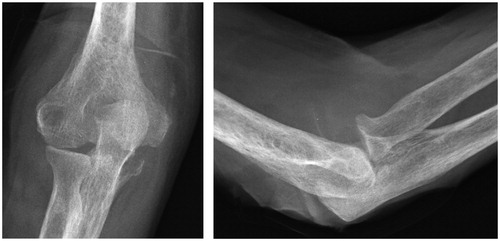
A 79-year-old man of South Asian origin presented at the trauma and orthopedic unit of a district general hospital with atraumatic pain in his right elbow, which he had had for 6 months, and a persistent cough. Given the demographics of the patient and the presenting symptoms, there was high clinical suspicion of tuberculosis, which we investigated accordingly. Routine blood tests and radiographs of the chest and elbow did not give a specific diagnosis (). In accordance with National Institute of Health and Clinical Excellence (Citation2011) guidelines, a bronchial lavage was then performed. Samples were sent for microscopy and culture, looking specifically for acid-fast bacilli. The final culture results were reported after 8 weeks and were negative. The elbow was painful but not swollen, and there was no indication for further investigation at this stage.
Throughout this time, routine clinical assessments did not reveal any systemic signs or symptoms of acute or chronic infection. The patient remained clinically well and afebrile, and routine blood tests were within reference ranges except for a mild rise in C-reactive protein. This, combined with the negative culture results, reassured us that tuberculosis was unlikely. As the elbow remained painful and swollen, but with no clinical evidence of intra-articular involvement, the patient was given the diagnosis olecranon bursitis and steroid injections were administered, initially with good response. However, a few months later he returned with worsening pain and reduced range of motion. At this time, de novo swellings were noted over the posterolateral distal humerus. He had no further respiratory issues.
Aspiration under sterile conditions revealed purulent fluid, which was sent for microscopy and culture. Due to the previous (negative) culture results, tuberculosis was not suspected. Initial results did not reveal any organisms.
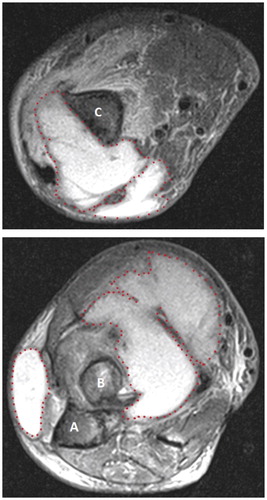
Because of his swollen and inflamed elbow, he was now started empirically on intravenous flucloxacillin. When there was no response to this intervention, magnetic resonance imaging (MRI) of the elbow was performed and revealed a large, multi-loculated collection in continuity with the elbow joint and marked synovial proliferation with bony erosions (). These radiological findings gave high suspicion of tuberculosis (Malavia and Kotwal Citation2003). Incision and drainage was performed, and tissue and fluid specimens were sent for a polymerase chain reaction (PCR) test for Mycobacterium tuberculosis complex DNA, which was positive. 1 week after the PCR results, the sample from the first aspiration confirmed the presence of alcohol- and acid- fast bacilli. This was after an extended culture period of 11 weeks.
Figure 2. MRI showed a multi-loculated collection at the distal humerus (upper panel) and the proximal radio-ulnar joint (lower panel). Key: A: ulna; B: radius; C: humerus.
The patient was started on standard quadruple therapy for Mycobacterium tuberculosis, to which he responded well. However, plain radiographs 2 months after the commencement of treatment showed evidence of further osteoarticular destruction (). Examination of the elbow joint showed full healing of the surgical wounds and a resolution of the swelling, but a residual functional deficit in keeping with the bony destruction.
Discussion
Infections with Mycobacterium tuberculosis are notorious for their propensity to mimic other pathologies, and as such they present a significant diagnostic challenge (Harisinghani et al. Citation2000, Walls and Shingadia Citation2007, LoBue et al. Citation2010) . Osteoarticular tuberculosis used to be an often-missed subset of these infections, due to its perceived rarity.
The incidence of tuberculosis is increasing in the United Kingdom according to the UK Health Protection Agency (Citation2012), which attributes this to migration, increasing rates of immunosuppressive disease, multidrug-resistant strains of Mycobacterium, and increasing exposure of healthcare workers (Pigrau-Serrallach and Rodríguez-Pardo Citation2013). This rising incidence has been recognized in all aspects of healthcare (Magnussen et al. Citation2013), but despite the increased awareness, cases can still be missed—leading to significant morbidity.
As demonstrated by our case, delay in diagnosis of tuberculous arthritis can result in irreversible osteoarticular destruction. It is therefore imperative that an accurate diagnosis be obtained in a timely manner, to minimize functional deficit and morbidity. Despite our high suspicion of tuberculosis and appropriate first-line investigations, we were falsely reassured by the negative lavage and initially negative aspiration culture. The resulting delay in diagnosis and initiation of definitive treatment led to significant damage to the elbow. Our case is very similar to a case reported by Holder et al. in 1985, where tuberculous arthritis presented as chronic bursitis of the olecranon. In that case, the patient presented with a 3-month history and underwent serial bursal debridements over the course of 4 years before the diagnosis of Mycobacterium tuberculosis was confirmed by extended culture for acid-fast bacilli.
This highlights the difficulty in identifying Mycobacterium as the causative agent, particularly given its propensity to mimic other pathologies. Even 30 years on from Holder’s case report, when tuberculosis is a far more recognized disease in the western world with advances in diagnostic technology, cases can still be missed and clinicians must remain vigilant.
- Holder S F, Hopson C, Vonkuster L. Tuberculous arthritis of the elbow presenting as chronic bursitis of the olecranon: a case report. J Bone Joint Surg (Am) 1985; 67(7): 1127-112
- Harisinghani M, McLoud T, Shepard J, Ko J, Shroff M, Mueller R. Tuberculosis from head to toe. Radiographics 2000; 20 (2): 449-70.
- Malavia A, Kotwal P. Arthritis associated with tuberculosis. Best Pract Res Clin Rheumatol 2003; 17(2): 319-43.
- Walls T, Shingadia D. The epidemiology of tuberculosis in Europe. Arch Dis Child 2007; 92 (8): 726–9.
- LoBue P, Enarson D, Thoen T. Tuberculosis in humans and its epidemiology, diagnosis and treatment in the United States. Int J Tuberc Lung Dis 2010; 14(10): 1226-32.
- National Institute for Health and Clinical Excellence. CG117. Tuberculosis: Clinical diagnosis and management of tuberculosis, and measures for its prevention and control. NICE; 2011
- Health Protection Agency (2012) Tuberculosis in the UK: 2012 report (HPA, London) [online] Available from: http://www.hpa.org.uk/webw/HPAweb&HPAwebStandard/HPAweb_C/1317134916916 (accessed 29 April 2015).
- Magnussen A, Dinneen A, Ramesh P. Osteoarticular tuberculosis: increasing incidence of a difficult clinical diagnosis. BJGP 2013; 63 (612): 385-6.
- Pigrau-Serrallach C, Rodríguez-Pardo D. Bone and joint tuberculosis. Eur Spine J 2013; 22(4): 556–66.