A 13-year-old girl presented at our tertiary referral center with bilateral posterior radial head dislocation and aplasia of the ulnar coronoid process (). She was pain-free, had a 30-degree lack of elbow extension, limited forearm pronation and supination (80–20 degrees on the right side, 80–0 degrees on the left side), but no signs of elbow instability. After several years without any relevant restrictions during her daily life activities, she returned to our outpatient clinic at the age of 17 with increasing pain on both sides and distinct radiological signs of posterior humeroulnar dislocation due to aplasia of the ulnar coronoid process (). A review of the literature did not yield any information about that specific deformity or any possible treatment options. We decided to reconstruct the right elbow via an anteromedial approach, using a tricortical iliac crest bone graft as a coronoid equivalent and artificial bony restraint to the elbow joint.
Figure 1. At age 13. Posterior radial head dislocation in both elbows with a bilaterally missing, aplastic ulnar coronoid process. Note the convex posterior contour of the ulna, which is a common finding in cases with congenital dorsal radial head dislocation. There was no humeroulnar dislocation visible on the right side (A, C) and minimal dislocation on the left side (B, D). However, both elbows were stable on clinical examination and the patient did not report any pain or any other symptoms.
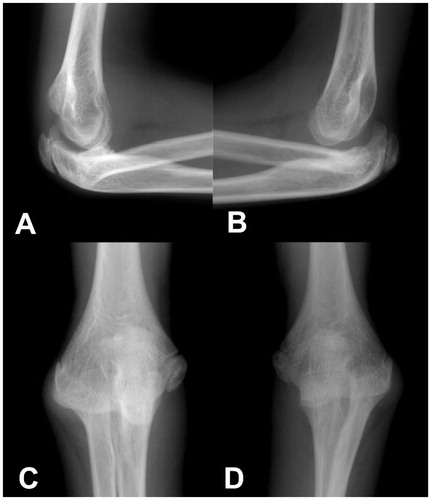
Figure 2. At age 17. A and B. Progredient posterior dislocation in both elbows. C. The postoperative 3D CT-scan shows the reconstructed anterior elbow buttress. D. At the latest follow-up 12 months after surgery, with full consolidation of the graft and a well-reduced elbow joint.
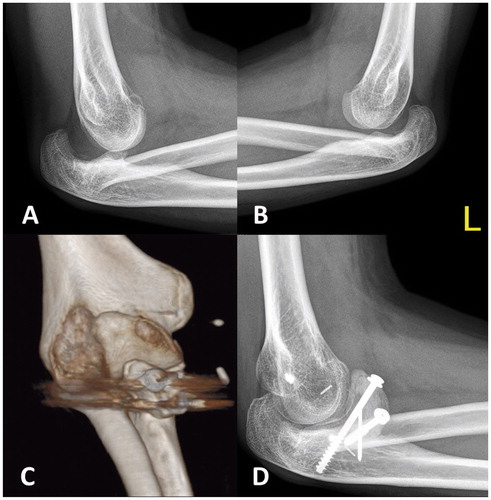
Firstly, the aplastic, cartilaginous remnant of the coronoid process was resected to form a cancellous bone ground for graft attachment. Thereafter, the bone graft was fixed with 2 cannulated 4.5-mm screws; the apophysis of the graft was orientated towards the trochlea humeri to serve as a joint surface (). No attempt was made to reduce the dislocated radial head. However, we additionally enforced the hyperlax ulnar collateral ligaments by use of two 3.5-mm suture anchors. The anterior joint capsule was closed, the musculus brachialis was re-attached to the capsule, and finally prophylactic forearm fasciotomies were made. A dynamic external elbow fixator was used in order to give temporary stability and allow early mobilization of the elbow joint.
