Abstract
Recently, sustained and controlled drug delivery has become the demand, and research has been undertaken in achieving much better drug product effectiveness, reliability and safety. The in situ polymeric system has gained much attention, to develop a controlled release system. It has been used as a vehicle for local and systemic drug delivery. Nowadays, it has created much interest, because of its characteristics of high vascularization, high permeability, rapid onset of action, low enzymatic degradation, and avoidance of hepatic first pass metabolism. The main aim of this review is to provide knowledge of different mechanisms of nasal absorption and approaches for nasal drug delivery.
Introduction
For the past few decades, most of the routine drugs are being administered by parenteral and oral routes (CitationChaudhary et al. 2014). Although the oral route is convenient and cheap, sometimes inefficiencies such as low solubility of drug, and the first pass effect (orally absorbed drugs are transported via liver to the general circulation where they metabolized) (CitationGagandeep et al. 2014), may cause it to suffer from poor bioavailability (e.g. Griseofulvin) (CitationArida et al. 2007). The greater first pass effect of the drug (the rate and extent of the drug reaching systemic circulation), the lower the bioavailability. This route is also not suitable for unconscious patients (CitationIllum 2007). Therefore, to solve this problem, the parenteral route is proposed, which is accurate, and enables immediate onset of reaction and 100% bioavailability, but it is unacceptable if the drug is proposed for the treatment of chronic disease, because this route also has a risk of embolism and attaining high concentrations, rapidly leading to greater risk of adverse effects. Therefore, a different route is preferred (CitationGarg 2014). Also, the percutaneous (transdermal) route is used for controlled delivery of drug (stable blood levels) and does not suffer from first pass metabolism, but its use is limited due to low permeability of the skin to many drugs (CitationMao et al. 2004). To control these issues, nonparenteral routes, also called transmucosal routes, including the nasal, buccal, pulmonary, rectal and vaginal routes, are used. These routes have few benefits or advantages, such as the possibility of self-administration. The nasal mucosal route of administration achieves faster and higher level of drug absorption. This route has attained great attraction for drug delivery of various drugs (CitationGarg and Goyal 2012).
Intranasal drug delivery (Mucoadhesive drug delivery system)
Traditionally, the medication for local diseases, such as rhinitis and nasal congestion, has not been administered through the nasal cavity. However, over the last few decades, intranasal (IN) delivery has been gaining much more attention as a promising route of drug administration for systemic therapy (CitationGavini et al. 2006). Presently, it is being recognized for the delivery of therapeutic compounds including biopharmaceuticals, and for topical nasal treatments such as antihistamines and corticosteroids, and also for systemic delivery of analgesics, sedatives, hormones, vaccines, and cardiovascular drugs by means of the nasal mucosa (CitationGarg and Goyal 2014b). This is because of the anatomy and physiology of the nasal passage, such as the highly vascularized epithelium, ready accessibility, large surface area, permeable endothelial membrane, high total blood flow, and the prevention of first-pass metabolism (CitationMainardes et al. 2006). IN administration is a “needleless” and non- invasive method of drug delivery through the nose to the brain, and hence an alternative for systemic drug delivery (CitationAlam et al. 2010). Therapy through IN administration has been an accepted as a form of treatment in the ayurvedic system of Indian medicine, and is called “Nasya Karma”. Drug delivery through the nose is uncomplicated and convenient, and can include the delivery of solutions, suspensions, powders, in situ gel, and ointments (CitationGarg and Goyal 2014c).
The avoidance of first pass metabolism, quick onset of action, and lowered systemic exposure to drug are the main advantages of IN delivery. Nose-to-brain delivery of drug moieties are possible through the olfactory region, by neuronal and extracellular pathways located at the roof of the nasal cavity, whose neuroepithelium is the only part of the central nervous system (CNS) that is directly exposed to the external environment (CitationGarg and Goyal 2014a). The therapeutic agents are carried to the CNS through the olfactory neuroepithelium by the trigeminal nerve systems and olfactory nerve pathways (CitationAli et al. 2010). In both intravenous as well as oral administration, the blood-brain barrier (BBB) restricts the brain's access to the drug. However, the intranasal route of delivery can also provide a route of entry to the brain that circumvents the BBB, because the olfactory receptor cells are in direct contact with the CNS (CitationWang et al. 2008).
Recently, the nasal mucosa has been examined as a possible route of administration to achieve a faster and higher level of drug absorption (CitationGarg et al. 2012a). The nasal cavity provides a number of distinctive benefits, such as ease of access, good permeability mainly for lipophilic and low molecular weight drugs, low proteolytic activity, prevention of harsh environmental conditions and hepatic first pass metabolism, and potential direct delivery to the brain. Significantly, a number of invasive techniques in drug carrier systems, like the use of nanoparticles, liposomes, nanoemulsions, chemical modifications, the prodrug approach, and other invasive strategies like intraparenchymal, intraventricular, and intrathecal delivery are used to increase the CNS-targeting of drugs (CitationHaque et al. 2012). Large investigative studies have shown that when administered intranasally, vaccines can encourage both local and systemic immune responses. and show the advantages and limitations of intranasal delivery along with their respective associated factors.
Table I. Advantages (associated factors) of intranasal delivery (CitationSam et al. 1995).
Table II. Limitations (associated factors) of intranasal delivery (CitationGarg et al. 2014a).
Barriers for nasal drug delivery
Low bioavailability, muco-ciliary clearance, and enzymatic degradation act as major barriers for nasal drug delivery. Some important characteristics of various barriers which mainly affect the nasal drug delivery are discussed below.
Low bioavailability (CitationIllum 2000)
Bioavailability of polar drugs is mainly low (about 10% for low molecular weight drugs and 1% for peptides such as calcitonin and insulin).
With a large molecular weight, polar drugs have limited nasal absorption.
Drugs can cross the epithelial cell membrane by the transcellular and paracellular routes between cells.
Polar drugs with a molecular weight below 1000 Da will pass the membrane by the latter routes.
Nasal absorption of polar drugs is enhanced by co-administration of absorption-enhancing agents.
