these papers, searches were conducted in Medline/Ovid, Embase and Google Scholar, combining the terms “sacroiliac joint”, “arthrodesis” and “fusion”. From the articles retrieved from this search, all of the articles and references were cross-checked to find further possible evidence. The results included only 30 papers and book chapters ().
When planning the study in 2005–2006, only 18 papers were available, describing 277 patients and 13 different surgical techniques. Although many different techniques were used, they all involved either open anterior or open dorsal fusion. In the beginning (1921–1940), there were mostly descriptions of these new surgical techniques and short descriptions of the results obtained for the first patients. In these materials, a large proportion of the patients were surgically treated for infections or for SIJ arthritis. The authors reported, in general, excellent to good outcomes in 50–60% of the patients, fair results in 20% and poor results in 20%. No further documentation was found from between 1941 and 1974, likely because the SIJ lost attention to the herniated disc. Until 2006, there were only case series, and only 4 of these 18 series were prospective registrations of outcomes. Only one larger study was available when we started our investigation, and this large study did not actually evaluate SIJ fusion but instead fixation with SIJ screws and without fusion (Citationvan Zwienen et al. 2004). All of these studies had short follow-up periods, except for one that had 5.8 years of follow-up (CitationBuchowski et al. 2005). Since 2006, 12 more case series have been published, all of which were designed as retrospective reviews of prospective registered outcome measurements, and these studies are referred to as prospective in the appendix because the outcome measures were collected pre- and post-operatively. These studies reported the surgical outcomes of 354 patients, and all of these reports were the results of minimally invasive surgery (MIS).
The diagnostic criteria and the criteria for surgery are not standardized, and surgery for PGP is controversial. There have been few studies and only limited knowledge about this treatment option (). Hence, it is difficult for healthcare providers to give proper advice to patients with PGP regarding surgery.
History of pelvic joint fusions in Norway
In 1974 orthopaedic surgeon Rolf Hagen, Martina Hansens Hospital, published his experience with conservative and surgical treatment of 23 patients with SIJ pain. Over a 20 year period from 1951–1971, eight patients were operated on with the surgical technique described by Smith-Peterson (CitationHagen 1974). Six out of these 8 had a good result, 1 had a fair result and 1 did not have any effect at all. From the middle of 1970’s to late 1990’s a few orthopedic surgeons in Norway performed SIJ fusions and some also did fusion to the pubic symphysis. Especially, orthopaedic surgeon Einar Sudmann at Hagavik Hospital, developed a systematic approach to the SIJ problem, as he registered the surgical outcome of 81 patients together with complications in a database. Einar Sudmann and the rest of the orthopaedic surgeons performing SIJ fusions did however not achieve the results they wanted. Because the outcomes were unpredictable, the complication rate appeared unacceptably high and the need for additional spinal surgery, the enthusiasm diminished. During the 1990’s most orthopedic surgeons had stopped performing SIJ fusions except professor Olav Røise, orthopedic pelvic trauma surgeon at Oslo University hospital. In the early 2000s the medical literature on surgical treatment of PGP was sparse and without high quality studies, and because of this professor Røise decided to stop doing the surgery until a study protocol was established. In 2004 a pilot study with 4 patients was conducted and in 2005 Olav Røise together with Britt Stuge, PT, PhD, Finnur Snorrason, MD, PhD and May Arna Risberg, PT, professor at OUS, started to plan this project.
The lack of documentation regarding the results after SIJ fusion and the fact that Sudmann performed SIJ fusion on more than 80 patients between 1977 and 1998 led us to the last two research questions: What are the outcomes of SIJ fusion, and what are the long-term results after SIJ fusion?
Aims of the thesis
The main questions and aims of the thesis are:
Paper I
Is the RSA method valid to measure pelvic movement?
The aims were to (1) measure the accuracy, precision, and condition numbers of pelvic RSA with different marker distributions in a phantom model, (2) explore whether frontal markers around the symphysis improve the condition number and precision and whether it is possible to avoid markers in the cranial part of the sacrum, and (3) to compare the precision obtained by a phantom with the precision in patients.
Paper II
What is the movement in the SIJ during the single-leg-stance test?
The aims were to (1) measure movement in the SIJs during the single-leg stance test by using RSA, in patients with severe PGP and to (2) identify whether there were any differences between movements in the SIJs of the standing leg and the hanging leg.
Paper III
What is the outcome of unilateral anterior SIJ fusion combined with fusion of the pubic symphysis?
The primary aim of this prospective study was to examine changes in pain and physical function at 3, 6, and 12 months after SIJ fusion. The secondary aims were to evaluate post-operative health-related quality of life and patient satisfaction with treatment.
Paper IV
What are the long-term results of SIJ fusion?
The main purpose was to evaluate long-term functioning, pain and health-related quality of life (HRQoL) in patients who had previously undergone pelvic joint fusion surgery. Further aims were to compare the 1-year outcomes with the long-term results and to compare patients who underwent surgery with PGP patients who did not undergo surgery.
Patients
Papers I, II and III
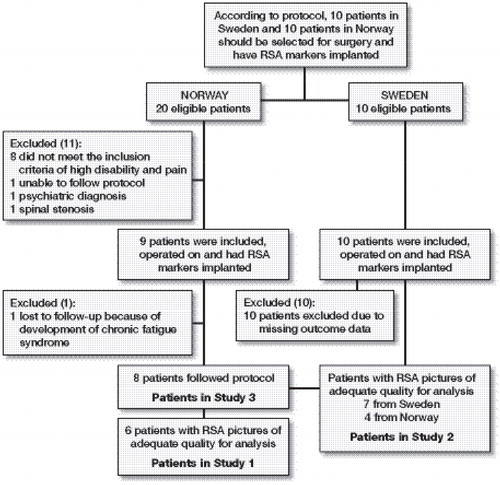
The patients in papers I, II and III consisted of patients from the same cohort. Originally, we planned to include and operate on 10 patients at Oslo University Hospital, Norway, and 10 patients at Ängelholm Hospital, Sweden, during the inclusion period from 2007 to 2010. In Norway, 20 patients were examined, but only 9 met the criteria for participation (). The patients were included according to the criteria provided in .
Table 2. Inclusion and exclusion criteria
In Sweden, 10 patients were also selected for surgery, but unfortunately, there were problems with the collection of questionnaires, primarily due to large administrative changes and the loss of key personnel in the Orthopedic Department at Ängelholm Hospital. Some preoperative and 1-year data were available, but the collection of questionnaires was incomplete. Hence, these patients were excluded from paper III.
All of the Swedish patients, however, had RSA markers implanted and were thus available for the RSA study (paper II). After evaluating the RSA data from all of the patients, six patients were excluded because of poor x-ray quality, so 11 patients were eligible for inclusion in paper II (). The patients were excluded because of misplaced markers in the soft tissue or insufficient visualization of the markers on radiographs during the software analysis. In paper I, we were able to use RSA pictures from 6 of the 9 Norwegian patients (). The Swedish patients did not undergo double examinations; therefore, they were not included in paper I.
Paper IV
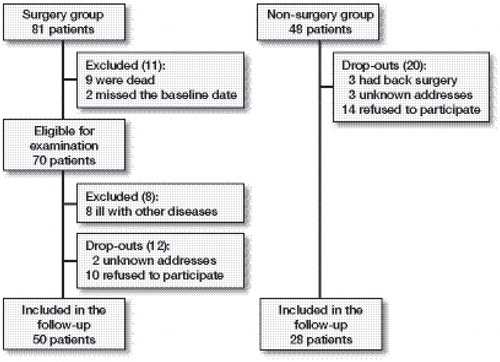
The patients in paper IV were operated on at Hagavik Orthopaedic Hospital between 1977 and 1998 by Sudmann and co-workers. The data came from 50 subjects at 1 year after SIJ fusion and from long-term follow-ups. Eighty-one patients underwent SIJ fusion during this period. These patients were registered in a database and were asked in 2009 to participate in long-term follow-up. The study population is described in . During the 1990s, the surgeons became increasingly reluctant to perform SIJ fusion, and a number of patients were refused surgery. Twenty-eight of these patients constituted the non-surgery group.
The patients were selected and operated on primarily by one of the authors (E.S.). The criteria for surgery were based on the patient history and on radiological and clinical examinations. The inclusion criteria were pain in the SIJ >1 year after pregnancy or trauma, pain with an idiopathic origin, severe disability and resistance to conservative treatment. The clinical tests performed included tenderness at the superior and inferior posterior iliac spines, active and passive straight leg raise tests, Patrick Faber’s test, passive hip rotation, forcible inward rotation and extension of the hip joint. Further tests included normal neurological and gynecological exams, normal spinal x-rays, symphysis movement of less than 3 mm on plain radiographs during a one-leg stance, normal radiculography, negative rheumatology tests and negative blood tests.
Methods
Design
Paper I
In paper I, the accuracy and precision of pelvic RSA were evaluated in an experimental setting using a phantom model, and the precision was also measured in vivo by double examinations. We used a plastic pelvic phantom (Sawbones® 1301; Pacific Research Laboratories, Inc., Vashon, WA, USA) attached to a micrometer to measure the true value of movement, and these values were compared to the values obtained from the RSA measurements. Because the number of markers needed has been questioned, the accuracy and precision were also evaluated with different numbers and distributions of markers.
Paper II
In paper II, we used RSA to measure the in vivo movement of the SIJ in patients with PGP in the single-leg stance.
Paper III
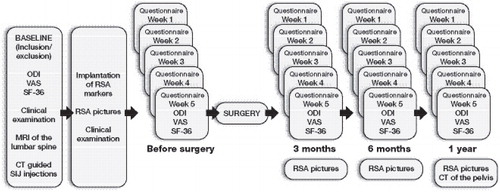
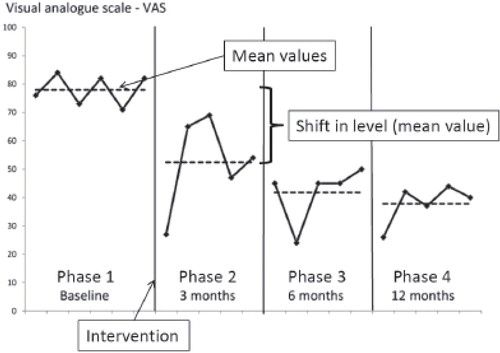
In paper III, a single-subject research design was used to evaluate the individual response and outcomes of pain, disability and health-related quality of life after SIJ fusion. The use of multiple measurements, at baseline and after the intervention, allowed us to consider the patients as their own controls. Five data collection sessions were conducted in each of the following 4 phases: prior to surgery (baseline) and at 3, 6, and 12 months after surgery.
Single-subject research design (SSRD)
A randomized controlled trial is the gold standard for examining the effects of an intervention. Because SIJ fusion is performed on few patients, a single-center randomized controlled design was difficult to apply due to the small number of available participants. Single-subject research designs (SSRDs), however, have been recommended as useful for examining clinical accountability (CitationEngel and Schutt 2009). If properly applied, an SSRD can provide a systematic approach for documenting clinical changes and can also provide evidence regarding the efficacy of a treatment modality (CitationEngel and Schutt 2009). SSRD refers to a study of a single patient or a small number of patients observed over time, during which the treatment and outcome variables are controlled. The design consists of multiple measurements before (baseline) and at different phases after the intervention (CitationEngel and Schutt 2009). The data are then presented graphically with a mean value in each phase, and the changes between the phases are shifts in level ().
Figure 10. Example of graphical presentation of data from one patient. Mean value (dotted line); all measurements in each phase (black line); the four phases (phase 1 before the intervention and phases 2, 3 and 4 after the surgery).
An SSRD focuses on individual responses and repeated measures, which improve the validity of the study. When an SSRD is replicated across patients, the internal and external validity is strengthened, allowing inferences to be made about effectiveness (CitationGonnella 1989, CitationZhan and Ottenbacher 2001, CitationLogan et al. 2008).
Paper IV
Paper IV was a cross-sectional study of the patients who underwent SIJ fusion at Hagavik Hospital in Norway between 1977 and 1998, and the data consist of surgical results 1 year after surgery and over a long-term follow-up. In 2009, all of the eligible patients () received by mail invitations to participate and a questionnaire. The long-term outcomes of the patients who underwent SIJ fusion were compared to those of a semi-matched group of patients who did not undergo this surgery. At 1 year, the surgeon graded each joint as good, fair or poor. The clinical outcomes were graded according to the following criteria. A joint with negative SIJ tests and no or minor pain that did not interfere with the patient’s work was graded “good”. A joint with obvious improvement compared to the pre-operative status and little pain but with pain that interfered with work (professional or at home) was graded “fair”. A joint was graded “poor” if there was no relief from pain or if the joint deteriorated after surgery. In cases of bilateral surgery, each of the patient’s joints could receive a different grade. According to the grading of the joints one year after surgery, the patients were allocated to three different subgroups ().
Figure 11. Each joint was graded after 1 year as good, fair or poor. For comparison purposes, three different subgroups were created based on this 1-year grading.
