Abstract
Foreign bodies lodged in the intraconal space of the orbit pose a surgical challenge due to its deep location behind the globe. Image-guided endoscopic transnasal surgery facilitates the localization of the metallic foreign bodies and enables its safe removal with minimal surrounding tissue damage and optic nerve injury.
Introduction
Intraorbital foreign bodies are usually a result of high-velocity injuries, and efforts to retrieve them are technically challenging due to their deep location within the orbit. Intraconal foreign bodies are especially difficult to remove considering the confined space within the muscle cone and the close proximity to the optic nerve that increases the risk of intraoperative optic nerve injury. Minimally invasive endoscopic surgery has the advantage of gaining access transnasally into the medial intraconal space with minimal surrounding tissue damage and with no unsightly external scars. An image-guided system further facilitates the removal by localizing the foreign body. Here, we report a case of an intraconal metallic foreign body, successfully removed endoscopically with the aid of an image-guided navigation system.
Case report
A 40-year-old industrial worker presented with painful loss of vision after sustaining a high-velocity injury to the right eye caused by a flying metal shard. He had just removed his protective eyewear at the time of injury. On examination, the right visual acuity was light perception in all quadrants. There were no external injuries to the right eyelid, but uveal tissue could be seen on the nasal aspect of the right conjunctiva (). Right relative afferent defect was present indicating right optic nerve dysfunction. There was hyphema and subconjunctival hemorrhage; however, the cornea was clear with deep anterior chamber in the right eye. There was a large fibrin clump in the anterior chamber indicating intense inflammation. The right lens appeared cataractous with iris pigments on the anterior capsule. There was no view of the right fundus. The right scleral penetrating wound measured 5 mm × 7 mm, located 2 mm from the nasal limbus. The left eye was unremarkable. A computed tomography (CT) of the right orbit revealed a retrobulbar metallic foreign body in the medial intraconal space, measuring 9 mm × 5 mm. The foreign body was located just posterior to the right globe, lying next to the optic nerve ().
Figure 1. Bold arrow shows uveal tissue prolapse at the point of foreign body entry nasally, 1 mm from the nasal limbus. The entry wound is stellate-shaped. Almost half the anterior chamber is filled with hyphema (thin arrow).
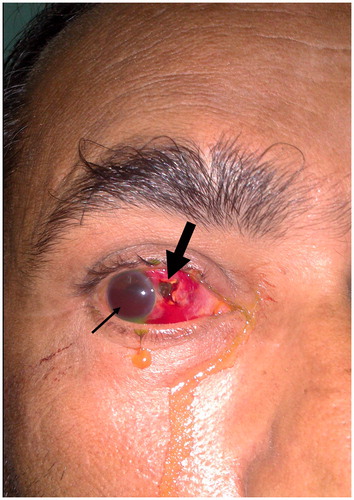
Figure 2. An axial cut section of a CT scan image of the right orbit shows a metallic foreign body embedded in the medial intraconal space, lying posterior to the globe and adjacent to the optic nerve.

Primary repair of the right sclera was performed and intravitreal antibiotics were given within 10 h of injury. Postoperatively, topical and parenteral steroids were commenced, together with intensive topical antibiotic for the right eye. In view of the medial intraconal location of the metallic foreign body in the orbit, a referral was made to the otorhinolaryngology team.
Right endoscopic transnasal surgery was performed four days postinjury. However, the foreign body could not be located. Postoperative X-ray imaging showed the retained metallic foreign body in the medial aspect of the right orbit.
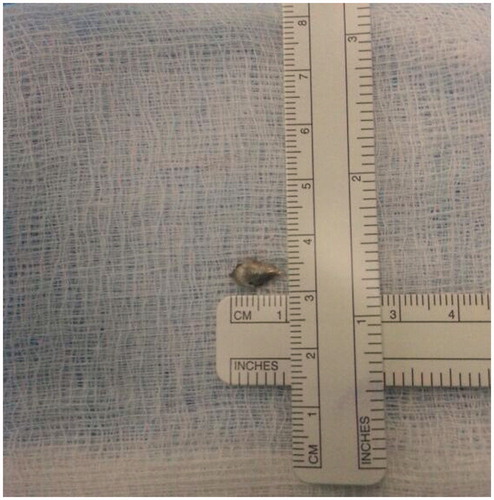
A repeat endoscopic transnasal surgery was performed the next day with the assistance of an image-guided surgery (IGS) system to detect the exact location of the metallic foreign body. With the guidance of the IGS system, the foreign body was successfully removed transnasally. The metal appeared tapered on all sides and measured 10 mm × 5 mm ().
Postoperatively, the reverse relative afferent pupillary defect in the right eye gradually resolved. Subsequently, he underwent vitrectomy for vitreous hemorrhage and retinal detachment repair. Unfortunately, he developed proliferative vitreoretinopathy and his best corrected vision was only hand movement.
Discussion
The main challenge in removing any intraorbital foreign body is in obtaining adequate surgical access to retrieve the foreign body with minimal surrounding tissue damage. The risk of surgical complications in such a challenging procedure could possibly outweigh the risk of foreign body retention in some cases. It can be understood why some ophthalmologists would prefer to leave the foreign bodies in or even resort to enucleation. The risk of surgical complications is further compounded by the difficult localization of the intraocular foreign bodies, despite modern day imaging modalities. Small metallic intraorbital foreign bodies are difficult to localize using the computed tomography (CT) scanning, due to streak artifacts. Conventional orbital X-ray imaging, on the other hand, have no such artifacts; however, they do not reveal as much tissue details as the CT scan. Although magnetic resonance imaging (MRI) provides very detailed soft tissue architecture, it is contraindicated in cases of metallic foreign bodies.
