Abstract
Purpose:
The aim of this narrative review was to summarise the cost analyses and supporting trial data for aspirin prophylaxis in primary prevention.
Methods:
A PubMed search using the term ‘aspirin and cost-effective and primary prevention’ was performed. Professional meetings (2009) were also searched for any relevant abstracts contacting the terms ‘aspirin’ and ‘cost effectiveness’. Where possible, outcomes were discussed in terms of cost implications (expressed as quality-adjusted life-year [QALY], disability-adjusted life-year or incremental cost-effectiveness ratio) in relation to the annual risk of cardiovascular disease. Aspirin was included in cost-effectiveness models that determined direct cost savings.
Results:
A total of 67 papers were identified using PubMed, and 17 cost-effectiveness studies, which assessed aspirin in primary prevention (largely based on the key primary prevention studies), and two abstracts were included in the review. These analyses showed that low-dose aspirin was cost effective in a variety of scenarios. In the UK, Germany, Spain, Italy and Japan, the mean 10-year direct cost saving (including follow-up costs and aspirin costs) per patient was €201, €281, €797, €427 and €889 with aspirin use in patients with an annual coronary heart disease risk of 1.5%. Cost-effectiveness analyses were affected by age, risk level for stroke and myocardial infarction (MI), risk of bleeds and adherence to aspirin. Underutilisation is a major limiting factor, as the appropriate use of aspirin in an eligible population (n = 301,658) based on the NHANES database would prevent 1273 MIs, 2184 angina episodes and 565 ischaemic strokes in patients without previous events; this would result in a direct cost saving of $79.6 million (€54.7 million; 2010 values), which includes aspirin costs.
Conclusions:
Most analyses in primary prevention have shown that low-dose aspirin is a cost-effective option, and is likely to meet the willingness of a healthcare system to pay for any additional QALY gained in the majority of healthcare systems.
Key words::
Introduction
The healthcare costs and loss of productivity associated with cardiovascular diseases are high across all countries ()Citation1–6, and this economic burden is likely to have the most impact on low- to middle-income countries where an estimated US$84 billion (€57.8 billion; 2010 values [US$ 1 = €0.69]) of economic production will be lost from heart disease, stroke and diabetes alone from 2006 to 2015Citation7.
Table 1. Healthcare costs and loss of productivity attributable to cardiovascular diseases across several countries.
Effective and cost-effective treatment strategies are needed in order to reduce the economic burden associated with cardiovascular disease. Long-term prophylaxis with antithrombotic agents could play an important role in preventing vascular events, and the use of aspirin as an antithrombotic agent is recommended in primary prevention in patients at high-risk of future cardiovascular eventsCitation8,Citation9. However, there are no ‘global’ overviews discussing the cost effectiveness of this approach. This article aims to provide an up-to-date summary of the economic analyses for the use of aspirin for the primary prevention of cardiovascular disease in patients at high-risk of future cardiovascular events.
Methods
This was a narrative, non-systematic review of primary prevention cost-effectiveness studies assessing the role of aspirin. A PubMed search was performed using the term ‘aspirin and primary prevention and cost effectiveness’ to identify all published papers up to January 2010; a total of 67 papers were identified. These papers were then searched manually, and any editorials, papers that did not include models which utilised aspirin costs or those that included secondary prevention or non-cardiovascular outcomes were excluded, and a total of 17 cost-effectiveness studies were reviewed. Abstracts presented at the American Heart Association Quality of Care and Outcomes Research in Cardiovascular Disease and Stroke Conference (2009), American College of Cardiology annual conference (2009), the 69th Scientific Sessions of the American Diabetes Association (ADA) (2009), and the European Society of Cardiology annual meeting (2009) were searched using the terms ‘aspirin’ and ‘cost effectiveness’, and two relevant abstracts are discussed.
The aspirin primary prevention trials, including those on which these cost analyses are based, are also discussed. Where possible, outcomes were discussed in terms of cost implications (expressed as quality-adjusted life-year [QALY], disability-adjusted life-year [DALY] or incremental cost-effectiveness ratio [ICER]) in relation to the annual risk of cardiovascular disease. Unless otherwise stated, QALY is defined as a measure that combines the effect of a drug on life expectancy with its effect on quality of life. An increase of one QALY is an increase of 1 year of perfect health due to the drug; DALY is defined as an indicator of the global burden of disease measured on a scale of 0 (perfect health) to 10 (death), and ICER is broadly defined as the ratio of change in costs to change in effects.
