Abstract
We report the case of a 52-year-old man presenting an extensive lumbosacral necrosis after bilateral internal iliac arteries embolization following unstable pelvic fracture. Coverage of the defect was performed using two extended lumbar artery perforator flaps in a propeller fashion. Good functional and esthetic result was achieved at one-year follow-up.
Introduction
Hemodynamically unstable pelvic fracture is a major cause of death in polytrauma patients and stabilization with internal iliac arteries embolization is sometimes a life-saving intervention. However, due to lack of the gluteal artery vascular network, cutaneous and subcutaneous lumbosacral necrosis can occur in a minority of cases (3%).[Citation1] In such situation, reconstruction can be challenging if the defect is large as there is limited arterial supply in the affected area, including recipient vessels for free flaps.
Here we describe an uncommon indication for large lumbar artery perforator (LAP) flaps to reconstruct lumbosacral defects following bilateral internal iliac arteries embolization. Lumbar artery perforator flaps can be used as a reliable salvage tool in this setting. To our knowledge, we report the first case of bilateral LAP flaps to cover a lumbosacral defect following bilateral internal iliac arteries embolization.[Citation2–4]
Case report
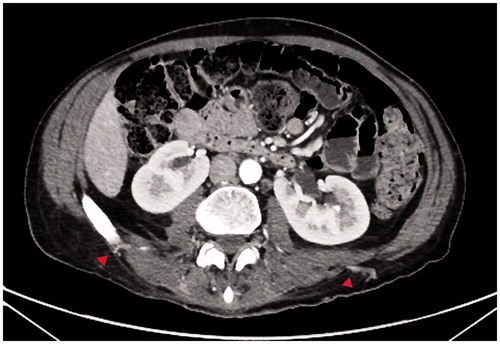
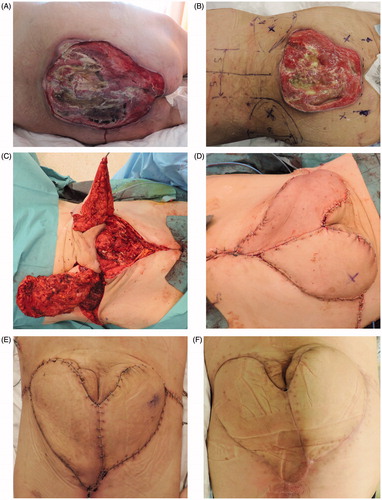
A 52-year-old man known for schizophrenia attempted suicide with a 12 m fall, leading to open book pelvic fracture resulting in hemorrhagic shock (). He was stabilized by bilateral nonselective internal iliac arteries embolization (Video 1, available as supplemental material online). As a complication, he developed skin necrosis in the lumbosacral area. The defect size was 20 × 20 cm (400 cm2) extending from L4 to S4 and total bone exposure. Considering the necessity of a reliable coverage after bone debridement and the relative patient instability precluding a free flap, a reconstruction based on propeller LAP flaps was planned (six weeks after initial trauma, in reason of the hemodynamic and systemic fragility after the polytraumatism, requiring multiple orthopedics interventions). Planification included angio-CT () with 3D reconstruction to exactly localize lumbar perforators. The most suitable vessels in this case were L4 perforators on both sides. Perforators were then double-checked with an ultrasound Doppler probe and marked on the skin preoperatively (Video 2, available as supplemental material online). Flaps were designed from the posterior midline toward the anterosuperior iliac spine. The horizontal distance from the posterior midline to the perforators was 9 cm on both sides and the distance from the posterior midline to the medial edge of the flap was 4 cm (). After extensive bone debridement with posterior corpectomy and dura mater exposure, flaps were raised on each side (23 × 10 cm and 20 × 10 cm; left and right sides, respectively) (). Fasciocutaneous flaps were raised from lateral to medial including the lumbar fascia and the pedicle was dissected with microinstruments. The pedicle included L4 lumbar perforator, accompanying vein and cutaneous nerve. To fit the defect, we rotated the flaps to 90° on the right and 120° on the left providing a substantial coverage with the large amount of subcutaneous tissue and effectively covering the exposed dura mater with the thick lumbar fascia. Wounds were closed in layers over Blake suction drains (Ethicon, Johnson and Johnson, Sommerville, New Jersey, USA; Aesthesio, DanMic Global, San Jose, California, USA). A peroperative venous congestion required skin secondary closure at 6 d (). Flaps were monitored by Doppler ultrasound and clinical evaluation by the nurse every 2 h. Wound healing was uneventful (). Selective antibiotic iv therapy was administered according to bone microbiology (Escherichia Coli and Enterococcus faecalis osteomyelitis). The patient showed no complications at one-year follow-up with return to daily activities. Semmes–Weinstein sensation test (Aesthesio, DanMic Global MMC) at one year showed protective sensation with monofilament test ranging from 2 to 4 g (4.31–4.36 monofilaments size) in all reconstructive areas, indicating good to moderate protective sensibility.[Citation5,Citation6]
Figure 1. T1 (A) and T2 (B) MRI axial sections showing sacral fracture. (C) Radiography showing external fixation for bilateral ilio–ischio–pubic fractures and coiling of both internal iliac arteries.
