Abstract
Background and purpose — Low bone mineral density (BMD) may jeopardize the initial component stability and delay osseointegration of uncemented acetabular cups in total hip arthroplasty (THA). We measured the migration of uncemented cups in women with low or normal BMD.
Patients and methods — We used radiostereometric analysis (RSA) to measure the migration of hydroxyapatite-coated titanium alloy cups with alumina-on-alumina bearings in THA of 34 female patients with a median age of 64 (41–78) years. 10 patients had normal BMD and 24 patients had low systemic BMD (T-score ≤ −1) based on dual-energy X-ray absorptiometry (DXA). Cup migration was followed with RSA for 2 years. Radiographic follow-up was done at a median of 8 (2–10) years.
Results — Patients with normal BMD did not show a statistically significant cup migration after the settling period of 3 months, while patients with low BMD had a continuous proximal migration between 3 and 12 months (p = 0.03). These differences in cup migration persisted at 24 months. Based on the perceived risk of cup revision, 14 of the 24 cases were “at risk” (proximal translation of 0.2 to 1.0 mm) in the low-BMD group and 2 of the10 cases were “at risk” in the normal-BMD group (odds ratio (OR) = 8.0, 95% CI: 1.3–48). The radiographic follow-up showed no radiolucent lines or osteolysis. 2 cups have been revised for fractures of the ceramic bearings, but none for loosening.
Interpretation — Low BMD contributed to cup migration beyond the settling period of 3 months, but the migrating cups appeared to osseointegrate eventually.
Cementless total hip arthroplasty (THA) was originally designed for middle-aged patients with normal bone quality (Spotorno et al. Citation1995). However, undiagnosed osteoporosis, which is not uncommon in postmenopausal women with hip osteoarthritis (Glowacki et al. Citation2003, Mäkinen et al. Citation2007, Lingard et al. Citation2010), may jeopardize achievement of immediate press-fit stability of uncemented components. Indeed, we recently found that low bone mineral density (BMD; osteopenia or osteoporosis) and age-related geometric changes of the proximal femur affected initial stability and delayed osseointegration of uncemented femoral stems in THA in female patients (Aro et al. Citation2012). It is possible that low systemic BMD may also compromise the initial stability of uncemented acetabular cups.
The success of bone ingrowth into or onto the microroughened/porous surface of an acetabular component depends on the degree of initial stability (Illgen and Rubash Citation2002). If the initial stability is compromised, implant micromotion may delay or even inhibit osseointegration to host bone. Cup stability is dependent on the geometric implant design, close implant-bone apposition, and frictional or interference press-fit fixation (Kraay et al. Citation2012). The inherent quality of the host bone is arguably equally important in achieving initial stability, although there is little information on the issue.
Patients with supposedly compromised bone quality due to rheumatoid arthritis or sequelae after a fracture of the femoral neck have shown increased migration of both cemented and uncemented cups in radiostereometric analysis (RSA) (Önsten et al. Citation1993, Snorrason et al. Citation1993, Digas et al. Citation2004). Adjunctive screw and spike fixation has been recommended in patients with poor bone quality, but the benefit of additional screw fixation has been questioned in RSA studies of primary THAs (Thanner et al. Citation2000, Pakvis et al. Citation2012).
There is no doubt that migration exceeding the detection level of RSA is predictive of clinical implant loosening (Kärrholm Citation2012). A recent meta-analysis confirmed that excessive migration of an acetabular cup at 2 years implies an elevated risk of late revision (Pijls et al. Citation2012). In the present study, we complemented our previous RSA analyses of the femoral stem migration in cementless THA of female patients with primary hip osteoarthritis (Moritz et al. Citation2011, Aro et al Citation2012) by investigating the stability of uncemented acetabular cups in the same study population.
Patients and methods
This study was performed as a 2-year, single-center RSA study on female patients who underwent cementless THA between August 2003 and March 2005. The enrolled patients were called in for the radiographic follow-up study, which was performed between October 2012 and January 2013.
