Abstract
Background and purpose — The discrepancy between symptoms and radiographic severity of knee osteoarthritis (OA) is well described. However, little is known about whether radiographic severity is predictive of the clinical result of nonoperative treatment. We investigated whether radiographic severity and treatment type were associated with improvements in pain after nonoperative treatment of patients with knee OA.
Patients and methods — A 5-year consecutive series of patients deemed not eligible for total knee arthroplasty (TKA) by an experienced orthopedic surgeon was contacted 1–5 years later. Radiographic severity, age, sex, and BMI were registered at the consultation. At follow-up, patients were asked to answer a questionnaire on type of treatment and improvements in pain after treatment.
Results — Of 1,848 patients who were not eligible for TKA, 1,414 (77%) completed the follow-up questionnaire (mean age 66 (24–96) years; 55% women). Radiographic severity was not associated with improvements in pain even after adjusting for treatment type, age, sex, and BMI (p > 0.1). The odds ratio of improvement was higher by a factor of 2 in patients who received physiotherapy or multimodal treatment than in patients who did not.
Interpretation — Radiographic severity was not associated with improvements in pain after nonoperative treatment. Patients who are not eligible for TKA can confidently be referred to nonoperative treatment even if they have severe radiographic OA. The treatment should preferably be multimodal, including physiotherapy, as recommended in Danish and international clinical guidelines.
Knee osteoarthritis (OA) is a major cause of chronic musculoskeletal pain (Peat et al. 2001) and a leading cause of functional disability in the elderly (CitationGuccione et al. 1994). Due to demographic changes, the burden of symptomatic OA is expected to increase rapidly in the future (CitationHootman and Helmick 2006), which highlights the need for early-stage nonoperative treatment strategies, with the potential to reverse or prevent further progression of the disease (CitationHunter 2011).
While pain and functional disability are the hallmark symptoms of knee OA, radiographic characteristics are often used to characterize the severity of the disease. Since several tissue structures are potential sources of pain (CitationDieppe 2005, CitationSkou et al. 2013), a key question is the extent to which the radiographic severity can predict the clinical result of nonoperative treatment. In other words, which treatment should be recommended for a specific level of radiographic severity, and is nonoperative treatment equally effective for different levels of radiographic severity?
In spite of the fact that the discrepancy between symptoms and radiographic severity is well described (CitationBedson and Croft 2008), only 2 previous studies have addressed this issue in patients with knee OA (CitationWang et al. 2004, CitationJuhl et al. 2014). One meta-regression analysis found similar effects of exercise on symptoms at all levels of radiographic severity (CitationJuhl et al. 2014). Another study found that patients with the most advanced radiographic severity were less likely to report a reduction in symptoms after intraarticular injection of hyaluronic acid (CitationWang et al. 2004). Whether these conflicting results are due to the different nature and effects of the 2 treatments on knee OA symptoms or to other factors is unknown. This calls for further analysis of the mediating effects of radiographic severity on the effects of nonoperative treatment. Such knowledge would help guide clinicians in their decision on referral to nonoperative treatment in both primary and secondary care.
The main purpose of this study was to investigate whether radiographic severity is associated with improvements in pain after nonoperative treatments in patients with knee OA who are not eligible for a total knee arthroplasty (TKA). The secondary purpose was to investigate whether various nonoperative treatments may be associated with improvements in pain. We hypothesized that radiographic severity of OA is inversely associated with self-reported improvements, and that all forms of treatment would result in larger improvement in pain than no treatment.
Patients and methods
Study design
This was a retrospective cohort study conforming to the STROBE statement for reporting of observational studies (von CitationElm et al. 2007).
Participants
2,262 consecutive patients with knee OA who were deemed not eligible for a TKA by an experienced orthopedic surgeon in the Northern Health Care Region, Denmark, between June 21, 2005 and February 2, 2012 were identified through the National Patient Registry. All the patients were then contacted by regular post 1–5 years after their initial consultation and asked to complete a follow-up questionnaire concerning their knee pain.
Patients with a previous ipsilateral knee arthroplasty, patients who underwent a surgical procedure of their knee (TKA or other surgery) during the follow-up period, and patients who had died or were unable to answer due to illness were excluded from the study. We decided not to include those who had undergone surgery as nonoperative treatment failures, since undergoing surgery does not necessarily mean that the original nonoperative treatment was unsuccessful and since the questionnaire was designed to evaluate nonoperative treatment only. So there was a risk of introducing uncertainties in the analysis if we included those who underwent surgery.
