Abstract
Background and purpose — Increased mortality after hip fracture is well documented. The mortality after hospitalization for upper extremity fracture is unknown, even though these are common injuries. Here we determined mortality after hospitalization for upper extremity fracture in patients aged ≥16 years.
Patients and methods — We collected data about the diagnosis code (ICD10), procedure code (NOMESCO), and 7 additional characteristics of 5,985 patients admitted to the trauma ward of Central Finland Hospital between 2002 and 2008. During the study, 929 women and 753 men sustained an upper extremity fracture. The patients were followed up until the end of 2012. Mortality rates were calculated using data on the population at risk.
Results — By the end of follow-up (mean duration 6 years), 179 women (19%) and 105 men (14%) had died. The standardized mortality ratio (SMR) for all patients was 1.5 (95% CI: 1.4–1.7). The SMR was higher for men (2.1, CI: 1.7–2.5) than for women (1.3, CI: 1.1–1.5) (p < 0.001). The SMR decreased with advancing age, and the mortality rate was highest for men with humerus fractures.
Interpretation — In men, the risk of death related to proximal humerus fracture was even higher than that reported previously for hip fracture. Compared to the general population, the SMR was double for humerus fracture patients, whereas wrist fracture had no effect on mortality.
Hip fractures are associated with increased mortality in both women and men (Roberts and Goldacre 2003, CitationHaleem et al. 2008, CitationAbrahamsen et al. 2009, CitationHindmarsh et al. 2009, CitationHaentjens et al. 2010, CitationMundi et al. 2014), as are osteoporotic vertebral fractures (van CitationStaa et al. 2001, CitationO’Neill and Roy 2005, CitationHarris et al. 2010). The influence of upper extremity fracture on mortality is far less studied, and the findings reported have been inconsistent. However, some reports suggest that proximal humerus fracture may be associated with increased mortality during the first year after the fracture (CitationShortt and Robinson 2005, CitationPiirtola et al. 2008). In contrast, the reported survival of wrist fracture patients may resemble or be better than that of the general population (CitationO’Neill and Roy 2005, CitationShortt and Robinson 2005).
We investigated mortality in adults with an upper extremity fracture that required inpatient care in a trauma unit. In addition, we compared this mortality with mortality in the general population.
Patients and methods
Patient population
This study included all patients aged ≥ 16 years who were admitted to the trauma ward of Central Finland Hospital (CFH) in Jyväskylä, Finland, between January of 2002 and December of 2008. Patients under the age of 16 were treated at the department of pediatric surgery instead, and they were excluded from the study. CFH is the only public hospital in the Central Finland Hospital District (CFHD) and offers trauma care to a population of 250,000, which is approximately 5% of the population of Finland. Fracture patients living in the catchment area of the hospital district who are in need of surgical treatment are referred to CFH. They are hospitalized due to a planned surgical procedure, due to a severe fracture, or due to other conditions (e.g. poor general condition, frailty associated with advanced age, or significant comorbidities).
At the trauma ward, each patient’s social security number, municipality, diagnosis (ICD 10 code), procedure code (NOMESCO, Finnish version), code of external cause (ICD 10), side of injury, and time of arrival at the emergency department and ward were recorded in a registry. Complications during treatment were also recorded.
The first sustained upper extremity fracture was regarded as the index fracture. Some patients presented with multiple fractures together with soft tissue injuries. The mortality rate for patients presenting with multiple fractures was calculated. However, the concomitant injuries were not taken into account when calculating mortality rates. The mortality status of patients at the end of 2012 was obtained from Statistics Finland. The causes of death were classified according to the ICD 10 classification.
Statistics
The expected number of deaths was calculated on the basis of age-, sex- and calendar period-specific mortality rates in the Finnish population. The relative survival was calculated as the ratio between the survival observed and the survival expected in a population matched with regard to age, sex, and calendar period using the Ederer-II method (CitationEderer and Heise 1959). The standardized mortality ratio (SMR) was calculated as the ratio between the number of deaths observed and the number of deaths expected, with 95% confidence intervals (CIs), assuming a Poisson distribution.
