Abstract
Objective The current standard used to measure setting time for Mineral Trioxide Aggregate (MTA) involves indentation testing with arbitrary weights. This study compared indentation testing against rheological measurements and assessed the influences of particle size and the inclusion of bismuth oxide on the setting time of experimental MTA and Portland cement (PC).
Material and methods Two PCs (P1 and P2) of different particle sizes were produced using the same clinker. From these two PCs, two experimental MTAs (M1 and M2) were created with the addition of bismuth oxide. Particle size distributions were assessed using laser diffraction analysis. Indentation setting time tests were performed in accordance to the Gillmore needle test. Elastic modulus was assessed using a strain-controlled rheometer at 1 rad s−1 and an applied strain of 0.01%.
Results P1, P2, M1 and M2 cements had median particle sizes of 6.1, 12.5, 6.5 and 13.0 μm, respectively. Using indentation testing, final setting times were ranked P1 < M1 < P2 < M2. The ranking of the final setting time corresponded with the rheological assessment of time required to reach 95% of the elastic modulus plateau.
Conclusions The time to reach 95% elastic modulus plateau of 9.3 min corresponds to a time close to the point where the material can be overlaid with another restorative material to give a final restoration. The 95% plateau value for elastic modulus may be a more useful parameter for determining how the setting reaction of PC and MTA cements progress over time.
Introduction
Mineral trioxide aggregate (MTA) is an important dental cement with multiple uses in both endodontics and pediatric dentistry.[Citation1–3] Its handling has been viewed as difficult, and its setting reaction is known to be slow.[Citation4] There have been numerous attempts to improve the handling properties and to accelerate the setting reaction of MTA cements.
Indentation tests are used commonly for analyzing the setting characteristics. These tests assess the point when the setting material has sufficient resistance to indentation from a standardized weight. The ISO methods used currently for assessing the setting time of MTA, namely, ISO 6876 and 9917.1 are designed for testing endodontic sealers and dental restorative materials, respectively. Both ISO tests involve indenting the cement, with resistance to indentation illustrating the final set.[Citation5,Citation6] ASTM C 266, also known as the Gillmore needle test, defines initial set using a similar indentation pressure to ISO 6876, and final set with a similar indentation pressure to ISO 9917.1.[Citation7] Applying different indentation tests can produce quite different outcomes. For example, ProRoot MTA® (Dentsply International Inc, Johnson City, USA) has a setting time of 32 min according to ISO 6876,[Citation8] but 3.8 h according to ISO 9917.1.[Citation9]
Despite the convenience and simplicity of indentations testing for MTA cements, the validity of this approach is questionable. The ability of a cement to resist indentation from an arbitrary weight has limited relevance to whether the material is nearing the end of its setting reaction. From a clinical point of view, indentation from a small area point load does not reflective of the forces applied to the material when placed within the tooth. This is particularly the case in endodontics where occlusal load should not appreciably affect a material placed in a perforation repair or other radicular location. Furthermore, indentations tests do not provide insight into the kinetics of the setting reaction of MTA.
An alternative method of measuring setting time is by utilizing rheometric measurements. Rheometry has been used previously to assess the flow properties of endodontic sealers through narrow capillaries (as a model of flow into root canals) [Citation10] and the setting of glass ionomer cements using either a “displacement rheometer”, which measures the developing elastic recovery of the sample as it cures [Citation10] or a cone/plate rheometer in steady shear mode.[Citation11,Citation12] To date, the use of rheology to characterize MTA cements has been limited to one investigation,[Citation13] which compared MTA to Biodentine® (Septodont, Saint-Maur-des-Fossés, France) and Fuji IX® (GC, Tokyo, Japan). The initial setting point was arbitrarily set at an elastic modulus of 10 MPa and 100 MPa as final set. Based on this, the MTA cement evaluated had an initial setting time of 70 min, and a final setting time of 175 min. These long time periods conflict with clinical evidence that MTA is restorable after 45 min using GIC placed above the MTA,[Citation14] and after 10 min with composite resin placed above the MTA.[Citation15] Thus, the MTA had reached a restorable condition despite not reaching either the traditional definitions of setting based on indentation tests, or when applying the arbitrary elastic modulus values of 10 and 100 MPa to indicate initial and final setting, respectively.