Study participants
The main inclusion criteria were female patients aged less than 80 years with advanced primary hip osteoarthritis and without any severe incapacitating systemic disease (class 1–3 according to the Physical Status Classification of The American Society of Anesthesiologists (ASA)). The exclusion criteria were inflammatory arthritis, hereditary skeletal disease, untreated parathyroid disease, osteoporosis-drug therapy or corticosteroid therapy, any other medication affecting bone metabolism, and severe osteoporosis (T-score of less than −3.5).
A cohort of 110 consecutive patients who were scheduled for a cementless THA was invited to participate, and 61 of them consented to screening. They underwent studies for exclusion of undiagnosed primary or secondary osteoporosis (Mäkinen et al. Citation2007). Of those screened, 43 were eligible for recruitment. Exclusions were due to use of corticosteroid with or without concomitant bisphosphonate therapy (n = 8) or osteoporosis requiring initiation of bisphosphonate therapy (n = 10). Of the 43 patients recruited, 3 were excluded postoperatively due to periprosthetic femoral fracture (7 days, 9 days, and 21 days after surgery) and 6 were excluded for poor visualization of RSA markers. 34 patients were eventually included in the study.
For the data analysis, the patients were divided into groups with normal BMD or low BMD, based on their lowest T-score measured in preoperative dual-energy X-ray absorptiometry (DXA) (). DXA measurements were performed at the proximal femurs, the lumbar spine, and the distal non-dominant forearm with a Hologic QDR 4500C densitometer (Hologic Inc., Waltham, MA). A T-score value of ≤ −1 at any of the locations studied was used as the criterion for inclusion in the low-BMD group. The average time between the DXA measurements and surgery was 37 (SD 31) days.
Table 1. Baseline demography, preoperative and postoperative Harris hip score (HHS), and Western Ontario and McMaster arthritis index (WOMAC). Values are mean (SD)
Surgery and RSA
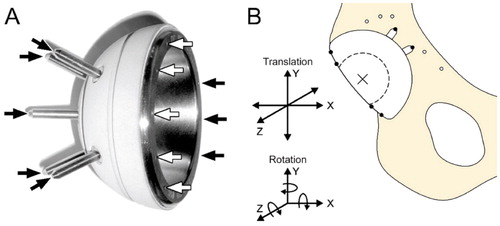
All patients received a CE-certified custom-modified cementless THA implant with ceramic-on-ceramic bearings (ABG II; Stryker Europe). Both the femoral stem (Aro et al. Citation2012) and the acetabular cup () were marked with RSA beads, by the manufacturer. The hemispherical titanium alloy cup had a grit-blasted surface with vacuum plasma-sprayed hydroxyapatite (HA) coating (porosity < 10%, crystallinity > 75%, crystal grain size 20–50 μm, thickness 60 ± 30 μm) and 2 circular grooves aimed at promoting osseointegration. The cups had 8 tantalum beads (1.0 mm) on the outer rim (). The 5-hole version of the cup was designed for use with tapered alumina insert and 28-mm alumina head (Biolox; CeramTec AG, Plochingen, Germany). It accommodated additional RSA beads (1.0 mm) on the tips of 5 custom-modified fixation spikes ().
Figure 1. A. The custom-modified acetabular cup with 8 RSA beads (arrows) inserted in the opening and additional RSA beads inserted at the tips of the 5 fixation spikes of the cup. B. The anatomical orientation of the coordinate system used to evaluate the translational and rotational migration of the cup.
The surgery was performed using an anterolateral Hardinge approach. During the operation, 4–6 tantalum beads (0.8 mm) were inserted into the cancellous bone of the acetabular socket. The cups were inserted using under-reaming with press-fit.
Baseline RSA imaging was performed within 7 days after surgery, with follow-up at 3, 6, 12, and 24 months. The accuracy of the RSA setup was validated with a phantom model (Mäkinen et al. Citation2004) and the international RSA guidelines were used (Valstar et al. Citation2005).
