Abstract
Objective: To determine the treatment pattern and impact on healthcare costs of anxiety disorders and major depressive disorder (MDD), and influence of their concomitance and subsequence.
Methods: A retrospective cohort study was conducted using a US reimbursement claims database. Adult patients with an incident diagnosis of anxiety or MDD (index date) were included. Their sociodemographic data, diagnoses, healthcare resource use and associated costs were collected over the 6 months preceding and 12 months following index date.
Results: A total of 599,624 patients were identified and included. Patients with phobia or post-traumatic stress disorder had the highest 12-month costs ($8,442 and $8,383, respectively). Patients with social anxiety disorder had the lowest costs ($3,772); generalized anxiety disorder ($6,472) incurred costs similar to MDD ($7,170). Costs were substantially increased with emergence of anxiety during follow-up in MDD patients ($10,031) or emergence of MDD in anxiety patients ($9,387). This was not observed in patients with both anxiety and MDD at index date ($6,148).
Conclusion: This study confirms the high burden of costs of anxiety, which were within the same range as MDD. Interestingly, the emergence of anxiety or MDD in the year following a first diagnosis of MDD or anxiety, respectively, increased costs substantially. Major limitations were short follow-up and lack of absenteeism costs.
Introduction
Anxiety disorders are the most common mental illness in the US, with a 12-month prevalence of 18% and a lifetime prevalence reaching 30% of the populationCitation1,2. By comparison, the lifetime prevalence of mood disorders is about 20%, and that of substance abuse is approximately 15%Citation1.
Anxiety disorders comprise heterogeneous conditions including generalized anxiety disorder (GAD), obsessive-compulsive disorder (OCD), panic disorders, phobias, posttraumatic stress disorder (PTSD) and social anxiety disorders (SAD). However, the intensity and number of symptoms can fluctuate and diagnosis can be difficult and/or masked by other conditions. The clinical presentation of anxiety disorders is further complicated by frequent comorbidity with major depressive disorders (MDD). It is estimated that one-third of patients with anxiety disorder will develop comorbid mood disorder sometime within 12 months after diagnosisCitation3 and more than half the patients diagnosed with mood disorder will develop comorbid anxiety at some point during the 12 months following diagnosisCitation3,4.
In accordance with their high prevalence, anxiety disorders are associated with a high economic burden. Direct costs of anxiety disorders were estimated to be $46.6 billion in 1990 and $63.1 billion in 1998 in the USCitation5,6. More recently, healthcare resource use related to anxiety disorders in the US was evaluated from face-to-face interviews conducted by the National Comorbidity Survey-Replication (NCS-R) and by the World Health Organization (WHO) world mental health (WMH) surveys but, to the authors' knowledge, no cost estimation was performed in these studiesCitation7,8. On the other hand a recent review of cost of illness and cost-effectiveness studies clearly showed the considerable financial burden caused by anxiety disordersCitation9. However, this review also highlighted the difficulty of comparing costs due to large differences in the diagnoses, cost categories and years of study (from 1987 to 2006) considered. As a consequence, direct costs varied quite importantly between studies; e.g. the costs associated with GAD ranged from $2,400 to $28,000. Moreover, only a few studies considered all anxiety disorders simultaneously. Among them, an estimation of the healthcare costs of patients diagnosed with anxiety and prescribed antidepressants (AD) was performed using data from a reimbursement claims database in the USCitation10. This study showed that AD users with both diagnoses of anxiety and depression had higher costs than AD users with depression only. Another study using a similar design showed that healthcare resource use and related costs were increased in patients with both anxiety disorder and depressionCitation11. In these studies, 12-month concomitance was considered and no distinction was made between truly concomitant and subsequent comorbidities, which might, however, correspond to different conditions with different patterns of healthcare resource use.