Within rheology, the parameter of elastic modulus is of particular interest, since it measures resistance to elastic (temporary) deformation under a force. Tracking changes in elastic modulus over time can document the change in a material from a liquid-like state (with less resistance) to a solid-like state (with greater resistance). The elastic modulus will asymptotically approach a plateau value at long time periods when the material is fully set. Therefore, rather than a fixed modulus being chosen for the initial setting point, a better choice would be to use a certain percentage of the final modulus. One study proposed a setting time based upon the accumulation of 95% of deformation recovery.[Citation10] While the choice of a percentage is arbitrary, the results must match the clinical properties of the material.
The setting properties of MTA cement are influenced by the particle size of the Portland cement (PC) particles. Commercial brands of MTA have different particle sizes, but many have smaller particle sizes than ProRoot MTA®, the original MTA product. Products with smaller particle sizes set more rapidly when setting is evaluated using indentation tests.[Citation16] A typical MTA cement is four parts Portland cement (PC) and one part bismuth oxide (Bi2O3).[Citation17] The latter is insoluble in water and does not contribute to the setting reaction.[Citation18] Adding the Bi2O3 makes the cement radiopaque, but it also alters the water-powder ratio, with more water required to hydrate the combined powder compared to PC powder alone.[Citation19] Moreover, adding Bi2O3 or other radiopaque agents to the PC powder dilutes the system and physically separates the PC particles, which then changes the flow, workability and setting time of the cement.[Citation19–21]
The current literature on the particle size of MTA describes particle sizes distributions that represent the combined distributions of PC and Bi2O3. This overlooks the properties and influences of the particle sizes of PC and Bi2O3 on the properties of MTA. Accordingly, this study was undertaken to assess the changes in rheological setting properties which occur in experimental MTA from the inclusion of Bi2O3, and as PC particle size is reduced. The study compared the setting time using traditional indentation testing with that from “95% of plateau elastic modulus” as a definition of the setting time for MTA. The choice of 95% reflects a close alignment with the observed clinical handling of the material, i.e. ProRoot MTA® can be restored at 10 min.[Citation15] Therefore, the chosen parameter within the setting properties should be close to 10 min since the feature of considerable relevance to the clinician is the property of restorability.
Material and methods
Two PC powders of different fineness but manufactured from the same cement clinker, were supplied by Si Powders Pty Ltd (Toowoomba, Australia, Lot: UFGP0907/MilledGP; UFGP0907/TS8GP). The regular powder (P2) was created by routine milling processes to create Portland cement. The finer powder (P1) was produced using by jet-milling the regular powder which abrades the larger particles into smaller particles while selectively collecting particles of lower mass and size.
From these PC powders, experimental MTA cements were created by the addition of Bi2O3 (Alfa Aesar®, MA, Lot No E11Y009) to a final level of 20%. This approach generated a regular (P2) and fine (P1) PC, and a regular (M2) and a fine (M1) experimental MTA, from the same original clinker. All four prepared powders were then mixed at powder to water ratio of 3:1 by mass, as recommended in the original MTA patent.[Citation17]
Determination of particle size distribution
Laser diffraction was used to measure the particle size distribution (PSD) of the cement powders, as employed in previous studies.[Citation16] One gram of each cement was suspended in 1 L of methylated spirits as the dispersion liquid. The sample within the dispersion liquid was collected by the Mastersizer 2000 analyzer (Malvern Instruments, Worcestershire, UK). Analysis by the Mastersizer was completed within four seconds. This instrument can measure particles within the range of 0.02–2000 μm.