The range of motion of the elbow was restricted to 40–110 degrees for 4 weeks in order to avoid shear forces on the graft during extension, and active and passive physiotherapy was initiated 2 days postoperatively. The fixator was removed 8 weeks postoperatively and replaced by a forearm splint until consolidation was seen on CT-scans 2 months postoperatively. At the latest follow-up examination 1 year postoperatively, the patient was very satisfied with the intervention (). She had no pain and showed improved elbow range of motion (20–140 degrees) and forearm pronation and supination (80–60 degrees). 8 months after the index intervention, an identical procedure was performed on the contralateral side but without enforcement of the collateral ligaments. Elbow range of motion and forearm pronation and supination improved on this extremity to 20–140 and 80–45 degrees, respectively. The postoperative course remained uneventful without any complications on both operated extremities.
Discussion
Congenital elbow deformities in children and adolescents are rare disorders, which are most often related to a congenital posterior (or less often anterior) dislocation of the radial head. While results after surgical reconstruction and nonoperative treatment in patients with congenital radial head dislocation have been reported (Bengard et al. Citation2012), we are not aware of any published case accompanied by an additional congenital aplasia of the ulnar coronoid process. Although generally mild to moderate functional impairment may be present in patients with congenital radial head dislocation, reports after surgical interventions have shown various outcomes, so surgery is (in our opinion) mainly indicated when pain is the primary complaint. However, our reported case also showed a marked, deteriorating elbow instability at mid- to terminal-extension range, caused by a previously undescribed coronoid aplasia. The coronoid process is one of the main stabilizers of the elbow joint, especially during flexion-extension range, besides the joint capsule and collateral ligaments (Morrey and An Citation1983, Closkey et al. Citation2000). Our technique to reconstruct the anterior buttress of the elbow joint was successful in achieving stability without any loss of range of motion. A similar technique was previously reported in cases with comminuted coronoid fractures (Chung et al. Citation2007), and combined fractures of the olecranon, radial head, and coronoid process (Kohls-Gatzoulis et al. Citation2004). In contrast to other authors who investigated outcomes after different methods of open reduction and internal fixation techniques for coronoid fractures (Garrigues et al. Citation2011), we preferred the use of screws over suture lasso fixation because a good compression of the iliac bone graft could be achieved by this means. We observed neither implant failure nor malunion or heterotopic ossification at 1-year follow-up. We believe that this method is a valuable treatment option to regain elbow stability whenever the coronoid process is absent. An additional collateral ligament reconstruction may be added, depending on the individual situation. Early mobilization is crucial to avoid elbow stiffness, as reported previously for a posttraumatic situation (Kohls-Gatzoulis et al. Citation2004); so the addition of temporary monolateral external fixation is in our opinion a good option to allow early remobilization. Nevertheless, patients should be counseled about the inherent risks of this procedure—such as recurrent instability, reduced joint range of motion, or potential osteoarthritis in the long term.
SF operated on the patient and wrote the manuscript. JR operated on the patient. RG revised the manuscript. WG operated on the patient and revised the manuscript.
- Bengard M J, Calfee R P, Steffen J A, Goldfarb C A. Intermediate-term to long-term outcome of surgically and nonsurgically treated congenital, isolated radial head dislocation. J Hand Surg Am 2012; 37 (12): 2495-501.
- Chung C H, Wang S J, Chang Y C, Wu S S. Reconstruction of the coronoid process with iliac crest bone graft in complex fracture-dislocation of elbow. Arch Orthop Trauma Surg 2007; 127 (1): 33-7.
- Closkey R F, Goode J R, Kirschenbaum D, Cody R P. The role of the coronoid process in elbow stability. A biomechanical analysis of axial loading. J Bone Joint Surg (Am) 2000; 82 (12): 1749-53.
- Garrigues G E, Wray W H 3rd, Lindenhovius A L, Ring D C, Ruch D S. Fixation of the coronoid process in elbow fracture-dislocations. J Bone Joint Surg (Am) 2011; 93 (20): 1873-81.
- Morrey B F, An K N. Articular and ligamentous contributions to the stability of the elbow joint. Am J Sports Med 1983; 11 (5): 315-9.
- Kohls-Gatzoulis J, Tsiridis E, Schizas C. Reconstruction of the coronoid process with iliac crest bone graft. J Shoulder Elbow Surg 2004; 13 (2): 217-20.