Polarity lipophilic:
LMW lipophilic -100% bioavailability
HMW amphipathic -10% bioavailability
Peptides < 1%
Examples
Surfactants (Sodium lauryl sulfate, sodium dodecyl sulfate, phosphatidylcholines, laureth-9)
Bile salts (Sodium glycocholate, sodium taurocholate, sodium deoxycholate)
Fatty acids and their derivatives (linoleic acid)
Phospholipids (lysophosphatidylcholine)
Various cyclodextrin and cationic compounds like chitosan, poly-L-arginine, and poly-L-lysine
Fusidic acid derivatives (sodium tauradihydrofusidate)
Muco-ciliary clearance (CitationSoane et al. 1999)
It is an essential factor which involves the combined action of the mucus and cilia, which defend against inhaled foreign particles in the respiratory tract.
Across the nasal mucosa, it leads to decreased transport of drugs because of high clearance.
It has also been shown that for liquid and powder formulations which are not bioadhesive, the half-life for clearance is of the order of 15–30 min.
The bioadhesive excipients are used in the formulations as an approach to overcome the rapid muco-ciliary clearance.
The clearance may also be decreased by depositing the formulation in the anterior and less ciliated part of the nasal cavity, thus leading to improved absorption.
Enzymatic degradation (CitationGarg et al. 2014d)
When peptides and proteins cross the nasal mucosa, there is the possibility of an enzymatic degradation of the molecule in the lumen of the nasal cavity or during passage through the epithelial barrier, which can limit the bioavailability of the drug.
These two sites contain exopeptidases such as mono and diamino peptidases, that can cleave peptides at their N and C termini, and endopeptidases such as serine and cysteine, which can attack internal peptide bonds. The use of enzyme inhibitors, cosolvents, and prodrugs may be the approaches to overcome this barrier.
Mechanism of drug absorption
The first step in the absorption of drug from the nasal cavity is passage through the mucus. Small, uncharged particles easily pass through this layer, though large or charged particles may find it more difficult to cross. The principle protein in the mucus is mucin, which has the potential to bind to solutes, hindering diffusion (CitationGarg et al. 2014b). Structural changes in the mucus layer are possible as a result of environmental changes (i.e. pH, température, etc.) subsequent to a drug's passage through the mucus. Different mechanisms for absorption through mucosa exist (CitationGarg et al. 2014c). They include transcellular (simple diffusion across the membrane) and paracellular transport (movement between cell and transcytosis by vesicle carriers). Drug absorbed can potentially be metabolized before reaching the systemic circulation, and has limited residence time in the cavity (CitationGarg et al. 2011a). Different mechanisms, such as passive diffusion (transcellular), passive diffusion (paracellular), carrier-mediated transport, transcytosis, absorption, and efflux transport have been used for drug transport through the nasal epithelium (CitationGarg et al. 2011b). discusses some important comparisons between the two mechanisms, which are widely used in drug transport through the nasal epithelium.
Table III. Mechanism of drug passage through the mucus.
Factors influencing nasal drug absorption
Factors related to drug
Molecular weight
Fisher et al. concluded that the permeation of drugs less than 300 Da is not significantly influenced by the physicochemical properties of the drug (like molecular weight, size, formulation pH, and pKa of molecule). As molecular weight increases, nasal absorption of drug increases (CitationFisher et al. 1992).
Chemical form
The chemical form of the drug is an important factor for absorption. Conversion of the drug into a salt or an ester form can change its absorption; for example in situ absorption of carboxylic acid esters of L-tyrosine was significantly greater than that of unmodified L-Tyrosine (CitationGarg et al. 2012b).
Polymorphism
Polymorphism affects the rate of drug dissolution, solubility, and absorption through biological membranes (CitationGarg et al. 2013).
Solubility & dissolution rate
Both are important factors in determining nasal absorption of drugs from powders and suspensions. In the nasal cavity, the deposited particles need to be dissolved prior to absorption. No absorption takes place if particles remain in the nasal cavity. The mucosa in nasal cavity is insufficient for dissolution of drug particles, when compared to gastrointestinal fluid available in the case of oral drug delivery (CitationGoyal et al. 2013a).
Lipophilicity
On increasing lipophilicity, the permeation of the compound through the nasal mucosa increases because of high lipophilicity, though it has some hydrophilic character. Lipophilic compounds easily cross biological membranes through the transcellular route, since they are fit to partition into the lipid (bilayer) of the cell membrane and diffuse into and traverse the cell in the cell cytoplasm. Systemic bioavailability is decreased due to the hydrophilic nature of many drugs (CitationGoyal et al. 2013b).
Partition coefficient and pKa
The pH partition theory states that non ionized species are absorbed well, when compared with ionized species, and hence it is the same in the case of nasal absorption as well.
In a study of the constant relationship between the physicochemical properties of drugs and their nasal absorption, the results showed that a quantitative relationship existed between the partition coefficient and the nasal absorption constant.
In biological tissues, drug concentration increases with increase in the lipophilicity or partition coefficient of the drug (CitationGoyal et al. 2014a).
Factors related to formulation
Physicochemical properties of formulation
pH and mucosal irritation
In addition to the properties of the nasal surface, the pH of the formulation can affect a drug's permeation. Both the pH and pKa of drug are considered to rationalize systemic absorption. To avoid nasal irritation, the pH of the nasal formulation should be adjusted to 4.5–6.5. Avoiding irritation results in obtaining efficient drug permeation and prevents the growth of bacteria. Nasal secretions contain lysozyme, which, at acidic pH, destroys certain bacteria. Under alkaline conditions, lysozyme is inactivated and the nasal tissue is susceptible to microbial infection (CitationGoyal et al. 2014b).
Osmolarity
Isotonic solutions are administered for shrinkage of the nasal epithelial mucosa, because of the effect of osmolarity on the absorption. This results in increased permeation of the compound because of structural changes. Isotonic solutions also known to inhibit or cease ciliary activity (CitationHussain et al. 2014).
Viscosity
A higher viscosity of the formulation increases contact time between the drug and the nasal mucosa, thereby increasing permeation time. At the same time, highly viscous formulations interfere with the normal functions like ciliary beating or muco-ciliary clearance, and thus alter the permeability of drugs (CitationJohal et al. 2014).
