Abstract
Background:
Cardiovascular diseases are among the leading causes of death worldwide and studies have found a direct relationship between levels of low-density lipoprotein cholesterol and coronary heart disease. Statins are the most commonly prescribed medications to lower cholesterol, a major controllable risk factor for coronary heart disease.
Objective:
This study aims to find what factors in the first year of statin therapy are predictive of long-term all-cause mortality.
Methods:
Data for this retrospective cohort study were collected on patients identified as new statin users between December 1, 2006 and November 30, 2007 at five Veterans Affairs Healthcare Systems from Southern California and Nevada. Multiple independent variables were assessed utilizing a logistic regression model assessing for all cause mortality at 6 years follow-up. The independent variables included race, age, ethnicity, body mass index, socioeconomic status, and baseline comorbidities. Secondary analysis analyzed high-density lipoprotein levels, adherence, total cholesterol, and triglycerides.
Results:
Increased age, increased medication count, hypertension, diabetes, tobacco use, chronic obstructive pulmonary disease, and congestive heart failure were all associated with an increased risk of mortality. Hispanic ethnicity, Asian race, and increased body mass index were associated with decreased risk of mortality. There were no significant associations between mortality and race, LDL outcomes at 1 year, or annual income level.
Conclusion:
There is clear evidence that statin use is associated with decreased events in cardiovascular disease and total mortality. This study found multiple independent variables as predictors of mortality in new start statin users after a 6 year follow-up, but differences in lipid groups after 1 year were not predictive of long-term mortality in the cohort studied.
Keywords: :
Introduction
Cardiovascular diseases are among the leading causes of death worldwide, with more than 2150 deaths each dayCitation1,Citation2. Many studies have found a direct relationship between levels of low-density lipoprotein (LDL) cholesterol (or total cholesterol) and the rate of new-onset coronary heart disease (CHD) in men and women who were initially free of CHDCitation3,Citation4. When other risk factors are present, including diabetes and hypertension, this risk increases even more. This has led to large numbers of clinical trials providing strong evidence that CHD incidence is reduced in cholesterol-lowering therapy. A meta-analysis involving 10 trials of 79,494 subjects found that statins reduce coronary events, strokes, and all-cause mortality without increasing non-coronary mortalityCitation5.
Statins are the most commonly prescribed medications to lower cholesterol. High cholesterol is one of the major controllable risk factors for coronary heart disease, heart attack, and stroke, consequently increasing the use of statins throughout the yearsCitation6. It is evident that statin use has a clear benefit on stroke and total mortality by greatly reducing cholesterol. Despite the positive results linking statin use and reduction in CHD, studies have shown poor adherence to these medicationsCitation7. A systematic review and meta-analysis of 22 cohorts determined several sociodemographic, medical, and healthcare utilization characteristics were associated with statin non-adherenceCitation8. These factors are useful guides for targeting statin adherence interventions, especially since adherence is an essential factor to receiving the full benefits of these medications.
Although there have been studies identifying predictors of adherence and non-adherence to statins, there is less evidence identifying reliable predictive variables of mortality among new statin users. In particular, the Veteran population is of importance due to the prevalence of risk factors within this group. Over 90% are male and more than 40% are over 65 years of age, both of which are risk factors of CHD-related deathsCitation9. This study aims to identify variables in the first year of statin therapy that are predictive of long-term mortality.
Methods
This retrospective cohort study used data from the Veterans Affairs facilities within the Veterans Integrated Service Network 22, including sites from Loma Linda, Long Beach, Los Angeles, San Diego, and Las Vegas. Data were collected on study subjects identified as new statin users between December 1, 2006, and November 30, 2007.
Socioeconomic status was determined by zip code median household income and divided into five quintiles from lowest to highest income. Adherence rates were defined as medication possession ratio (MPR) >0.8. MPR was calculated as the number of days of statin drug supply the patient filled divided by the number of days in the specific time period.
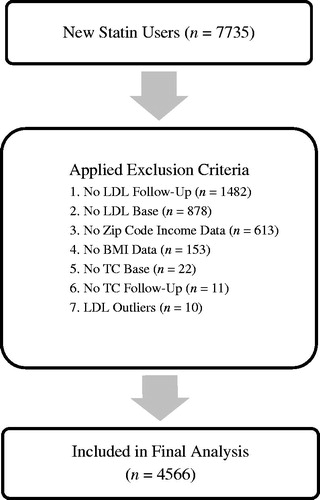
Inclusion criteria included age 18 years or older, diagnosis of dyslipidemia, new statin user per the dates listed above, enrollment in the VA system for at least 2 years before the study period, and eligibility to receive prescription benefits from the VA. Patients were excluded if they had missing baseline or follow-up body mass index (BMI), LDL, and total cholesterol (TC) laboratory data, or if they were missing zip code income data ().
