Abstract
The circulatory assistance, mainly the extra-corporeal membrane oxygenation (ECMO) restores hemodynamics and serves to limit the myocardial work, in order to avoid left ventricular dilation, high end-diastolic pressures, increased wall stress, subendocardial ischemia and consequently worsening pulmonary congestion and edema. In patients with large myocardial damage, sometimes an additional unloading of the left ventricle is warranted. We report a case of percutaneous blade and balloon atrial septostomy (BAS) as an add-on to the circulatory assistance to unload the left heart in a cardiogenic shock related to H1N1 infection.
Keywords::
Introduction
The prevalence of influenza-associated myocarditis remains unknown because of a lack of comprehensive screening, with only a handful of clinical cases and autopsy findings reported in the literature (Citation1). Whether such an association holds for the novel influenza A strain, pandemic-2009-H1N1, remains unclear. Some authors (Citation2) claimed that potentially reversible cardiac dysfunction is a relatively common complication associated with hospitalized pandemic-2009-H1N1 influenza. We report a case of cardiogenic shock related to H1N1 infection with the subsequent management of the heart unload.
Case
A 47 year-old woman, with a history of Hodgkin's lymphoma treated by radiotherapy and right breast ductal carcinoma treated by ablative surgery and adjuvant anthracyclines (5-fluorouracil and cyclophosphamide) five years ago with no subsequent repercussion on the left ventricle function during routine cardiac ultrasound follow-up, was addressed from another hospital to our department for symptoms of left heart failure. Four weeks before admission, she had experienced fever, cough and shortness of breath that was treated by oral antibiotics (cefpodoxime) for five days without net clinical improvement. The thoracic CT-scan that was done in the other hospital overviewed a compressed bilateral pleural effusion that was diagnosed as a transudate on biochemical analysis. On admission in our department, her electrocardiogram showed diffuse T-wave inversion. The laboratory investigations revealed normal WBC (5700/ml) and high CRP (134mg/l). Approximately one hour later and during the cardiac ultrasound that highlighted a severe myocardial dysfunction (the left ventricular ejection fraction (LVEF) at 15%), she experienced clinical aggravation as manifested by acute cardiogenic shock, neurological deterioration and electro-mechanical dissociation that required cardiopulmonary resuscitation with external cardiac massage and mechanical ventilation. In front of the severe abnormal contraction and the hemodynamic instability despite full inotropic support using vasoactive drugs and primary noradrenaline, she was immediately assisted by the cardiovascular surgical team with a peripheral venoarterial ECMO.
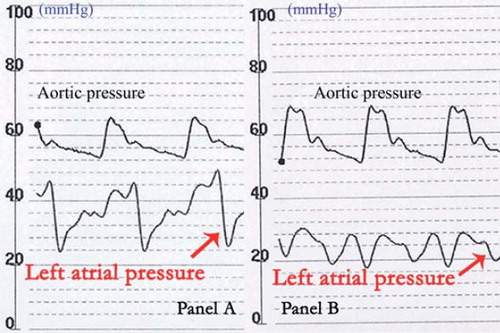
The coronary angiography that was done few hours later to eliminate coronary disease at the origin of her cardiac arrest did not show any significant stenosis that might explain her symptoms, and the right heart catheterization showed a stagnation of iodine contrast in the trunk of the pulmonary artery and its branches (, arrows) revealing high left ventricle filling pressures and suggesting that the ECMO was insufficient to unload the left heart. We performed blade and balloon atrial septostomy (BAS) () creating an atrial septal defect (ASD) with left to right shunt to manage the severe and refractory acute lung edema. The left ventricular unload assumed by the ASD was immediately efficacious on the pulmonary edema, and the mean left atrium pressure declined significantly (from 37 to 25 mmHg) (). Indeed, the adequacy of BAS was assessed by a better ECMO output. Two days later, she presented a sinusitis with purulent rhinorrhea, and the polymerase chain reaction (PCR) highlighted (H1N1) influenza A virus. She was treated with oseltamivir. The purulent collections of the maxillary sinuses secondarily required a surgical drainage. The H1N1virus PCR became negative at day seven. The hemodynamics allowed the ECMO ablation at day six with no aggravation of right heart symptoms and the weaning from mechanical ventilation was possible at day nine. Upon awakening, there was no neurologic disorder and the severe cardiac dysfunction persisted. A classic treatment of heart failure was progressively initiated based on beta-blockers and angiotensin converting enzyme-inhibitors. The evolution was marked by a progressive amelioration of the heart function and the patient was discharged and remained asymptomatic. The echocardiographic assessment showed a remarkable improvement of the cardiac function (LVEF at 57%) with a non-significant residual intertribal shunt.