Ethics
A research permit was granted by Central Finland Hospital on December 16, 2012.
Results
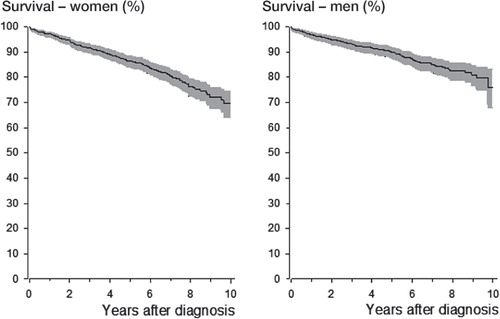
Between 2002 and 2008, 929 women and 753 men sustained at least 1 upper extremity fracture and were admitted to the trauma ward at CFH in Finland. The 1,682 patients had 1,989 fractures in total. The cohort was followed up for 10,106 person-years and the mean follow-up time was 6.0 years. The women were generally older than the men at the time of the upper extremity fracture: mean age 62 (SD 18) years in women vs. 46 (SD 17) years in men (p < 0.001). At the end of the follow-up period, 179 women and 105 men had died. The mortality for all patients was 3.0% (CI: 2.3–4.0) at 1 year, 7.7% (CI: 6.5–9.1) at 3 years, and 12% (CI: 11–14) at 5 years after the upper extremity fracture (). The mortality rate was 32 (CI: 28–37) per 1,000 person-years for women and 23 (CI: 19–28) per 1,000 person-years for men. The risk of dying was twice as high for men than for women, and between the sexes the age-adjusted hazard ratio (HR) for death was 2.0 (CI: 1.5–2.6).
Figure 1. Kaplan-Meier survival curves for 1,682 patients hospitalized for upper extremity fracture. The gray area indicates the 95% confidence interval.
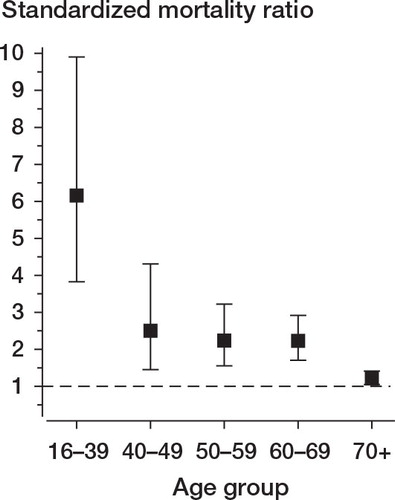
The relative survival of both women and men decreased linearly with time (). The SMR for all patients was 1.5 (CI: 1.4–1.7). The SMR for women was 1.3 (CI: 1.1–1.5) and for men it was 2.1 (CI: 1.7–2.5) (p < 0.001). The SMR for upper extremity fracture patients decreased with advancing age (). In patients younger than 60 years, the SMR was 2.2 (CI: 1.3–3.7) for women and 3.0 (CI: 2.3–4.1) for men. In patients who were 60 years old or more, the corresponding SMR values for women and men were 1.2 (CI: 1.1–1.5) and 1.6 (CI: 1.3–2.1).
Figure 2. The relative survival of 1,682 patients hospitalized for upper extremity fracture (929 women and 753 men). The whiskers show the 95% confidence intervals, and the dashed line represents the expected survival in the general population.
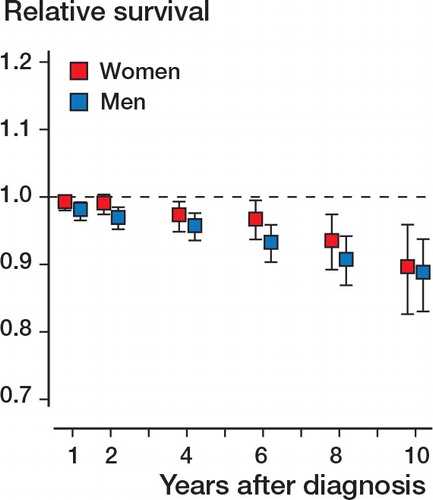
Figure 3. Standardized mortality ratios for 1,682 patients hospitalized for upper extremity fracture, by age group, with 95% confidence intervals. The dashed line represents the expected survival in the general population (standardized mortality ratio = 1).
