Abstract
Radial artery spasm is one of the most commonly encountered problems during transradial interventions with a reported incidence in the range of 6–10%. Balloon-assisted tracking (BAT) of guide catheter has recently been described as a novel technique to overcome difficult radial artery anatomies including tortuosity, loops and spasm. In this report, we describe the successful use of BAT in a patient with radial artery spasm during primary angioplasty.
Keywords::
Introduction
Transradial coronary catheterization has been associated with reduced access site bleeding complications, mortality and healthcare costs (Citation1). The transradial approach has now become the primary access site for many operators and its safety and efficacy has been proven in various procedures including primary percutaneous intervention, complex bifurcation lesions, left main angioplasty and recanalization of chronic total occlusions (Citation2–4).
Radial artery spasm remains one of the major limitations of transradial interventions with a reported incidence in the range of 6–10% and represents the most common cause of access site crossover (Citation5–6). Several factors have been associated with its occurrence including small radial artery diameter and tortuosity, large sheath diameter, multiple catheter exchanges, low body mass index, female gender and diabetes mellitus (Citation7). Intra-arterial administration of antispastic agents such as non-dihydropyridine calcium channel blockers (diltiazem, verapamil) and isosorbide dinitrate (ISDN), and adequate sedation has been shown to significantly reduce the incidence of radial spasm (Citation8). Despite prophylactic treatment, radial artery spasm can still occur and prevent successful completion of the transradial procedure. In this case report, we describe the utilization of the recently described balloon-assisted tracking (BAT) technique to overcome severe radial artery spasm in a young female patient undergoing primary percutaneous intervention for acute myocardial infarction.
Case
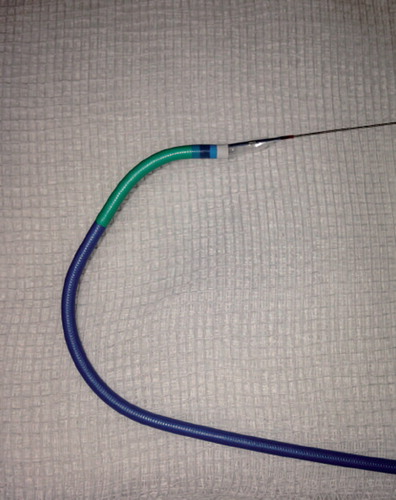
A 34-year-old woman with a background of cutaneous lupus and chronic tobacco use was transferred to our institution after being resuscitated from an out-of-hospital VF arrest. Her ECG showed anterior ST elevation. Emergency coronary angiography via the right radial artery (RRA) demonstrated an occluded proximal left anterior descending artery (LAD) (). Due to RRA spasm during exchange of the diagnostic catheters, a 5Fr JL3.5 guiding catheter was used for LAD intervention. The occlusion was successfully crossed with a BMW guidewire (Abbott Vascular, USA) and the lesion was pre-dilated with a 2.5x15 mm balloon with restoration of TIMI III flow. During unsuccessful manipulations that failed to advance a 3.5 × 18 mm everolimus-eluting bioresorbable scaffold (ABSORB; Abbott Vascular, Santa Clara, CA, USA) the guiding catheter and wire positions were lost. Attempts to exchange for a 6Fr JL3.5 guiding catheter were unsuccessful due to severe RRA spasm which was not responding to high doses of intra-arterial vasodilators (verapamil and ISDN) and intravenous benzodiazepines (). A new 0.014 inch BMW guidewire was advanced into the ascending aorta and a 2.0 × 15 mm balloon, which partially protruded from the distal end of the guide catheter, was inflated at 4 atm proximally to the site of the radial spasm. This allowed smooth advancement of the 6Fr guide into the ascending aorta where the 0.014 inch guidewire was exchanged for the standard 0.035 inch guidewire and the left coronary artery was successfully engaged (). LAD was re-wired and intervention was completed with deployment of the 3.5 × 18 mm ABSORB stent ().