The RSA images were analyzed for migration relative to the baseline using UmRSA version 6.0.3.7 software (RSA BioMedical Innovations AB, Umeå, Sweden). The linear and angular movements were determined on 3 axes (x, y, and z) ( and ). The stability of individual markers and sufficiency of distribution were evaluated through mean error of rigid body fitting (ME) and condition number (CN) (Table 3, see Supplementary data). The cutoff points for ME and CN were kept at around 0.35 and 150, respectively. All patients were subjected to a double examination at least once, with repositioning between examinations, resulting in a total of 82 double measurements. The precision of the RSA measurements was calculated based on the differences measured in double examinations for each axis. The precision (the upper limit of 95% confidence interval (CI)) of the RSA measurements for translational migration was 0.35 mm for the x-axis, 0.25 mm for the y-axis, and 0.46 mm for the z-axis, and for rotational migration it was 1.79 degrees for the x-axis, 2.03 degrees for the y-axis, and 1.20 degrees for the z-axis.
Table 2. Acetabular cup migration in patients with normal BMD or low BMD at 24 months
In a recent meta-analysis of RSA studies (Pijls et al. Citation2012), acetabular cups with proximal translation of 1.0 mm or more at 2 years were considered to be at high risk of revision. Proximal translations of 0.2–1.0 mm and ≤ 0.2 mm were considered to indicate an elevated risk of revision and a low rate of revision, respectively. To this effect, we assigned each individual patient a risk classification of “high”, “at risk”, or “low” based on the extent of proximal translation at 24 months.
Functional recovery
Western Ontario and McMaster arthritis index (WOMAC) and Harris hip score (HHS) were collected at baseline and at each follow-up. The scores were subsequently evaluated for differences between the 2 BMD groups.
Conventional radiography
Conventional 2-plane radiographs were obtained postoperatively and at 6, 12, and 24 months. Of the 34 study patients, 23 took part in the radiographic follow-up at a median time of 9 (7–10) years. 4 patients had died of other comorbidities and 7 patients were unable to attend the follow-up visit, but they could be interviewed by telephone. In these 11 cases (3 with normal BMD and 8 with low BMD), cup survival was confirmed based on review of electronic medical records and the latest hip radiographs taken at a median of 3 (2–10) years. None of the patients were lost to follow-up. The serial radiographs were reviewed for postoperative appearance of radiolucent or reactive lines, or of osteolysis.
Statistics
The primary outcome measure was the relationship between the BMD group assigned and the migration measured by RSA at 24 months.
All relevant data were tested for normality using the Kolmogorov-Smirnov test. Parametric statistical tests were preferred. The equality of variances was established using Levene’s test. Student’s t-test was used as the independent-samples t-test.
The relationship between the BMD group assigned (normal BMD or low BMD) and cup migration on different axes at 24 months was evaluated using independent-sample t-test or, alternatively, the Mann-Whitney U-test when the assumption of normality was breached. The extent of any statistically significant difference between the BMD groups was further evaluated using age- and BMI-controlled multiple linear regression. Age was controlled for due to a minor but statistically significant difference in the mean ages of the 2 BMD groups ().
Fisher’s exact test was used to evaluate the relationship between the BMD group and the perceived risk of revision as determined by the risk classification system (Pijls et al. Citation2012). Repeated-measures ANOVA was used for comparison of WOMAC and HHS between the normal-BMD group and the low-BMD group, followed by paired-samples t-test as the post-hoc test in the comparison of time-related changes.
In order to delineate the outcome of the whole patient population, 1-sample t-test was used to detect statistically significant deviations of the mean movement from zero migration during the first 3 months after surgery. Any further migrations were evaluated using either Friedman test or repeated-measures ANOVA based on the normality of the data.
Data were analyzed as of the date of last data collection (July 2015). Statistical significance was assumed from a p-value ≤ 0.05 after Bonferroni correction for multiple tests, where applicable. All statistical analyses were done using IBM SPSS Statistics for Windows v. 21.0.
Ethics
The study had ethical approval from the Ethics Committee, Hospital District of Southwest Finland (entries 4/2002 §76 and 9/2012 §271).