Buffer capacity
Nasal formulations are administered in small volumes ranging from 25 to 200 μL. Therefore, nasal secretions may alter the pH of the administrated dose, which can affect the concentration of nonionized drug available for absorption. Hence, an adequate formulation buffer capacity may be required to maintain the pH in situ (CitationJoshi et al. 2014a).
Drug concentration, dose, & dose volume
These are three interrelated parameters that impact the performance of the nasal delivery.
Therapeutic dose: upper limit 25 mg/dose
Higher the drug concentration, higher the permeation
Dose volume: 0.05–0.15 ml/dose (CitationJoshi et al. 2014b)
Physiological factors
Effect of deposition on absorption
Deposition of the formulation in the anterior portion of the nose provides a longer nasal residence time and better absorption, and this is an area of low permeability, whereas in the posterior portion of the nose, where the drug permeability is generally higher, the deposited drug is eliminated by muco-ciliary clearance and therefore has a shorter residence time. (CitationKalia et al. 2014).
Nasal blood flow
The nasal mucosal membrane is very rich in vasculature and plays an important role in thermal regulation and humidification of the inhaled air, and therefore the drug absorption will depend upon the vasoconstriction and vasodilatation of the blood vessels (CitationKataria et al. 2014).
Effect of enzymatic activity
Many enzymes might affect the stability of drugs which are present on the nasal mucosa. For example, proteins and peptides are subjected to degradation by proteases and amino-peptidases at the mucosal membrane (CitationKaur et al. 2014a).
Effect of muco-ciliary clearance
The muco-ciliary clearance is inversely related to the residence time, and therefore inversely proportional to the absorption of drugs administered. It is important to maintain the nasal clearance mechanism to perform normal physiological functions like removal of dirt, allergens, and bacteria (CitationKaur et al. 2014b).
Effect of pathological conditions
Intranasal pathologies such as infections, nasal surgery, cold, and allergic rhinitis may affect the nasal muco-ciliary transport process and/or capacity for nasal absorption. Nasal pathology also alters mucosal pH, and thus affects the absorption of drugs (CitationKaur et al. 2014c).
Strategy to overcome these factors
Different methods to improve nasal absorption
Permeation enhancers
A variety of permeation enhancers have been investigated to improve the nasal absorption, like fatty acids, bile salts, phospholipids, surfactants, cyclodextrin, etc., which act via different mechanisms such as inhibition of enzyme activity, reduction of mucus viscosity, decreasing muco-ciliary clearance, opening tight junctions, and solubilizing or stabilizing the drug (CitationKaur et al. 2014d).
Prodrug approach
Prodrugs are the inactive chemical moiety which become active at the target site. This approach is mainly used to improve the physicochemical properties such as taste, solubility, and stability of formulation. This approach includes derivatization of C and N termini, esters, and cyclic prodrugs (CitationKaur et al. 2014f).
In situ gel
The conversion into gel by the influence of stimuli including temperature, pH, and ionic concentration, is possible with substances like Carbopol, cellulose derivatives, lecithin, chitosan, etc. (CitationKaur et al. 2014e). These formulations generally control the problems of administration.
Nasal enzyme inhibitors
Enzyme inhibitors like protease and peptidase are used as inhibitors for the formulation of peptide and protein molecules. Other examples are bile salts, amastatin, bestatin, boroleucine, fusidic acids, etc. (CitationKaur et al. 2014g).
Structural modification
Drug structure can be modified without changing the pharmacologic activity, to improve nasal absorption. Chemical modifications are mainly used to modify the physiochemical properties of the drug such that they lead to improved nasal absorption of drug (CitationKaur et al. 2014h).
Mucoadhesion
Mucoadhesion can be defined as the state in which two materials are held together for a long period. Mucoadhesive polymers make intimate contact with the biological membrane, and after the establishment of contact, they penetrate into the tissue surface. Natural polymers can be easily obtained from natural sources, and require an environmentally-friendly method of processing with low cost. Some examples include potato starch, rice starch, maize starch, wheat starch, guar gum, tragacanth, xanthan gum, etc. Synthetic polymers produce environmental pollution during synthesis, and have a high cost of production. These polymers include poly ethylene oxide, poly vinyl alcohol, methyl cellulose, ethyl cellulose, hydroxyl propyl methyl cellulose, etc. (CitationKaur et al. 2014i).
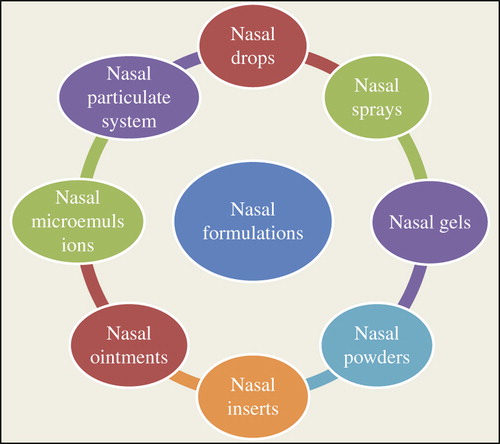
Nasal formulations
Various nasal formulations such as nasal drops, nasal sprays, nasal gels, nasal powders, nasal inserts, nasal ointments, and so on, are used to deliver the drug into the target site that is brain () (CitationKaur et al. 2014j). Among these formulations, in situ gelling systems are widely used for brain targeting.