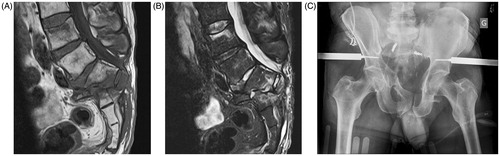
Figure 3. (A) Lumbo-sacral defect extending from L4 to S4 (B) Preoperative skin markings with perforators. (C) Intraoperative flap raising after extensive bone debridement (head of patient on the left, feet on the right). (D) Venous congestion on the left LAP flap right requiring stich removal and partial secondary closure. (E) Uneventful healing after secondary closure. (F) Postoperative follow-up (three months).
Discussion
Unstable pelvic ring injuries have a very high mortality rate due to massive retroperitoneal hemorrhage and consecutive hypovolemic shock. Early control of the bleeding is of utmost importance. Pelvic packing and external fixation are useful devices in the management of low pressure hemorrhage as are venous bleeding and bleeding from the fracture site, whereas angiography and subsequent embolization will be preferred if there is active bleeding secondary to a disruption of the arterial tree. If rapid control of the hemorrhage is needed, selective embolization is sometimes not possible and a nonselective embolization will be performed. In extremely serious cases, bilateral nonselective internal iliac occlusion is necessary.[Citation7]
Gluteal necrosis complicates ∼3% of nonselective bilateral intern iliac arteries embolization performed following a trauma.[Citation1] Selective embolization of internal iliac arteries branches and nonselective embolization performed unilaterally appear to be safe with no consecutive skin necrosis.[Citation8]
There are a few options to cover a sacral defect, as fascio and myocutaneous gluteal rotational flaps or V-Y advancement perforator flaps.[Citation9] Unfortunately the tissues used in these cases have a vascular supply emerging from the internal iliac arteries previously embolized and are therefore not viable anymore in this setting. A free flap may not be conceivable due to the lack of a functional recipient vessel. Both perforasomes and propeller principles become the keys to achieve optimal soft tissue coverage where standard reconstructive procedures are powerless.
Kato et al. described in 1999 a pedicled lumbar artery perforator flap. According to cadaveric dissections and clinical studies the skin territories supplied by each lumbar artery perforator were described.[Citation10] Lumbar arteries emerge from the posterior part of the aorta and then travel behind the quadratus lumborum muscle and in front of the erector spinae muscle. There are typically four arteries on each side generally giving 4–8 perforators. crossing the lumbar fascia laterally to the erector spinae muscles from 5 to 9 cm from midline. The perforators emerging from the second and fourth lumbar arteries are bigger in size (mean pedicle length of 5–6 cm with a diameter of 2–4 mm). Vein and cutaneous nerve travel along perforator artery. A fasciocutaneous flap can be designed up to 12 × 27 cm because a single perforator vascularizes a territory extending from the posterior midline to the lateral border of rectus sheath through vascular networking in the subcutaneous layer. The precise anatomy of lumbar perforator arteries was recently updated using 3D computed tomographic angiogram reconstruction on a series of six human cadavers to establish reliability for breast reconstruction.[Citation11] L1 and L4 perforators showed longer pedicles than L2 and L3 with a decreasing diameter from L1 to L4. L1 perforator was found on a line at the lower edge of 12th rib, whereas L4 perforated the lumbar fascia on a line between the two posterosuperior iliac crests.
Kato et al. applied their findings to treat four patients presenting sacral defects due to pressure ulcers and radiation ulcers with flaps ranging from 5.5 × 14 cm to 8 × 27 cm. All flaps survived and provided good functional and esthetic results.[Citation10] In 2002 de Weerd and Weum reported the use of lumbar perforator flaps to cover a sacral defect in a patient presenting a combination of deep burn and pressure sore measuring in the sacral region. Two propeller lumbar artery perforator flaps were used measuring 12 × 27 cm each, providing effective coverage to the defect.[Citation5] They noted a preserved protective sensibility with Semmes–Weinstein monofilament testing at eight weeks postoperatively on most of the flap skin surface.