Mie theory was applied as it is the preferred method when there are particles below 50 μm, with testing performed in accordance with ISO 13320:2009.[Citation22] The particle absorption index used was 0.1. The refractive index (RI) of a heterogeneous material was calculated using weighted averages, based on the equipment manufacturer’s recommendations. The dispersant, methylated spirits, had a RI of 1.36 (5% methanol at a RI of 1.327 and 95% ethanol at a RI of 1.362).[Citation23] The RI for PC was 1.68 [Citation24] and the RI for MTA was 1.844 (80% of PC at RI 1.68 and 20% of Bi2O3 at RI 2.5).[Citation25] The particle absorption index used was 0.1. A sample of ProRoot MTA® powder (Lot no. 9001766) was also assessed, using a RI of 1.844.
Indentation testing
Portland cement (PC) and experimental MTA powders were mixed with water at a powder-to-water ratio of 3:1 (by mass) using mixing capsules for a period of 30 s, within a dental amalgamator. The mixed samples were placed into metal molds with internal dimensions of 5 mm depth, 10 mm length and 8 mm width, and the surface flattened. The samples were incubated at 37 °C and 95% humidity, as per ISO 9917.1.[Citation5] Indentation tests were used to determine the initial and final setting times, following ASTM C 266–08.[Citation7] The initial setting time was based on the sample resisting a load of 113.4 g applied using a needle diameter of 2.11 mm. The duration from the time of mixing and the point in time where the 113.4 g needle did not mark the surface with a complete circular indentation was deemed as the initial set time. The final set time was performed using the same method, but using a load of 453.6 g and a needle diameter of 1.06 mm. There were seven replicates used to assess initial and final setting time measurements for each of the cements.
Rheology testing
The elastic modulus and viscous modulus of the setting cements were tested following a method similar to that from a previous study,[Citation13] using an ARES strain-controlled rheometer (Advanced Rheometric Expansion System, TA Instruments, New Castle, DE). The mixed samples were placed between two parallel plates covered in emery paper, 25 mm in diameter with a 0.6–0.7 mm gap. The lower plate was maintained at a temperature of 38 °C, and a closed chamber was used to maintain a constant temperature and 100% relative humidity, to prevent desiccation. The rheometer was operating in an oscillatory (sinusoidal) mode with an oscillation frequency of 0.159 Hz and an applied strain of 0.01%. Under these conditions, the applied strain was less than that required to alter the structure of the material, approximately 0.05%, established from performing a strain sweep on the cements using the rheometer, the changes in elastic shear modulus over a period of 30 min were measured.
Using rheometry, the “setting time” was defined as the point in time when the material reached 95% of its plateau elastic modulus. In all cases a plateauing of the elastic modulus was seen within the 30 min of data collection so the value of the modulus at 30 min was taken as the ultimate modulus.
Results
Particle size distributions
The PSDs of the P1, P2, M1, M2 cements, Bi2O3 and ProRoot MTA® are summarized in .
Table 1. PSDs of PC, experimental MTA and the bismuth oxide used to produce MTA.
The Bi2O3 used to create the experimental MTA cements had a median size of 6.5 μm, and 90% of particles (d90) were below 16.4 μm. This was similar to the d90 value for the finer powder used (). As expected, P2 cement and M2 MTA (P2 with Bi2O3) had larger particles and were similar in particle size, while P1 and M1 were also similar but had finer particles ().
Indentation setting times
Data for setting times using indentation testing are shown in . For experimental MTA, initial setting times, finer particle size samples had a faster initial setting time than those with larger particle sizes. The fine powder MTA set the fastest, while the large particle size MTA set the slowest. Comparing the groups, M1 < P1 < P2 < M2 with all differences between groups being statistically significant (p < 0.05).
Table 2. Indentation testing initial and final setting times.
In terms of final setting, the inclusion of Bi2O3 delayed the setting reaction, with PC showing a faster final setting time than the experimental MTA of the same particle size. As was seen for initial setting times, finer particle size samples had a faster final setting time than those with larger particle sizes. Comparing the groups, P1 < M1 < P2 < M2, with all differences between groups being statistically significant (p < 0.05).