The aim of the present analysis was firstly to provide further evidence of the costs of the different anxiety disorders, secondly to provide precisions about treatment patterns (e.g. time to prescription from diagnosis), and finally to describe the influence of the dynamic relationship between the diagnoses of anxiety and MDD (concomitance or subsequence) on treatment pattern and 12-month healthcare resource use.
Methods
Data extraction
This retrospective cohort study was conducted using data from the PharMetrics database, a large US administrative claims database (IMS Health, Watertown, MA, USA), which includes data from 86 health plans covering over 55 million people. Database elements include patient demographics, health plan enrolment information, inpatient and outpatient billing, diagnoses and procedures, and outpatient prescription drug dispensing claims. Diagnoses in the medical claims are coded using the International Classification of Diseases, Ninth Revision, clinical modification (ICD-9-CM) codes, procedures are coded using Current Procedural Terminology (CPT) and Healthcare Common Procedure Coding System (HCPCS) codes, and prescription drug claims are coded using National Drug Codes (NDC). Claims data from healthcare providers are updated on a monthly basis. Data quality is constantly checked by PharMetrics, and data are formatted for pharmacoepidemiological analyses.
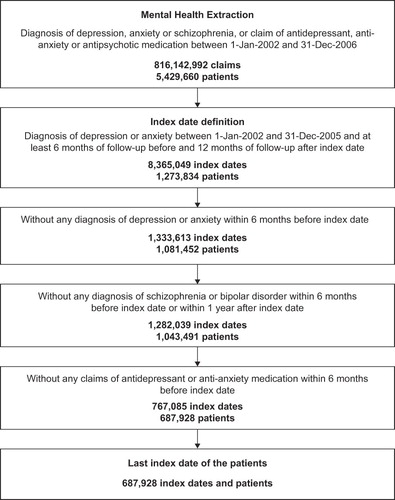
In the present study, data were extracted from the PharMetrics database for any patients aged 18 years or older and having, (1) an incident diagnosis (index date) of anxiety disorder or MDD between January 1st, 2002 and December 31st, 2005, (2) no antidepressant or anti-anxiety agent during the 6 months preceding index date (baseline period), (3) no diagnosis of anxiety or MDD during the baseline period, (4) data available for the baseline period before index date and 12 months of follow-up after index date (i.e. the patient was affiliated to the healthcare plan during this period), and (5) no diagnosis of schizophrenia or bipolar disorder during this 18-month study period (). The ICD-9 codes used for the study are presented in Appendix 1.
Cohorts
For the study of anxiety disorders, patients were included in the cohort corresponding to this first diagnosis recorded. Patients with panic, SAD, other phobia, PTSD, OCD, stress or GAD at index date were included in the ‘anxiety disorders’ cohort as well as the respective sub-cohorts. MDD was used as benchmark to compare results of anxiety disorders, so that two additional cohorts were created: patients with MDD only at index date were included in the ‘MDD’ cohort and patients with both an anxiety disorder and MDD at index date were included in the ‘anxiety plus MDD’ cohort.
To study the dynamic relationship between anxiety and depression, four additional patient cohorts were constituted according to the presence or absence of anxiety and MDD diagnosis at index date and during the follow-up: ‘anxiety only’ (only anxiety during the study period), ‘MDD only’ (only MDD during the study period), ‘anxiety then MDD’ (anxiety at index date and MDD during the follow-up) and ‘MDD then anxiety’ (MDD at index date and anxiety during the follow-up).
Study variables
Demographic and clinical characteristics of the patients were described through age, gender, type of health plan, geographic region, payer type and Charlson Comorbidity Index (CCI)Citation12. The Charlson Comorbidity Index contains 19 categories of comorbidities, primarily defined by ICD-9-CM diagnosis codes. Higher scores represent a higher burden of comorbidity by evaluating the presence of various ICD-9-CM codes during the baseline period derived CCI scores for this study.
Psychiatric medication use and time to treatment onset were evaluated through reimbursement claims for antidepressants selective serotonin reuptake inhibitor (SSRI), serotonin-noradrenalin reuptake inhibitor (SNRI), tricyclic antidepressants (TCA), other antidepressants and anxiolytics (benzodiazepines, other anxiolytics), measured at index date and during the follow-up period.