Results
RSA migration
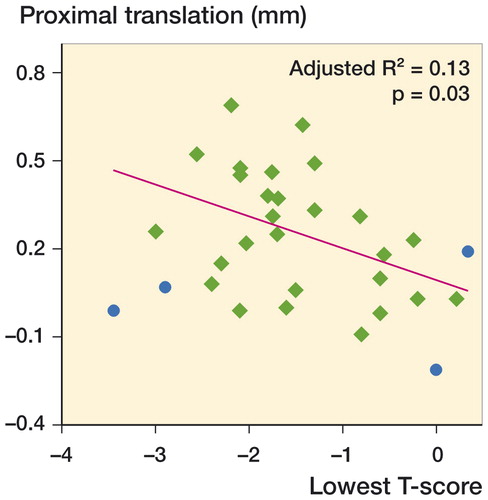
There was a statistically significant difference in cup migration between patients with normal BMD and those with low BMD. At 24 months, the patients belonging to the low-BMD group showed greater translation along the y-axis (proximal translation), while other modes of translation or rotation did not differ significantly between the groups (). Linear regression between the assigned BMD group and proximal translation was statistically significant even after age and BMI had been controlled for (β = 0.60, p = 0.001). Age did not predict proximal translation at a statistically significant level (β = −0.007, p = 0.2) whereas BMI did (β = 0.40, p = 0.01). The overall adjusted multiple linear regression model fit was R2 = 0.39.
The difference in proximal cup migration between the patients with normal BMD and those with low BMD appeared to progress after the settling period of 3 months ( and ). An extra analysis was therefore performed. Patients with low BMD had statistically significant proximal translation (paired-samples t-test, p = 0.03) between 3 and 12 months but not between 12 and 24 months (paired-samples t-test, p = 1.0). Patients in the normal-BMD group did not show statistically significant proximal migration at any time after 3 months (repeated-measures ANOVA, p = 0.9) as a sign of cup stability.
Figure 2. The proximal translation (mean ± SD) of the acetabular cups in patients with normal or low BMD during the first 24 months after surgery.
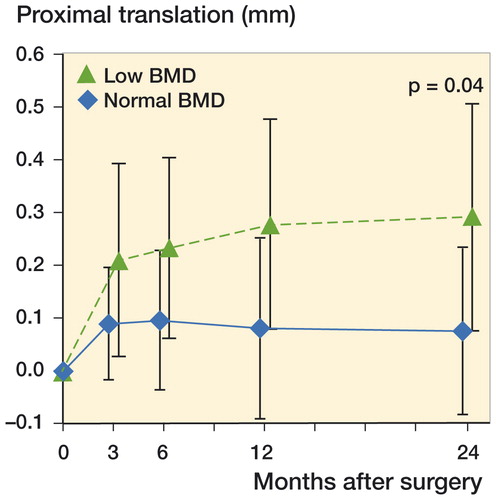
Figure 3. Proximal migration of the acetabular cups at 24 months plotted against the lowest T-score of each individual patient (diamonds). Outliers excluded from the linear regression (due to elevated Cook’s distance) are marked with round dots.
When the patients with low BMD and those with normal BMD were analyzed as 1 group, the cup showed statistically significant migration only during the first 3 months. By 3 months, translation occurred on the x-axis (0.14 mm, CI: 0.06–0.22; p = 0.006) and the y-axis (0.17 mm, CI: 0.11–0.23; p = 0.003). The initial rotation occurred on the z-axis alone (0.44°, CI: 0.20–0.68; p = 0.006).
Perceived risk of cup revision
By 24 months, there were no cases of high proximal translation (1 mm or more). In the low-BMD group, there were 14 (out of 21) cases “at risk of revision” (proximal translation of 0.2–1.0 mm), while in the normal-BMD group there were only 2 (out of 10) such cases, with the difference between the BMD groups being statistically significant (OR = 8.0, CI: 1.3–48; p = 0.02). The low-BMD group had a mean proximal translation of 0.29 (SD 0.21) mm, which lay within the classification limits of “at risk of revision”. The mean proximal translation in the normal-BMD group was 0.08 (SD 0.16) mm, corresponding to the classification “at low risk of revision”.