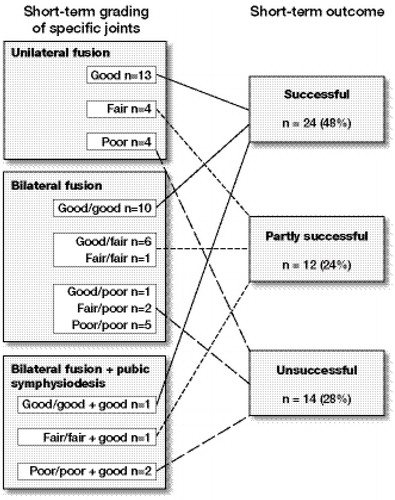
Twenty-four patients (48%) had all of their joints classified as “good” and were assigned to the “successful” subgroup. Fourteen patients (28%) had at least one joint classified as “poor” and were assigned to the “unsuccessful” subgroup. Twelve patients (24%) had their worse joint scored as “fair” and represented the “partly successful” subgroup (). These three subgroups formed the baseline for comparing the long-term effects. The patients’ 1-year outcomes were prospectively registered in a DOS Advanced Revelation relational database by the surgeons responsible for the operations.
Data collection
Papers I, II and III
The patients in papers I, II and III were included after a baseline evaluation. At baseline, a clinical evaluation was performed, and the patients completed questionnaires. It has previously been shown that female patients with PGP have variations in pain intensity during the menstrual cycle, with a relapse around menstruation (Mens et al. 1996). For this reason, the patients completed a questionnaire every Thursday for 5 weeks during each phase, to ensure that the evaluations were performed throughout the entire menstrual cycle (). The questionnaires were returned weekly by mail. All of the patients underwent 3 clinical examinations, and in all but two cases, CT-guided SIJ injections were administered before the decision to perform SIJ fusion was made. The CT-guided injections were administered by two experienced radiologists, and the patients filled out a VAS scale before and at 2 hours after the injections. The SIJ injections were not used as inclusion criteria but rather as one of several factors to strengthen the diagnosis before surgery. The patients underwent surgery to fuse the more painful SIJ, and the pubic symphysis was operated on in all of the cases.
RSA images were obtained pre-operatively and after 3, 6 and 12 months, but the pre-operative images were used in papers I and II because a pre-operative clinical test (single-leg stance) was evaluated.
Paper IV
In paper IV, the patients received a similar questionnaire to that of the patients in paper III. They completed it and returned it in a pre-paid envelope.
Outcome measures
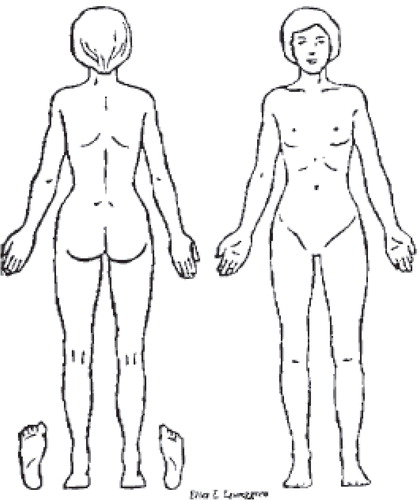
In papers III and IV, the patients completed a questionnaire consisting of the Norwegian versions of the Oswestry disability index (ODI), a visual analog scale (VAS) and the short form-36 (SF-36). Our main outcome was the ODI, and the secondary outcomes were the VAS, the SF-36 and self-reported satisfaction with treatment. In paper III, the patients also registered their pain distribution on a pain diagram.
Oswestry disability index (ODI)
The ODI was initiated by John O’Brian in 1976, and it has become one of the most commonly used condition-specific outcome measures for patients with LBP (CitationFairbank and Pynsent 2000). The questionnaire measures limitations in various activities of daily living, and the disability is graded using 10 items, for a total score ranging from 0 to 100. Each item consists of 6 statements, and these statements are scored from 0 to 5, with 0 indicating normal function and 5 a grade of high disability. A maximum score of 50 can be achieved, and this score sum is doubled and expressed as a percentage. A high score indicates a high grade of disability, and a 10-point difference represents a significant clinical change (CitationFairbank and Pynsent 2000, CitationHagg et al. 2003). The Norwegian version of the questionnaire was used (CitationGrotle et al. 2003). The ODI was tested for test-retest reliability, and at 24 hours, the reliability was 0.99. When the interval was increased to 4 days and one week, the test-retest reliability values were 0.91 and 0.83, respectively (CitationFairbank and Pynsent 2000).
Visual analogue scale (VAS)
Each patient’s most severe morning and evening pain intensity was assessed using a 100 mm VAS (0=no pain, 100=worst possible pain) (CitationRevill et al. 1976). The patients answered two questions: (1) How severe is your pain in the morning, immediately after you leave your bed? and (2) How severe is your pain in the evening, immediately before you go to bed? The VAS was found to be sensitive to changes in pain intensity, and it has been validated for this use (CitationHagg et al. 2003, CitationVon et al. 2000).
Pain diagrams
In addition to the VAS, a pain diagram was used to localize the pain and pain referrals (), and when used as a pain locator, it has shown reliable results (CitationOhlund et al. 1996). The patients were asked to draw a cross where they experienced pain.
Short form-36 (SF-36)
Health-related quality of life was assessed using the Norwegian version of the SF-36 (CitationLoge et al. 1998). This questionnaire is divided into 8 sub-scales: physical function, physical role, bodily pain, generic health, vitality, social function, emotional role and mental health. The score is converted to a 0–100 scale for each of these 8 items, and a high score indicates good health status.
Self-reported satisfaction with treatment
Additionally, the patients answered the following two questions: “Have you experienced any effects of the surgery? If so, would you grade these effects as excellent, good, some, minor or no effects?” and “How do you tolerate physical activity now, compared to before surgery?”
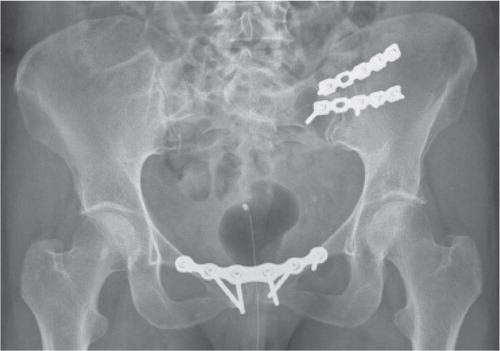
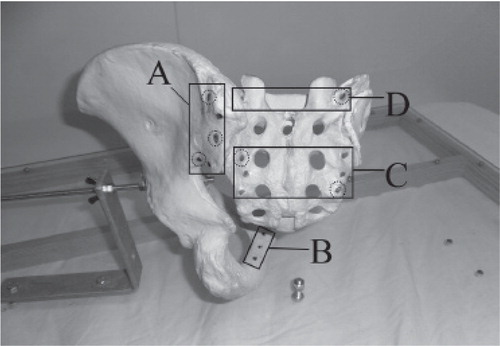
Surgical intervention
All of the patients in paper III received unilateral SIJ fusion combined with symphysiodesis. An anterior approach with a skin incision over the iliac crest was used to reach the SIJ. The joint was partially resected, and the bone was grafted with cancellous bone from the ipsilateral iliac crest. Two AO (Arbeitsgemeinschaft für Osteosynthesefragen) reconstruction plates or AO-DC plates (Synthes®, Synthes GmbH, Switzerland) were used () to achieve stabilization. The pubic symphysis was accessed through a bikini line incision. A 2 × 2 cm bone block was removed and replaced with a bone graft from the iliac crest, and a Matta plate was applied (). Post-operatively, the patients received epidural anesthesia pain relief and 1–2 days of wound drainage. The patients were advised to avoid full weight-bearing activities for 8 weeks after the surgery.
The patients in paper IV were operated on using a dorsal approach, with either trans-iliac fusion or intra/extra-articular fusion between the ilium and the sacrum. When the trans-iliac fusion was performed, an iliac window was constructed to access the joint (CitationSmith-Peterson 1921). The joint surface was cleared of cartilage and was decorticated. The cortical iliac window was used as a graft and was typically hammered into the sacrum to promote intra-articular bone formation and conduction. Additional cancellous bone was compacted around the cortical graft. In dorsal intra/extra-articular fusion, iliac crest autografts were added after joint removal and bone decortication (CitationWaisbrod et al. 1987). The pubic symphysis was fused in four patients using an open technique, with an iliac crest block bone autograft and plating.
Radiostereometric analysis (RSA)
RSA was invented by Selvik in 1974 and has primarily been used to measure the 3-dimensional motion of implants and to obtain measurements of implant wear. Small tantalum (1 mm) markers were implanted into the bone segments under general anesthesia through a small skin incision in the dorsal part of the sacrum and in both ilia.
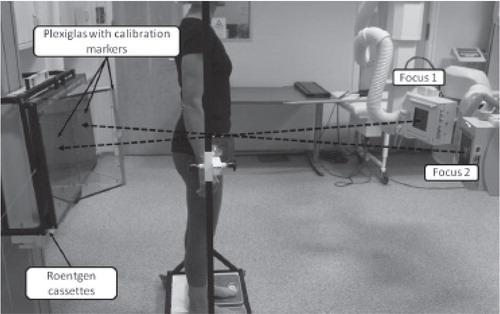
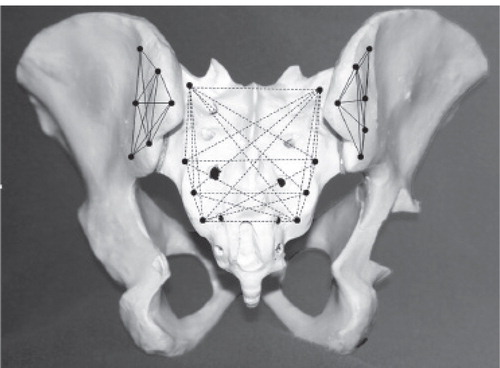
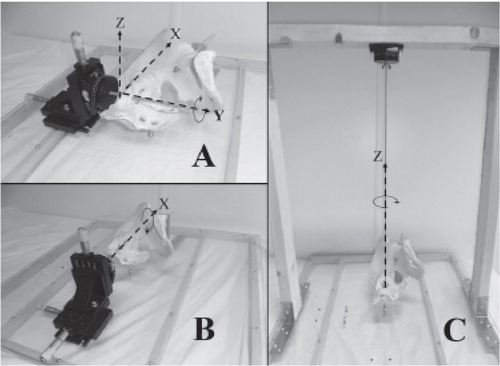
Both in the phantom and in the patients, approximately 8 markers were inserted into each bony segment (), and the movement between these marker segments was later measured. The calibration cage contained markers, so the markers in the patients could be assigned to a 3D coordinate system (). Two to 3 weeks after RSA x-rays were obtained with two angulated x-ray tubes (approximately 40°). The x-ray films were placed behind a calibration cage ().
Figure 15. Markers placed in the sacrum and the innominate bone. The markers represent a marker segment, and the movement between these segments is calculated by the computer.
Accuracy and precision of the pelvic RSA
Paper I
A good 3-D configuration relies on the distance between the markers and the distribution of the markers on all three axes, and a condition number (CN) expresses the quality of a marker segment (CitationMakinen et al. 2004). Guidelines for standardization of the RSA of implants have recommended at least three noncollinear markers in each segment (rigid body) (Valstar et al. 2005). The CN is a mathematical expression of how the markers relate to a straight line passing through the segment (CitationRyd et al. 2000). A low CN represents a good distribution of markers in the segment. A CN of less than 110 is considered a reliable distribution (Valstar et al. 2005), and an upper limit of 150 has been recommended. The CN will influence the precision and accuracy, and a factor of importance is how well the RSA system calculates the placement of each marker. The precision of each marker can be influenced by soft tissue disturbances and by the stability of the markers. If the markers are not thoroughly inserted into the bone and are partially or completely in the soft tissue, the markers can become unstable. This instability can occur in the sacrum because of the thick and strong dorsal interosseous ligaments covering the bone, particularly in the cranial part. Unstable markers should be excluded if they move more than 0.35 mm between two examinations (mean error [ME] of rigid body fitting) (Valstar et al. 2005).
The accuracy and precision of RSA have been tested in different settings and have been reported to be high. Despite the use of pelvic RSA in clinical research, the accuracy and precision have not been fully evaluated. The accuracy of the measurement is the closeness of the measurement to its true value. In phantom models, accuracy reflects the level of agreement between the true value of movement and the results obtained using RSA. Systematic error (bias) of the system occurs when the differences between systems and experiments are uniform (CitationRanstam et al. 2000). In paper I, the true value of movement was measured with a phantom attached to a micrometer (), and these values were compared to the measurements from pelvic RSA. This value should ideally be zero.
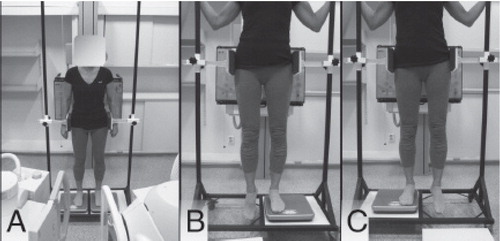
Figure 18. The setup of the pelvic phantom with the sacrum attached to a translation stage and a rotation rod are shown for (A) Y rotation and all translations, (B) X rotation, and (C) Z rotations.
The precision (spread) of the measurement is the degree of closeness of repeated measurements under unchanged conditions. Under optimal conditions, the difference between two examinations should be zero (CitationRanstam et al. 2000). The precision was measured in the phantom model and was evaluated in the patients using 17 double examinations in six patients.
To evaluate the influence of different marker distributions on accuracy and precision, the eight markers in each segment were divided into four different marker segments (). We wanted to determine whether the markers in the pubic symphysis could increase the precision and how many markers were needed in each segment to achieve precision and accuracy. To examine the need for frontal markers, we performed tests with and without frontal markers. To examine the need for cranial markers in the sacrum, we performed tests with and without these markers. Finally, three dorsal markers in the ilium and three markers in the sacrum were randomly selected () and were tested against eight markers.