Few reports exist on gluteal necrosis after internal iliac artery embolization.[Citation1–3] Among these, in one case only a transposition flap including lumbar perforators was used to cover a limited defect of 5 × 7 cm. To our knowledge, the LAP flap has never been described in extensive lumbosacral defects following bilateral internal iliac arteries embolization. In contrast, we reported here an extensive (400 cm2) and challenging defect, including posterior spine corpectomy and dural exposure. Soft tissue coverage and healing was uneventful using double propeller LAP flaps.
We evaluated the residual protective sensibility with Semmes–Weinstein monofilament testing for comparison with de Weerd et al. study. However, a pressure-specified sensory device could have provided reliable and easily reproducible results according to recent studies evaluating skin sensibility after reduction mammaplasty and tongue reconstruction.[Citation12–14]
In conclusion, a drawback to consider is the shortness of the pedicle which may limit the rotational axis. If the rotational axis of the propeller flap is too wide, venous congestion may occur and a two-step procedure with secondary closure may be necessary. LAP flap present many advantages in lumbosacral defects, being an alternative to free flaps, avoiding the need for microsurgical anastomosis and reducing operating time. Minimal donor site morbidity is present as there is no muscle sacrifice or deeper dissection as in subcostal perforator flaps. Indeed protective sensation is preserved as showed at one-year follow-up. Finally, replacing ‘like with like’ allows for similar tissue texture and good esthetic results.
Video 1: Bilateral internal iliac arteries embolization showing embolized internal arteries
Download Microsoft Video (AVI) (232 MB)Video 2: Pre-operative doppler US probe locating L4 perforators bilaterally
Download QuickTime Video (14.3 MB)Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
References
- Velmahos GC, Chahwan S, Hanks SE, et al. Angiographic embolization of bilateral internal iliac arteries to control life-threatening hemorrhage after blunt trauma to the pelvis. Am Surg. 2000;66:858–862.
- Takahira N, Shindo M, Tanaka K, et al. Gluteal muscle necrosis following transcatheter angiographic embolisation for retroperitoneal haemorrhage associated with pelvic fracture. Injury 2001;32:27–32.
- Gilleard O, Stammers J, Ali F. Gluteal necrosis following pelvic fracture and bilateral internal iliac embolization: Reconstruction using a transposition flap based on the lumbar artery perforators. Int J Surg Case Rep. 2012;3:86–88.
- Al-Thunyan A, Al-Meshal O, Al-Hussainan H, et al. Buttock necrosis and paraplegia after bilateral internal iliac artery embolization for postpartum hemorrhage. Obstet Gynecol. 2012;120(Pt 2):468–470.
- De Weerd L, Weum S. The butterfly design: Coverage of a large sacral defect with two pedicled lumbar artery perforator flaps. Br J Plast Surg. 2002;55:251–253.
- Feng Y, Schlösser FJ, Sumpio BE. The Semmes Weinstein monofilament examination is a significant predictor of the risk of foot ulceration and amputation in patients with diabetes mellitus. J Vasc Surg. 2011;53:220–226.
- Karadimas EJ, Nicolson T, Kakagia DD, et al. Angiographic embolisation of pelvic ring injuries. Treatment algorithm and review of the literature. Int Orthop. 2011;35:1381–1390.
- Auerbach AD, Rehman S, Kleiner MT. Selective transcatheter arterial embolization of the internal iliac artery does not cause gluteal necrosis in pelvic trauma patients. J Orthop Trauma 2012;26:290–295.
- Windhofer C, Michlits W, Gruber S, et al. Reconstruction in the buttock region using the local fasciocutaneous infragluteal (FCI) flap. J Plast Reconstr Aesthetic Surg. 2010;63:126–132.
- Kato H, Hasegawa M, Takada T, et al. The lumbar artery perforator based island flap: Anatomical study and case reports. Br J Plast Surg. 1999;52:541–546.
- Bissell MB, Greenspun DT, Levine J, et al. The lumbar artery perforator flap: 3-dimensional anatomical study and clinical applications. Ann Plast Surg. 2015 [Epub ahead of print].
- Santanelli F, Paolini G, Bittarelli D, et al. Computer-assisted evaluation of nipple-areola complex sensibility in macromastia and following superolateral pedicle reduction mammaplasty: A statistical analysis. Plast Reconstr Surg. 2007;119:1679–1683.
- Longo B, Campanale A, Farcomeni A, et al. Long-term sensory recovery of nipple-areola complex following superolateral pedicled reduction mammaplasty. Plast Reconstr Surg. 2013;132:735–742.
- Longo B, Pagnoni M, Ferri G, et al. The mushroom-shaped anterolateral thigh perforator flap for subtotal tongue reconstruction. Plast Reconstr Surg. 2013;132:656–665.