Functional recovery and radiographic outcome
The cup migration measured by RSA had no effect on the subjective or functional recovery from the hip replacement (). Both groups showed a significant improvement in the outcome measures postoperatively (p < 0.001 for both).
During the median follow-up time of 8 (2–10) years, cups of 2 patients in the low-BMD group were revised for fracture of a ceramic liner at 3 years and fracture of a ceramic head at 4 years. None of the cups were revised for loosening. Conventional radiographs did not show a postoperative appearance of either radiolucent or reactive lines, or of periprosthetic osteolysis. 2 patients have reported occasional audible squeaking.
Discussion
Confirming our hypothesis, patients with normal preoperative BMD did not show statistically significant cup migration after the settling period of 3 months, while patients with low BMD had minor but sustained proximal cup migration for up to 12 months.
The results of the whole patient population are in line with those of previous RSA studies of cementless acetabular cups (Önsten et al. Citation1996, Thanner et al. Citation2000, Digas et al. Citation2004, Rohrl et al. Citation2006, Zhou et al. Citation2006, Pakvis et al. Citation2012). The current study, like a recent meta-analysis (Pijls et al. Citation2012), showed that the migration occurs mainly along the y-axis (proximal translation). Interestingly, the increased migration in patients with low BMD was not evident statistically when the study patients were analyzed as 1 group. This finding suggests that the effect of low BMD does not become apparent in RSA studies without subgroup analysis of patients with defined BMD status. To our knowledge, this is the first study to report the RSA migration of the acetabular cup as a function of DXA-measured systemic BMD. Our results confirm the observations of Digas et al. (Citation2004), who reported increased migration of uncemented cups (as measured with RSA) in patients with osteoporosis suggested by their diagnosis (rheumatoid arthritis, failed femoral neck fracture, or being on cortisone treatment). These authors stratified and randomized patients based on preoperative DXA measurements, but they did not report the influence of preoperative DXA status on migration. In a randomized study of bisphosphonate treatment, Saari et al. (Citation2014) followed the changes in acetabular BMD and measured RSA migration of revision cups, but preoperative systemic DXA was not investigated as a predictor of cup migration.
3 patients were excluded due to early periprosthetic fracture of the proximal femur, which is a characteristic complication of the ABG II stem (Mäkelä et al. Citation2010). In line with the arthroplasty register records (Eskelinen et al. Citation2006, Mäkelä et al. Citation2010), our radiographic follow-up results of the ABG II acetabular cup were unremarkable, with no signs of radiolucent lines or osteolysis—resembling the “radiological silence” reported by Nourissat et al. (Citation2013). To date, 2 cups have been revised due to fracture of a ceramic head and a liner. 2 patients have complained of occasional squeaking. These complications are annoying unresolved problems with ceramic-on-ceramic bearings (Park et al. Citation2015, Hamilton et al. Citation2015).
Our study design did not include determination of the local acetabular BMD. We applied the lowest T-score from any of the DXA-measured skeletal sites as the indicator of systemic bone quality, because osteoarthritis may interfere with local BMD measurements and cause false-negative results (Mäkinen et al. Citation2007). In fact, using systemic BMD has advantages over using local BMD, as osteoporosis may go unnoticed unless BMD measurements are performed at sites distant from joints affected by osteoarthritis (Lingard et al. Citation2010).
The current analyses were part of a clinical study designed to evaluate the frequency of osteoporosis in female patients scheduled for cementless THA, and to determine the effect of reduced BMD on THA. At the time the study was initiated, systemic BMD status in female patients with primary hip osteoarthritis had not been studied systematically. This base study can provide the necessary data for power analyses when designing future studies.
Consecutive patients were recruited without any attempt to control the number of patients recruited in each BMD group, so the sizes of the groups were different. Although the normal-BMD group was small, we believe that it was representative. There were no outliers in the normal-BMD group, which showed stable cups after the settling period of 3 months. This is in line with the expected healing period (i.e. osseointegration). Another limitation of the recruitment methodology was that, for ethical reasons, patients with severe osteoporosis were put on osteoporosis medication and were therefore excluded.