Healthcare-related costs (reimbursed amounts paid by health plans) were studied during the 6-month baseline period before the index date and the 1-year follow-up period. The 6-month baseline costs were annualized (i.e. multiplied by 2) for comparisons are easier between baseline costs and follow-up costs, as well as with results from other studies. Costs were inflated to year 2006 using OECD reportsCitation13.
Statistical analyses
Quantitative variables (except costs) were expressed as mean (SD). Since costs are typically highly skewed, they were presented as mean, 5th (P5) and 95th (P95) percentiles. Qualitative variables were expressed as frequencies and percentages. Times to treatment were summarized with both mean and median to identify potential skewness in the data. Student's t-test and chi-square tests were used to compare, respectively, quantitative variables and qualitative variables.
Costs were compared using multivariate generalized linear model regression with log link and Gamma distributionCitation14,15. Use of medications (antidepressants or anxiolytics) at index date and during follow-up was modeled using multivariate logistic regression. Univariate analyses on times to treatment were performed using a Kaplan-Meier test. MDD and MDD only cohorts were used as reference. All multivariate models were adjusted on the following baseline characteristics: age, gender, region, CCI, payer type, plan type, baseline psychiatric medication use (yes, no; use of antidepressant and/or anxiolytic at index date), and total healthcare-related cost during the baseline period. Anxiety cohorts and cohorts based on the concomitant or subsequent presence of anxiety and MDD were compared using relative risks (RR) calculated from these multivariate models. MDD and MDD only cohorts were respectively used as reference. A relative risk of 2 for an anxiety group is then interpreted as the costs in this group being twice as high as those in the reference group.
Results
Patients
A total of 599,264 patients were identified () and included in the analysis: 49.7% in the anxiety disorders cohort, 45.1% in the MDD cohort and 5.2% in the anxiety plus MDD cohort. In the anxiety cohort, 71.4% of the patients had a diagnosis of GAD, 18.3% a diagnosis of stress and 6.5% a diagnosis of panic. Other types of anxiety represented less than 2% of the patients (1.2% PTSD, 1.1% OCD, 1.0% other phobias and 0.4% SAD).
Table 1. Baseline socio-demographic and medical characteristics according to index diagnosis.
Two-thirds of patients were female and the mean age was approximately 40 years in all groups, except OCD and SAD patients, which included a smaller proportion of female (53.7 and 41.2%, respectively) and were younger (36.0 and 32.4 years, respectively). SAD and OCD patients also had a lower mean CCI (0.1 and 0.2, respectively) than other patients (0.3–0.4).
Psychiatric medication use
Anxiolytic drugs were prescribed () at index date at the highest frequencies to patients with panic (14.0%), other phobia (12.0%) and GAD patients (11.5%). These were also prescribed anxiolytic drugs at the highest frequency during follow-up (30.3, 34.7, and 24.7%, respectively, p< 0.01).
Table 2. Antidepressant (AD) and anxiolytic (AX) drugs use according to index diagnosis.
Among patients with anxiety disorder at index date, those with OCD, SAD or anxiety plus MDD had the highest frequency of antidepressant prescription at index date (13.5, 11.6, and 16.7%, respectively) and also during follow-up (56.0, 55.7, and 51.5%, respectively). With relative risks (RRs) of 1.6, 1.4, and 1.2, respectively, this frequency was even higher than in patients with MDD only at index date (p< 0.0001); RRs ranged from 0.5 to 0.7 for other anxiety disorders (p< 0.001).
The prescription of both an anxiolytic drug and an AD during follow-up, concomitantly or not, was more frequently observed in panic (16.6%, p< 0.0001) and anxiety plus MDD patients (16.1%, p< 0.0001). The presence of at least one prescription of anxiolytic drug or antidepressant during follow-up was more frequent in SAD (61.3%, p< 0.0001) and OCD patients (58.5%, p< 0.0001).