In situ gelling system
For the past 30 years, greater attention has been directed towards the development of controlled and sustained drug delivery systems. A vast amount of research has been carried out in designing polymeric systems such as in situ gels (CitationKaur et al. 2014k). This system has received significant attention over the past few years. In Latin, in situ means ‘in position’ or ‘in its original place’ (CitationMalik et al. 2014). The routes of administration for in situ gel could be oral, ocular, rectal, vaginal, injectable and intra-peritoneal. “Gel” is the state between liquid and solid, which consists of physically crosslinked networks of long polymer molecules, with liquid molecules trapped within a three dimensional polymeric network swollen by a solvent (CitationMarwah et al. 2014). Many numbers of in situ gel-forming systems have been investigated, and many copyrights for their use in different biomedical applications, including drug delivery, have been reported (CitationPeppas and Langer 1994). This system is a liquid aqueous solution before the administration, and a gel at physiological conditions. Prolonged and sustained release of the drug is reproducible, and the in situ gel is biocompatible, with magnificent stability and reliable quantities of medication, making it more accurate (CitationModgill et al. 2014a). There are various routes for in situ gel drug delivery, for example, oral, ocular, vaginal, rectal, intravenous, intraperitoneal, etc. (CitationModgill et al. 2014b). This new idea of making a gel in situ was proposed for the first time in the early 1980s. Gelation happens through crosslinking of the polymer chain, which can be attained through covalent bond formation (chemical crosslinking) or non-covalent bond formation (physical crosslinking) (CitationCarlfors et al. 1998). The major advantages of in situ gel systems are the ease of administration, improved local bioavailability, reduced dose concentration, reduced dosing frequency, improved patient compliance and comfort, and simple formulation and manufacturing, involving less investment and cost (CitationMorie et al. 2014). Different mechanisms exist which provoke the formulation of in situ gels, such as those based on physiologic stimuli (e.g. temperature modifications, pH-triggered systems) (CitationPabreja et al. 2014), those based on physical changes in biomaterials (e.g. solvent exchange and swelling) (CitationRohilla et al. 2014a), and those based on chemical reactions (e.g. UV radiation, ionic crosslinking, and ion-activated systems) (CitationRohilla et al. 2014b). In this approach, there is no need for any organic solvents, copolymerization agents, or a directly applied trigger for gelation (CitationCho et al. 2003). In situ gel formulation is executed for targeted delivery through the vaginal and rectal routes, and the nasal mucosa, circumventing the hepatic first pass metabolism, which is basically important for the delivery of proteins and peptides that are usually administered via the intravenous route because of their susceptibility to the gastrointestinal proteases (CitationIllum 2003).
Mechanisms of in situ gelling systems
Physiological stimulus-based in situ formulation
Thermally triggered systems
In drug delivery research, the temperature-responsive hydrogels are probably the most usually studied class of environment-responsive polymer systems, because they are easy to control and have practical advantages, both in vitro and in vivo. Gelling can be achieved by means of a polymer that is a solution at room temperature (< 25°C) and undergoes gelation when it comes in contact with the site of application due to an increase in temperature (35–37°C) (CitationWei et al. 2002). The ambient and physiologic temperature is the best significant temperature range for such a system, such that experimental management is facilitated and no external source of heat is required to cause gelation. A temperature-sensitive in situ gel undergoes a volume phase-transition or sol-gel phase-transition at a critical temperature, specifically at the lower critical solution temperature (LCST) or upper critical solution temperature (UCST). LCST polymers reveal a hydrophilic-to-hydrophobic transition with increasing temperature. LCST polymers include poly (N-isopropylacrylamide) (PNIPAM), poly (N,N-diethylacrylamide) (PDEAM), poly(vinyl ether) (PVE), poly(N-vinylalkylamide) (PNVAAM), polyphosphazene derivatives, and poly(ethylene oxide)-b-poly(propylene oxide) (PEO-b-PPO). UCST polymers exhibit a hydrophobic-to-hydrophilic transition with increasing temperature. UCST polymers include polyacrylamide/poly acrylic acid interpenetrating polymer networks (PAAm/PAAcIPN) (CitationSharma et al. 2014a).
They are classified into:
Positively thermosensitive gels
Negatively thermosensitive gels
Thermally reversible gels ()
Table IV. Characteristics of different thermosensitive gels.
These three principal mechanisms have been proposed to explain the sol-to-gel transition after an increase in temperature.
Gradual dissolution of the polymer,
Increased micellar aggregation, and
The improved embarrassment of the polymeric network.
pH-Triggered systems
The pH is another important environment-sensitive parameter for drug delivery, because the pH change occurs at many specific or pathologic body sites, for example stomach, intestine, endosome, vagina, blood vessels, lysosome, and tumor extracellular sites. All pH-responsive polymers contain suspended acidic or basic groups that also accept or release protons in response to changes in environmental pH. Polyelectrolytes are known as the polymers with a large number of ionizable groups (CitationSharma et al. 2014b).
As the external pH increases, swelling of the hydrogel increases in the case of weakly anionic (acidic) groups, but decreases when the polymer contains weakly cationic (basic) groups. Examples: Anionic pH-responsive polymers are based on
– Poly (acrylic acid) (PAA), (Carbopol)
– Polyvinyl acetal diethylaminoacetate solutions form hydrogels at a neutral pH condition at pH 4, with a low viscosity.
– Other examples are Polymethacrylic acid (PMMA), Polyethylene glycol (PEG), Cellulose acetate phthalate (CAP) latex, Pseudolatexes, etc. (CitationRon and Bromberg 1998).
In situ gel formation based on physical mechanism
In situ gel formation (physical mechanism) is based mainly on swelling and diffusion.
Swelling
In situ gel development occurs when the substance absorbs water from the surrounding environment and swells to cover the desired space. An example is Myverol 18–99 (glycerol mono-oleate), which is a polar lipid that swells in water to form lyotropic liquid crystalline phase structures that have some bioadhesive properties and can be degraded in vivo by enzymatic action (CitationSharma et al. 2014c).
Diffusion
Solvent exchange diffusion: In this method, the solvent diffuses from the polymer solution into surrounding tissue, and the outcome is precipitation or solidification of the polymer matrix. N- methyl pyrrolidone (NMP), dimethyl sulfoxide (DMSO), tetrahydrofuran, and triacetin have been shown to be useful solvents (CitationSingh et al. 2014a).
In situ gel formation based on chemical reactions
Ionic crosslinking, enzymatic crosslinking, and photo polymerization chemical reactions mainly cause gelation.