The value of proximal migration in predicting long-term failure rates of acetabular cups was confirmed recently (Pijls et al. Citation2012), but little is known about the mechanisms and causes thereof. Anti-resorptive therapy with intravenous zoledronic acid may prevent cup migration (Friedl et al. Citation2009). The surgical procedure per se (THA with an uncemented cup) causes a decrease in periprosthetic acetabular BMD (Digas et al. Citation2006) and a single intravenous dose of pamidronate can reduce the loss of periprosthetic bone (Wilkinson et al. Citation2001). If the loss of periprosthetic bone is inevitable, our RSA results in patients with normal BMD suggest that such an adverse remodeling does not affect cup stability. Indeed, in support of this hypothesis, negative findings on the benefits of anti-resorptive treatment have also been reported, at least with revision acetabular cups (Saari et al. Citation2014). It is important to recognize that patients with low BMD are prone to periprosthetic bone loss in the proximal femur (Alm et al. Citation2009). A similar response is possible in the acetabular region. We cannot exclude the possibility that the increased cup migration in patients with low BMD was in part related to the increased postoperative loss of periprosthetic acetabular bone and not only a result of the impaired preoperative bone quality.
The main strengths of our study were the highly screened homogenous patient population and the application of custom-modified RSA implants. Major potentially confounding factors such as corticosteroid therapy and inflammatory arthritis were used as exclusion criteria. The homogenous patient population enabled the use of a fairly small sample size recommended for RSA studies (Valstar et al. Citation2005, Derbyshire et al. Citation2009).
The ceramic-on-ceramic bearings were chosen over other options in order to avoid the side effects of released metal ions and polyethylene wear particles (Malviya et al. Citation2010, Nich et al. Citation2013). The use of non-elastic ceramic-on-ceramic bearings may have added to the peak impact forces transmitted to the bone-implant interface. Theoretically, the increased impact forces could have worsened the proximal cup migration in the presence of compromised bone quality. However, a comparative RSA study has shown no statistically significant difference in cup migration between ceramic-on-ceramic bearings and metal-on-polyethylene bearings (Zhou et al. Citation2006).
One could argue against the use of uncemented cups, especially in patients with impaired bone quality (Hailer et al. Citation2010). The clinical value of bioactive HA coating remains unclear. Routine HA coating of uncemented cups may not be indicated (Lazarinis et al. Citation2010) but, based on preclinical studies, HA coating should be beneficial in helping incorporation of implants in osteopenic bones (Soballe et al. Citation1991).
In conclusion, our study has produced the first evidence of increased migration of uncemented cups in female patients with low systemic BMD. It appears that the normal settling period of 3 months was only extended, and that the migrating cups eventually osseointegrated with the host bone. Further research is certainly needed to establish what —if any—effect the increased proximal migration of uncemented cups in patients with low BMD has on the long-term clinical results.
Supplementary data
Table 3 is available on the Acta Orthopaedica website at www.actaorthop.org, identification number 8878.
SF analyzed the data and prepared the manuscript. NM performed the RSA measurements and prepared the manuscript. ES helped with the DXA measurements. JJA helped in data gathering and prepared the manuscript. HTA designed the study, operated on patients, and prepared the manuscript.
The study was financially supported by the Academy of Finland, Turku University Hospital, and Stryker Europe, which took no part in the organization of the study, in analysis of the results, or in writing of the manuscript.
- Alm J J, Mäkinen T J, Lankinen P, Moritz N, Vahlberg T, Aro H T. Female patients with low systemic BMD are prone to bone loss in Gruen zone 7 after cementless total hip arthroplasty. Acta Orthop 2009; 80 (5): 531–7.
- Aro H T, Alm J J, Moritz N, Mäkinen T J, Lankinen P. Low BMD affects initial stability and delays stem osseointegration in cementless total hip arthroplasty in women: A 2-year RSA study of 39 patients. Acta Orthop 2012; 83 (2): 107–14.
- Derbyshire B, Prescott R J, Porter M L. Notes on the use and interpretation of radiostereometric analysis. Acta Orthop 2009; 80 (1): 124–30.