Follow-up questionnaire
The questionnaire contained questions on treatment type, improvements in pain, and the patient’s opinion concerning their knee and associated problems.
Primary outcome: improvements in pain
Changes in knee pain after the treatment were assessed using a 4-point scale (“Pain-free”, “Better”, “Unchanged”, or “Worse”) in response to the question: “Has your pain improved?”. The results were dichotomized into Improved (“Pain-free” and “Better”) and Not improved (“Unchanged” and “Worse”) in the statistical analyses.
Treatment type
Treatment type was assessed using the question “Which treatment did you receive after your initial consultation at the hospital?” with “Physiotherapy”, “Pain killers”, “Injection”, and “Others” being the possible answers. If the participant chose “Other”, he/she was asked to state which treatment was received. The participants were allowed to tick more than one box when appropriate.
Patients’ opinion concerning their knee and associated problems
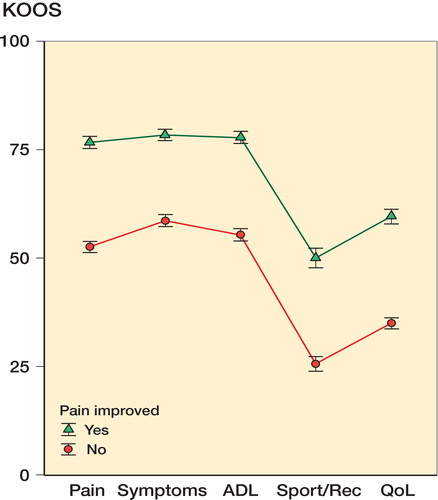
This was assessed using the knee injury and osteoarthritis outcome score (KOOS), which consists of the 5 subscales “Pain”, “Other symptoms”, “Function in activities of daily living (ADL)”, “Function in sports and recreation (Sport/Rec)”, and “Knee-related quality of life (QOL)” (CitationRoos et al. 1998, CitationRoos and Toksvig-Larsen. 2003).
Other measures
Radiographic severity was graded by one of the authors (CAD) using the original Kellgren-Lawrence (K&L) scale (CitationKellgren and Lawrence 1957). The reliability (Cohen’s kappa) of this grading was assessed for 33 of the participants, and this showed acceptable reliability with an intra-tester reliability of 0.82 (adjusted agreement of 88%) and an inter-tester reliability of 0.91 (adjusted agreement of 94%) compared to an experienced high-volume orthopedic surgeon evaluating K&L scores daily (OS).
Body mass index (BMI) was registered by a nurse at the consultation with the orthopedic surgeon (not routinely). BMIs were divided into 3 groups in the statistical analyses (≤ 24.9, 25.0–29.9, and ≥ 30.0).
Statistics
Primary analysis
We used logistic regression analysis and analysis of variance (ANOVA; to test the significance of each independent variable as a whole) to assess the association between improvements in pain following nonoperative treatment (Improved/Not improved) and radiographic severity adjusted for treatment type, age, sex, and BMI. We considered age as a continuous variable, and sex, treatment type, radiographic severity (K&L), and BMI as categorical variables.
We performed logistic regression analyses and ANOVAs with the following explanatory variables (5 models): (1) Main effect: K&L. (2) Main effects: K&L, age, sex, and treatment type. (3) Main effects: K&L, age, sex, BMI, and treatment type. (4) Main effects: K&L, age, sex, and treatment type. Pairwise interaction between K&L and each of the 3 other independent variables (age, sex, and treatment type). (5) Main effects: K&L, age, sex, BMI, and treatment type. Pairwise interaction between K&L and each of the 4 other independent variables (age, sex, BMI, and treatment type).
Secondary analyses
Additionally, the models were used to assess whether improvements in pain (Improved/Not improved) were associated with treatment type (No treatment, Physiotherapy, Pain killers, Injection, Other nonoperative, Two or more nonoperative).
KOOS was used to describe the population at follow-up and to compare those who had improvement in pain after nonoperative treatment to those who had not improved, using ANOVA. Post hoc Welch 2-sample t-tests were used to test for differences in each KOOS subscale.