Foreign bodies in the intraconal space pose an even more difficult challenge when they are small, making localization extremely difficult. Lesions in the intraconal space are associated with the highest rate of surgical complications in orbital surgeries.[Citation1] Approaches that have been described to gain surgical access to the medial intraconal space include transcranial,[Citation2–4] transconjunctival,[Citation5,Citation6] transmaxillary [Citation7,Citation8] and eyelid [Citation9,Citation10] approaches. Due to the invasiveness of these approaches, transnasal endoscopic surgery is becoming increasingly popular as a safe surgical technique to access the medial intraconal space.[Citation11–12] Successful removal of orbital foreign bodies using endoscopic surgery has been reported by several authors.[Citation13–15] Although endoscopic transnasal surgery provides a minimally invasive approach to remove foreign bodies in the intraconal space, the risk of inadvertent optic nerve injury still exists. This is because small intraconal foreign bodies are especially difficult to visualize through the endoscope when they are embedded deep in the orbital fat.
Image guided navigation has existed for the past 15 years and has been utilized to facilitate the removal of foreign bodies in the orbit.[Citation16] It not only accurately enables localization of small foreign bodies in the orbit, but also reduces unnecessary tissue dissection, minimizes bleeding and damage to surrounding tissues, prevents injury to the optic nerve and reduces operating time. Endoscopic removal of intraorbital foreign bodies under navigation from image guidance systems is not a novel procedure and has been described by Koo Ng.[Citation15] In his report, the use of an image-guided navigation system combined with endoscopic surgery has enabled the successful retrieval of a foreign body lodged in the orbital apex. A combination of the minimally invasive endoscopic transnasal approach with an image-guided surgical system, greatly enhances the chances of surgical success with minimal ocular morbidities. This winning surgical combination enabled the preservation of the globe and the surgeon could avoid evisceration/enucleation. However, this combined procedure is limited to foreign bodies located on the medial aspect of the orbital cavity and the orbital apex.
Acknowledgements
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Disclosure statement
The authors declare that they have no conflict of interest.
References
- Purgason PA, Hornblass A. Complications of surgery for orbital tumors (1992) Ophthal Plast Reconstr Surg. 1992;8:88–93.
- Abuzayed B, Kucukyuruk B, Tanriover N, et al. Transcranial superior orbitotomy for the treatment of intraorbital intraconal tumors: surgical technique and long-term results in single institute (2012). Neurosurg Rev. 2012;35:573–582; discussion 582.
- Iwata A, Matsumoto T, Mase M, et al. Chronic, traumatic intraconal hematic cyst of the orbit removed through the fronto-orbital approach–case report (2000). Neurol Med Chir (Tokyo). 2000;40:106–109.
- Maus M, Goldman HW. Removal of orbital apex hemangioma using new transorbital craniotomy through suprabrow approach. Ophthal Plast Reconstr Surg. 1999;15:166–170.
- Pillai P, Lubow M, Ortega A, et al. Endoscopic transconjunctival surgical approach to the optic nerve and medial intraconal space: a cadaver study. Neurosurgery. 2008;63:204–208; discussion 208–209.
- Kiratli H, Bulur B, Bilgic S. Transconjunctival approach for retrobulbar intraconal orbital cavernous hemangiomas. Orbital surgeon's perspective. Surg Neurol. 2005;64:71–74.
- Schultheiß S, Petridis AK, Harbony RE, et al. The transmaxillary endoscopic approach to the orbit. Acta Neurochir (Wien). 2013;155:87–97.
- Lyson T, Sieskiewicz A, Rogowski M, et al. The transmaxillary endoscopic approach to the inferior part of the orbit: how I do it. Acta Neurochir (Wien). 2015;157:625–628.
- Pelton RW. The anterior eyelid crease approach to the orbit. Curr Opin Ophthalmol. 2009;20:401–405.
- Pelton RW, Patel BC. Superomedial lid crease approach to the medial intraconal space: a new technique for access to the optic nerve and central space. Ophthal Plast Reconstr Surg. 2001;17:241–253.
- McKinney KA, Snyderman CH, Carrau RL, et al. Seeing the light: endoscopic endonasal intraconal orbital tumor surgery. Otolaryngol Head Neck Surg. 2010;143:699–701.
- Tomazic PV, Stammberger H, Habermann W, et al. Intraoperative medialization of medial rectus muscle as a new endoscopic technique for approaching intraconal lesions. Am J Rhinol Allergy. 2011;25:363–367.
- Feichtinger M, Zemann W, Karcher H. Removal of a pellet from the left orbital cavity by image-guided endoscopic navigation. Int J Oral Maxillofac Surg. 2007;36:358–361.
- Khan-Lim D, Ellis J, Saleh H, et al. Endoscopic transnasal removal of orbital foreign body. Eye. 1999;13(Pt 5):667–668.
- Ng NKFK, Jaberoo MC, Pulido M, et al. Image guidance removal of a foreign body in the orbital apex. Orbit. 2009;28:404–407.
- Klimek L, Wenzel M, Mösges R. Computer-assisted orbital surgery. Ophthalmic Surg. 1993;24:411–417.