Abstract
Massive pulmonary embolism poses a therapeutic challenge, especially when thrombolytics are controversial. We describe the complicated course of an exceptional case of massive pulmonary embolism exhibiting paradoxic embolization with a thrombus lodged in the foramen ovale. Thrombolysis was considered contraindicated and surgical intervention was performed. Postoperatively, persistent pulmonary hypertension and impending right ventricular (RV) failure necessitated the initiation of extracorporeal life support (ELS), accompanied by therapeutic heparinization, inhaled nitric oxide, levosimendan and sildenafil. On day 8, the patient was successfully weaned from ELS with excellent neurological recovery and virtual normalization of RV pressures and dimensions. (Contra-) indications for thrombolysis and surgical embolectomy are reviewed. The intriguing role of ELS in conjunction with therapeutic heparinization and pharmacological unloading of the right-sided vasculature and the RV is discussed.
Massive pulmonary embolism (PE) poses a therapeutic challenge (1,2). Especially in sub-acute presentation and paradoxic embolization, thrombolytics are controversial. Yet, the ultimate success of surgical embolectomy may be limited by persistent pulmonary hypertension and right ventricular (RV) failure.
A 52-year old female presented with a three-week history of dyspnea and a transient ischemic attack (TIA). Following syncope during exercise testing, the EKG showed signs of RV overload (). Echocardiography (echo) revealed RV dilation (), elevated pressures and a thrombus (arrow) lodged in the foramen ovale ( and ; intra-atrial septum (circle), mitral valve (MV), aorta (AO), left- (LA) and right atrium (RA)). CT-scanning confirmed massive PE ().
Figure 1. EKG on admission showing electrocardiographic signs of right-ventricular overload, i.e. vertical-to-right axis, right bundle branch block.
Figure 2. Transthoracic echocardiographic 4-chamber view showing an enlarged right ventricle (RV), right atrium (RA) and a thrombus (arrow) crossing the interatrial septum.
Figure 3. Transesophageal echocardiographic short-axis view showing the right atrium (RA), left atrium (LA), aorta (AO) and thrombus through the foramen ovale (arrow).
Figure 4. Transesophageal 3-dimensional echocardiographic view through the roof of the left-(LA) and right atrium (RA) looking down on the mitral valve (MV) and the thrombus (arrow).
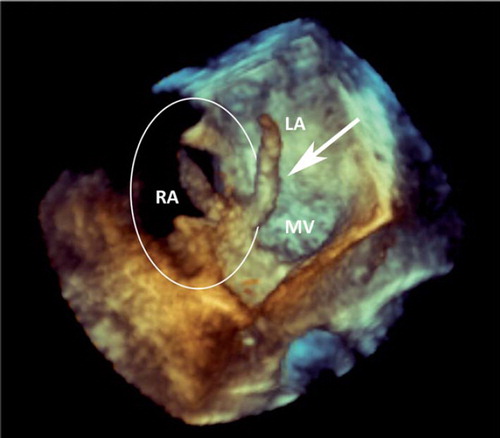
Figure 5. Contrast-enhanced CT scans of the chest showing adjacent slices with bilateral thrombi (arrows).
This high-risk scenario warrants an aggressive approach considering thrombolysis as a therapeutic mainstay (Citation1). If the latter is contraindicated surgical embolectomy should be performed, while catheter-based techniques are reserved for patients unsuitable for either thrombolysis or surgery (Citation1). In this case, thrombolysis was considered contraindicated due to the risk of immediate thrombus disintegration and subsequent systemic embolization. A recent TIA forms a relative contraindication for thrombolysis. However, considering the sub-acute history and the large LA thrombus, silent strokes may have occurred carrying the risk of hemorrhagic conversion (Citation1). Moreover, recent literature on surgical embolectomy reports improved outcome and challenges the prominent role of thrombolysis by proposing to expand potential indications to hemodynamic stability with RV dysfunction and large thrombus load (Citation2). After weighing the abovementioned considerations, the clinical presentation and large partially left-sided intracardiac thrombus, surgical intervention was performed.
Thrombectomy, closure of the foramen ovale and pulmonary embolectomy were postoperatively complicated by persistent pulmonary hypertension and impending RV failure. Thus, extracorporeal life support (ELS), i.e. peripheral veno-arterial extracorporeal membrane oxygenation was initiated, accompanied by therapeutic heparinization, inhaled nitric oxide, levosimendan, and sildenafil. ELS was gradually reduced using an extracorporeal arterio-venous bridge under echocardiographic and invasive monitoring. Weaning from ELS was accomplished on day eight and hospital discharge on day 26, with excellent neurological recovery and virtual normalization of RV pressures and dimensions. Surgical thrombo-embolectomy is a therapeutic option for complex cases of massive PE, yet, aggressive unloading of the RV by combined measures of mechanical circulatory support and medical therapy should be considered postoperatively awaiting RV adaptation and diminution of pulmonary vascular resistance. In this sense, it is tempting to speculate whether prolonged ELS in conjunction with pharmacological RV unloading and therapeutic heparinization alone would allow to circumvent surgical embolectomy in selected patients, e.g. in those with significant RV dysfunction and hemodynamic stability. This notion is supported by the finding that heparin results in a residual pulmonary vascular resistance, RV function and dimension comparable to thrombolysis seven days after the onset of therapy (Citation1).
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Meneveau N. Therapy for acute high-risk pulmonary embolism: Thrombolytic. Cur Opin Cardiol. 2010;25:560–7.
- Samoukovic G, Malas T, deVarennes B. The role of pulmonary embolectomy in the treatment of acute embolism: A literature review from 1968 to 2008. Interact Cardiovasc Thorac Surg. 2010;11:265–70.