Treatment by an anxiolytic or an AD usually occurred within the first 2 months following initial diagnosis, except for stress disorders and PTSD (about 3 months); but time to treatment onset varied largely between groups and treatments. Mean time to the first prescription of an anxiolytic drug was the shorter in panic (41.0 days) and GAD patients (49.4 days), and the longer in OCD (115.2 days) and MDD patients (116.4 days). Compared to MDD patients (46.8 days), mean time to the first antidepressant treatment was shorter in anxiety plus MDD (42.0 days p< 0.001) and longer in patients with PTSD (91.8 days, p< 0.001) or stress (92.5 days, p< 0.001).
Healthcare-related costs
Overall, baseline and follow-up healthcare costs () in anxiety disorder patients were broadly similar to those observed in MDD and anxiety plus MDD patients. Baseline 12-month healthcare costs ranged from $1,982 in SAD patients to $6,882 in PTSD and $6,885 in stress patients. During the follow-up period, these costs reached $8,442 in phobic patients and $8,383 in PTSD patients. Patients with SAD had the lowest costs ($3,772). GAD, which was the most prevalent anxiety disorder, incurred costs similar to MDD ($6,472 vs. $7,170, respectively). The higher increase was observed in phobia (+$3,264) and SAD patients (+$1,790). It was only +$650 in stress patients and +$1,014 in MDD patients. The healthcare costs following index date were mostly hospitalization and outpatient. This was followed by office visits and pharmacy.
Table 3. Healthcare costs ($US), during baseline period and the 1-year follow-up. Results were adjusted for inflation and are presented as mean -[P5; P95].
Analyses according to the concomitance of anxiety and MDD
Among patients with anxiety only at index date, 15.9% had a diagnosis of MDD during the 1-year follow-up (). Conversely, among those with MDD only at index date, 14.6% had a diagnosis of anxiety disorder during follow-up. Although statistically significant, no major difference was observed between these cohorts with regards to gender, age and CCI. However, as compared to the distribution of disorders in those with anxiety only at index date, patients with anxiety then MDD or MDD then anxiety had a lower proportion of GAD (73.3 vs. 61.5% and 59.2%, respectively, p< 0.001), and a higher proportion of stress (16.6 vs. 27.5% and 24.7%, respectively, p< 0.001) and PTSD (1.0 vs. 2.3% and 4.3%, respectively, p< 0.001). Differences were also observed with regard to antidepressant and anxiolytic treatments (). A larger proportion of patients with anxiety then MDD or MDD then anxiety were prescribed an antidepressant drug during follow-up (p< 0.001). In addition, compared to other cohorts, a smaller proportion of patients with MDD only had an anxiolytic drug prescribed during follow-up (p< 0.001). The mean time to treatment onset was shorter in the MDD only (44.8 days) and anxiety plus MDD cohorts (42.0 days) (p< 0.001). It was the longer in patients with anxiety then MDD (77.0 days, p< 0.001).
Table 4. Type of anxiety and treatment according to the concomitance of anxiety and MDD.
Patients with anxiety then MDD ($9,387) or MDD then anxiety ($10,031) showed the highest healthcare costs during the follow-up period (RR ≈1.5 compared to MDD only, p< 0.001), which was mostly due to inpatient and outpatient costs (). They also had the highest increase in costs from baseline to follow-up (+$2,739 and +$3,343, respectively). Costs increased by only $966 in anxiety only patients and $615 in MDD only patients.
Table 5. Annualized (12-month) healthcare costs ($US) according to the MDD/anxiety status, during the 6 months preceding index date and 1-year follow-up. Results were adjusted for inflation and are presented as mean [P5; P95].
Discussion
The present study showed that a diagnosis of anxiety was associated with increased healthcare costs over the 12 months following index date and that these costs varied greatly according to the type of anxiety and depression comorbidity. They were highest when anxiety or depression was followed by a subsequent diagnosis of depression or anxiety, respectively, during the following year.