Ionic crosslinking
In this class of in situ gels, the sol-to-gel transition is induced by the presence of various ions (mono or divalent cations such as Na+, K+, Ca++, and Mg++ ions) (84). Naturally occurring anionic polymers such as gellan gum, sodium alginate, carrageenan, and xyloglucan have the characteristic property of cationic-induced gelation.
K-carrageenan forms stiff, delicate gels in response to small amounts of K+, i-carrageenan forms elastic gels mainly in the presence of Ca2+.
Gellan gum, commercially available as Gelrite® or Kelcogel®, is an anionic deacetylated exo cellular polysaccharide secreted by Pseudomonas elodea that undergoes in situ gelling in the presence of mono- and divalent cations, including Ca2+, Mg2+, K+ and Na+, involving a three-dimensional network by complexation and hydrogen bonding with water.
Low-methoxy pectin (degree of esterification < 50%) gelation can be caused by divalent cations, particularly in the presence of free Ca2+ ions which crosslink the galacturonic acid chains in a manner described by the egg-box model. Gelation of pectin also occurs in the presence of H+ ions (divalent ions). The main advantage is that pectin is water soluble, and therefore organic solvents are not needed.
Similarly, alginic acid undergoes gelation in the presence of divalent/polyvalent cations. It is a linear block copolymer polysaccharide, for example Ca2+ due to the interaction with guluronic acid block in alginate chains (CitationSingh et al. 2014b).
Xyloglucan is a polysaccharide derived from tamarind seeds. When xyloglucan is partially degraded by B- galactosidase, the resultant product exhibits thermally reversible gelation by the lateral stacking of the rod shaped chains. The sol-gel transition temperature varies with the degree of galactose elimination, and warming on body temperature, it forms thermally reversible gels (CitationKawasaki et al. 1999).
Enzymatic crosslinking
In this group of in situ gels, the sol-to-gel transition is catalyzed by natural enzymes. They have not been investigated broadly but seem to have some advantages over chemical and photochemical approaches. For example,
An enzymatic process operates capably under physiologic conditions without the need for potentially harmful chemicals such as monomers and initiators.
Intelligent stimuli-approachable delivery systems using in situ gels that can discharge insulin have been investigated.
Cationic pH-responsive polymers containing immobilized insulin and glucose oxidase can swell, releasing the entrapped insulin in a pulsatile fashion in response to blood glucose level. A convenient mechanism for controlling the rate of gel formation is provided by adjusting the amount of enzyme, which allows the mixtures to be injected before gel formation (CitationPodual et al. 2000).
Photo-polymerization
For over more than decade, in situ photo-polymerization has been used in biomedical applications. Monomers (reactive macromeres) and initiator solution can be injected into a tissue site. The application of electromagnetic radiation is used to form a gel.
Acrylate or similar functional groups are typically used as the polymerizable groups on the individual monomers and macromere because they rapidly go through photo polymerization in the presence of a suitable photo initiator.
Classically long wavelength UV and visible wavelengths are used; short UV wavelength is not used because of incomplete penetration of tissue and biological risk. For example, the initiator ketone, such as 2,2 dimethoxy-2-phenyl acetophenone, is used for UV photo-polymerization. Other initiators, camphorquinone and ethyl eosin, are used in visible light systems.
Photo polymerizable systems, when introduced to the desired site via injection, get photo-cured in situ with the help of fiber optic cables and then discharge the drug for a prolonged period of time.
At physiologic temperature, photo reactions provide rapid polymerization rates.
Moreover, the systems are easily placed in complex-shaped volumes leading to an implant formation (CitationBurkoth and Anseth 2000).
Application of intranasal in situ gel delivery
Intranasal delivery is an economic, convenient, simple, and noninvasive method of delivery to target the brain. Through this system, various molecules, such as peptides, proteins, vaccines, analgesics, antidepressants, and antimalarial, antiepileptic, antimigraine, antiemetic, and anticonvulsant drugs etc., are successfully administered to the target site (CitationSingh et al. 2012, CitationSingh et al. 2014c). gives an overview of reported studies related to drug delivery by in situ gel systems to the targeted site (brain).
Table V. Overview of studies reported related to in-situ gel.
Conclusions
This study has been conducted in view of prevalent interest in intranasal mucosal delivery, which provides a needle-free, non- invasive method of targeting the brain by passing the BBB and avoiding hepatic first-pass metabolism in delivering the drug to the brain. This method allows drug direct delivery to the CNS by the olfactory pathway through the mucosa, and provides benefits such as patient compliance and comfort, low exposure, and fewer side effects. It is predictable that intranasal formulations will go on to achieve market potential. The nasal mucosa offers controlled-release drug delivery, but due to certain limitations, the use of the intranasal route for administration of drugs is limited. To decrease these limitations, the mucoadhesive polymeric system is used. The first requirement for controlled drug delivery is to focus on patient comfort, which is offered here by the in situ gelling system. In situ gels also offer a number of other advantages, such as prolonged or sustained release of drug. For the past few decades, extraordinary and novel research on pH-induced, temperature-sensitive, and ion-induced gel-forming formulations have been described in literature. Use of good biodegradable biocompatible, and water-soluble polymers to formulate in situ nasal gels can make them further suitable and excellent as drug delivery systems.
Acknowledgements
The author Dr. Amit K Goyal is thankful to Department of Biotechnology (DBT), New Delhi (under IYBA scheme; BT/01/IYBA/2009 dated May 24, 2010).
Declaration of interest
The authors confirm that the content of this article has no conflicts of interest.
References
- Alam, MI, Beg, S, Samad, A, Baboota, S, Kohli, K, Ali, J, et al. 2010. Strategy for effective brain drug delivery. Eur J Pharm Sci. 40: 385–403.
- Ali, J, Ali, M, Baboota, S, Sahani, JK, Ramassamy, C, Dao, L, Bhavna 2010. Potential of nanoparticulate drug delivery systems by intranasal administration. Curr Pharm Des. 16:1644–1653.
- Arida, AI, Al-Tabakha, MM, Hamoury, HA. 2007. Improving the high variable bioavailability of griseofulvin by SEDDS. Chem Pharm Bull (Tokyo). 55:1713–1719.