- Digas G, Thanner J, Anderberg C, Kärrholm J. Bioactive cement or ceramic/porous coating vs. conventional cement to obtain early stability of the acetabular cup. randomised study of 96 hips followed with radiostereometry. J Orthop Res 2004; 22 (5): 1035–43.
- Digas G, Kärrholm J, Thanner J. Different loss of BMD using uncemented press-fit and whole polyethylene cups fixed with cement: Repeated DXA studies in 96 hips randomized to 3 types of fixation. Acta Orthop 2006; 77 (2): 218–26.
- Eskelinen A, Remes V, Helenius I, Pulkkinen P, Nevalainen J, Paavolainen P. Uncemented total hip arthroplasty for primary osteoarthritis in young patients: A mid-to long-term follow-up study from the finnish arthroplasty register. Acta Orthop 2006; 77 (1): 57–70.
- Friedl G, Radl R, Stihsen C, Rehak P, Aigner R, Windhager R. The effect of a single infusion of zoledronic acid on early implant migration in total hip arthroplasty. A randomized, double-blind, controlled trial. J Bone Joint Surg Am 2009; 91 (2): 274–81.
- Glowacki J, Hurwitz S, Thornhill T S, Kelly M, LeBoff M S. Osteoporosis and vitamin-D deficiency among postmenopausal women with osteoarthritis undergoing total hip arthroplasty. J Bone Joint Surg Am 2003; 85-A (12): 2371–7.
- Hailer N P, Garellick G, Kärrholm J. Uncemented and cemented primary total hip arthroplasty in the Swedish hip arthroplasty register. Acta Orthop 2010; 81 (1): 34–41.
- Hamilton W G, McAuley J P, Blumenfeld T J, Lesko J P, Himden S E, Dennis D A. Midterm results of delta ceramic-on-ceramic total hip arthroplasty. J Arthroplasty 2015 Jun 3. [Epub ahead of print]
- Illgen R, 2nd, Rubash H E. The optimal fixation of the cementless acetabular component in primary total hip arthroplasty. J Am Acad Orthop Surg 2002; 10 (1): 43–56.
- Kärrholm J. Radiostereometric analysis of early implant migration - a valuable tool to ensure proper introduction of new implants. Acta Orthop 2012; 83 (6): 551–2.
- Kraay M J, Rowbottom J S, Razek M G. The acetabular component in primary total hip arthroplasty. Seminars in Arthroplasty 2012; 23: 163–6.
- Lazarinis S, Kärrholm J, Hailer N P. Increased risk of revision of acetabular cups coated with hydroxyapatite. Acta Orthop 2010; 81 (1): 53–9.
- Lingard E A, Mitchell S Y, Francis R M, Rawlings D, Peaston R, Birrell F N, McCaskie A W. The prevalence of osteoporosis in patients with severe hip and knee osteoarthritis awaiting joint arthroplasty. Age Ageing 2010; 39 (2): 234–9.
- Malviya A, Ramaskandhan J, Holland J P, Lingard E A. Metal-on-metal total hip arthroplasty. J Bone Joint Surg Am 2010; 92 (7): 1675–83.
- Moritz N, Alm JJ, Lankinen P, Mäkinen TJ, Mattila K, Aro HT. Quality of intertrochanteric cancellous bone as predictor of femoral stem RSA migration in cmentless total hip arthroplasty. J Biomech 2011; 44: 221–7.
- Mäkelä K T, Eskelinen A, Paavolainen P, Pulkkinen P, Remes V. Cementless total hip arthroplasty for primary osteoarthritis in patients aged 55 years and older. Acta Orthop 2010; 81 (1): 42–52.
- Mäkinen T J, Koort J K, Mattila K T, Aro H T. Precision measurements of the RSA method using a phantom model of hip prosthesis. J Biomech 2004; 37 (4): 487–93.
- Mäkinen T J, Alm J J, Laine H, Svedström E, Aro H T. The incidence of osteopenia and osteoporosis in women with hip osteoarthritis scheduled for cementless total joint replacement. Bone 2007; 40 (4): 1041–7.