In both sexes, fractures of the humerus were associated with higher mortality than the rest of the fracture types (). For humerus fractures (including all anatomic locations), the SMR was 2.0 (CI: 1.7–2.4); it was 1.7 (CI: 1.4–2.1) for women and 2.9 (CI: 2.3–3.8) for men. For proximal humerus fractures, the SMR was 2.2 (CI: 1.8–2.6); it was 1.6 (CI: 1.2–2.0) for women and 4.5 (CI: 3.3–6.1) for men. For wrist fractures, the SMR was 0.96 (CI: 0.74–1.2); it was 0.87 (CI: 0.65–1.2) for women and 1.5 (CI: 0.88–2.6) for men.
Table 1. Distribution of upper extremity fractures and mortality (per 1,000 person-years) in men and women hospitalized for upper extremity fracture (n = 1,682)
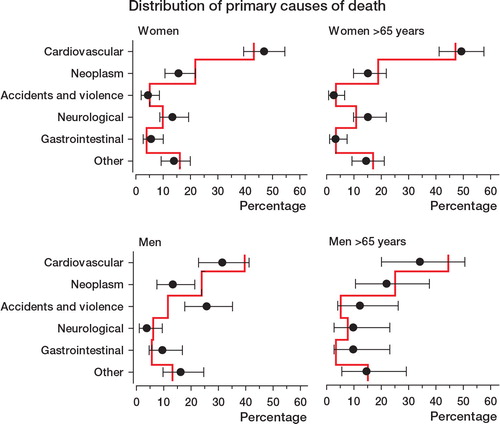
Cardiovascular diseases were the leading primary cause of death after upper extremity fracture in both sexes. Accidents and violence were the second most common cause of death in men (26%) but they accounted for only 4.5% of deaths in women. Conversely, neurological disease accounted for 13% of the deaths in women but only 3.8% of the deaths in men. When compared with the general population, deaths due to accidents and violence were more frequent in men. On the other hand, deaths due to neoplasms were less frequent in the cohort patients than in the general population ().
Discussion
In this population-based study, we found that mortality was higher in patients who were hospitalized after upper extremity fracture. This increase was greater in men than in women, and was highest after fractures of the humerus. Other authors have reported increased mortality after proximal humerus fracture, especially in men, with wrist fractures having little effect on mortality in outpatients and inpatients combined (CitationO’Neill and Roy 2005, CitationShortt and Robinson 2005, CitationPiirtola et al. 2008). Our results show that this is also true when only hospitalized patients are considered.
The increased mortality after hip fracture is well documented, with 2 studies reporting SMRs of 2.18 and 2.43 in women with hip fracture and 3.17 and 3.51 in men with hip fracture (CitationCenter et al. 1999, CitationBliuc et al. 2009). The SMR after humerus fracture in our population was almost as high as the SMR after hip fracture. Remarkably, men with proximal humerus fracture had an even higher SMR.
We know of only 1 previous study that addressed mortality after hospitalization for upper extremity fracture (CitationDeakin et al. 2007). The 1-year mortality in that British population after upper extremity fracture (4%) was similar to what we have observed (3%). A weakness of the British study was that it did not take account of the fracture site on the upper limb. The few previous studies on mortality after upper extremity fracture analyzed inpatients and outpatients as a single group. In addition, in those studies the populations were heterogeneous, the fracture sites were grouped in a variety of ways, and different methods were used to express mortality (CitationBarrett et al. 2003, CitationJohnell et al. 2004, CitationO’Neill and Roy 2005, CitationDeakin et al. 2007, CitationPiirtola et al. 2008, CitationIoannidis et al. 2009, CitationHuntjens et al. 2010, CitationMorin et al. 2011). Thus, we cannot really compare our findings to mortality rates reported by others. The authors of only 3 studies have reported SMRs for fracture patients (CitationCenter et al. 1999, CitationBliuc et al. 2009, CitationMelton et al. 2013). However, the 2 former studies did not address upper extremity fractures as a separate category, while Melton et al. collapsed different fracture site categories into larger groups. Mortality rates for upper extremity fracture cases treated in outpatient settings are likely to differ from those in inpatients, as cases with more severe injuries and comorbidities are more likely to be hospitalized. Comparisons of mortality in upper extremity fracture patients treated in inpatient and outpatient settings are thus important. However, to our knowledge there have not been any data reported concerning mortality in upper extremity fracture patients treated exclusively as outpatients.