- Basu, S, Bandyopadhyay, AK. 2010. Development and characterization of mucoadhesive in situ nasal gel of midazolam prepared with Ficus carica mucilage. AAPS PharmSciTech. 11:1223–1231.
- Bird, S, Derry, S, Moore, RA. 2014. Zolmitriptan for acute migraine attacks in adults. Cochrane Database Syst Rev. 5:CD008616.
- Burkoth, AK, Anseth, KS. 2000. A review of photocrosslinked polyanhydrides: in situ forming degradable networks. Biomaterials. 21:2395–2404.
- Cao, SL, Chen, E, Zhang, QZ, Jiang, XG. 2007. A novel nasal delivery system of a Chinese traditional medicine, Radix Bupleuri, based on the concept of ion-activated in situ gel. Arch Pharm Res. 30:1014–1019.
- Cao, SL, Ren, XW, Zhang, QZ, Chen, E, Xu, F, Chen, J, et al. 2009. In situ gel based on gellan gum as new carrier for nasal administration of mometasone furoate. Int J Pharm. 365:109–115.
- Carlfors, J, Edsman, K, Petersson, R, Jornving, K. 1998. Rheological evaluation of Gelrite in situ gels for ophthalmic use. Eur J Pharm Sci. 6:113–119.
- Chaudhary, S, Garg, T, Murthy, RS, Rath, G, Goyal, AK. 2014. Recent approaches of lipid-based delivery system for lymphatic targeting via oral route. J Drug Target. 22:871–882.
- Chen, E, Chen, J, Cao, SL, Zhang, QZ, Jiang, XG. 2010. Preparation of nasal temperature-sensitive in situ gel of Radix Bupleuri and evaluation of the febrile response mechanism. Drug Dev Ind Pharm. 36:490–496.
- Cho, KY, Chung, TW, Kim, BC, Kim, MK, Lee, JH, Wee, WR, Cho, CS. 2003. Release of ciprofloxacin from poloxamer-graft-hyaluronic acid hydrogels in vitro. Int J Pharm. 260:83–91.
- Doring, K, Best, C, Birklein, F, Kramer, HH. 2014. Zolmitriptan inhibits neurogenic inflammation and pain during electrical stimulation in human skin. Eur J Pain.
- Fisher, AN, Illum, L, Davis, SS, Schacht, EH. 1992. Di-iodo-L-tyrosine-labelled dextrans as molecular size markers of nasal absorption in the rat. J Pharm Pharmacol. 44:550–554.
- Gagandeep, Garg, T., Malik, B, Rath, G, Goyal, AK. 2014. Development and characterization of nano-fiber patch for the treatment of glaucoma. Eur J Pharm Sci. 53:10–16.
- Garg, T. 2014. Current nanotechnological approaches for an effective delivery of bio-active drug molecules in the treatment of acne. Artif Cells Nanomed Biotechnol. 1–8.
- Garg, T, Goyal, AK. 2012. Iontophoresis: drug delivery system by applying an electrical potential across the skin. Drug Deliv Lett. 2:270–280.
- Garg, T, Goyal, AK. 2014a. Biomaterial-based scaffolds–current status and future directions. Expert Opin Drug Deliv. 11:767–789.
- Garg, T, Goyal, AK. 2014b. Liposomes: targeted and controlled delivery system. Drug Deliv Lette. 4:62–71.
- Garg, T, Goyal, AK. 2014c. Medicated chewing gum: patient compliance oral drug delivery system. Drug Deliv Lett. 4:72–78.
- Garg, T, Goyal, AK, Arora, S, Murthy, R. 2012a. Development, optimization & evaluation of porous chitosan scaffold formulation of gliclazide for the treatment of Type-2 diabetes mellitus. Drug Deliv Lett. 2:251–261.
- Garg, T, Kumar, A, Rath, G, Goyal, AK. 2014a. Gastroretentive drug delivery systems for therapeutic management of peptic ulcer. Crit Rev Ther Drug Carrier Syst. 31:531–557.
- Garg, T, Rath, G, Goyal, AK. 2014b. Ancient and advanced approaches for the treatment of an inflammatory autoimmune disease-psoriasis. Crit Rev Ther Drug Carrier Syst. 31:331–364.
- Garg, T, Rath, G, Goyal, AK. 2014c. Biomaterials-based nanofiber scaffold: targeted and controlled carrier for cell and drug delivery. J Drug Target. 1–20.
- Garg, T, Rath, G, Goyal, AK. 2014d. Comprehensive review on additives of topical dosage forms for drug delivery. Drug Deliv.
- Garg, T, Singh, O, Arora, S, Murthy, R. 2011a. Dendrimer—A novel scaffold for drug delivery. Int J Pharm Sci Rev Res. 7:211–220.
- Garg, T, Singh, O, Arora, S, Murthy, R. 2011b. Patented microencapsulation techniques and its application. J Pharm Res. 4:2097–2102.
- Garg, T, Singh, O, Arora, S, Murthy, R. 2012b. Scaffold: a novel carrier for cell and drug delivery. Crit Rev Ther Drug Carrier Syst. 29:1–63.
- Garg, T, Singh, S, Goyal, AK. 2013. Stimuli-sensitive hydrogels: an excellent carrier for drug and cell delivery. Crit Rev Ther Drug Carrier Syst. 30:369–409.
- Gavini, E, Hegge, AB, Rassu, G, Sanna, V, Testa, C, Pirisino, G, Karlsen, J, Giunchedi, P. 2006. Nasal administration of carbamazepine using chitosan microspheres: in vitro/in vivo studies. Int J Pharm. 307:9–15.
- Goyal, AK, Rath, G, Garg, T. 2013a. Nanotechnological approaches for genetic immunization. DNA RNA Nanobiotechnol Med Diagnos Treatment Dis. 67–120.
- Goyal, G, Garg, T, Malik, B, Chauhan, G, Rath, G, Goyal, AK. 2013b. Development and characterization of niosomal gel for topical delivery of benzoyl peroxide. Drug Deliv.
- Goyal, G, Garg, T, Rath, G, Goyal, AK. 2014a. Current nanotechnological strategies for an effective delivery of drugs in treatment of periodontal disease. Crit Rev Ther Drug Carrier Syst. 31:89–119.