- Nourissat C, Essig J, Asencio G. The cementless anatomic Benoist Girard (ABG) II total hip arthroplasty: a minimum 8-year follow-up study. J Arthroplasty 2013; 28 (4): 707–11.
- Nich C, Takakubo Y, Pajarinen J, Ainola M, Salem A, Sillat T, Rao A J, Raska M, Tamaki Y, Takagi M, Konttinen Y T, Goodman S B, Gallo J. Macrophages-key cells in the response to wear debris from joint replacements. J Biomed Mater Res A 2013; 101 (10): 3033–45.
- Önsten I, Bengner U, Besjakov J. Socket migration after charnley arthroplasty in rheumatoid arthritis and osteoarthritis. A roentgen stereophotogrammetric study. J Bone Joint Surg Br 1993; 75 (5): 677–80.
- Önsten I, Carlsson A S, Sanzen L, Besjakov J. Migration and wear of a hydroxyapatite-coated hip prosthesis. A controlled roentgen stereophotogrammetric study. J Bone Joint Surg Br 1996; 78 (1): 85–91.
- Pakvis D, Luites J, van Hellemondt G, Spruit M. A cementless, elastic press-fit socket with and without screws. Acta Orthop 2012; 83 (5): 481–7.
- Park K S, Seon J K, Yoon T R. The survival analysis in third-generation ceramic-on-ceramic total hip arthroplasty. J Arthroplasty 2015 May 19. [Epub ahead of print]
- Pijls B G, Nieuwenhuijse M J, Fiocco M, Plevier J W, Middeldorp S, Nelissen R G, Valstar E R. Early proximal migration of cups is associated with late revision in THA: A systematic review and meta-analysis of 26 RSA studies and 49 survivalstudies. Acta Orthop 2012; 83 (6): 583–91.
- Rohrl S M, Nivbrant B, Snorrason F, Kärrholm J, Nilsson K G. Porous-coated cups fixed with screws: A 12-year clinical and radiostereometric follow-up study of 50 hips. Acta Orthop 2006; 77 (3): 393–401.
- Saari T M, Digas G, Karrholm J N. Risedronate does not enhance fixation or BMD in revision cups: Randomised study with three years follow-up. Hip Int 2014; 24 (1): 49–55.
- Snorrason F, Kärrholm J, Holmgren C. Fixation of cemented acetabular prostheses. the influence of preoperative diagnosis. J Arthroplasty 1993; 8 (1): 83–90.
- Soballe K, Hansen E S, Brockstedt-Rasmussen H, Hjortdal V E, Juhl G I, Pedersen C M, Hvid I, Bunger C. Fixation of titanium and hydroxyapatite-coated implants in arthritic osteopenic bone. J Arthroplasty 1991; 6 (4): 307–16.
- Spotorno L, Grappiolo G, Mumenthaler A. The CLS system. Conception and evolution of an idea. In: Morscher E W (ed). Endoprosthesis, Springer-Verlag Berlin Heidelberg 1995; 271–96.
- Thanner J, Kärrholm J, Herberts P, Malchau H. Hydroxyapatite and tricalcium phosphate-coated cups with and without screw fixation: A randomized study of 64 hips. J Arthroplasty 2000; 15 (4): 405–12.
- Valstar E R, Gill R, Ryd L, Flivik G, Borlin N, Kärrholm J. Guidelines for standardization of radiostereometry (RSA) of implants. Acta Orthop 2005; 76 (4): 563–72.
- Wilkinson J M, Stockley I, Peel N F, Hamer A J, Elson R A, Barrington N A, Eastell R. Effect of pamidronate in preventing local bone loss after total hip arthroplasty: A randomized, double-blind, controlled trial. J Bone Miner Res 2001; 16 (3): 556–64.
- Zhou Z K, Li M G, Borlin N, Wood D J, Nivbrant B. No increased migration in cups with ceramic-on-ceramic bearing: An RSA study. Clin Orthop Relat Res 2006; 448: 39–45.