Statistical analysis
Baseline comparisons between the mortality group and the survival group were performed using t-test and chi-square test. The primary outcome measure of mortality predictors at 6 years follow-up for new statin users were analyzed using a logistic regression model. The independent variables assessed included race, age, ethnicity, BMI, socioeconomic status, LDL outcomes at 1 year, and baseline comorbidities. Data are reported including odds ratios with 95% confidence interval and p-values. All analyses were performed using SPSS version 18 (SPSS Inc, Chicago, IL).
Results
Study population
There were a total of 7735 patients who met inclusion criteria, and 4566 patients were included in the final analysis after applying the exclusion criteria. Patients in the mortality group were older (p < 0.001), on more medications (p < 0.001), had higher total cholesterol levels (p ≤ 0.001) and had higher incidence of hypertension (p < 0.001), vascular disease (p < 0.001), chronic obstructive pulmonary disease (p = 0.001), congestive heart failure (p < 0.001), history of myocardial infarction (p < 0.001), and angina (p = 0.008). Patients in the survival group were more likely to be Hispanic (p < 0.001), with higher BMI (p < 0.001) and LDL cholesterol (p < 0.001) ().
Independent variables
Age, medication count, ethnicity, and BMI were predictors of long-term mortality. In addition, patients with comorbidities such as hypertension (OR = 1.46, 95% CI = 1.08–1.98, p = 0.015), diabetes (OR = 1.36, 95% CI = 1.07–1.72, p = 0.012), tobacco use (OR = 1.52, 95% CI = 1.16–1.99, p = 0.002), COPD (OR = 1.88, 95% CI = 1.40–2.53, p ≤ 0.001), and congestive heart failure (OR = 1.80, 95% CI = 1.23–2.63, p = 0.002) all showed an increased risk of mortality. There were no significant associations between mortality and race, LDL outcomes at 1 year, and annual income level, as shown in .
Table 1. Baseline demographics.
Table 2. Odds ratios of mortality via logistic regression.
Discussion
This study showed that different lipid outcomes after the first year of statin therapy were not indicative of long-term mortality. Other significant predictors of mortality in new start statin users were seen after a 6 year follow-up period. Age, race, number of medications, comorbidities, and BMI were shown to be predictive of long-term mortality in a veteran population, much of which was expected. These factors are all independent predictors of death. Statin users in the mortality groups were more likely to be taking more medications, an indicator of their underlying diseases, also predictive of mortality.
Previous studies have shown a highly significant negative association between statin use and mortalityCitation10,Citation11. In an overview of 16 individual trials including 29,000 subjects, patients assigned to statin drugs experienced significant reductions in risks of stroke and total mortalityCitation12. The benefit of statin use is clearly evident. However, the results of our study showed that actual differences in LDL levels at a given point in time among statin users appeared to confer no predictive effect on long-term mortality outcomes. Patient stratification between high potent (rosuvastatin and atorvastatin) vs non-potent statins did not affect the outcome. Sub-groups including HDL, TG, and TC further showed no predictive value of long-term mortality. Statin doses and whether the treatment goal of LDL was attained at 1 year follow-up were not assessed in this study.
The study by Blackburn et al.Citation13 reported a detectable excess of cardiovascular morbidity associated with non-adherence to statin therapy. Numerous other studies have shown that a reduction in LDL is associated with a decreased risk in cardiovascular events and total mortality. These findings suggest that occurrences of cardiovascular events can be prevented with improvements in maintaining adherence in statin users. Although our analysis showed no significant difference in adherence as a predictor of long-term mortality, it should be mentioned that cardiovascular outcomes were not assessed. In addition, LDL values in both survival and mortality groups suggest uncontrolled LDL levels at 1 year follow-up, which may be due to the low adherence rates to statin therapy in both groups. Therefore, risk factors for cardiovascular events and total mortality including male gender, older age, vascular disease, COPD, hypertension, and diabetes took the lead in the risk factor evaluation in the multiple regression analysis, despite the great differences in their baseline rates.