We performed a non-responder analysis based on age (Welch 2-sample t-test) and sex (Fisher’s exact test) in patients who responded to the follow-up questionnaire, comparing those with complete data to those who did not have complete data.
Odds ratios (ORs) were used to assess whether each of the explanatory variables was associated with improvements in pain. We used 1% as the level of statistical significance and R statistical software version 3.1.1 to perform the analyses (CitationR Core Team 2014).
Ethics and registration
According to the National Committee on Health Research Ethics in Denmark, ethical approval was not needed. The study was conducted in accordance with the Declaration of Helsinki. It was registered at ClinicalTrial.gov (NCT02091830).
Results
Participants
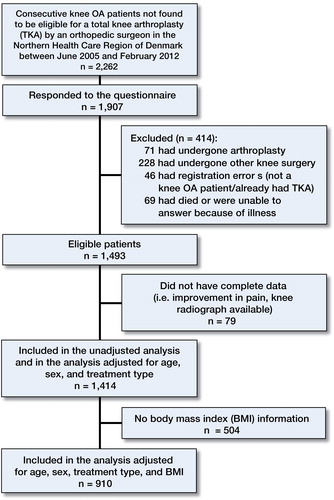
414 patients (22%) were excluded for various reasons. Of the 1,493 patients who were eligible for the study, 1,414 (95%) responded to the questionnaire with complete data on improvement in pain and treatment type, with knee radiographs available from their consultation with the orthopedic surgeon. Of the 1,414 participants, BMI was available for 910 (64%) ().
Apart from physiotherapy, pain killers, and injections, knee orthoses and foot orthoses were some of the most frequently used nonoperative treatments (). At follow-up, the mean KOOS values (with range) for all 1,414 participants were 64 (0–100), 68 (7–100), 66 (0–100), 37 (0–100), and 46 (0–100) for the subscales Pain, Symptoms, ADL, Sport/Rec, and QOL, respectively.
Table 1. Descriptive data on the participants a
Primary analysis
There was no association between radiographic severity and self-reported improvement in pain. When we adjusted for type of treatment, sex and age—and also the same variables and BMI—this did not change the estimates, showing that there was no association between radiographic severity and self-reported improvement in pain ().
Table 2. Results from the logistic regression analyses. Outcome: improvement in pain
When we included the predefined interactions in the analysis (models 4 and 5), similar estimates were found and no significant interactions were apparent (data not shown).
Secondary analyses
Compared to no treatment, physiotherapy (OR = 2.4 and 2.4) and 2 or more nonoperative treatments (OR = 2.1 and 2.2) were significantly associated with improvement in pain when we adjusted for radiographic severity, age, and sex—and when we adjusted for the same variables and BMI ().
Mean KOOS values for the 648 participants with improved pain were significantly higher than for the 766 participants without improvement in pain following nonoperative treatment (p < 0.001). Mean differences (with 95% confidence interval (CI)) in KOOS subscale scores were 24 (22–6) for Pain, 20 (18–22) for Symptoms, 22 (20–24) for ADL, 24 (22–27) for Sport/Rec, and 25 (23–27) for QOL ().
Non-responder analysis
The 79 participants with incomplete data were older (mean difference 6.6 years (95% CI: 3.9–9.4)), but had similar sex distribution (p = 0.30) to the 1,414 participants examined in the primary and secondary analyses.
Discussion
We found that radiographic severity was not associated with improvement in pain after nonoperative treatment in patients with knee OA. This was also true after adjusting for known confounders and the type of treatment the patient received. Our findings confirm a recent meta-analysis demonstrating that physiotherapy (exercise) has similar effects on symptoms irrespective of the level of radiographic severity (CitationJuhl et al. 2014). This shows that the orthopedic surgeon can confidently refer a patient with severe radiographic knee OA for nonoperative treatment to improve symptoms.
Since knee OA is known to progress (CitationThorstensson et al. 2009), and since the prevalence of knee OA can be expected to increase substantially in the future (CitationHolt et al. 2011), early treatment strategies could be important to reduce the disease burden in the future by preventing (or even reversing) progression of the disease (CitationHunter 2011). Physiotherapy (exercise and patient education) in combination with weight loss (if needed) is recommended as the core treatment of knee and hip OA in evidence-based guidelines (CitationFernandes et al. 2013, CitationMcAlindon et al. 2014). Our study supports this, by demonstrating that nonoperative treatment (physiotherapy and a combined treatment) is associated with improvements in symptomatic knee OA. Since the diagnosis of knee OA can be given on a clinical basis (CitationZhang et al. 2010), and since only 0.5% of radiographs reveal pathology needing specific treatment (osteonecrosis, osteochondral lesion, fracture, and subluxation) (CitationSkou et al. 2014b), nonoperative treatment can be initiated regardless of the availability or severity of a radiograph.