Rheological testing
For the elastic modulus plateau, the differences between experimental MTA and the corresponding PC (i.e. P1 versus M1 and P2 versus M2) were small and did not reach statistical significance. The finer particle powders showed a reduced time to reach the 95% maximal value for elastic modulus compared to the larger particle powders. As before, finer particle samples had lower final setting times than larger particle samples, and PC had a faster setting time than experimental MTA samples made from powders of the same particle size (P1 < M1 < P2 < M2). The faster setting time corresponded with a greater elastic modulus plateau (P1 > M1 > P2 > M2) ().
Table 3. Plateau elastic modulus and the time to reach 95%.
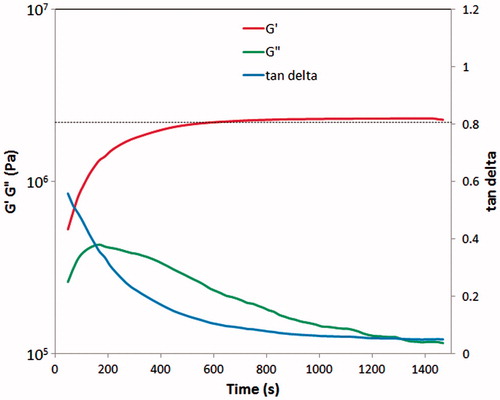
shows the transition of the elastic modulus (G′) and viscous modulus (G″) modulus over time for M1. The horizontal dotted line shows 95% of the plateau modulus. These trends are representative of the materials tested since in all cases (P1, P2, M1, M2) the G″ value increased initially and then fell. The material is initially visco-elastic at the point where G′ and G″ are similar in magnitude, albeit at low values. At this point, during initial stages of the setting process, interlocking of crystals begins to occur and both the elastic and viscous moduli rise. At this stage, the cement mix is becoming progressively thicker, and is less able to flow. At later times, as crystallite interlocking becomes more complete, the viscous modulus (G″) falls. The value for tan delta (the ratio G″/G′) tracks the transition from viscoelasticity to elasticity.
Discussion
The results of this study provide several useful insights into testing the setting process of PC and materials such as MTA which are based on this. The first point is that reducing the particle size of the powder accelerates the setting reaction. For both PC and the experimental MTA, the finer particle cements had faster setting times, regardless of whether the testing method was indentation or rheology. Of note, the fine powder used in the study had a median particle size half that of the standard PC powder, and the corresponding reduction of setting time using the plateau elastic modulus method was also halved, for both PC and experimental MTA. However, the extent of acceleration seen using indentation testing for assessing final setting was much less marked.
The second key point is that the inclusion of Bi2O3 slows the setting reaction, and this effect is seen more so with indentation testing than with rheometry. There are several explanations which can be offered, and these are not exclusive. First, the addition of the Bi2O3 radiopaquer dilutes the PC powder. Second, Bi2O3 particles may impair the extension of crystallites during the hydration phase. Finally, Bi2O3 may act as a barrier between the PC particles and the water during the initial hydration stage.
Previous work using rheology arbitrarily set an elastic modulus of 10 MPa as initial set and 100 MPa as the final set. For MTA, this would correspond to times of 70 and 175 min, respectively.[Citation13] Neither of the 10 or 100 MPa values correspond to realistic loads that the material would be expected to be subjected to during its setting.
This study utilized an experimental MTA, M1, which had a comparable PSD, initial indentation set time, and, final setting time to ProRoot MTA®. For this experimental material, the time to reach 95% of the plateau for elastic modulus of 9.3 min. This time point at which the material had become significantly more resistant to deformation is similar to the time point at which ProRoot MTA® is ready to be overlaid with a permanent restoration, which is 10 min.[Citation15] For example, in pediatric dentistry, when MTA is placed during a pulpotomy, it is then overlaid with a permanent restorative material in the same appointment.[Citation27–30] Likewise, when MTA is used in endodontics, it will be overlaid with a conventional restorative material. These additional restoratives alter the distribution of forces though the tooth and reduce the load which reaches the MTA during its curing phase.