Previous research has shown that comorbidity plays a role in the mortality associated with fractures (CitationBarrett et al. 2003, CitationShortt and Robinson 2005). However, one-quarter of the increased mortality seen after hip fracture is causally related to the fracture itself (CitationKanis et al. 2003). In our population, the relative mortality after upper extremity fracture increased linearly for several years after the fracture, whereas the mortality related to hip fracture is highest in the first year after the fracture and then levels off (CitationO’Neill and Roy 2005). This suggests that the upper extremity fracture in itself has only a minor influence on the death of the patient, and it may suggest that the fracture is an indicator of certain characteristics of the patient―such as frailty, or a risky lifestyle. To our knowledge, no one has estimated the direct effect of upper extremity fracture on mortality.
The relative mortality was highest in patients aged 16 to 39 years. This finding of increased mortality in younger people is in agreement with previous studies (CitationJohnell et al. 2004, CitationShortt and Robinson. 2005). However, to our knowledge, no previous studies have examined mortality after hospitalization for upper extremity fracture in such a young patient population. Based on our registry data, we cannot speculate on the reasons behind this observation.
In a previous Finnish study, cardiovascular diseases accounted for half of the causes of death in men aged ≥ 65 years (CitationPiirtola et al. 2008). The corresponding percentage in our analysis was smaller, accounting for one-third of all deaths. However, the rate of cardiovascular deaths in older women (49%) was in line with the findings of the previous Finnish study. Interestingly, deaths due to accidents and violence in older men were more common in our population (12% as opposed to 4%).
Strengths and weaknesses
One strength of the present study was that adults of all ages were included. In Finland, all deaths and causes of death are recorded by Statistics Finland. We therefore had access to accurate data on the mortality of the fracture patients and to that of the general population. This also allowed us to calculate SMRs. SMR is a measure of mortality in a cohort in relation to the mortality in the general population. SMRs therefore enable accurate comparisons of mortality in different populations. Because of our population-based material, we believe that our results can be generalized to similar patients in other developed countries.
Our registry did not include data on patient comorbidities, so we could not study the influence of comorbidity on mortality. Upper extremity fractures are common. For proximal humerus fractures alone, an incidence rate of 105 per 105 for patients older than 60 years has been reported in Finland (CitationPalvanen et al. 2006), as compared to 26 per 105 in our material (for all ages). Thus, several patients in the control population are bound to have sustained an upper extremity fracture. Therefore, our results possibly underestimate the increased mortality associated with upper extremity fractures.
AS: design of study, interpretation of data, and writing of manuscript; JP: design of study, interpretation of data, and critical revision of manuscript; HK: design of study, analysis and interpretation of data, and critical revision of manuscript; EL, MH: interpretation of data and critical revision of manuscript; IK: acquisition of data, design of study, interpretation of data, and critical revision of manuscript.
This study was supported by grants from the Finnish Research Foundation for Orthopaedics and Traumatology, Finska läkare sällskapet (Finnish medical association), Dorothea Olivia, Karl Walter och Jarl Walter Perkléns minnesstiftelse (D.O, K.W and J.W Perklén’s foundation)
No competing interest declared.
- Abrahamsen B, van Staa T, Ariely R, Olson M, Cooper C. Excess mortality following hip fracture: A systematic epidemiological review. Osteoporos Int 2009; 20 (10): 1633-50.