Figure 19. The RSA markers were divided into different marker segments (MS): MS A = five dorsal markers in the ilium; MS B = three frontal markers in the inferior pubic ramus; MS C = six sacral markers; and MS D = two cranial markers in the sacrum. Circles = three randomly selected markers in the ilium and three randomly selected markers in the sacrum.
In paper II, three pairs of images were obtained: one with the subject standing on both feet, one with the subject standing on the right foot and one with the subject standing on the left foot (). The sacrum was defined as the fixed segment, and the movement of the innominate bone was relative to the sacrum.
Main results
Paper I
Overall, the RSA method applied to the SIJ was found to be accurate and to have high precision.
Accuracy
When we applied translations and rotations to the micrometer, the RSA had good ability to detect these movements. With 8 markers in both the sacrum and ilium, the mean accuracy was between -0.03° and 0.05° for the rotations (). For translation, there was a small underestimation in the Z-direction of 0.07 mm. The resolution of the micrometer was 0.04° and 0.01 mm; therefore, these deviations from zero were not sufficiently large to be considered a systematic error that required correction.
Table 3. Accuracy of the phantom
Precision
For the RSA measurements in the phantom, there was high precision in all of the analyses, from 8 markers in each segment down to 3 markers in each segment. The precision (LOS) in the phantom was between 0.06° and 0.25° for rotation and between 0.03 mm and 0.16 mm for translation with 8 markers in each segment; with 3 markers in each segment, the precision was between 0.14° and 0.26° and between 0.09 mm and 0.21 mm. The precision in the patients was lower than in the phantom, with precision for rotation between 0.2° and 0.7° and for translation between 0.3 mm and 0.5 mm.
Analysis of different marker distribution and numbers of markers
The CN in the phantom varied from 17 to 59 in the sacrum and from 29 to 117 in the ilium, with varying numbers of markers and different marker distributions. When the markers placed in the symphysis were removed from the phantom, the CN increased from 29 to 92. The ME was reduced (p = 0.001) when the frontal markers were removed. There was no difference in the accuracy, but the precision decreased from 0.11° to 0.22° in the Z rotation (p = 0.010) and from 0.08 mm to 0.18 mm in the X translation (p = 0.003). In vivo, the removal of the frontal markers did not affect the precision. The CN in the ilium increased from 38 to 96 (p = 0.001), and the ME had a tendency (p = 0.048) to be lower in the ilium without the frontal markers. When the two cranial markers were removed, there was a reduction (p = 0.012) in the accuracy of the Y translation from -0.03 mm to -0.01 mm, and the precision was reduced from 0.11° to 0.22° in the Z rotation (p = 0.023), as well as in the X translation (p = 0.005), where it decreased from 0.08 mm to 0.24 mm. When three randomly selected markers were analyzed compared with eight markers, there were reductions in the precision of the Y and Z translations (p = 0.016 and p = 0.013, respectively), but there was no reduction in accuracy.
Paper II
Eleven patients (4 from Norway and 7 from Sweden) with long-term PGP were analyzed. Only small movements in the SIJ were detected, and only 15% of the measurements exceeded the precision of the RSA. Although some of the mean values were significantly different from zero, all but one of these mean values was less than the precision of the RSA.
The main findings in this study were as follows.
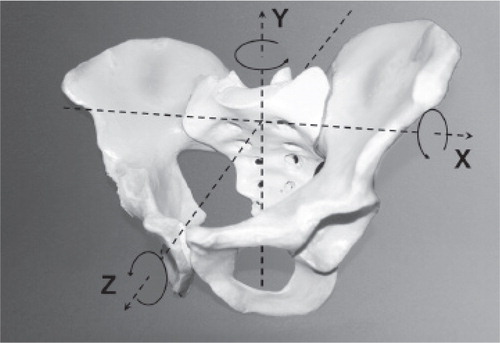
• When the patients performed a single-leg stance, there was almost no detectible movement.
• There was a mean of 0.5° of rotation on both sides around a helical axis (the true axis of rotation).
• When the movements were assessed based on the coordinate system (), a small, 0.3° (SD 0.2) rotation around the Z-axis in the SIJ of the standing leg (p < 0.001) was observed. This rotation was significantly different from that of the hanging-leg SIJ (p = 0. 036).
• No translations were detected.
• With the exception of the 0.2° difference observed in the Z-axis rotation (p = 0.036), no differences were observed in the movement between the SIJs of the standing leg and the hanging leg (p-values between 0.055–0.978).
• There were no differences between the 18 symptomatic joints and the four asymptomatic joints with regard to the total amount of rotation (diff: -0.2, p = 0.335 on the standing side; diff: 0.0, p=0.896 on the hanging side) or translation (diff: -0.1, p = 0.398 on the standing side; diff: 0.1, p = 0.687 on the hanging side).
Paper III
Nine consecutive patients received unilateral anterior SIJ fusion with concomitant fusion of the pubic symphysis. One patient developed chronic fatigue syndrome during the follow-up and dropped out of the study after 6 months. The remaining eight patients followed the study protocol; the baseline characteristics of these patients are presented in .
Table 4. Pre-operative patient characteristics
The ODI scores for each patient are presented in . All but one patient exhibited a decrease of more than 10 points on the ODI from the pre-operative period to the 1-year follow-up. One patient experienced no effects. There was a strong association between ODI and time, with a 17-point decrease (p <0.001) at 1 year after surgery (). The graphs showed significant variations in the measurements at each time point. At baseline, a difference of more than 40 points between the maximum and minimum values was observed in two patients, and only two patients had less than a 10-point difference.
Figure 21. The mean ODI of each individual patient is presented, together with the regression line from the mixed model (ODI = 54.2 – 5.7 × time).
The VAS scores of each patient are presented in . The patients experienced a reduction in pain, with a decrease from 82 points at baseline to 57 points after 1 year (p < 0.001, regression coefficient of -8.4) (). All of the patients reported a decrease in pain. Pre-operatively, a difference of 43 points between the maximum and minimum scores was observed in one patient, and none of the patients had variations of less than 10 points.
Figure 22. The mean VAS of each patient is presented, together with the regression line from the mixed model (VAS = 81.7 – 8.4 × time).
At baseline, seven of eight patients had bilateral SIJ symptoms. At the 1-year follow-up, only two patients experienced pain in the fused joint; however, six of the seven patients reported discomfort on the contralateral side. Seven patients had pain in the pubic symphysis before surgery, and five continued to have pain in this area at the 1-year follow-up.
On the SF-36, the patients experienced a mean 20-point improvement in physical function and bodily pain (p < 0.001), a 15-point improvement in social functioning (p = 0.008) and a 6-point improvement in general health (p = 0.009).
All of the patients reported that the surgery had positive effects; one patient reported minor effects, two reported some effects, and five reported good effects of the surgery. None of the patients reported excellent results. With regard to tolerance of physical activity, seven patients reported some improvement, and one patient reported major improvement.
There were 3 major complications: one infection, one case of complex regional pain syndrome with drop-foot and one loss of bladder sensation. There were also 3 cases of transient sensitivity loss of the lateral femoral cutaneous nerve as a possible complication of bone harvesting from the iliac crest. All of the patients reported high post-operative pain levels, and they required epidural treatment for 5–7 days. They were hospitalized for 7–10 days and were discharged with prescribed opioids.
Paper IV
The demographics of the patients who did and did not undergo surgery are presented in . The non-surgical group was younger and had a shorter follow-up period than the surgical group.
Table 5. Characteristics of the participants in the long-term follow-up study
The patients who underwent surgery had a mean ODI of 33 (95% CI 24–42) and an evening VAS of 54 (95% CI 46–63) 23 years after SIJ fusion (). The subgroup of patients with a successful 1-year outcome had significantly lower scores on the ODI and the VAS than the patients with unsuccessful outcomes at 1 year. There was a 16 point difference in ODI score between these two groups, and this difference was regarded as both clinically and statistically significant (p=0.034). The difference in VAS between these two groups was 28 (p=0.011). There were positive correlations between the 1-year outcome and three different long-term outcomes; VAS in the morning (ρ = 0.34, p = 0.0016), VAS in the evening (ρ = 0.42, p = 0.013) and ODI (ρ = 0.43, p = 0.002). There were no significant differences in ODI (p = 0.54), morning VAS score (p = 0.54), evening VAS score (p = 0.50) or SF-36 score between the group that underwent surgery and the non-surgery group at the long term-follow-up.
Table 6. Results of Oswestry disability index, visual analogue scale and SF-36. Values are adjusted means (95% CI)
Discussion
Methodological considerations
Study designs and patient selection
The study design and the patient selection are important for drawing scientific conclusions from studies and, furthermore, to make the results generalizable. When these subjects are discussed, the terms internal and external validity are often used, and these terms address different quality aspects of the study. Internal validity is e.g. the extent to which the observed effect of an intervention can be explained by the treatment itself, rather than by chance or other systematic errors. Internal validity must be good to be able to draw conclusions that can be generalized (Citationvan der Worp et al. 2010). The study must be reproducible and reliable, and any form of bias should be minimized. External validity, in contrast, is the extent to which the results can be generalized.
Paper I
Paper I reported a methodological study in which we used a phantom model to attempt to explain what occurs in vivo. The external validity of a phantom model study can be questioned because the results from a phantom study cannot be transferred directly to the analysis of patients. Therefore, we analyzed precision in both the phantom and in patients. When the 3D position of each individual marker was calculated, the soft tissue was an important factor that could disturb x-rays, and the markers were likely not as stable in patients as in the phantom. These factors rendered the measurements in patients less accurate and less precise. Hence, patient precision should always be determined by double examination. We used a micrometer as the “gold standard” or true value. This micrometer had a resolution of 0.04° and 0.01 mm. The accuracy was less than 0.07 mm for translation and 0.05° for rotation; better resolution would be required to allow the conclusion that this deviation constituted actual bias (systematic error). The bias measured in our study was small and could be explained by the resolution of the micrometer. An interpretation of this bias might be that the RSA method had no bias that had to be corrected for when the measurements were obtained.
As expected, the precision was better in the phantom than in the patients. In the patients, the precision of the rotations had an LOS of less than 0.7° in all directions, and the precision of the translations was less than 0.5 mm. These values were comparable to the precision measurements reported by others (CitationTullberg et al. 1998, CitationSturesson et al. 2000b). The RSA method has been widely used in the study of hip prostheses. Using double examinations, precision has been reported to be between a low of 50 µm and 150 µm (CitationBragdon et al. 2002). When RSA is used in the SIJ, the segments are large, although the spread of the markers occurs mostly along a craniocaudal straight line in the ilia. However, the distance between the segments (sacrum and ilium) is larger than in the analysis of the implants. Abdominal and pelvic soft tissue can also decrease the quality of marker visualization on radiographs. Furthermore, absolutely zero motion between two examinations can hardly be expected. Because the patients were allowed to move between examinations, it is possible that the joints might have aligned differently between the two examinations. Hence, when precision is evaluated in patients, the joint alignment must be considered. All of these factors could explain why the precision was lower than the numbers reported in the analysis of the implants.
We evaluated the RSA in our lab with our set-up and equipment. One could argue that this evaluation weakened the external validity. However, the software that we used had the ability to compensate for the deviation automatically because it retrograde-calculated the positions of the tubes depending on the control markers in the calibration cage. As long as the same software is used, our results should be transferable to other studies as well.
Paper II
We believe the internal validity of measuring movement in the SIJ during the single-leg stance to be good. Both the method and the patients were well described, and the study could easily be replicated. We knew about the high accuracy and precision from paper I, and we did not find any bias for which we had to correct. We also included patients suffering from clinically verified severe PGP; hence, we believe these results to be sustainable.
External validity might have been influenced because only 11 patients were included. They were, however, recruited from two different clinics, and the results were uniform between the two clinics, strengthening the validity of our results.
Paper III
The study design is an important factor in strengthening internal validity. In a prospective registration with repeated measures, such as an SSRD, some of the threats to internal validity can be controlled. Recommendations have been made to rate the quality of an SSRD, and a 14 question checklist was developed to obtain a quality rating (CitationLogan et al. 2008). According to this quality rating, a study can be categorized as strong if more than 11 out of 14 questions can be answered in the affirmative. The 14 questions are divided into five different items: descriptions of the participants, independent variables, dependent variables, design and analysis.
First, the participants should be well described to enable replication of the study. There are no defined criteria to select patients for SIJ fusion. The diagnosis of PGP is mostly based on medical history and a combination of different clinical tests (CitationVleeming et al. 2008). Radiological examinations are primarily used to exclude serious pathologies that could explain the symptoms, and SIJ injections are administered to attempt to establish evidence for the SIJ as the origin of PGP. In our inclusion criteria () we used the medical history of pelvic joint pain, a combination of 5 different clinical tests, a high level of disability measured by the ODI and a high level of pain measured by the VAS. In addition, the patients had to have undergone conservative treatment without positive effects. We did not include the SIJ injection among the inclusion criteria because there is uncertainty about the diagnostic value of SIJ injections, particularly when this procedure is performed infrequently (CitationSimopoulos et al. 2012). We performed SIJ injections in most of the patients, and the results might have influenced the final decision regarding whether to perform surgery as the effect of the injection was not blinded for the research team. Similar inclusion criteria have been used in many of the studies published in recent years. Hence, we believe that our study can be reproduced, and furthermore, the results can be compared with those of other studies in which SIJ fusion is performed (CitationRudolf 2012, CitationCummings and Capobianco 2013, CitationEndres and Ludwig 2013). Concerning the first item regarding description of participants, one point could be added to the total score.