- Goyal, G, Garg, T, Rath, G, Goyal, AK. 2014b. Current nanotechnological strategies for treating glaucoma. Crit Rev Ther Drug Carrier Syst. 31:365–405.
- Haque, S, Md, S, Alam, MI, Sahni, JK, Ali, J, Baboota, S. 2012. Nanostructure-based drug delivery systems for brain targeting. Drug Dev Ind Pharm. 38:387–411.
- Hoffler, D, Nebe, K, Wiethoff, EO. 1972. [Studies on the absorption of the combined administration of erythromycin and bromohexine hydrochloride]. Arzneimittelforschung. 22:97–100.
- Hussain, T, Garg, T, Goyal, AK, Rath, G. 2014. Biomedical applications of nanofiber scaffolds in tissue engineering. J Biomater Tissue Eng. 4:600–623.
- Iguchi, A, Matsuu, A, Matsuyama, K, Hikasa, Y. 2014. The efficacy of artemisinin, artemether, and lumefantrine against Babesia gibsoni in vitro. Parasitol Int. 64:190–193.
- Illum, L. 2000. Transport of drugs from the nasal cavity to the central nervous system. Eur J Pharm Sci. 11:1–18.
- Illum, L. 2003. Nasal drug delivery–possibilities, problems and solutions. J Control Release. 87:187–198.
- Illum, L. 2007. Nanoparticulate systems for nasal delivery of drugs: a real improvement over simple systems? J Pharm Sci. 96:473–483.
- Johal, HS, Garg, T, Rath, G, Goyal, AK. 2014. Advanced topical drug delivery system for the management of vaginal candidiasis. Drug Deliv. 1–14.
- Joshi, D, Garg, T, Goyal, AK, Rath, G. 2014a. Advanced drug delivery approaches against periodontitis. Drug Deliv. 1–15.
- Joshi, D, Garg, T, Goyal, AK, Rath, G. 2014b. Development and characterization of novel medicated nanofibers against periodontitis. Curr Drug Deliv.
- Kalia, V, Garg, T, Rath, G, Goyal, AK. 2014. Development and evaluation of a sublingual film of the antiemetic granisetron hydrochloride. Artif Cells Nanomed Biotechnol. 1–5.
- Kasirer, MY, Welsh, C, Pan, J, Shifrin, Y, Belik, J. 2014. Metoclopramide does not increase gastric muscle contractility in newborn rats. Am J Physiol Gastrointest Liver Physiol. 306:G439–44.
- Kataria, K, Sharma, A, Garg, T, Goyal, AK, Rath, G. 2014. Novel technology to improve drug loading in polymeric nanofibers. Drug Deliv Lett. 4:79–86.
- Kaur, M, Garg, T, Narang, RK. 2014a. A review of emerging trends in the treatment of tuberculosis. Artif Cells Nanomed Biotechnol. 1–7.
- Kaur, M, Garg, T, Rath, G, Goyal, AK. 2014b. Current nanotechnological strategies for effective delivery of bioactive drug molecules in the treatment of tuberculosis. Crit Rev Ther Drug Carrier Syst. 31:49–88.
- Kaur, M, Malik, B, Garg, T, Rath, G, Goyal, AK. 2014c. Development and characterization of guar gum nanoparticles for oral immunization against tuberculosis. Drug Deliv.
- Kaur, N, Garg, T, Goyal, AK, Rath, G. 2014d. Formulation, optimization and evaluation of curcumin-beta-cyclodextrin-loaded sponge for effective drug delivery in thermal burns chemotherapy. Drug Deliv. 1–10.
- Kaur, P, Garg, T, Rath, G, Murthy, RS, Goyal, AK. 2014e. Development, optimization and evaluation of surfactant-based pulmonary nanolipid carrier system of paclitaxel for the management of drug resistance lung cancer using Box-Behnken design. Drug Deliv. 1–14.
- Kaur, P, Garg, T, Rath, G, Murthy, RS, Goyal, AK. 2014f. Surfactant-based drug delivery systems for treating drug-resistant lung cancer. Drug Deliv. 1–12.
- Kaur, P, Garg, T, Vaidya, B, Prakash, A, Rath, G, Goyal, AK. 2014g. Brain delivery of intranasal in situ gel of nanoparticulated polymeric carriers containing antidepressant drug: behavioral and biochemical assessment. J Drug Target. 1–12.
- Kaur, R, Garg, T, Das Gupta, U., Gupta, P, Rath, G, Goyal, AK. 2014h. Preparation and characterization of spray-dried inhalable powders containing nanoaggregates for pulmonary delivery of anti-tubercular drugs. Artif Cells Nanomed Biotechnol. 1–6.
- Kaur, R, Garg, T, Malik, B, Gupta, UD, Gupta, P, Rath, G, Goyal, AK. 2014i. Development and characterization of spray-dried porous nanoaggregates for pulmonary delivery of anti-tubercular drugs. Drug Deliv. 1–6.
- Kaur, R, Garg, T, Rath, G, Goyal, AK. 2014j. Advanced aerosol delivery devices for potential cure of acute and chronic diseases. Crit Rev Ther Drug Carrier Syst. 31:495–530.
- Kaur, V, Garg, T, Rath, G, Goyal, AK. 2014k. Therapeutic potential of nanocarrier for overcoming to P-glycoprotein. J Drug Target. 1–12.
- Kawasaki, N, Ohkura, R, Miyazaki, S, Uno, Y, Sugimoto, S, Attwood, D. 1999. Thermally reversible xyloglucan gels as vehicles for oral drug delivery. Int J Pharm. 181:227–234.
- Mainardes, RM, Urban, MC, Cinto, PO, Chaud, MV, Evangelista, RC, Gremiao, MP. 2006. Liposomes and micro/nanoparticles as colloidal carriers for nasal drug delivery. Curr Drug Deliv. 3: 275–285.
- Majithiya, RJ, Ghosh, PK, Umrethia, ML, Murthy, RS. 2006. Thermoreversible-mucoadhesive gel for nasal delivery of sumatriptan. AAPS PharmSciTech. 7:67.