Surprisingly, in our study only 41% of patients with knee OA who were found not to be eligible for a TKA by an orthopedic surgeon received nonoperative treatment within 1–5 years after the consultation, and only 10% received physiotherapy. Considering that the KOOS scores for the 5 subscales were up to 30 points lower than reference values from a population-based cohort with adults of similar age (CitationParadowski et al. 2006), it appears unlikely that the reason for this lack of treatment was that the patients had less severe symptoms of knee OA. It is well known that clinical practice does not reflect all recommendations of guidelines (CitationDeHaan et al. 2007, CitationSnijders et al. 2011, CitationDhawan et al. 2014). A recent study showed results similar to ours, demonstrating that only 10% of patients who received a TKA had undergone physiotherapy specifically for their knee OA in the preceding 5 years (CitationDhawan et al. 2014). Based on the small proportion that received nonoperative treatment, it was not surprising that only half felt that their pain had improved since their consultation with the orthopedic surgeon. Given the results of our study, improvement of adherence to the guidelines has the potential to improve pain in a higher proportion of patients with knee OA; introducing a nationwide initiative comprising physiotherapist-led exercise and education could be a way of accomplishing this (CitationSkou et al. 2014a).
Some limitations of the study should be considered. First of all, BMI was not available for all the participants. However, the analysis with adjustment for BMI showed similar results to the analysis without adjustment for BMI. Secondly, regression towards the mean could influence the improvements found from treatment. However, as the odds of improvements were higher in patients who received physiotherapy or multimodal treatments than in patients who had no treatment (serving as a control group), regression towards the mean appears less important. Furthermore, the assessment of improvement in pain was done using an unvalidated scale, which could be regarded as a limitation. However, statistically significant differences were found between those whose pain improved and those whose pain did not improve, in all KOOS subscales—a reliable, validated, and responsive outcome measure (CitationRoos and Lohmander 2003). This supports the validity of the results from the primary analysis. Another limitation of the study was the lack of information on what the physiotherapy involved. Since the effects of physiotherapy-related treatments are known to vary (CitationMcAlindon et al. 2014), the effect of physiotherapy found in our study represents an average of the effects of different treatments—both treatments known to be effective (e.g. exercise and education) and treatments of uncertain effectiveness (e.g. ultrasound) (CitationMcAlindon et al. 2014). Thus, the treatment of knee OA with exercise and education as recommended in clinical guidelines (CitationFernandes et al. 2013, CitationMcAlindon et al. 2014) is likely to result in an even better chance of improvement in pain than was demonstrated in our study.
To summarize, the level of radiographic severity was not associated with improvement in pain after nonoperative treatment. In patients who are not eligible for TKA, the orthopedic surgeon can confidently refer patients for nonoperative treatment even in severe radiographic knee OA and in patients with high BMI. The treatment should preferably be a combined treatment including physiotherapy, as recommended in clinical guidelines.
Study conception and design: STS, MMA, MSR, and OS. Acquisition of data: CAD. Analysis and interpretation of data: STS, CAD, MMA, MSR, and OS. Drafting of the article and/or revising it critically for important intellectual content: STS, CAD, MMA, MSR, and OS. STS had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
We thank student nurse Signe Bruun Pedersen and medical secretary Pia Nygreen Christensen for helping with the identification of patients for the study and with the administration of questionnaires. The study did not receive any external funding.
No competing interests declared.
- Bedson J, Croft PR. The discordance between clinical and radiographic knee osteoarthritis: A systematic search and summary of the literature. BMC Musculoskelet Disord 2008; 9: 116.
- DeHaan MN, Guzman J, Bayley MT, Bell MJ. Knee osteoarthritis clinical practice guidelines -- how are we doing? J Rheumatol 2007; 34 (10): 2099–105.