The next two items on the checklist consisted of six questions about independent and dependent variables. The intervention was well described in our study and could be easily replicated. We also believe that the independent variables were well defined because a thorough presentation of the patients was undertaken. The dependent variables are well known and described. The ODI, VAS and SF-36 have been tested for test-retest properties, and the questionnaires have been evaluated for use in the Norwegian population (CitationLoge et al. 1998, CitationGrotle et al. 2003). To score six of six points on these questions, the assessors had to be unaware of the phases of the study, and in our study, we had no opportunity to comply with this requirement. Both the patients and the examiners were fully aware of the phase in which they were. The last quality criterion in item covering the dependent variables was the stability of the measurements. Our patients did not show stability of measurements during any phase. Patients with PGP have reported cyclic variations in symptoms, and as many as 72% report relapses during menstruation (CitationMens et al. 1996). To account for these potential variations, we repeatedly collected the patients’ data for a 5-week period and discovered a large variation in the values during each phase. For some patients at baseline, a 40-point difference in the ODI and a 43-point difference in the VAS were observed over the 5-week period. Although the stability of the measurements is important for internal validity, one strength of an SSRD is its ability to detect these individual variations, which is important for studying patients with PGP. Some of these variations could be corrected for in large group studies, but conclusions from small case series, with single measurements, should be interpreted with caution because these threats to the internal validity cannot be controlled. Another finding that strengthened the validity of this study was that we measured both morning VAS and evening VAS. Patients with PGP have reported experiencing more pain in the evening than in the morning (CitationStuge et al. 2004b), and we found a difference of more than 20 points in the VAS between the morning and the evening. Furthermore, the evening pain showed a greater decrease between baseline pre-operatively and at 1 year of follow-up. Hence, when the VAS score is used, this variation must be taken into consideration. According to the SSRD quality checklist, our study scored 4 of 6 points in the questions regarding independent and dependent variables.
The next item covers the description of the design. The study was conducted according to guidelines for SSRDs (CitationZhan and Ottenbacher 2001, CitationGrotle et al. 2003, CitationEngel and Schutt 2009), and an adequate number of participants (more than 3) was investigated. To score the maximum on this item, the effect should be observed in three or more subjects, and in our study, 7 of 8 experienced positive effects of the intervention. Because all of the questions on this item were answered affirmatively, 3 more points could be added for a total score of maximum 14.
The last item covers the analysis of the data. We presented the data according to the guidelines, and because we had 8 patients, we were also able to conduct a statistical analysis of the whole group. All 4 of the criteria concerning analysis of the data were met, and the total of the SSRD rating was 12 of 14, which is regarded as strong quality by the authors of the rating system (CitationLogan et al. 2008).
One other threat to the internal validity, which is not addressed in the rating, is that the observed results were normal variations in symptoms, and there was another event between baseline and follow-up that could explain this effect. The patients had a chronic condition with mean 11-year duration, so we believe the baseline phase was representative of the pre-operative status. To correct for events in between that could explain the measured effect, we obtained measurements in 3 post-operative phases.
With an SSRD, the findings are generalizable if the study is replicated among 3 or more subjects (CitationLogan et al. 2008). The patients included in papers I, II and III had severe PGP, and they had symptoms from the pelvic girdle for an average of 11 years. They had a mean baseline ODI value of 54, a mean morning VAS of 60 and a mean evening VAS of 82, and only patients with an ODI greater than 40 and/or a VAS greater than 50 were included. Hence, this was a selected group of patients with PGP. In comparison, patients with PGP in the weeks after pregnancy were reported to have an ODI of 42 and an evening VAS of 58 (CitationStuge et al. 2004a). The patients reported by Stuge et al. (2004a) did not reach a chronic phase and responded well to conservative treatment. Our patient selection was undertaken by applying strict inclusion criteria, and lumbar spine pathology was excluded by lumbar MRI. Hence, we believe that these patients were representative of patients with severe and long-lasting chronic PGP. The results, however, should be interpreted with the knowledge that these patients were a selected group of patients.
A randomized controlled trial is the gold standard for examining the effects of an intervention, and an understanding has developed that only group studies can produce scientific data (CitationGonnella 1989). Because SIJ fusion has been performed on few patients, a single-center randomized controlled design was difficult to establish due to the small number of participants. However, a single-subject research design (SSRD) has been recommended as a useful method for examining clinical accountability (CitationZhan and Ottenbacher 2001). When an SSRD is replicated across patients, the internal and external validity is strengthened and allows inferences to be made about effectiveness. Pelvic fusion in patients with PGP is a rare procedure and is only performed in severe cases in which conservative treatment modalities have been unsuccessful. A randomized controlled trial of this procedure was difficult to perform because the alternative treatment modality (conservative treatment) had already been attempted by most of the patients. Hence, compliance in such a conservative group could have been a great challenge. Because an SSRD with multiple measurements is designed to study small samples of patients, this design was chosen. A limitation of our study was the short follow-up period of 1 year, which is regarded to be too short for a clinical trial, but in paper IV, we reported that the 1-year outcomes after SIJ fusion were sustained 23 years later. Hence, a 1-year follow-up might be sufficient. Despite the limitations of the SSRD, we believe that our study contributes valuable information regarding the effects of pelvic joint fusion.
Paper IV
The design of the study in paper IV was cross-sectional and included 50 patients with SIJ pain who underwent SIJ fusion, combined with a long-term follow up. The 1-year outcomes were compared to outcomes recorded in 2009 and to a comparison group. To compare the 1-year results, a sub-group classification was created (), and we were aware of the limitations of this subgroup classification. The sub-grouping might not have been optimal, although the post-operative joint pain was classified according to specific criteria. The primary aim of the study was to examine the long-term outcomes of SIJ fusion, not to evaluate the effects of the surgery compared to a control group. There was great selection bias in the two groups. First, they differed in age and length of follow-up, and second, they most likely did not have the same baseline status in pain and function. The comparison must be interpreted with these limitations in mind.
We found a correlation between the 1-year results and the long-term results. With the same inclusion criteria and the same surgical technique, these results could be generalized to this population. With a long-term follow-up, there are several opportunities for bias. We only examined 50 patients, and because the follow-up was as long as 23 years, some of these patients could have experienced other events that would explain the findings.
Outcome measures
Because PGP is a multi-factorial condition, a questionnaire should address different aspects of the patient’s experience. To detect changes in pain, disability, and health-related quality of life, we used three different questionnaires: the ODI, a VAS and the SF-36. There are several generic instruments that measure pain perception, functional disability and health-related quality of life, but when we started this project, no condition-specific questionnaire was available (CitationStuge et al. 2011). Because PGP is a subtype of low back pain with a unique clinical presentation (CitationO’Sullivan and Beales 2007), a condition-specific questionnaire, the Pelvic Girdle Questionnaire, was later developed (Stuge et al. 2011). The closest to a condition-specific questionnaire that was available were the ODI, the Quebec Back Pain Disability Scale and the Roland Morris scales, and these instruments have frequently been used in research on PGP (CitationVleeming et al. 2008). We used the ODI because most studies have used this questionnaire to investigate interventions in PGP, and it has been shown that the ODI is an appropriate instrument to measure changes in functional status in patients with chronic LBP (CitationGrotle et al. 2004).
We decided to use a VAS instead of a numeric rating scale because most of the studies used this outcome measure after SIJ fusion (CitationKeating et al. 1997, CitationSchutz and Grob 2006, CitationZiran et al. 2007). A numeric rating scale would most likely have been better than a VAS to detect changes in chronic patients (CitationGrotle et al. 2004), because the responsiveness has proven to better for NRS compared to VAS when these scales are used on chronic patients. In addition to the VAS, a pain diagram was used to localize local pain and its referrals; for this use, the pain diagram has shown reliable results (CitationOhlund et al. 1996).
As a generic instrument, we used the SF-36, which has also been used in the evaluation of patients undergoing SIJ fusion (CitationBuchowski et al. 2005). The Norwegian versions of the questionnaires have been evaluated, and they have sufficient properties with regard to validity, reliability and responsiveness (CitationLoge et al. 1998). With the selection of these outcome measures, we first hoped to detect possible changes in pain, physical function and health-related quality of life after SIJ fusion, and second, we were able to compare our results to the available literature.
The SIJ
Movement in the SIJ
The literature has disagreed regarding the amount of movement that occurs in the SIJ, with reports ranging from movement that can be detected by an examiner (CitationHungerford et al. 2007) to RSA studies demonstrating almost no movement (Sturesson et al. 1989, Sturesson et al. 1997, Sturesson et al. 1999, Sturesson et al. 2000b, Sturesson et al. 2000a, Tullberg et al. 1998). The first aim of thesis was to determine whether the RSA was reliable (paper I). In the phantom model, we measured the accuracy and did not find any bias that had to be corrected for when this examination was used. In the patients, the RSA had a precision for translation of less than 0.5 mm in all directions, and for rotation, the precision was less than 0.3° around the Y and Z axes and 0.7° around the X axis (). We also discovered that the markers only needed to be placed in the dorsal part of the pelvis and that 3-4 markers were sufficient if the marker distribution was good (appropriate three-dimensional distances between the markers). We found the RSA technique to be highly accurate and precise. We therefore concluded that the RSA results were reliable and valid because these reports used the same set-up. Nevertheless, some questions regarding the SIJ movements should be addressed.
What is the movement in the SIJ?
There has been evidence that, during and after pregnancy, movements are increased in the pelvic joints and that patients with pain have greater movement than asymptomatic controls (CitationMens et al. 2009). However, the importance of SIJ movement when patients develop chronic PGP is more uncertain. Some RSA studies have been performed, and the overall findings were that the movement in the SIJ is small, and it seems to be normally distributed (Sturesson et al. 1989). When changing from a supine to a standing position, a total of 1.2° of forward rotation of the sacrum has been reported relative to the innominates, and the movement is 1.6° when the patients change from a supine to a sitting position (Sturesson et al. 1989). In the standing position, the SIJ seems more or less locked. Using RSA, Sturesson et al. (2000b) found a total of 1.2° of rotation in each SIJ when alternating among the straddle position, standing with the left hip maximally extended and right hip maximally flexed and standing with the right hip maximally extended and the left hip maximally flexed. When these authors analyzed the movement during the standing hip flexion test (movement between standing on both feet and standing on one foot with the other hip maximally flexed), a small total movement of 0.6° was reported (Sturesson et al. 2000a). This finding contradicted those of CitationHungerford et al. (2007), who stated that the SIJ movement could be felt by hand during the Stork test. In addition, Sturesson et al. (1989) did not find any differences in movement between symptomatic and asymptomatic SIJs. Hence, there is movement in the SIJ, but there does not seem to be hyper-mobility of the SIJ in patients with chronic PGP (CitationHungerford et al. 2007, Sturesson et al. 1989).
If the SIJ has a limited range of motion, why should we even attempt to measure the SIJ movement in the diagnosis of PGP?
The Chamberlain x-ray projection has been used to attempt to diagnose SIJ movement, and in paper II, we wanted to determine whether there was movement in the SIJ during the single-leg stance test. We only found minor movement, with total rotation of 0.5° in both the standing leg SIJ and the hanging leg SIJ. Researchers have used this method to establish a relationship between movement detected in the pubic symphysis and pain in the SIJ (Anderson and Peterson 1944, Chamberlain 1930, CitationMens et al. 1999, Siegel et al. 2008), but the findings have not been uniform. Hence, based on the results of paper II, the Chamberlain examination was likely inadequate for examining SIJ movement in patients with PGP. Furthermore, there did not seem to be any difference between symptomatic and asymptomatic SIJs. Based on the range of motion being limited and the measuring methods lacking proper precision, it does not seem valid to measure SIJ movement in clinical practice.
If the range of movement in the SIJ is limited, why would SIJ fusion help these patients?
As described in the European guidelines, the stability of the SIJ is more a matter of altered laxity or stiffness than an increased range of motion (CitationVleeming et al. 2008). Using Doppler imaging and small vibrations made by a vibrating device, authors have been able to measure laxity (CitationDamen et al. 2002a, CitationDamen et al. 2002c). During pregnancy, increased laxity of the SIJ has been reported, but the values returned to pre-pregnancy status within 8 weeks (CitationDamen et al. 2002a). In this study, the authors found that asymmetrical laxity during pregnancy was associated with increased pain post-partum, but the magnitude of the laxity was not important. In another paper, the same authors demonstrated that a pelvic belt reduced laxity (CitationDamen et al. 2002b), and a pelvic belt was also shown to increase the functional abilities of patients with PGP because the ASLR improved with a pelvic belt (CitationMens et al. 1999). Sturesson et al. (1999) demonstrated that the movement was reduced by 50% when a pelvic frame was applied to the pelvis. The use of an external frame has been reported to reduce pain in patients with PGP (CitationSlatis and Eskola 1989). Hence, pelvic mobility could be more a matter of laxity within a small range of motion, and because a stabilizer such as a pelvic belt or frame can reduce symptoms, SIJ fusion might be an appropriate treatment option in some severe cases (Sturesson et al. 1999).
The SIJ as a pain generator
The SIJ has neural structures in the joint and in the surrounding ligaments, and these structures can be stressed, with pain as a consequence. However, there have been many theories and models created to explain the underlying causes of PGP and SIJ pain. It has been emphasized that the disorder of PGP must be viewed in a bio-psycho-social framework because many factors are important when treating a patient with a long-term pain syndrome (CitationO’Sullivan and Beales 2007).