Discussion
During the BAT technique, the conical shape of the partially protruding coated balloon at the tip of the guide catheter provides a smooth surface that can be advanced through the site of the radial spasm in a non-traumatic fashion, compared to the ‘razor effect’ that is produced when a non-covered catheter tip is advanced against resistance () (Citation9). For 5Fr diagnostic or guiding catheters a 1.5-mm balloon is recommended, while for 6Fr a 2.0 mm balloon is commonly preferred. Inflation of the balloon at low pressure (2–4 atm) keeps the balloon more flexible and can be used to overcome obstructions or tortuosities, while inflation at medium pressure (6 atm) allows better pushability against severe radial spasm or small arteries (Citation10). Patel et al. reported the successful use of the BAT technique in 60 patients with difficult anatomy including radial and subclavian loops or tortuosities, small radial artery diameter and radial spasm (Citation11). Although no complications have yet been reported with this technique, the use of BAT should be avoided in radial arteries with diameter less than 1.25 mm in view of the risk of perforation (Citation12).
Conclusion
Radial spasm represents the commonest cause of procedural failure during radial catheterisation. BAT is an extremely useful and easy-to-use technique that can increase the success rates and prevent endothelial damage.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Feldman DN, Swaminathan RV, Kaltenbach LA, Baklanov DV, Kim LK, Wong SC, et al. Adoption of radial access and comparison of outcomes to femoral access in percutaneous coronary intervention: An updated report from the national cardiovascular data registry (2007–2012). Circulation 2013;127:2295–306.
- Rathore S, Hakeem A, Pauriah M, Roberts E, Beaumont A, Morris JL. A comparison of the transradial and the transfemoral approach in chronic total occlusion percutaneous coronary intervention. Catheter Cardiovasc Interv. 2009;73:883–7.
- Amoroso G, Kiemeneij F. Transradial access for primary percutaneous coronary intervention: The next standard of care? Heart 2010;96:1341–4.
- Yang Y, Kandzari D, Gao Z, Xu B, Chen JL, Qiao SB, et al. Transradial versus transfemoral method of percutaneous coronary revascularization for unprotected left main coronary artery disease: Comparison of procedural and late-term outcomes. JACC Cardiovasc Interv. 2010;3:1035–42.
- Kristić I, Lukenda J. Radial artery spasm during transradial coronary procedures. J Invasive Cardiol. 2011;23:527–31.
- Ratib K, Chong AY, Routledge H, Nolan J. Spasm and occlusion in contemporary radial practice. JACC Cardiovasc Interv. 2010;3:885–6.
- Varenne O, Jégou A, Cohen R, Empana JP, Salengro E, Ohanessian A, et al. Prevention of arterial spasm during percutaneous coronary interventions through radial artery: The SPASM study. Catheter Cardiovasc Interv. 2006;68:231–5.
- Rosencher J, Chaïb A, Barbou F, Arnould MA, Huber A, Salengro E, et al. How to limit radial artery spasm during percutaneous coronary interventions: The spasmolytic agents to avoid spasm during transradial percutaneous coronary interventions (SPASM3) study. Catheter Cardiovasc Interv. 2014;84:766–71.
- Deora S, Shah S, Patel T. Balloon-assisted tracking in dealing with radial artery loop by transradial approach: A technical report. J Invasive Cardiol. 2014;26:E61–2.
- Patel T, Shah S, Pancholy S. Balloon-assisted tracking of a guide catheter through difficult radial anatomy: A technical report. Catheter Cardiovasc Interv. 2013;81:E215–8.
- Patel T, Shah S, Pancholy S, Rao S, Bertrand OF, Kwan T. Balloon-assisted tracking: A must-know technique to overcome difficult anatomy during transradial approach. Catheter Cardiovasc Interv. 2014;83:211–20.
- Verouden NJ, Kiemeneij F. Balloon-assisted tracking to overcome radial spasm during transradial coronary angiography: A case report. Case Rep Cardiol. 2014;2014:214310.