- Dhawan A, Mather RC3rd, Karas V, Ellman MB, Young BB, Bach BRJr, Cole BJ. An epidemiologic analysis of clinical practice guidelines for non-arthroplasty treatment of osteoarthritis of the knee. Arthroscopy 2014; 30 (1): 65–71.
- Dieppe PA. Relationship between symptoms and structural change in osteoarthritis: What are the important targets for therapy? J Rheumatol 2005; 32 (6): 1147–9.
- Fernandes L, Hagen KB, Bijlsma JW, et al. EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann Rheum Dis 2013; 72 (7): 1125–35.
- Guccione AA, Felson DT, Anderson JJ, et al. The effects of specific medical conditions on the functional limitations of elders in the framingham study. Am J Public Health 1994; 84 (3): 351–8.
- Holt HL, Katz JN, Reichmann WM, et al. Forecasting the burden of advanced knee osteoarthritis over a 10-year period in a cohort of 60-64 year-old US adults. Osteoarthritis Cartilage 2011; 19 (1): 44–50.
- Hootman JM, Helmick CG. Projections of US prevalence of arthritis and associated activity limitations. Arthritis Rheum 2006; 54 (1): 226–9.
- Hunter DJ. Lower extremity osteoarthritis management needs a paradigm shift. Br J Sports Med 2011; 45 (4): 283–8.
- Juhl C, Christensen R, Roos EM, Zhang W, Lund H. Impact of exercise type and dose on pain and disability in knee osteoarthritis: A systematic review and meta-regression analysis of randomized controlled trials. Arthritis Rheumatol 2014; 66(3): 622–36.
- Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis 1957; 16 (4): 494–502.
- McAlindon TE, Bannuru RR, Sullivan MC, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage 2014; 22 (3): 363–88.
- Paradowski PT, Bergman S, Sunden-Lundius A, Lohmander LS, Roos EM. Knee complaints vary with age and gender in the adult population. population-based reference data for the knee injury and osteoarthritis outcome score (KOOS). BMC Musculoskelet Disord 2006; 7: 38.
- R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria 2014.
- Roos EM, Lohmander LS. The knee injury and osteoarthritis outcome score (KOOS): From joint injury to osteoarthritis. Health Qual Life Outcomes 2003; 1: 64.
- Roos EM, Toksvig-Larsen S. Knee injury and osteoarthritis outcome score (KOOS) - validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes 2003; 1: 17.
- Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee injury and osteoarthritis outcome score (KOOS)--development of a self-administered outcome measure. J Orthop Sports Phys Ther 1998; 28 (2): 88–96.
- Skou ST, Graven-Nielsen T, Rasmussen S, Simonsen O, Laursen MB, Arendt-Nielsen L. Widespread sensitization in patients with chronic pain after revision total knee arthroplasty. Pain 2013; 154 (9): 1588–94.
- Skou ST, Simonsen M, Odgaard A, Roos EM. Predictors of long-term effect from education and exercise in patients with knee and hip pain. Dan Med J 2014a; 61 (7): A4867.
- Skou ST, Thomsen H, Simonsen OH. The value of routine radiography in patients with knee osteoarthritis consulting primary health care: A study of agreement. Eur J Gen Pract 2014b; 20 (1): 10–6.
- Snijders GF, den Broeder AA, van Riel PL, Straten VH, de Man FH, van den Hoogen FH, van den Ende CH, NOAC Study Group. Evidence-based tailored conservative treatment of knee and hip osteoarthritis: Between knowing and doing. Scand J Rheumatol 2011; 40 (3): 225–31.
- Thorstensson CA, Andersson ML, Jonsson H, Saxne T, Petersson IF. Natural course of knee osteoarthritis in middle-aged subjects with knee pain: 12-year follow-up using clinical and radiographic criteria. Ann Rheum Dis 2009; 68 (12): 1890–3.
- von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, STROBE Initiative. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007; 370 (9596): 1453–7.
- Wang CT, Lin J, Chang CJ, Lin YT, Hou SM. Therapeutic effects of hyaluronic acid on osteoarthritis of the knee. A meta-analysis of randomized controlled trials. J Bone Joint Surg Am 2004; 86-A (3): 538–45.
- Zhang W, Doherty M, Peat G, et al. EULAR evidence-based recommendations for the diagnosis of knee osteoarthritis. Ann Rheum Dis 2010; 69 (3): 483–9.