In our studies, we primarily examined the bio-mechanical properties of the SIJ. Sacroiliac fusion immobilized the SIJ, and the effects could be observed as a direct consequence of increased stabilization of the pelvic joints. With this approach to the problem, the premise was that the SIJ was the major pain generator. According to the results of SIJ injections in patients with PGP, as well as in patients with non-specific LBP, this premise could be true (CitationSimopoulos et al. 2012). With a single injection and with a cut-off of between 50% and 80% pain relief, an average prevalence of 30–35% was observed, and a higher cut-off (>80%) yielded a slightly lower prevalence (CitationSimopoulos et al. 2012). With a dual block (confirmatory blocks), the prevalence was estimated to be 25%, but with a wide range of 10–40%. When SIJ injections have been used as a “gold standard”, the prevalence has varied because the “gold standard” is not standardized. Furthermore, the patients have often been selected differently, resulting in a prevalence with a broad range. Schwarzer et al. (1995) studied 100 patients with low back pain, and after screening (pain below L5–S1 and over the SIJ), 43 patients were assigned to SIJ injections due to suspected SIJ pain. Thirteen of 43 experienced positive effects from the injections (more than 75% relief), representing a 30% prevalence in patients with suspected SIJ pain, but in the entire sample of LBP patients, the prevalence was 13%. Hence, in a selected population, the prevalence became greater. Using injections only, Laplante et al. (2012) found a 18% prevalence of SIJ pain in 153 cases of patients with non-specific LBP, and interestingly, the prevalence in a population of 54 patients with suspected SIJ pain was 19% (CitationMaigne et al. 1996). The highest prevalence reported was 62% in a highly selected group of patients (CitationSlipman et al. 1998). These patients had 3 positive SIJ provocation tests, and they were assigned to a rehabilitation program. Those who failed this program received diagnostic SIJ injections. Thirty-one of 50 had positive responses to the injections, yielding a prevalence in this population of 62%. Based on these investigations, it seems that the SIJ could be a source of pain in a large proportion of patients with suspected PGP, as well as in patients with non-specific LBP.
Some researchers have proposed that the pain is caused by subluxation or displacement of the SIJ, and the treatment has thus primarily been based on manipulation to correct this (CitationO’Sullivan and Beales 2007). Positive short-term effects of this treatment have been reported (CitationWright 1995), but the effects did not seem to last. Although these manipulations have effects on the symptoms, the position of the SIJ does not seem to be altered during these treatments (Tullberg et al. 1998). Hence, subluxation of the joint as a reason for PGP seemed not to be correct.
Disturbances in the motor control of the lumbo-pelvic musculature has been emphasized as a possible cause of PGP because this impairment alters the ability to transfer load through the pelvis and triggers nociceptive structures (CitationO’Sullivan and Beales 2007). A treatment program focusing on training in motor control has been shown to have statistically and clinically significant and long-lasting effects on PGP post-partum (Stuge et al. 2004a, Stuge et al. 2004b), but some patients did not respond to this treatment. Different patterns of motor control impairments could explain these findings, and PGP has been associated with both excessive and insufficient motor activation of the pelvic musculature (CitationO’Sullivan and Beales 2007). It has been suggested that over-activity of the pelvic floor muscles might reduce force closure by counter-nutation in the SIJ, and it could be a possible mechanism for maintaining pain and disability in patients with PGP (CitationPool-Goudzwaard et al. 2004). Stuge et al. (2012, 2013) found that women with PGP had a statistically significantly smaller levator hiatus, even at rest, and a tendency for higher vaginal resting pressure might indicate increased activity of the pelvic floor muscles. The reason for this is unknown, but could be a response to SIJ pain. Under pelvic floor muscle contraction, the coccyx moves in a ventral and cranial direction (CitationBo et al. 2001), and it most likely generates counter-nutation in the SIJ (CitationPool-Goudzwaard et al. 2004). Because counter-nutation might lead to increased tension in the ligamentous structures (CitationSnijders et al. 1993), sustained contraction of the pelvic floor muscles might be a non-optimal strategy, leading to stress on the ligaments and resulting in pain. Palsson and Graven-Nielsen (2012) recently showed that superficial ligament structures were potential pain sources in PGP (Palsson and Graven-Nielsen 2012, Stuge et al. 2012, Stuge et al. 2013).
Another group receiving increasing interest is patients with failed back surgery. In patients with persistent pain after spinal fusion, Depalma et al. (2011) used SIJ injections and found the SIJ was the source of pain in 43%, and 83% of these patients had fusion to the sacrum. These findings were similar to those of another study that found 35% positive blocks in patients with pain after spinal fusion (CitationMaigne and Planchon 2005). Increased SIJ degeneration was found, compared to un-operated subjects, 5 years after spinal fusion, particularly in cases with lumbosacral fusion (CitationHa et al. 2008). Patients with a suspected SIJ origin of pain after spinal fusion also reported a different type of pain than that for which they primarily underwent surgery (CitationMaigne and Planchon 2005). The importance of SIJ degeneration in patients with suspected SIJ pain is not fully understood because degenerative changes have been observed in both asymptomatic and symptomatic patients (CitationElgafy et al. 2001). However, with the use of finite element analysis, increased stress in the SIJ has been reported, particularly if there was a sacro-lumbar fusion (CitationIvanov et al. 2009), and increased tension on the SIJ structures can possibly cause pain. Based on these studies, the SIJ could be a pain generator in patients with failed back surgery; furthermore, these patients have reported responding positively to SIJ fusion (CitationRudolf 2013).
Surgery as a treatment for PGP
In paper III, we found a mean 17-point decrease in the ODI (from 54 to 37) and a mean 25-point decrease in the VAS (from 82 to 57) one year after SIJ fusion was performed. Pre-operatively, these patients had a high degree of disability and high levels of pain. One patient did not experience any effects from the intervention, but the remainder had significant decreases in ODI and VAS scores. The minimal clinically significant difference has been suggested to be 10 points in the ODI (CitationHagg et al. 2003), and in our study, 7 of 8 patients achieved this difference. For the VAS, the minimal clinically significant difference has been suggested to be 18 (CitationHagg et al. 2003). Six of 8 patients had a change of 18 or greater on the VAS: one had a 16-point change, and one had a small change of only 3. As a group, the patients experienced positive effects from surgery, and the changes seemed to be of statistical and clinical significance.
In the long-term follow-up (reported in paper IV), the patients had a mean ODI score of 33 (95% CI: 24–42) and a mean VAS score of 54 (95% CI: 46–63), comparable to the 1-year results reported in paper III. Compared to a comparable non-surgery group, the operated patients in the long-term follow-up had lower ODI (33 compared to 37) and VAS scores (54 compared to 60), but these differences were not statistically significant. There are possible explanations for this lack of difference. The most tempting interpretation to make of this finding is that SIJ fusion had no effects, but the study was not designed to draw such a conclusion. The non-surgery group differed from the surgery group with regard to age and length of follow-up. The non-surgery group was diagnosed with severe PGP by the same surgeon, but the patients in that group were likely less disabled at baseline than the group of patients who underwent surgery; hence, the comparison might have had limited validity. What was discovered, however, was that the patients with successful short-term results had significantly better outcomes than the patients with poor short-term results, and the short-term results were correlated with both the ODI and VAS over the long-term follow-up. The studies in both paper III and paper IV had specific selections of patients, and with the use of the inclusion criteria described in paper III, it seems that positive effects from surgery could be expected.
In our study (paper III), there was clinical improvement, but the patients continued to have moderate disability and relatively high pain scores after 1 year, and one patient did not experience any effects at all. One explanation for this finding is the limitation of the use of outcomes. Most of the patients had bilateral SIJ pain at inclusion (7 of 8), but only the most painful joint and the symphysis were fused. Because the outcome measures tested the overall pain and functioning of the patients, the non-fused joints influenced the measured values of the ODI, VAS and SF-36. In paper III, 6 of 8 patients were pain-free in the fused joint, but six of seven reported pain on the contralateral side, which could indicate that the function and pain could have been further improved if the patients had undergone fusion of the other joint as well.
How do our results compare to those of other studies?
When the literature was explored, only 28 original papers and 2 book chapters were found (), and most of the older papers did not include any validated outcome measures. There were only case seriess without control groups. The patient selection and surgical techniques also differed in almost every paper, and no studies reported the outcomes of our surgical method. Hence, a comparison of our results to others is difficult, but there have been several studies that have reported the outcomes of SIJ fusion using similar inclusion criteria. A positive effect of surgery has been observed in 50% to 90% of patients (), and this finding is in accord with the positive effects observed in our 1-year outcomes. In a prospective study of 58 patients, Citationvan Zwienen et al. (2004) reported a mean increase in physical outcomes from 37 to 61 (p < 0.001) as measured using the Majeed score (0 – poor, 100 – good), and the same positive results have been reported in several papers (, ).
Table 7. Outcome of studies using ODI or/and VAS/NRS as outcome measures
Although positive results have been reported, a number of patients have not experienced effects from surgery. In our long-term study, 28% of patients did not experience any effects from surgery, and these findings were comparable to those of other studies (Citationvan Zwienen et al. 2004, CitationBuchowski et al. 2005, CitationWise and Dall 2008, CitationRudolf 2012, CitationDuhon et al. 2013, CitationSmith et al. 2013). Most of these patients had complications or non-union events, but some experienced no effects without any clear explanation. Open surgery causes extensive surgical trauma, and some of these patients may have experienced pain due to soft tissue trauma caused by surgical exposure. It has been shown that 10–15% of patients develop chronic pain after simple iliac crest bone harvesting (CitationLaurie et al. 1984, CitationDelawi et al. 2007), which is a similar, but much smaller, procedure to open SIJ fusion. In our study, one patient did not experience any effects from the surgery. This patient had a more generalized pain pattern than the others and it is possible that the SIJ was not the major source of pain in this case, although this patient had a positive response to the SIJ injection. In contrast, the patients who reported sharp and localized pain in the SIJ area did benefit from surgery. It has been reported that the outcomes improved if patients with psychosomatic disorders were excluded, with the success rate increasing from 50% to 70% (CitationWaisbrod et al. 1987). Because SIJ fusion has effects in many patients with PGP, the SIJ or the surrounding ligaments could be the origin of pain in many of these patients, but in patients with more generalized pain patterns, other pain generators might influence the outcome of surgery. The reason for the effect of SIJ fusion is, however, not known. In theory, SIJ fusion can correct many biological disturbances, but it also has a psychological influence on the patient, including placebo effects.
The placebo effect after surgery has been shown to be an important factor in short-term efficacy (CitationTurner et al. 1994) and particularly in the treatment of chronic pain, in which the psychological component is believed to be an important factor. For example, in a study using sham surgery as much as 43% of the patients in the placebo group had pain relief after sham lumbar discectomies (CitationSpangfort 1972), and other similar sham procedures have also reported to have a significant effect on clinical outcome (CitationVandana and Tushar 2001). There are several factors in both the patients and examiners that contribute to the placebo effect. Patients with long-lasting diseases seems to be poorer placebo responders, but on the other hand placebo tend to work better in patients expecting to have changes in sensation of pain (Vandana and Tushar 2001). Our patients was included according to specific criteria and might feel a special need to become pain free, and this can enhance the placebo effect. They also got a relationship with the examiners because we used multiple testing. Hence, some of the positive effect of SIJ fusion seen in paper III can of course be placebo. In our long-term study (paper IV), almost three-quarters of the patients reported to be relieved, or almost relieved, from pain after 1 year, and 28% were not. The 1-year results for the operated patients seemed to be sustained throughout life because patients with successful 1-year results had both significantly less pain and less disability than the patients with unsuccessful 1-year results. With these results, it is difficult to believe that the placebo effect is the only contributor to successful surgical outcomes.
Future of SIJ fusions
It has been questioned whether MIS implants can improve the outcomes of SIJ fusion. Over the last decade, minimally invasive procedures have been introduced, and the use of implants has become popular. Between 2009 and 2013, more than 5000 patients were treated with a specific implant (CitationMiller et al. 2013). In the last few years, several manufacturers have created MIS implants for use in SIJ fusion, but studies have been published for only three of these implants. In 2008 and 2009, two papers were published regarding the use of a traditional, hollow, cylindrical screw across the SIJ (CitationAl-Khayer et al. 2008, CitationKhurana et al. 2009). To achieve fusion, the study authors filled the screw with BMP-2 or demineralized bone matrix. They reported the outcomes of 24 patients with suspected SIJ pain; the fusion rate was 100%, and the clinical outcomes were promising (). Later, Mason et al. (CitationMason et al. 2013) reported the outcomes of 55 patients using the same technique and reported no implant failures, two cases of nerve damage and no other complications. Although the complication rate was lower, the clinical outcomes were not better than those of our study (paper III) in which open anterior surgery was performed ().
Recently, two other MIS techniques have been developed: the iFuse implant (SI-bone Inc., San Jose, CA, USA) and the Distraction Interference Arthrodesis Neurovascular Anticipating (DIANA) implant (Signus Medizintechnik, Alzenau, Germany). Outcomes with the iFuse implant have been reported in 5 studies (), and the complication rate has been reported to be between 0% and 20%. The implant is a triangular, coated implant that is applied across the SIJ, and the SIJ is indirectly fused as the bone grows into the implant. The implant seems promising with regard to clinical outcomes and complication rates, and it has been reported to be cost-effective in the treatment of SIJ pain (CitationAckerman et al. 2013). In a retrospective, multi-center study of 263 patients, the implant showed better clinical outcomes than open surgery (3.5 points lower on a VAS at 12 months in the MIS group), fewer complications and a shorter hospitalization time (CitationSmith et al. 2013). Unfortunately, the authors of these studies have close connections to the corporation that produces these products (SI-bone) as consultants, stockholders or employees of the company, and the company has sponsored some of the studies. Hence, these results should be interpreted with caution and replicated by independent researchers. The DIANA is another type of titanium implant that is inserted dorsally into the recess. Only one original paper with 19 patients has been published, with a fair fusion rate and no infections or no nerve damage. The clinical outcomes, in contrast, were worse than our results (), with a decrease in the ODI from 64 to 57 and a reduction in the VAS from 85 to 60.
