Abstract
We described the novel use of intravascular ultrasound-virtual histology (IVUS-VH) imaging in two young adult male patients who presented with acute inferior ST-elevation myocardial infarction (STEMI) and we highlight the usefulness of this new invasive coronary imaging technique. Both patients had thrombotic occlusion of the right coronary arteries but the underlying pathophysiological mechanisms leading to acute thrombosis were different. The in vivo information obtained by IVUS-VH imaging was invaluable in pinpointing the likely etiology of STEMI and thus, guided our primary percutaneous coronary intervention strategy appropriately.
Keywords::
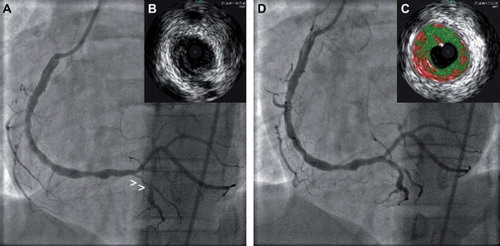
A 20 year old previously healthy male who is a chronic smoker presented with exertional chest pain. Electrocardiogram (ECG) showed ST elevation in the inferior leads. Emergency coronary angiography showed thrombotic occlusion in the mid right coronary artery (RCA). The left anterior descending and left circumflex arteries were normal. Primary percutaneous coronary intervention (PPCI) of RCA was initiated by performing manual aspiration thrombectomy. Flow was restored in RCA () revealing diffuse atherosclerosis along the whole vessel with significant stenoses in distal RCA and posterior descending artery (PDA). Intravascular ultrasound-virtual histology (IVUS-VH) imaging revealed plaque rupture () at proximal segment of PDA with presence of large amount of necrotic core () along the mid-distal RCA. We decided to treat the proximal PDA lesion by plain old balloon angioplasty (POBA) and the stenosis was reduced to 30% () with restoration of thrombolysis in myocardial infarction (TIMI) 3 flow. No coronary stenting was performed as the angiographic results were acceptable. Following PCI, he was treated with intravenous eptifibatide infusion for 18 h and remained stable. Several investigations were performed to look for secondary causes of the ST elevation myocardial infarction (STEMI) as he was relatively young. His lipid and blood sugar profiles were within normal limits. Echocardiogram did not show any evidence of intracardiac thrombus/shunt. Thrombophilia screen which included anti-thrombin, protein C deficiency, protein S deficiency and autoimmune markers were all negative. He was strongly advised to cease smoking as this was likely the primary cause of his premature presentation of STEMI.
Figure 1. (A) Coronary angiography showing diffuse atherosclerosis in RCA with site of plaque rupture denoted by small arrowheads (>). (B) Grey-scale IVUS showing plaque rupture at proximal PDA (inset). (C) VH assessment of mid-distal RCA showing large amount of necrotic core (inset). (D) Coronary angiography of RCA after POBA of PDA.
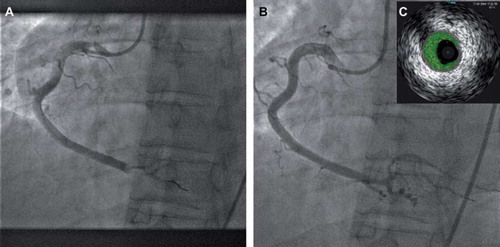
A 42 year old previously healthy male, a non-smoker presented with acute onset of chest pain. ECG showed ST elevation over the inferior leads. Emergency coronary angiography showed single vessel disease with thrombotic occlusion in the distal segment of a large caliber RCA (). After successful wiring of RCA, manual aspiration thrombectomy was performed. Huge amount of blood clots was successfully aspirated resulting in restoration of TIMI 3 flow and normalization of the inferior ST segments. The distal RCA looked relatively normal by subsequent angiography () with no obvious vessel narrowing. IVUS-VH imaging () showed no evidence of plaque rupture but there was some residual thrombus. He was treated conservatively with heparin and intravenous eptifibatide infusion. Just like the former case, several investigations were performed to rule out secondary causes of STEMI. Subsequent thrombophilia screen confirmed he had protein S deficiency and he was started on long term anti-coagulation.