This study illustrates that the time taken to reach 95% of the plateau value for the elastic modulus is the most useful parameter since it aligns to attributes of the set material which have meaning to clinicians. In contrast, indentation tests do not relate to how MTA is used clinically in dentistry, despite their obvious utility and relevance for assessing concrete used in construction or civil engineering projects, where resistance to point loads is important. Thus, clinicians should consider, when using ProRootMTA, to wait 10 min prior to placing another direct restoration atop as this time period enables MTA to reach its peak physical properties within clinically viable time frames.
Rheology as a method of assessing setting time provides several advantages over indentation testing. First, rheometers apply pressures onto the cement that is controlled by a machine while indentation relies upon the tester to use human judgment to drop a weighted needle at a minimized distance from the cement without touching the cement prior to its release. Second, rheometers use a small chamber that is part of the rheometer with controlled temperature and humidity to match physiological conditions. Indentation testing is not typically performed with controlled humidity. Third, rheometric findings can be plotted over time to assess progressive changes in a setting material. These changes relate to the progressive setting and hardening of a material which enable quantitative assessment. Indentation testing is a nominal descriptor with the defining point illustrating no known clinical applicability. Furthermore, indentation testing relies upon subjective visual assessment of whether a material has a full indentation. Furthermore, indentation testing relies upon subjective visual assessment of whether a material has a full indentation.
The final positive point regarding rheology is that when cement sets, a superficial water layer forms on top of the cement. Rheometer plates can use graded plates which engage into the cement to ensure the rheometer is assessing the properties of the cement instead of the water.[Citation31] Indentation testing is impeded by the superficial water layer which obstructs the subjective visual assessment of indentation.
Conclusion
As both PC and its dental cement derivatives such as MTA set slowly, the tests used to confirm that final set has been achieved should have meaning clinically, and be informative to clinicians when they are comparing various products. The time taken for the setting cement to reach 95% of the plateau value for the elastic modulus is suggested as a better and more useful parameter to express the dynamics of the setting reaction of these materials than the currently used indentation tests.
Acknowledgements
The authors thank SiPowders Pty Ltd providing the cement powders in this study and Cement Australia Pty Ltd for assistance with laser diffraction testing. We thank Mingyuan Lu for assistance with indentation testing.
Declaration of interest
This study was supported by the Australian Dental Research Foundation (Grant 2011001653).
References
- Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review-Part I: chemical, physical, and antibacterial properties. J Endod. 2010;36: 16–27.
- Torabinejad M, Parirokh M. Mineral trioxide aggregate: a comprehensive literature review–part II: leakage and biocompatibility investigations. J Endod. 2010;36: 190–202.
- Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review – Part III: clinical applications, drawbacks, and mechanism of action. J Endod. 2010;36:400–413.
- Camilleri J. Modification of mineral trioxide aggregate. Physical and mechanical properties. Int Endod J. 2008;41:843–849.
- ISO 9917-1. Dentistry: water-based cements. Geneva, Switzerland: International Organization for Standards; 2007.
- ISO 6876. Dental root canal sealing materials. Dentistry: water-based cements. Geneva, Switzerland: International Organization for Standards; 2007.
- ASTM C 266-08. Standard test method for time of setting of hydraulic-cement paste by gilmore needles. West Conshohocken (PA): ASTM Int; 2008.
- Silva WJd, Souza PHC, Rosa EAR, et al. Mineral Trioxide Aggregate as root canal filing material: comparative study of physical properties. Revista Odonto Ciência. 2010;25:386–390.
- Akbari M, Zebarjad SM, Nategh B, et al. Effect of nano silica on setting time and physical properties of mineral trioxide aggregate. J Endod. 2013;39:1448–1451.