In conclusion, the new MIS implants seem safer than open access surgery, with low reported complication rates. The surgical trauma is far less when using MIS, and consequently, the length of the hospital stay is shorter. The clinical outcomes have been reported to be as good, or even better, than the old open technique. However, more studies have to be performed; the studies must be of higher quality; and importantly, the studies must be performed independently of industry. Additionally, future studies should focus on optimal inclusion criteria for SIJ fusion.
Conclusions
This thesis showed the following:
• Radiostereometric analysis applied to the SIJ has high accuracy and precision and is suitable as a tool for investigating SIJ movement. In patients, more than 4 markers in each segment are recommended to ensure obtaining a proper segment to use in the analysis. The use of frontal markers does not improve the precision and is therefore unnecessary.
• In patients with PGP, the movements in the SIJ in the single-leg stance are small and almost undetectable by the precise RSA method. We measured a mean rotation of 0.5° in both the standing- and hanging-leg SIJs, and no translation was detected. There were no differences in total movement between the standing- and hanging-leg SIJs. The interpretation of the results of this study is that the Chamberlain examination is likely inadequate for examining SIJ movement in patients with PGP.
• One year after open unilateral anterior SIJ fusion combined with symphysis pubis fusion, positive and significant changes were observed in both physical function and pain. Despite these positive results, this procedure was associated with adverse events and complications.
• Patients with chronic PGP who underwent SIJ fusion reported being moderately disabled, with moderate or severe pain intensity, 23 years after surgery. Approximately half of these patients had successful 1-year outcomes, and in these patients, their good results were sustained 23 years after surgery. Two-thirds of the patients experienced positive long-term effects from fusion surgery, and 20% reported no effects from the surgery.
Summary
The sacroiliac joint (SIJ) might be the source of pain for 13-30% of patients with low back pain and possibly an even greater proportion of patients suffering from “failed back surgery”. This pain can be caused by specific pathology of the joint, but the specific role of the SIJ in unspecific pelvic girdle pain (PGP) disorder remains unknown. PGP is a common complaint in pregnancy that can cause disability, and in some women, the complaint continues after delivery. The origin and diagnosis of PGP are also unclear because radiological findings are often absent, and the diagnostic criteria lack sufficient evidence. However, it has become increasingly apparent that patients with PGP have different clinical presentations than patients suffering from low back pain. Based on the theory of pathological joint mobility, SIJ fusion combined with symphysis pubis fusion is a therapeutic option when conservative treatment has been unsuccessful.
This thesis includes four papers. In the first two papers, we used a specialized x-ray method, called radiostereometric analysis (RSA), to evaluate the movement of the SIJ, and in the last two papers, we evaluated the outcomes after SIJ fusion.
In paper I, we evaluated the RSA method when this method was applied to the SIJ. We used a phantom model to measure the true values of movements, and these values were compared to the measurements obtained by RSA imaging. By this process, we could determine whether there was any bias that had to be corrected for when this method was used. Furthermore, we measured the precision of the method in the phantom model and in patients. The main results were that the accuracy and precision of the RSA method were high, and the method could be used to measure SIJ movement.
In paper II, we used the RSA method to measure the movement in the SIJ in the single-leg stance. Chamberlain described a method for indirectly measuring SIJ movement by measuring the movement in the pubic symphysis on anterior-posterior (A-P) x-rays. This procedure was performed in the single-leg stance, and Chamberlain attempted to correlate the pubic movement with SIJ pain. However, there have been different reports regarding this relationship, which have made it difficult for clinicians to use the results of the Chamberlain test in the diagnosis of PGP, particularly when normal variations in the movement of the pubic symphysis have also proven to be large. We used RSA to measure the movement in the SIJ in the single-leg stance in 11 patients, and the movements were small and almost undetectable using the method. We measured a mean rotation of 0.5° on both the standing- and hanging-leg SIJs, and no translation was detected. There were no differences in total movement between the standing- and hanging-leg SIJs. From the results of this study, we consider the Chamberlain examination to likely be inadequate for evaluation of SIJ movement in patients with PGP.
In paper III, we used a single-subject design study to evaluate the outcomes of pain, disability and health-related quality of life 1 year after SIJ fusion in 8 patients with severe PGP. These patients were included by applying strict inclusion and exclusion criteria, and they were submitted to surgery with anterior unilateral SIJ fusion combined with a fusion to the pubic symphysis. One year after open unilateral anterior SIJ fusion combined with symphysis pubis fusion, positive and significant changes in both physical function and pain were observed. Despite these positive results, this procedure was associated with adverse events and complications.
In the last paper, paper IV, we performed a long-term follow-up of 50 patients who underwent SIJ fusion performed by Sudmann in Hagavik, Bergen, Norway. All of the patients completed a questionnaire that measured the outcomes of pain, disability and health-related quality of life, and these outcomes were compared with the 1-year outcomes collected by the Sudmann. A comparison group of 28 patients who did not receive SIJ fusion completed the same questionnaire. Patients with chronic PGP who underwent SIJ fusion reported being moderately disabled, with moderate or severe pain intensity 23 years after surgery. Approximately half of these patients had successful 1-year outcomes, and in these patients, good results were sustained 23 years after surgery. Two-thirds of the patients experienced a positive long-term effect from fusion surgery, and 20% reported no effects from the surgery. It appeared that this surgery was an appropriate treatment option for a select group of patients with severe PGP, but which patients would benefit from surgery remains unclear.
References
- Ackerman SJ, Polly DW, Knight T, Schneider K, Holt T, Cummings J. Comparison of the costs of nonoperative care to minimally invasive surgery for sacroiliac joint disruption and degenerative sacroiliitis in a United States Medicare population: potential economic implications of a new minimally-invasive technology. Clinicoecon Outcomes Res 2013; 5:575–587.
- Al-Khayer A, Hegarty J, Hahn D, Grevitt MP. Percutaneous sacroiliac joint arthrodesis: a novel technique. J Spinal Disord Tech 2008; 21 (5):359–363.
- Albert H, Godskesen M, Westergaard J. Evaluation of clinical tests used in classification procedures in pregnancy-related pelvic joint pain. Eur Spine J 2000; 9 (2):161–166.
- Albert H, Godskesen M, Westergaard J. Prognosis in four syndromes of pregnancy-related pelvic pain. Acta Obstet Gynecol Scand 2001; 80 (6):505–510.
- Albert H, Godskesen M, Westergaard J, Chard T, Gunn L. Circulating levels of relaxin are normal in pregnant women with pelvic pain. Eur J Obstet Gynecol Reprod Biol 1997; 74 (1):19–22.
- Albert HB, Godskesen M, Westergaard JG. Incidence of four syndromes of pregnancy-related pelvic joint pain. Spine (Phila Pa 1976 ) 2002; 27 (24):2831–2834.
- Alderink GJ. The sacroiliac joint: review of anatomy, mechanics, and function. The Journal of orthopaedic and sports physical therapy 1990; 13 (2):71–84.
- Anderson PL, Peterson VL. Clinical use of the Chamberlain technic in sacroiliac conditions. Journal of the American Medical Association 1944; 124 (5):269–271.
- Avilia JR. Primary pyogenic infection of the sacro-iliac articulation. A new approach to the joint. Report of Seven Cases. The Journal of Bone & Joint Surgery Case Connector 1941; 23 (4):922–928.
- Beales DJ, O’Sullivan PB, Briffa NK. Motor control patterns during an active straight leg raise in chronic pelvic girdle pain subjects. Spine (Phila Pa 1976 ) 2009; 34 (9):861–870.
- Belanger TA, Dall BE. Sacroiliac arthrodesis using a posterior midline fascial splitting approach and pedicle screw instrumentation: a new technique. J Spinal Disord 2001; 14 (2):118–124.
- Bellamy N, Park W, Rooney PJ. What do we know about the sacroiliac joint?. Semin Arthritis Rheum 1983; 12 (3):282–313.
- Berg G, Hammar M, Moller-Nielsen J, Linden U, Thorblad J. Low back pain during pregnancy. Obstet Gynecol 1988; 71 (1):71–75.
- Bjelland EK, Kristiansson P, Nordeng H, Vangen S, Eberhard-Gran M. Hormonal contraception and pelvic girdle pain during pregnancy: a population study of 91,721 pregnancies in the Norwegian Mother and Child Cohort. Hum Reprod 2013a; 28 (11):3134–3140.
- Bjelland EK, Stuge B, Engdahl B, Eberhard-Gran M. The effect of emotional distress on persistent pelvic girdle pain after delivery: a longitudinal population study. BJOG 2013b; 120 (1):32–40.
- Bo K, Lilleas F, Talseth T, Hedland H. Dynamic MRI of the pelvic floor muscles in an upright sitting position. Neurourol Urodyn 2001; 20 (2):167–174.
- Bragdon CR, Malchau H, Yuan X, Perinchief R, Karrholm J, Borlin N, Estok DM, Harris WH. Experimental assessment of precision and accuracy of radiostereometric analysis for the determination of polyethylene wear in a total hip replacement model. J Orthop Res 2002; 20 (4):688–695.
- Brunner C, Kissling R, Jacob HA. The effects of morphology and histopathologic findings on the mobility of the sacroiliac joint. Spine (Phila Pa 1976) 1991; 16 (9):1111–1117.
- Buchowski JM, Kebaish KM, Sinkov V, Cohen DB, Sieber AN, Kostuik JP. Functional and radiographic outcome of sacroiliac arthrodesis for the disorders of the sacroiliac joint. Spine J 2005; 5 (5):520–528.
- Bussey MD, Milosavljevic S, Bell ML. Sex differences in the pattern of innominate motion during passive hip abduction and external rotation. Man Ther 2009; 14 (5):514–519.
- Chamberlain WE, Milosavljevic S, Bell ML. The symphysis pubis in the roentgen examination of the sacroiliac joint. Am J Roentgenol Radium Ther Nucl Med 1930; 24: 621–625.
- Cibulka MT. Re: a radiostereometric analysis of the movements of the sacroiliac joints in the reciprocal straddle position. Spine (Phila Pa 1976 ) 2001; 26 (12):1404–1405.
- Cohen SP. Sacroiliac joint pain: a comprehensive review of anatomy, diagnosis, and treatment. Anesth Analg 2005; 101 (5):1440–1453.
- Cummings J, Capobianco RA. Minimally invasive sacroiliac joint fusion: one-year outcomes in 18 patients. Ann Surg Innov Res 2013; 7 (1):12.
- Damen L, Buyruk HM, Guler-Uysal F, Lotgering FK, Snijders CJ, Stam HJ. Pelvic pain during pregnancy is associated with asymmetric laxity of the sacroiliac joints. Acta Obstet Gynecol Scand 2001; 80 (11):1019–1024.
- Damen L, Buyruk HM, Guler-Uysal F, Lotgering FK, Snijders CJ, Stam HJ. The prognostic value of asymmetric laxity of the sacroiliac joints in pregnancy-related pelvic pain. Spine (Phila Pa 1976) 2002a; 27 (24):2820–2824.
- Damen L, Spoor CW, Snijders CJ, Stam HJ. Does a pelvic belt influence sacroiliac joint laxity?. Clin Biomech (Bristol , Avon ) 2002b; 17 (7):495–498.
- Damen L, Stijnen T, Roebroeck ME, Snijders CJ, Stam HJ. Reliability of sacroiliac joint laxity measurement with Doppler imaging of vibrations. Ultrasound Med Biol 2002c; 28 (4):407–414.
- Delawi D, Dhert WJ, Castelein RM, Verbout AJ, Oner FC. The incidence of donor site pain after bone graft harvesting from the posterior iliac crest may be overestimated: a study on spine fracture patients. Spine (Phila Pa 1976 ) 2007; 32 (17):1865–1868.
- DePalma MJ, Ketchum JM, Saullo TR. Etiology of chronic low back pain in patients having undergone lumbar fusion. Pain Med 2011; 12 (5):732–739.
- Dreyfuss P, Michaelsen M, Pauza K, McLarty J, Bogduk N. The value of medical history and physical examination in diagnosing sacroiliac joint pain. Spine (Phila Pa 1976 ) 1996; 12 (22):2594–2602.
- Duhon BS, Cher DJ, Wine KD, Lockstadt H, Kovalsky D, Soo CL. Safety and 6-month effectiveness of minimally invasive sacroiliac joint fusion: a prospective study. Med Devices (Auckl) 2013; 6: 219–229.
- Egund N, Olsson TH, Schmid H, Selvik G. Movements in the sacroiliac joints demonstrated with roentgen stereophotogrammetry. Acta Radiol Diagn (Stockh) 1978; 19 (5):833–846.
- Elgafy H, Semaan HB, Ebraheim NA, Coombs RJ. Computed tomography findings in patients with sacroiliac pain. Clin Orthop Relat Res 2001; (382):112–118.
- Endres S, Ludwig E. Outcome of distraction interference arthrodesis of the sacroiliac joint for sacroiliac arthritis. Indian J Orthop 2013; 47 (5):437–442.
- Engel RJ, Schutt RK. Single-Subject Design. In: The Practice of Research in Social Work. (Ed. Westby J). SAGE Publications, California, 2009; Second: 206–247.
- Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976) 2000; 25 (22):2940–2952.
- Foley BS, Buschbacher RM. Sacroiliac joint pain: anatomy, biomechanics, diagnosis, and treatment. Am J Phys Med Rehabil 2006; 85 (12):997–1006.
- Forst SL, Wheeler MT, Fortin JD, Vilensky JA. The sacroiliac joint: anatomy, physiology and clinical significance. Pain Physician 2006; 9 (1):61–67.
- Fortin JD, Dwyer AP, West S, Pier J. Sacroiliac joint: pain referral maps upon applying a new injection/arthrography technique. Part I: Asymptomatic volunteers. Spine (Phila Pa 1976 ) 1994; 19 (13):1475–1482.
- Gaenslen FJ. Sacro-iliac arthrodesis indications, authors technic and end-results. Journal of the American Medical Association 1927; 89 (24):2031–2035.
- Garras DN, Carothers JT, Olson SA. Single-leg-stance (flamingo) radiographs to assess pelvic instability: how much motion is normal?. J Bone Joint Surg Am 2008; 90 (10):2114–2118.
- Giannikas KA, Khan AM, Karski MT, Maxwell HA. Sacroiliac joint fusion for chronic pain: a simple technique avoiding the use of metalwork. Eur Spine J 2004; 13 (3):253–256.
- Gonnella C. Single-subject experimental paradigm as a clinical decision tool. Phys Ther 1989; 69 (7):601–609.
- Goode A, Hegedus EJ, Sizer P, Brismee JM, Linberg A, Cook CE. Three-dimensional movements of the sacroiliac joint: a systematic review of the literature and assessment of clinical utility. J Man Manip Ther 2008; 16 (1):25–38.
- Grotle M, Brox JI, Vollestad NK. Cross-cultural adaptation of the Norwegian versions of the Roland-Morris Disability Questionnaire and the Oswestry Disability Index. J Rehabil Med 2003; 35 (5):241–247.
- Grotle M, Brox JI, Vollestad NK. Concurrent comparison of responsiveness in pain and functional status measurements used for patients with low back pain. Spine (Phila Pa 1976) 2004; 29 (21):E492–E501.
- Güner G, Gurer S, Elmali N, Ertem K. Anterior sacroiliac fusion: a new video-assisted endoscopic technique. Surg Laparosc Endosc 1998; 8 (3):233–236.
- Ha KY, Lee JS, Kim KW. Degeneration of sacroiliac joint after instrumented lumbar or lumbosacral fusion: a prospective cohort study over five-year follow-up. Spine (Phila Pa 1976 ) 2008; 33 (11):1192–1198.
- Hagen R. Pelvic girdle relaxation from an orthopaedic point of view. Acta Orthop Scand 1974; 45 (4):550–563.
- Hagg O, Fritzell P, Nordwall A. The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J 2003; 12 (1):12–20.
- Hungerford B, Gilleard W, Lee D. Altered patterns of pelvic bone motion determined in subjects with posterior pelvic pain using skin markers. Clin Biomech (Bristol , Avon ) 2004; 19 (5):456–464.
- Hungerford BA, Gilleard W, Moran M, Emmerson C. Evaluation of the ability of physical therapists to palpate intrapelvic motion with the Stork test on the support side. Phys Ther 2007; 87 (7):879–887.
- Ivanov AA, Kiapour A, Ebraheim NA, Goel V. Lumbar fusion leads to increases in angular motion and stress across sacroiliac joint: a finite element study. Spine (Phila Pa 1976 ) 2009; 34 (5):E162–E169.
- Jacob HA, Kissling RO. The mobility of the sacroiliac joints in healthy volunteers between 20 and 50 years of age. Clin Biomech (Bristol , Avon ) 1995; 10 (7):352–361.
- Juhl M, Andersen PK, Olsen J, Andersen AM. Psychosocial and physical work environment, and risk of pelvic pain in pregnancy. A study within the Danish national birth cohort. J Epidemiol Community Health 2005; 59 (7):580–585.
- Kanakaris NK, Roberts CS, Giannoudis PV. Pregnancy-related pelvic girdle pain: an update. BMC Med 2011; 9: 15.
- Katz V, Schofferman J, Reynolds J. The sacroiliac joint: a potential cause of pain after lumbar fusion to the sacrum. J Spinal Disord Tech 2003; 16 (1):96–99.
- Keating JG, Avillar MD, Price J. Sacroiliac joint arthrodesis in selected patients with low back pain. Movement, stability & low back pain Churchill Livingstone, London 1997; 573–586.
- Khurana A, Guha AR, Mohanty KAhuja S, Ahuja S. Percutaneous fusion of the sacroiliac joint with hollow modular anchorage screws: clinical and radiological outcome. J Bone Joint Surg Br 2009; 91 (5):627–631.
- Kristiansson P, Svardsudd K. Discriminatory power of tests applied in back pain during pregnancy. Spine (Phila Pa 1976) 1996; 21 (20):2337–2343.
- Laplante BL, Ketchum JM, Saullo TR, DePalma MJ. Multivariable analysis of the relationship between pain referral patterns and the source of chronic low back pain. Pain Physician 2012; 15 (2):171–178.
- Larsen EC, Wilken-Jensen C, Hansen A, Jensen DV, Johansen S, Minck H, Wormslev M, Davidsen M, Hansen TM. Symptom-giving pelvic girdle relaxation in pregnancy. I: Prevalence and risk factors. Acta Obstet Gynecol Scand 1999; 78 (2):105–110.
- Laslett M, Aprill CN, McDonald B. Provocation sacroiliac joint tests have validity in the diagnosis of sacroiliac joint pain. Arch Phys Med Rehabil 2006; 87 (6):874–875.
- Laslett M, Aprill CN, McDonald B, Young SB. Diagnosis of sacroiliac joint pain: validity of individual provocation tests and composites of tests. Man Ther 2005a; 10 (3):207–218.
- Laslett M, McDonald B, Tropp H, Aprill CN, Oberg B. Agreement between diagnoses reached by clinical examination and available reference standards: a prospective study of 216 patients with lumbopelvic pain. BMC Musculoskelet Disord 2005a; 6 :28.
- Laslett M, Young SB, Aprill CN, McDonald B. Diagnosing painful sacroiliac joints: A validity study of a McKenzie evaluation and sacroiliac provocation tests. Aust J Physiother 2003; 49 (2):89–97.
- Laurie SW, Kaban LB, Mulliken JB, Murray JE. Donor-site morbidity after harvesting rib and iliac bone. Plast Reconstr Surg 1984; 73 (6):933–938.
- Lavignolle B, Vital JM, Senegas J, Destandau J, Toson B, Bouyx P, Morlier P, Delorme G, Calabet A. An approach to the functional anatomy of the sacroiliac joints in vivo. Anat Clin 1983; 5 (3):169–176.
- Lippitt AB. Percutaneous fixation of the sacroiliac joint. The Integrated Function of the Lumbar Spine and Sacroiliac Joint San Diego, CA 1995; 369–392.
- Logan LR, Hickman RR, Harris SR, Heriza CB. Single-subject research design: recommendations for levels of evidence and quality rating. Developmental medicine & child neurology 2008; 50 (2):99–103.
- Loge JH, Kaasa S, Hjermstad MJ, Kvien TK. Translation and performance of the Norwegian SF-36 Health Survey in patients with rheumatoid arthritis. I. Data quality, scaling assumptions, reliability, and construct validity. J Clin Epidemiol 1998; 51 (11):1069–1076.
- Lynch FW. The pelvic articulations during pregnancy, labor, and the puerperium: An X-ray study. Surg Gynecol Obstet 1920; 30 :575–580.
- Maigne JY, Aivaliklis A, Pfefer F. Results of sacroiliac joint double block and value of sacroiliac pain provocation tests in 54 patients with low back pain. Spine (Phila Pa 1976 ) 1996; 21 (16):1889–1892.
- Maigne JY, Boulahdour H, Chatellier G. Value of quantitative radionuclide bone scanning in the diagnosis of sacroiliac joint syndrome in 32 patients with low back pain. Eur Spine J 1998; 7 (4):328–331.
- Maigne JY, Planchon CA. Sacroiliac joint pain after lumbar fusion. A study with anesthetic blocks. Eur Spine J 2005; 14 (7):654–658.
- Makinen TJ, Koort JK, Mattila KT, Aro HT. Precision measurements of the RSA method using a phantom model of hip prosthesis. J Biomech 2004; 37 (4):487–493.
- Mason LW, Chopra I, Mohanty K. The percutaneous stabilisation of the sacroiliac joint with hollow modular anchorage screws: a prospective outcome study. Eur Spine J 2013; 22 (10):2325–2331.
- Mens JM, Pool-Goudzwaard A, Stam HJ. Mobility of the pelvic joints in pregnancy-related lumbopelvic pain: a systematic review. Obstet Gynecol Surv 2009; 64 (3):200–208.
- Mens JM, Vleeming A, Snijders R, Koes BW, Stam HJ. Validity of the active straight leg raise test for measuring disease severity in patients with posterior pelvic pain after pregnancy. Spine (Phila Pa 1976 ) 2002; 27 (2):196–200.
- Mens JM, Vleeming A, Snijders R, Stam HJ, Ginai AZ. The active straight leg raising test and mobility of the pelvic joints. Eur Spine J 1999; 8 (6):468–473.
- Mens JM, Vleeming A, Stoeckart R, Stam HJ, Snijders CJ. Understanding peripartum pelvic pain. Implications of a patient survey. Spine (Phila Pa 1976) 1996; 21 (11):1363–1369.
- Miller LE, Reckling WC, Block JE. Analysis of postmarket complaints database for the iFuse SI Joint Fusion System(R): a minimally invasive treatment for degenerative sacroiliitis and sacroiliac joint disruption. Med Devices (Auckl ) 2013; 6: 77–84.
- Miltner LJ, Lowendorf CS. Low Back Pain: A Study of 525 Cases of Sacro-Iliac and Sacrolumbar Sprain. The Journal of Bone & Joint Surgery 1931; 13 (1):16–28.
- Mitchell JI. Surgical treatment of affections of the lumbo-sacral and sacroiliac joints. Surgery 1938; 4: 33–43.
- Mixter WJ, Barr JS. Rupture of the intervertebral disc with involvement of the spinal canal. N Engl J Med 1934; 211 (5):210–215.
- O‘Sullivan PB, Beales DJ. Diagnosis and classification of pelvic girdle pain disorders--Part 1: a mechanism based approach within a biopsychosocial framework. Man Ther 2007; 12 (2):86–97.
- Ohlund C, Eek C, Palmbald S, Areskoug B, Nachemson A. Quantified pain drawing in subacute low back pain. Validation in a nonselected outpatient industrial sample. Spine (Phila Pa 1976) 1996; 21 (9):1021–1030.
- Olerud S, Walheim GG. Symphysiodesis with a new compression plate. Acta Orthop Scand 1984; 55 (3):315–318.
- Olsson CB, Grooten WJ, Nilsson-Wikmar L, Harms-Ringdahl K, Lundberg M. Catastrophizing during and after pregnancy: associations with lumbopelvic pain and postpartum physical ability. Phys Ther 2012; 92 (1):49–57.
- Ostgaard HC, Andersson GB, Karlsson K. Prevalence of back pain in pregnancy. Spine (Phila Pa 1976) 1991; 16 (5):549–552.
- Palsson TS, Graven-Nielsen T. Experimental pelvic pain facilitates pain provocation tests and causes regional hyperalgesia. Pain 2012; 153 (11):2233–2240.
- Pool-Goudzwaard A, van Dijke GH, van GM, Mulder P, Snijders C, Stoeckart R. Contribution of pelvic floor muscles to stiffness of the pelvic ring. Clin Biomech (Bristol , Avon ) 2004; 19 (6):564–571.
- Puhakka KB, Jurik AG, Schiottz-Christensen B, Hansen GV, Egund N, Christiansen JV, Stengaard-Pedersen K. Magnetic resonance imaging of sacroiliitis in early seronegative spondylarthropathy. Abnormalities correlated to clinical and laboratory findings. Rheumatology (Oxford) 2004a; 43 (2):234–237.
- Puhakka KB, Jurik AG, Schiottz-Christensen B, Hansen GV, Egund N, Christiansen JV, Stengaard-Pedersen K. MRI abnormalities of sacroiliac joints in early spondylarthropathy: a 1-year follow-up study. Scand J Rheumatol 2004b; 33 (5):332–338.
- Rand JA. Anterior sacro-iliac arthrodesis for post-traumatic sacro-iliac arthritis. A case report. J Bone Joint Surg Am 1985; 67 (1):157–159.
- Ranstam J, Ryd L, Onsten I. Accurate accuracy assessment: review of basic principles. Acta Orthop Scand 2000; 71 (1):106–108.
- Revill SI, Robinson JO, Rosen M, Hogg MI. The reliability of a linear analogue for evaluating pain. Anaesthesia 1976; 31 (9):1191–1198.
- Robinson HS, Eskild A, Heiberg E, Eberhard-Gran M. Pelvic girdle pain in pregnancy: the impact on function. Acta Obstet Gynecol Scand 2006; 85 (2):160–164.
- Robinson HS, Veierod MB, Mengshoel AM, Vollestad NK. Pelvic girdle pain--associations between risk factors in early pregnancy and disability or pain intensity in late pregnancy: a prospective cohort study. BMC Musculoskelet Disord 2010; 11: 91.
- Rudolf L. Sacroiliac Joint Arthrodesis-MIS Technique with Titanium Implants: Report of the First 50 Patients and Outcomes. Open Orthop J 2012; 6: 495–502.