Figure 2. (A) Coronary angiography showing thrombotic occlusion in distal RCA, (B) Coronary angiography of RCA after aspiration thrombectomy. (C) VH assessment of distal RCA showing presence of thrombus with minimal necrotic core (inset).
PPCI is the preferred reperfusion therapy for STEMI. Over the past decade, there have been several pivotal advances in devices, procedural techniques and adjunctive antithrombotic therapy in the revascularization strategies for PPCI. Although studies (Citation1) have shown lower rate of restenosis and stent thrombosis with IVUS guided PCI, limited data (Citation2,Citation3) exists on its use in PPCI. IVUS-VH (Citation4) is a new invasive intracoronary imaging technique that is able to characterize different tissue components in coronary plaques. Tissue characterization is performed by means of radiofrequency data analysis, which classifies them into four major components (fibrous, fibro-fatty, necrotic core and dense calcium). It is especially useful in identifying thin-capped fibroatheroma (TCFA) i.e. vulnerable coronary plaque lesion. Histopathological studies have shown that TCFA is the main precursor lesion for plaque rupture in STEMI. It is characterized by a necrotic core with an overlying thin fibrous cap and it contains numerous macrophages.
From the 2 cases, we demonstrated the usefulness of IVUS-VH imaging as an adjunctive tool in PPCI especially in young STEMI patients. Possible etiologies of STEMI in young adults (Citation5) (aged less than 45 years old) include coronary atherosclerosis (which predisposes to plaque rupture), hypercoagulable state, coronary artery spasm, coronary vasculitis, spontaneous coronary artery dissection and STEMI related to substance abuse. By ‘peeking’ inside the infarct-related artery, IVUS-VH imaging gave us a better understanding of the underlying pathophysiological mechanisms of STEMI in both our patients. For the first patient, we could confidently attribute the cause to be secondary to atherosclerotic plaque rupture. As for the latter, the IVUS-VH images mainly showed thrombus with no features of plaque rupture. This was suggestive of other pro-thrombotic mechanism at work. The in-vivo information obtained was invaluable to our decision-making for the appropriate revascularization strategy during PPCI. The former was successfully treated with POBA whereas the latter was successfully treated with manual aspiration thrombectomy. It would be potentially catastrophic if we were to stent the RCA in the latter as he had coagulation disorder which could predispose to stent thrombosis. Both patients had uneventful hospital course and remained asymptomatic at five and eight months follow-up. We believe IVUS-VH imaging can play an important adjunctive role in PPCI especially in young STEMI patients. It can provide important clues to the possible underlying etiology and guide our PPCI strategy appropriately. Further studies are needed to validate its use in this subgroup of patients.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Parise H, Maehara A, Stone GW, Leon MB, Mintz GS. Meta-analysis of randomized studies comparing intravascular ultrasound versus angiographic guidance of percutaneous coronary intervention in pre-drug-eluting stent era. Am J Cardiol. 2011;107:374–82.
- Maluenda G, Lemesle G, Ben-Dor I, Collins SD, Syed AI, Torguson R, . Impact of intravascular ultrasound guidance in patients with acute myocardial infarction undergoing percutaneous coronary intervention. Catheter Cardiovasc Interv. 2010;75:86–92.
- Murray SW, Stables RH, Palmer ND. Virtual histology imaging in acute coronary syndromes: Useful or just a research tool? J Invasive Cardiol. 2010;22:84–91.
- Garcia-Garcia HM, Gonzalo N, Regar E, Serruys PW. Virtual histology and optical coherence tomography: From research to a broad clinical application. Heart 2009;95:1362–74.
- Cengel A, Tanindi A. Myocardial infarction in the young. J Postgrad Med. 2009;55:305–13.