Patients with anxiety disorders often exhibit heterogeneous profiles. This was illustrated by specific characteristics observed in patients with SAD and OCD in the current study. They were less frequently female, were younger, had fewer comorbidities and were more frequently prescribed ADs than sufferers of other anxiety disorders or MDD. These findings are consistent with other recent studies on OCD and SAD in the USCitation16,17. Unfortunately, the lower number of treated women with SAD in the present study tends to confirm a hypothesis raised by Lipsitz et al that social phobia in women is more likely to go untreated due to possible societal gender biased (i.e. more acceptable for a women to be shy)Citation18. SAD and OCD patients were also less frequently prescribed anxiolytics after index date, which seems coherent with guidelines for the management of anxiety disordersCitation19.
In addition, patients with SAD and OCD were associated with lower healthcare expenditures relative to other groups before and after the index date, which seems related to their lower CCI and younger age, in line with the review of cost in anxiety disorders by KonnopkaCitation9. While SAD patients showed relatively low baseline healthcare costs but a steep increase after index date, patients with MDD, PTSD or stress had the highest baseline costs but only a slight increase after the index date (+$1,411, +$604 and +$953, respectively). The increase in healthcare cost in MDD patients was comparable to another study, but the authors did not find other studies that reported baseline costs in patients with SADCitation20. It has been suggested that the lower direct costs associated with SAD could be due to the avoidance behavior of these patients, which results in less contact with the healthcare systemCitation9. As a consequence, the increased costs after diagnosis and treatment may be due to the possible overcome of this avoidance behavior. Overall, cost distributions were similar between groups with inpatient costs the highest, followed by outpatient, office visit and pharmacy costs. This is in accordance with a review of the burden of GADCitation21.
The data presented suggest some poorer recognition of the severity of anxiety disorders compared with MDD. This is supported by the shorter times to treatment onset observed in MDD only patients (45 days) compared with anxiety only patients (54 days) and in MDD then anxiety (55 days) compared with anxiety then MDD patients (70 days). The very short time to treatment onset of anxiety plus MDD patients (42 days) was probably owing to a more severe and/or clear clinical presentation.
It has been reported that the proportion of treated patients who receive adequate treatment is approximately 34% for anxiety disordersCitation8. Current guidelines for the management of anxiety disorders recommend antidepressants as first-line treatment for most of the conditions under study. These guidelines no longer include anxiolytic drugs but this does not seem to be the case in real-life practice. It was observed that anxiolytics were prescribed more than ADs to patients with anxiety (but not MDD) at index date. During the follow-up period, anxiolytics were prescribed at similar frequencies in patients with at least one diagnosis of anxiety or depression, comorbid or not. By contrast, the frequency of AD prescription in patients with anxiety only during the observation period remained twice as low as in other patients. These treatment characteristics may suggest a different clinical pattern of patients or lack of knowledge concerning recommendations for use of ADs as first-line treatment in anxiety disorders. Analysis of time to treatment onset supports this hypothesis since patients with anxiety at index date were prescribed antidepressants on average 1 week after their prescription of an anxiolytic drug.
Interestingly, emergence of a second condition during the 12 months following index date (i.e. patients suffering anxiety then MDD or MDD then anxiety) showed the highest healthcare costs ($8,837 and $9,438, respectively), but also the highest cost increase after index date (+$2,573 and +$3,151, respectively). The lack of clinical information in the database renders difficult the drawing of conclusions or recommendations. However, it is interesting to observe that the time to treatment onset in the MDD then anxiety or anxiety then MDD sequences was larger than in patients with MDD only or anxiety only. Reversely, when the diagnoses of anxiety and depression were concomitant (i.e. at index date), the time to treatment onset were similar to or lower than MDD alone or anxiety alone (42 vs. 45 and 54 days, respectively); and so were the costs ($5,780 vs. 6,272 and 5,749, respectively). This may suggest that shortening time to treatment onset may help in reducing the burden of patients who suffer a second mental illness during the following year.