Discussion
In patients with cardiogenic shock or cardiac refractory cardiac arrest, the extra-corporeal life support (ECLS) plays a pivotal role to restore hemodynamics and to generate a temporary circulatory support using veno-arterial pumping through heart-lung machine in order to maintain organ perfusion (Citation3). Various techniques to unload the left ventricle have been reported: surgically, by placing a draining catheter into the left atrium via a mini-thoracotomy; and percutaneously with catheter based assist devices such the Impella (Abiomed, Danvers, Massachusetts, USA) micro-axial blood pump or the Tandem Heart (Cardiac Assist Inc., Pittsburgh, Pennsylvania, USA). These techniques are highly invasive with an increasing risk of infections, bleeding, or hemolysis and the risks of device displacement, valvular and endovascular trauma (dissection, distal embolization). So, they are not recommended in cases of mechanical aortic valve or significant aortic valvular disease or peripheral artery disease. BAS that was mainly described to treat primary pulmonary hypertension for congenital heart disease is an elegant alternative technique to unload the left heart. It can be achieved quickly in such ‘heavy’ patients without the risk of arterial or aortic valve damage. The potential complications of this technique that requires transseptal catheter based experience include needle perforation (left atrium wall, pulmonary vein), pericardial effusion or tamponade, hypotension and ventricular fibrillation. In our case, the ECMO was found inadequate to unload the left ventricle what appeared by the iodine contrast stagnation in the pulmonary trunk and by the low ECMO output. So, we choose BAS to unload the left ventricle and the efficacy was immediately overviewed on the pulmonary edema and the left atrium pressure allowing a relatively safe bridging to recovery. We previously reported two cases of BAS (Citation4,Citation5) as a bridge to heart transplant, and we wanted to emphasize with our present case the role of BAS as an advisable technique to supplement circulatory assistance as a bridge to recovery. Note that there was no need to perform ASD closure, but if necessary, this can be performed percutaneously.
Notice of correction
Changes have been made to an author name since the original online publication date of 2/20/2013.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the contents and writing of the paper.
References
- Mamas MA, Fraser D, Neyses L. Cardiovascular manifestations associated with influenza virus infection. Int J Cardiol. 2008;130:304–9.
- Martin SS, Hollingsworth CL, Norfolk SG, Wolfe CR, Hollingsworth JW. Reversible cardiac dysfunction associated with pandemic-2009-H1N1 influenza A. Chest 2010;137:1195–7.
- Massetti M, Tasle M, Le Page O, Deredec R, Babatasi G, Buklas D, . Back from irreversibility: Extracorporeal life support for prolonged cardiac arrest. Ann Thorac Surg. 2005;79:178–84.
- Dahdouh Z, Roule V, Lognoné T, Sabatier R, Grollier G. Percutaneous blade and balloon atrioseptostomy as a supplement to extracorporeal membrane oxygenation as a bridge to heart transplantation. Cardiovasc Revasc Med. 2012;13:69–71.
- Dahdouh Z, Roule V, Sabatier R, Lognoné T, Labombarda F, Pellissier A, . Extra-corporeal life support, transradial thrombus aspiration and stenting, percutaneous blade and balloon atrioseptostomy, all as a bridge to heart transplantation to save one life. Cardiovasc Revasc Med. 2012;13:241–5.