- Malik, R, Garg, T, Goyal, AK, Rath, G. 2014. Polymeric nanofibers: targeted gastro-retentive drug delivery systems. J Drug Target. 1–16.
- Mao, S, Chen, J, Wei, Z, Liu, H, Bi, D. 2004. Intranasal administration of melatonin starch microspheres. Int J Pharm. 272:37–43.
- Marwah, H, Garg, T, Goyal, AK, Rath, G. 2014. Permeation enhancer strategies in transdermal drug delivery. Drug Deliv. 1–15.
- Modgill, V, Garg, T, Goyal, AK, Rath, G. 2014a. Permeability study of ciprofloxacin from ultra-thin nanofibrous film through various mucosal membranes. Artif Cells Nanomed Biotechnol. 1–6.
- Modgill, V, Garg, T, Goyal, AK, Rath, G. 2014b. Transmucosal Delivery of Linagliptin for the Treatment of Type- 2 Diabetes Mellitus by Ultra-Thin Nanofibers. Curr Drug Deliv.
- Morie, A, Garg, T, Goyal, AK, Rath, G. 2014. Nanofibers as novel drug carrier – an overview. Artif Cells Nanomed Biotechnol. 1–9.
- Pabreja, S, Garg, T, Rath, G, Goyal, AK. 2014. Mucosal vaccination against tuberculosis using Ag85A-loaded immunostimulating complexes. Artif Cells Nanomed Biotechnol. 1–8.
- Peppas, NA, Langer, R. 1994. New challenges in biomaterials. Science. 263:1715–1720.
- Podual, K, Doyle, FJ, III, Peppas, NA. 2000. Dynamic behavior of glucose oxidase-containing microparticles of poly(ethylene glycol)-grafted cationic hydrogels in an environment of changing pH. Biomaterials. 21:1439–1450.
- Qiu, Y, Park, K. 2001. Environment-sensitive hydrogels for drug delivery. Adv Drug Deliv Rev. 53:321–339.
- Rohilla, R, Garg, T, Bariwal, J, Goyal, AK, Rath, G. 2014a. Development, optimization and characterization of glycyrrhetinic acid-chitosan nanoparticles of atorvastatin for liver targeting. Drug Deliv. 1–8.
- Rohilla, R, Garg, T, Goyal, AK, Rath, G. 2014b. Herbal and polymeric approaches for liver-targeting drug delivery: novel strategies and their significance. Drug Deliv. 1–17.
- Ron, ES, Bromberg, LE. 1998. Temperature-responsive gels and thermogelling polymer matrices for protein and peptide delivery. Adv Drug Deliv Rev. 31:197–221.
- Sam, E, Jeanjean, AP, Maloteaux, JM, Verbeke, N. 1995. Apomorphine pharmacokinetics in parkinsonism after intranasal and subcutaneous application. Eur J Drug Metab Pharmacokinet. 20:27–33.
- Sharma, A, Garg, T, Aman, A, Panchal, K, Sharma, R, Kumar, S, Markandeywar, T. 2014a. Nanogel-an advanced drug delivery tool: current and future. Artif Cells Nanomed Biotechnol. 1–13.
- Sharma, R, Garg, T, Goyal, AK, Rath, G. 2014b. Development, optimization and evaluation of polymeric electrospun nanofiber: A tool for local delivery of fluconazole for management of vaginal candidiasis. Artif Cells Nanomed Biotechnol. 1–8.
- Sharma, R, Singh, H, Joshi, M, Sharma, A, Garg, T, Goyal, AK, Rath, G. 2014c. Recent advances in polymeric electrospun nanofibers for drug delivery. Crit Rev Ther Drug Carrier Syst. 31:187–217.
- Singh, B, Garg, T, Goyal, AK, Rath, G. 2014a. Recent advancements in the cardiovascular drug carriers. Artif Cells Nanomed Biotechnol. 1–10.
- Singh, H, Sharma, R, Joshi, M, Garg, T, Goyal, AK, Rath, G. 2014b. Transmucosal delivery of Docetaxel by mucoadhesive polymeric nanofibers. Artif Cells Nanomed Biotechnol.
- Singh, K, Arora, N, Garg, T. 2012. RFID: a trustable security tool in pharmaceutical industry. Am J Pharm Tech Res. 2:113–127.
- Singh, O, Garg, T, Rath, G, Goyal, AK. 2014c. Microbicides for the treatment of sexually transmitted HIV infections. J Pharm. 1–18.
- Singh, RM, Kumar, A, Pathak, K. 2013. Thermally triggered mucoadhesive in situ gel of loratadine: beta-cyclodextrin complex for nasal delivery. AAPS PharmSciTech. 14:412–424.
- Soane, RJ, Frier, M, Perkins, AC, Jones, NS, Davis, SS, Illum, L. 1999. Evaluation of the clearance characteristics of bioadhesive systems in humans. Int J Pharm. 178:55–65.
- Wang, S, Chen, P, Zhang, L, Yang, C, Zhai, G. 2012. Formulation and evaluation of microemulsion-based in situ ion-sensitive gelling systems for intranasal administration of curcumin. J Drug Target. 20:831–840.
- Wang, X, Chi, N, Tang, X. 2008. Preparation of estradiol chitosan nanoparticles for improving nasal absorption and brain targeting. Eur J Pharm Biopharm. 70:735–740.
- Wei, G, Xu, H, Ding, PT, Li, SM, Zheng, JM. 2002. Thermosetting gels with modulated gelation temperature for ophthalmic use: the rheological and gamma scintigraphic studies. J Control Release. 83: 65–74.
- Whayne, TF Jr. 2014. Carvedilol versus metoprolol, but which metoprolol? Effect on inappropriate cardioverter-defibrillator therapy. J Am Coll Cardiol. 63:1933.
- Zhao, R, Liu, L, Wang, Y, Xiao, Z. 2014. Vinegar-baked Radix Bupleuri modulates the cell membrane constituents and inhibits the P-gp activity in rat hepatocytes. BMC Complement Altern Med. 14:357.