- Barrett JA, Baron JA, Beach ML. Mortality and pulmonary embolism after fracture in the elderly. Osteoporos Int 2003; 14 (11): 889-94.
- Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA 2009; 301 (5): 513-21.
- Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of osteoporotic fracture in men and women: An observational study. Lancet 1999; 353 (9156): 878-82.
- Deakin DE, Boulton C, Moran CG. Mortality and causes of death among patients with isolated limb and pelvic fractures. Injury 2007; 38 (3): 312-7.
- Ederer F, Heise H. Instructions to IBM 650 programmers in processing survival computations. Bethesda, National Cancer Institute 1959; Methodological note No. 10.
- Haentjens P, Magaziner J, Colon-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, Boonen S. Meta-analysis: Excess mortality after hip fracture among older women and men. Ann Intern Med 2010; 152 (6): 380-90.
- Haleem S, Lutchman L, Mayahi R, Grice JE, Parker MJ. Mortality following hip fracture: Trends and geographical variations over the last 40 years. Injury 2008; 39 (10): 1157-63.
- Harris MB, Reichmann WM, Bono CM, et al. Mortality in elderly patients after cervical spine fractures. J Bone Joint Surg Am 2010; 92 (3): 567-74.
- Hindmarsh DM, Hayen A, Finch CF, Close JC. Relative survival after hospitalisation for hip fracture in older people in New South Wales. Australia. Osteoporos Int 2009; 20 (2): 221-9.
- Huntjens KM, Kosar S, van Geel TA, et al. Risk of subsequent fracture and mortality within 5 years after a non-vertebral fracture. Osteoporos Int 2010; 21 (12): 2075-82.
- Ioannidis G, Papaioannou A, Hopman WM, et al. Relation between fractures and mortality: Results from the Canadian multicentre osteoporosis study. Cmaj 2009; 181 (5): 265-71.
- Johnell O, Kanis JA, Oden A, et al. Mortality after osteoporotic fractures. Osteoporos Int 2004; 15 (1): 38-42.
- Kanis JA, Oden A, Johnell O, De Laet C, Jonsson B, Oglesby AK. The components of excess mortality after hip fracture. Bone 2003; 32 (5): 468-73.
- Melton L JIII, Achenbach SJ, Atkinson EJ, Therneau TM, Amin S. Long-term mortality following fractures at different skeletal sites: a population-based cohort study. Osteoporosis Int 2013; 24:1689-1696
- Morin S, Lix LM, Azimaee M, Metge C, Caetano P, Leslie WD. Mortality rates after incident non-traumatic fractures in older men and women. Osteoporos Int 2011; 22 (9): 2439-48.
- Mundi S, Pindiprolu B, Simunovic N, Bhandari M. Similar mortality rates in hip fracture patients over the past 31 years. Acta Orthop 2014; 85 (1): 54-9.
- O’Neill TW, Roy DK. How many people develop fractures with what outcome? Baillieres Best Pract Res Clin Rheumatol 2005; 19 (6): 879-95.
- Palvanen M, Kannus P, Niemi S, Parkkari J. Update in the epidemiology of proximal humeral fractures. Clin Orthop 2006; 442: 87-92.
- Piirtola M, Vahlberg T, Lopponen M, Raiha I, Isoaho R, Kivela SL. Fractures as predictors of excess mortality in the aged-a population-based study with a 12-year follow-up. Eur J Epidemiol 2008; 23 (11): 747-55.
- Roberts SE, Goldacre MJ. Time trends and demography of mortality after fractured neck of femur in an English population. 1968-98: Database study. Bmj 2003; 327 (7418): 771-5.
- Shortt NL, Robinson CM. Mortality after low-energy fractures in patients aged at least 45 years old. J Orthop Trauma 2005; 19 (6): 396-400.
- van Staa TP, Dennison EM, Leufkens HG, Cooper C. Epidemiology of fractures in England and Wales. Bone 2001; 29 (6): 517-22.