This may also explain why the authors did not find increased costs in patients with anxiety and comorbid depression at index date, as shown in previous studies considering 12-month anxiety/MDD comorbidityCitation10,22,23. In the present study, patients with concomitant anxiety and MDD at index had the same costs after index date as patients with anxiety only ($5,780 vs. 5,749, respectively) or MDD only ($6,272). By contrast, patients with anxiety then MDD and patients with MDD then anxiety had costs that were, respectively, $3,088 and $3,166 higher than patients with concomitant conditions at index date. Therefore, increased costs are most probably not associated with the comorbidity per se but with the succession of anxiety and MDD, regardless of the first to occur. Interestingly, the costs found here were substantially higher than those of a similar study using the same database, which reported 12-month healthcare costs of $4,411 in anxiety-only patients (vs. $5,749 in the present study) and of $5,367 in anxiety patients with 12-month comorbid MDD (vs. $8,234 in the present study, regardless of the concomitance or subsequence of the comorbidity)Citation10. However, the study in question only considered patients treated by ADs while the present study considered any patient with a diagnosis of anxiety or MDD, regardless of treatments. AD treatment only concerning 30–56% of anxiety disorders, the difference found may be related to a reduced risk of subsequent development of MDD in patients treated. Furthermore, the authors also reported slightly different ranking of the anxiety disorders with the highest costs. Taken together, this suggests that anxiety patients who are prescribed AD incur lower costs than those who are not, which further supports better adherence to recommendations for the management of anxiety disorders.
Limitations of this study include short follow-up and the lack of absenteeism costs. Short follow-up limits consideration of certain costs occurring after the time window, especially those induced by the subsequent depression or anxiety. A longer follow-up could reveal additional costs and, therefore, further increase the differences observed between patients with anxiety only or MDD only compared with patients with anxiety then MDD or MDD then anxiety. Absenteeism is also an important, if not the most important, source of costs. Considering the heterogeneity of patients within the cohorts and sub-cohorts, it could be supposed that absenteeism and associated costs would vary largely between conditions. Performing the same analysis in other databases, with longer follow-up and absenteeism data, could be of value in this regard.
Another limitation inherent in the use of a reimbursement claims database is that diagnoses are neither mandatory nor quality-controlled on individual in claims form. Researchers cannot be certain that all patients actually have the condition they were diagnosed with, or that all patients with anxiety or depression have been correctly identified. To respond partly to this question, patients whose diagnosis at index date was confirmed during the follow-up period (i.e. at least one subsequent occurrence of this diagnosis) and those without confirmation of their index date diagnosis were identified. Comparison of these two populations was performed (data not shown, available upon request) and showed no major difference, in particular with regards to the main outcomes of the study (i.e. healthcare resource use and associated costs). This supports the overall accuracy of the diagnosis reported at index date.
Finally, other factors limit the findings owing to some intrinsic limitations of this type of database. Because of very large samples, some differences that reach statistical significance have little clinical relevance. In addition, as only privately insured patients are included in the database, the results may not generalize to publicly insured or uninsured patients, who may exhibit different cost patterns.
Conclusion
The present study confirms that anxiety disorders are associated with high healthcare costs, comparable to those of depression. With the large sample size of this study, present findings also supports more precise estimation of the direct costs, which are more likely close to $4,000–6,000 than to the previous lower ($2,000) or higher ($28,000) estimates. Furthermore, the results highlighted that emergence of anxiety or MDD in the year following an initial diagnosis of either MDD or anxiety increases costs substantially. A deeper understanding of these heterogeneous conditions and the dynamics of their occurrence, along with improved recognition, diagnosis and management would likely reduce the overall burden of anxiety.
Supplementary Material
Download PDF (180.8 KB)Transparency
Declaration of funding: This study was funded by H. Lundbeck A/S.