- Rudolf L. MIS fusion of the SI joint: does prior lumbar spinal fusion affect patient outcomes?. Open Orthop J 2013; 7: 163–168.
- Ryd L, Yuan X, Lofgren H. Methods for determining the accuracy of radiostereometric analysis (RSA). Acta Orthop Scand 2000; 71 (4):403–408.
- Sachs D, Capobianco R. One year successful outcomes for novel sacroiliac joint arthrodesis system. Ann Surg Innov Res 2012; 6 (1):13.
- Sachs D, Capobianco R. Minimally invasive sacroiliac joint fusion: one-year outcomes in 40 patients. Adv Orthop 2013; 2013: 536128.
- Schutz U, Grob D. Poor outcome following bilateral sacroiliac joint fusion for degenerative sacroiliac joint syndrome. Acta Orthop Belg 2006; 72 (3):296–308.
- Schwarzer AC, Aprill CN, Bogduk N. The sacroiliac joint in chronic low back pain. Spine (Phila Pa 1976) 1995; 20 (1):31–37.
- Shibata Y, Shirai Y, Miyamoto M. The aging process in the sacroiliac joint: helical computed tomography analysis. J Orthop Sci 2002; 7 (1):12–18.
- Siegel J, Templeman DC, Tornetta P, III. Single-leg-stance radiographs in the diagnosis of pelvic instability. J Bone Joint Surg Am 2008; 90 (10):2119–2125.
- Simopoulos TT, Manchikanti L, Singh V, Gupta S, Hameed H, Diwan S, Cohen SP. A systematic evaluation of prevalence and diagnostic accuracy of sacroiliac joint interventions. Pain Physician 2012; 15 (3):E305–E344.
- Slatis P, Eskola A. External fixation of the pelvic girdle as a test for assessing instability of the sacro-iliac joint. Ann Med 1989; 21 (5):369–372.
- Slipman CW, Jackson HB, Lipetz JS, Chan KT, Lenrow D, Vresilovic EJ. Sacroiliac joint pain referral zones. Arch Phys Med Rehabil 2000; 81 (3):334–338.
- Slipman CW, Sterenfeld EB, Chou LH, Herzog R, Vresilovic E. TThe value of radionuclide imaging in the diagnosis of sacroiliac joint syndrome. Spine (Phila Pa 1976) 1996; 21 (19):2251–2254.
- Slipman CW, Sterenfeld EB, Chou LH, Herzog R, Vresilovic E. The predictive value of provocative sacroiliac joint stress maneuvers in the diagnosis of sacroiliac joint syndrome. Arch Phys Med Rehabil 1998; 79 (3):288–292.
- Smidt GL, McQuade K, Wei SH, Barakatt E. Sacroiliac kinematics for reciprocal straddle positions. Spine (Phila Pa 1976) 1995; 20 (9):1047–1054.
- Smidt GL, Wei SH, McQuade K, Barakatt E, Sun T, Stanford W. Sacroiliac motion for extreme hip positions. A fresh cadaver study. Spine (Phila Pa 1976) 1997; 22 (18):2073–2082.
- Smith AG, Capobianco R, Cher D, Rudolf L, Sachs D, Gundanna M, Kleiner J, Mody MG, Shamie AN. Open versus minimally invasive sacroiliac joint fusion: a multi-center comparison of perioperative measures and clinical outcomes. Ann Surg Innov Res 2013; 7 (1):14.
- Smith-Petersen MN, Rogers WA. End-result study of arthrodesis of the aacro-iliac joint for arthritis – traumatic and non-traumatic. The Journal of Bone & Joint Surgery 1926; 8 (1):118–136.
- Smith-Peterson MN. Arthrodesis of the sacroiliac joint. A new method of approch. The Journal of Bone & Joint Surgery 1921; 3: 400–405.
- Snijders CJ, Vleeming A, Stoeckart R. Transfer of lumbosacral load to iliac bones and legs: Part 1: Biomechanics of self-bracing of the sacroiliac joints and its significance for treatment and exercise. Clinical Biomechanics 1993; 8 (6):285–294.
- Solonen KA. The sacroiliac joint in the light of anathomical, roentgenological and clinical studies. Acta Orthop Scand 1957; Suppl 27: 1–127.
- Spangfort EV. The lumbar disc herniation. A computer-aided analysis of 2,504 operations. Acta Orthop Scand 1972; Suppl 142: 1–95.
- Stanford G, Burnham RS. Is it useful to repeat sacroiliac joint provocative tests post-block?. Pain Med 2010; 11 (12):1774–1776.
- Stark JG, Fuentes JA, Fuentes TI, Idemmili C. The history of sacroiliac joint arthrodesis: a critical review and introduction of a new technique. Current Orthopaedic Practice 2011; 22 (6):545–557.
- Stuge B, Garratt A, Krogstad JH, Grotle M. The pelvic girdle questionnaire: a condition-specific instrument for assessing activity limitations and symptoms in people with pelvic girdle pain. Phys Ther 2011; 91 (7):1096–1108.
- Stuge B, Laerum E, Kirkesola G, Vollestad N. The efficacy of a treatment program focusing on specific stabilizing exercises for pelvic girdle pain after pregnancy: a randomized controlled trial. Spine (Phila Pa 1976) 2004a; 29 (4):351–359.
- Stuge B, Saetre K, Braekken IH. The association between pelvic floor muscle function and pelvic girdle pain--a matched case control 3D ultrasound study. Man Ther 2012; 17 (2):150–156.
- Stuge B, Saetre K, Ingeborg HB. The automatic pelvic floor muscle response to the active straight leg raise in cases with pelvic girdle pain and matched controls. Man Ther 2013; 18 (4):327–32.
- Stuge B, Veierod MB, Laerum E, Vollestad N. The efficacy of a treatment program focusing on specific stabilizing exercises for pelvic girdle pain after pregnancy: a two-year follow-up of a randomized clinical trial. Spine (Phila Pa 1976 ) 2004b; 29 (10):E197–E203.
- Sturesson B. Load and movement of the sacroiliac joint. 1999. Department of Orthopaedics, Lund University, Malmö. Thesis/Dissertation.
- Sturesson B, Selvik G, Uden A. Movements of the sacroiliac joints. A roentgen stereophotogrammetric analysis. Spine (Phila Pa 1976) 1989; 14 (2):162–165.
- Sturesson B, Uden G, Onsten I. Can an external frame fixation reduce the movements in the sacroiliac joint? A radiostereometric analysis of 10 patients. Acta Orthop Scand 1999; 70 (1):42–46.
- Sturesson B, Uden G, Vleeming A. A radiostereometric analysis of movements of the sacroiliac joints during the standing hip flexion test. Spine 2000a; 25 (3):364–368.
- Sturesson B, Uden G, Vleeming A. A radiostereometric analysis of the movements of the sacroiliac joints in the reciprocal straddle position. Spine 2000b; 25 (2):214–217.
- Sturesson B, Uden G, Uden A. Pain pattern in pregnancy and “catching” of the leg in pregnant women with posterior pelvic pain. Spine (Phila Pa 1976) 1997; 22 (16):1880–1883.
- Szadek KM, Hoogland PV, Zuurmond WW, De Lange JJ, Perez RS. Nociceptive nerve fibers in the sacroiliac joint in humans. Reg Anesth Pain Med 2008; 33 (1):36–43.
- Szadek KM, Hoogland PV, Zuurmond WW, De Lange JJ, Perez RS. Possible nociceptive structures in the sacroiliac joint cartilage: An immunohistochemical study. Clin Anat 2010; 23 (2):192–198.
- Torstensson T, Lindgren A, Kristiansson P. Corticosteroid injection treatment to the ischiadic spine reduced pain in women with long-lasting sacral low back pain with onset during pregnancy: a randomized, double blind, controlled trial. Spine (Phila Pa 1976) 2009; 34 (21):2254–2258.
- Tullberg T, Blomberg S, Branth B, Johnsson R. Manipulation does not alter the position of the sacroiliac joint. A roentgen stereophotogrammetric analysis. Spine (Phila Pa 1976) 1998; 23 (10):1124–1128.
- Turner JA, Deyo RA, Loeser JD, Von KM, Fordyce WE. The importance of placebo effects in pain treatment and research. JAMA 1994; 271 (20):1609–1614.
- Valstar ER, Gill R, Ryd L, Flivik G, Borlin N, Karrholm J. Guidelines for standardization of radiostereometry (RSA) of implants. Acta Orthop 2005; 76 (4):563–572.
- van der Worp HB, Howells DW, Sena ES, Porritt MJ, Rewell S, O’Collins V, Macleod MR. Can animal models of disease reliably inform human studies?. PLoS Med 2010; 7 (3):e1000245.
- van der Wurff P. Clinical diagnostic tests for the sacroiliac joint: motion and palpation tests. Aust J Physiother 2006; 52 (4):308.
- van der Wurff P, Buijs EJ, Groen GJ. A multitest regimen of pain provocation tests as an aid to reduce unnecessary minimally invasive sacroiliac joint procedures. Arch Phys Med Rehabil 2006; 87 (1):10–14.
- van der Wurff P, Hagmeijer RH, Meyne W. Clinical tests of the sacroiliac joint. A systematic methodological review. Part 1: Reliability. Man Ther 2000a; 5 (1):30–36.
- van den Bosch P, Meyne W, Hagmeijer RH. Clinical tests of the sacroiliac joint. Man Ther 2000b; 5 (2):89–96.
- van Zwienen CMA, van den Bosch EW, Snijders CJ, van Vugt AB. Triple Pelvic Ring Fixation in Patients With Severe Pregnancy-Related Low Back and Pain. Spine 2004; 29 (4):478–484.
- Vandana R, Tushar R. Placebos: current status. Indian J pharmacology 2001; 33 (6):396–409.
- Vleeming A, Albert HB, Ostgaard HC, Sturesson B, Stuge B. European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur Spine J 2008; 17 (6):794–819.
- Vleeming A, Pool-Goudzwaard AL, Stoeckart R, van Wingerden JP, Snijders CJ. The posterior layer of the thoracolumbar fascia. Its function in load transfer from spine to legs. Spine (Phila Pa 1976) 1995; 20 (7):753–758.
- Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat 2012; 221 (6):537–567.
- Vleeming A, Schuenke MD, Sturesson B, Willard FH. Authors’ response to the letter to the editors by Professor M. T. Cibulka: a critical interpretation of sacroiliac joint movement studies. J Anat 2013; 222 (3):391–395.
- Vleeming A, van Wingerden JP, Dijkstra PF, Stoeckart R, Snijders CJ, Stijnen T. Mobility in the sacroiliac joints in the elderly: a kinematic and radiological study. Clin Biomech (Bristol , Avon ) 1992a; 7 (3):170–176.
- Vleeming A, Van Wingerden JP, Dijkstra PF, Stoeckart R, Snijders CJ, Stijnen T. Mobility in the sacroiliac joints in the elderly: a kinematic and radiological study. Clin Biomech (Bristol , Avon ) 1992b; 7 (3):170–176.
- Vleeming A, Volkers AC, Snijders CJ, Stoeckart R. Relation between form and function in the sacroiliac joint. Spine 1990; 15 (2):133–136.
- Vogler JB, III, Brown WH, Helms CA, Genant HK. The normal sacroiliac joint: a CT study of asymptomatic patients. Radiology 1984; 151 (2):433–437.
- Vollestad NK, Torjesen PA, Robinson HS. Association between the serum levels of relaxin and responses to the active straight leg raise test in pregnancy. Man Ther 2012; 17 (3):225–230.
- Von Schubert E. Rontgenuntersuchungen des knochernen Beckens im Profilbild: exakte messung der Bekkenneigung bei lebenden. Zentralbl Gynakol 1929; 53: 1064–1068.
- Von KM, Jensen MP, Karoly P. Assessing global pain severity by self-report in clinical and health services research. Spine (Phila Pa 1976 ) 2000; 25 (24):3140–3151.
- Waisbrod H, Krainick JU, Gerbershagen HU. Sacroiliac joint arthrodesis for chronic lower back pain. Arch Orthop Trauma Surg 1987; 106 (4):238–240.
- Walker JM. The sacroiliac joint: a critical review. Phys Ther 1992; 72 (12):903–916.
- Weisl H. The movements of the sacroiliac joint. Acta Anat (Basel) 1955; 23 (1):80–91.
- Wise CL, Dall BE. Minimally invasive sacroiliac arthrodesis: outcomes of a new technique. J Spinal Disord Tech 2008; 21 (8):579–584.
- Wright A. Hypoalgesia post-manipulative therapy: a review of a potential neurophysiological mechanism. Man Ther 1995; 1 (1):11–16.
- Wu WH, Meijer OG, Bruijn SM, Hu H, van Dieen JH, Lamoth CJ, van Royen BJ, Beek PJ. Gait in Pregnancy-related Pelvic girdle Pain: amplitudes, timing, and coordination of horizontal trunk rotations. Eur Spine J 2008; 17 (9):1160–1169.
- Wu WH, Meijer OG, Uegaki K, Mens JM, van Dieen JH, Wuisman PI, Ostgaard HC. Pregnancy-related pelvic girdle pain (PPP), I: Terminology, clinical presentation, and prevalence. Eur Spine J 2004; 13 (7):575–589.
- Zhan S, Ottenbacher KJ. Single subject research designs for disability research. Disabil Rehabil 2001; 23 (1):1–8.
- Ziran BH, Heckman D, Smith WR. CT-guided stabilization for chronic sacroiliac pain: a preliminary report. J Trauma 2007; 63 (1):90–96.