- Lacey S, Pitt Ford TR, Watson TF, et al. A study of the rheological properties of endodontic sealers. Int Endod J. 2005;38:499–504.
- Cook WD. Dental polyelectrolyte cements. III. Effect of additives on their rheology. Biomaterials. 1983;4:85–88.
- Cook WD. Dental polyelectrolyte cements: II: effect of powder/liquid ratio on their rheology. Biomaterials. 1983;4:21–24.
- Septodont. BiodentineTM Active Biosilicate Technology; [cited 2015 Jun 24]. Available from: http://www.plandent.no/images/Marketing/Infosenter/Biodentine%20Scientific%20File_web_dokumentasjon.pdf.
- Yesilyurt C, Yildirim T, Tasdemir T, et al. Shear bond strength of conventional glass ionomer cements bound to mineral trioxide aggregate. J Endod. 2009;35:1381–1383.
- Tsujimoto M, Tsujimoto Y, Ookubo A, et al. Timing for composite resin placement on mineral trioxide aggregate. J Endod. 2013;39:1167–1170.
- Ha WN, Kahler B, Walsh LJ. Particle size changes in unsealed mineral trioxide aggregate powder. J Endod. 2014;40:423–426.
- Torabinejad J, White DJ. Tooth filling material and method of use. WIPO Patent Publication WO 94/24955; Nov 1994.
- Fridland M, Rosado R. Mineral trioxide aggregate (MTA) solubility and porosity with different water-to-powder ratios. J Endod. 2003;29:814–817.
- Gurney LR, Bentz DP, Sato T, et al. Reducing set retardation in high-volume fly ash mixtures with the use of limestone. J Transport Res Board. 2012;2290: 139–146.
- Camilleri J, Gandolfi MG. Evaluation of the radiopacity of calcium silicate cements containing different radiopacifiers. Int Endod J. 2010;43:21–30.
- Camilleri J. Evaluation of the physical properties of an endodontic Portland cement incorporating alternative radiopacifiers used as root-end filling material. Int Endod J. 2010;43:231–240.
- ISO 13320. Particle size analysis – laser diffraction methods. Geneva, Switzerland: International Organization for Standards; 2009.
- Polyanskiy M. RefractiveIndex.INFO – Refractive index database. [cited 2015 Nov 10] Available from: http://refractiveindex.info/.
- Malvern Instruments Ltd. Sample dispersion & refractive index guide. Worcestershire (UK): Malvern Instruments Ltd.;1997.
- Phelly Materials Inc. Bismuth oxide. [cited 2015 Nov 10]. Available from: http://www.phelly.com/bi2o3/.
- Choi Y, Park SJ, Lee SH, et al. Biological effects and washout resistance of a newly developed fast-setting pozzolan cement. J Endod. 2013;39:467–472.
- Aeinehchi M, Dadvand S, Fayazi S, et al. Randomized controlled trial of mineral trioxide aggregate and formocresol for pulpotomy in primary molar teeth. Int Endod J. 2007;40:261–267.
- Agamy HA, Bakry NS, Mounir MM, et al. Comparison of mineral trioxide aggregate and formocresol as pulp-capping agents in pulpotomized primary teeth. Pediatr Dent. 2004;26:302–309.
- Saltzman B, Sigal M, Clokie C, et al. Assessment of a novel alternative to conventional formocresol-zinc oxide eugenol pulpotomy for the treatment of pulpally involved human primary teeth: diode laser-mineral trioxide aggregate pulpotomy. Int J Paediatr Dent. 2005;15:437–447.
- Moretti AB, Sakai VT, Oliveira TM, et al. The effectiveness of mineral trioxide aggregate, calcium hydroxide and formocresol for pulpotomies in primary teeth. Int Endod J. 2008;41:547–555.
- Banfill P. Rheology of fresh cement and concrete. Rheol Rev. 2006;2006:61–130.