Declaration of financial/other relationships: C.F., N.D., and D.S. have disclosed that they are employees of H. Lundbeck A/S; K.M. has disclosed that he has served as a paid consultant for H. Lundbeck. A/S. P.A. has disclosed that he has no relevant financial relationships.
The JME peer reviewers 1 and 2 have not received an honorarium for their review work on this manuscript. Both have disclosed that they have no relevant financial relationships.
AcknowledgmentsThe authors gratefully acknowledge the editorial assistance of Guillaume Hébert, PhD, in the preparation and execution of the present study.
References
- Kessler RC, Berglund P, Demler O, Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005;62:593-602
- Kessler RC, Chiu WT, Demler O, Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005;62:617-627
- de Graaf R, Bijl RV, Smit F, Risk factors for 12-month comorbidity of mood, anxiety, and substance use disorders: findings from the Netherlands Mental Health Survey and Incidence Study. Am J Psychiatry 2002;159:620-629
- Kessler RC, Berglund P, Demler O, The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA 2003;289:3095-3105
- DuPont RL, Rice DP, Miller LS, Economic costs of anxiety disorders. Anxiety 1996;2:167-172
- Greenberg PE, Sisitsky T, Kessler RC, The economic burden of anxiety disorders in the 1990s. J Clin Psychiatry 1999;60:427-435
- Wang PS, Aguilar-Gaxiola S, Alonso J, Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet 2007;370:841-850
- Wang PS, Lane M, Olfson M, Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005;62:629-640
- Konnopka A, Leichsenring F, Leibing E, Cost-of-illness studies and cost-effectiveness analyses in anxiety disorders: a systematic review. J Affect Disord 2009;114:14-31
- Stein MB, Cantrell CR, Sokol MC, Antidepressant adherence and medical resource use among managed care patients with anxiety disorders. Psychiatr Serv 2006;57:673-680
- McLaughlin TP, Khandker RK, Kruzikas DT, Overlap of anxiety and depression in a managed care population: Prevalence and association with resource utilization. J Clin Psychiatry 2006;67:1187-1193
- Charlson ME, Pompei P, Ales KL, A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373-383
- OECD. Country statistical profiles 2009: United States. 2009 [updated 2009; cited 2009 November 30]; Available from: http://stats.oecd.org/index.aspx?queryid=18175
- Blough DK, Ramsey SD. Using Generalized Linear Models to Assess Medical Care Costs. Health Services and Outcomes Research Methodology 2000;1:185-202
- Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ 2001;20:461-494
- Norberg MM, Calamari JE, Cohen RJ, Quality of life in obsessive-compulsive disorder: an evaluation of impairment and a preliminary analysis of the ameliorating effects of treatment. Depress Anxiety 2008;25:248-259
- Schultz LT, Heimberg RG, Rodebaugh TL, The appraisal of social concerns scale: psychometric validation with a clinical sample of patients with social anxiety disorder. Behav Ther 2006;37:392-405
- Lipsitz JD, Schneier FR. Social phobia. Epidemiology and cost of illness. Pharmacoeconomics 2000;18:23-32
- Clinical practice guidelines. Management of anxiety disorders. Can J Psychiatry 2006;51:9-91S
- Simon GE, Chisholm D, Treglia M, Course of depression, health services costs, and work productivity in an international primary care study. Gen Hosp Psychiatry 2002;24:328-335
- Hoffman DL, Dukes EM, Wittchen HU. Human and economic burden of generalized anxiety disorder. Depress Anxiety 2008;25:72-90
- Marciniak MD, Lage MJ, Dunayevich E, The cost of treating anxiety: the medical and demographic correlates that impact total medical costs. Depress Anxiety 2005;21:178-184
- Zhu B, Zhao Z, Ye W, The cost of comorbid depression and pain for individuals diagnosed with generalized anxiety disorder. J Nerv Ment Dis 2009;197:136-139