Several limitations should be considered for this study. Timing of cardiovascular events or mortality was not assessed. In addition, some degree of time immortal bias may be present because no patient’s died in the first year (as per inclusion criteria requiring LDL outcomes at 1 year). In addition, follow-up LDL outcomes were performed after 1 year only, extrapolation of values beyond that time point are not possible. The study was performed in a veteran population primarily comprised of male patients, limiting generalizability of the analysis. Although this group is of particular interest when looking at the risk factors associated with coronary heart disease, associations between lipid variables and mortality in a broader patient population may vary. In addition, homeless veterans without a zip code were excluded from this study. According to the annual homeless assessment report (AHAR) to Congress from the US Department of Housing and Urban Development, there were an estimated 75,609 homeless veterans on a single night in the US in 2009Citation14. The exclusion of this population omitted patients with significant health risks not accounted for in this study.
Conclusion
While many studies have examined the risks and benefits between statin and non-statin users, this study attempts to recognize the predictors of mortality in new start statin users. Multiple independent variables have been identified as predictors of mortality in statin users after a 6 year follow-up. Different lipid outcomes after the first year of statin therapy were not indicative of long-term mortality. Future studies should further assess optimal lipid-lowering therapies in the veteran population, especially in the later stages of life to improve clinical outcomes.
Transparency
Declaration of funding
This study was not funded. Skaggs School of Pharmacy and Pharmaceutical Sciences provided funding for the research assistant, as part of their Summer Research Internship Program.
Declaration of financial/other interests
The authors have no relevant financial or other relationships to disclose. JDA Peer Reviewers on this manuscript have received an honorarium from JDA for their review work, but have no other relevant financial relationships to disclose.
Acknowledgements
The authors thank the Skaggs School of Pharmacy and Pharmaceutical Sciences at University of California, San Diego for the summer research grant which funded the work of the research assistant.
References
- Hoyert DL, Xu J. Deaths: preliminary data for 2011. National Vital Statistics Reports 2012;61:1-4
- Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation 2014;129:28-292
- Kannel WB, McGee D, Gordon T. A general cardiovascular risk profile: the framingham study. Am J Cardiol 1976;38:46-51
- Huxley R, Lewington S, Clarke R. Cholesterol, coronary heart disease and stroke: a review of published evidence from observational studies and randomized controlled trials. Semin Vasc Med 2002;2:315-23
- Cheung BM, Lauder IJ, Lau CP, et al. Meta-analysis of large randomized controlled trials to evaluate the impact of statins on cardiovascular outcomes. Br J Clin Pharmacol 2004;57:640-51
- Mann D, Reynolds K, Smith D, et al. Trends in statin use and low-density lipoprotein cholesterol levels among US adults: impact of the 2001 national cholesterol education program guidelines. Ann Pharmacother 2008;42:1208-15
- Naderi SH, Bestwick JP, Wald DS. Adherence to drugs that prevent cardiovascular disease: meta-analysis on 376,162 patients. Am J Med 2012;125:882-7
- Mann DM, Muntner P, Falzon L, et al. Predictors of nonadherence to statins: a systematic review and meta-analysis. Ann Pharmacother 2010;44:1410-21
- National Center for Veterans Analysis and Statistics. Quick facts. Washington, DC. www.va.gov/vetdata. Accessed March 25, 2014
- Fukuta H, Sane D, Brucks S, et al. Statin therapy may be associated with lower mortality in patients with diastolic heart failure. Circulation 2005;112:357-63
- Afilalo J, Duque G, Steele R, et al. Statins for secondary prevention in elderly patients: a hierarchical bayesian meta-analysis. J Am Coll Cardiol 2008;51:37-45
- Hebert PR, Gaziano M, Chan KS, et al. Cholesterol lowering with statin drugs, risk of stroke, and total mortality: an overview of randomized trials. JAMA 1997;278:313-21
- Blackburn DF, Dobson RT, Blackburn JL, et al. Cardiovascular morbidity associated with nonadherence to statin therapy. Pharmacotherapy 2012;25:1035-43
- Henry M, Cortes A, Morris S. The 2013 annual homeless assessment report to Congress. The U.S. Department of Housing and Urban Development, 2013. pp 38-9. Washington, DC. https://www.onecpd.info/resources/documents/AHAR-2013-Part1.pdf. Accessed March 25, 2014