Clinical evidence supporting the use of aspirin in the prevention of primary cardiovascular events
The evidence supporting the use of aspirin for primary cardiovascular prevention is largely based on six key trials involving 95,870 patients: the Physicians’ Health StudyCitation10, British Male Doctors’ TrialCitation11, Hypertension Optimal TrialCitation12, Women’s Health StudyCitation13, Thrombosis Prevention ProjectCitation14 and the Primary Prevention ProjectCitation15 ()Citation16. Five of the trials are placebo-controlled, one is open-label, and one is also a comparator study (vs. warfarin). A meta-analysis involving these six trialsCitation10–15 showed that aspirin was significantly superior in preventing total CHD, non-fatal myocardial infarction (MI), and total cardiovascular events (all p < 0.001)Citation17. The most recent meta-analysis performed by the Antithrombotic Trialists’ Collaboration (ATC)Citation16, which also examined these six trialsCitation10–15 showed that 1671 serious vascular events occurred in patients allocated to aspirin compared with 1883 events in patients allocated to placebo (0.51 vs. 0.57%, p = 0.0001); these authors concluded that aspirin was associated with a 12% relative risk (RR) reduction (RR = 0.88 [95% CI, 0.82–0.94]) in serious vascular events. This difference was mainly due to a reduction in non-fatal MI following aspirin treatment (0.18 vs. 0.23%, respectively; p < 0.0001; RR = 0.77 [95% CI, 0.67–0.89]) (). Although a previous meta-analysis involving these trials had shown that stroke reduction was significant (p = 0.02) in women, but not men and the reduction in MI was significant in men (p = 0.001) but not womenCitation18, the analysis by the ATC showed that the aggregate reduction in serious vascular events was not significantly dependent on sex, age, smoking history, blood pressure, cholesterol, body mass index, diabetes or predicted risk of coronary heart disease (CHD)Citation16.
Figure 1. The effect of aspirin on the annual rate of vascular events. Rate ratios are indicated by squares and their 99% confidence intervals by horizontal lines. Subtotals and their 99% confidence intervals are represented by diamonds. CHD, coronary heart disease; CI, confidence interval; MI, myocardial infarction. Reprinted from Antithrombotic Trialists’ (ATT) Collaboration; Baigent C, Blackwell L, Collins R, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet 373:1849–1860, copyright 2009, with permission from Elsevier.
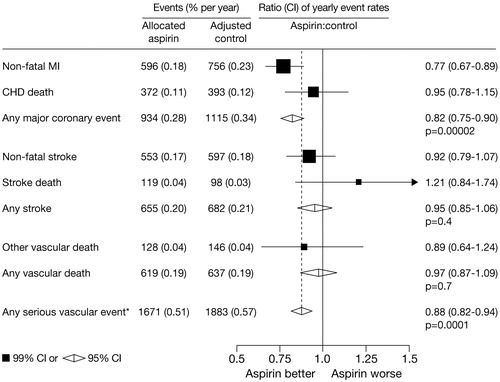
Table 2. An overview of the aspirin primary prevention trials in low- to moderate-risk patients.
Based on these data, a number of organisations such as the US Preventive Services Task Force (USPSTF) and the World Health Organization (WHO) have produced thresholds for aspirin use based on the benefits in terms of event avoided versus the risk of a gastrointestinal bleed (the risk : benefit ratio) in men and women, which are relevant to most countriesCitation8,Citation19. In the USPSTF guidelines, the risk : benefit ratio for aspirin becomes positive in men aged 45–59 years when the 10-year CHD risk is ≥4% (this increases to ≥9% for men aged 60–69 years and to ≥12% for men aged 70–79 years) and for a women aged 55–59 years, the risk : benefit threshold is positive when the 10-year stroke risk is ≥3% (this increases to ≥8% in women aged 60–69 years and to ≥11% in women aged 70–79 years). In most countries, the WHO recommend aspirin in patients with a cardiovascular risk ≥30%; aspirin should probably not be given to individuals with a cardiovascular risk 20 to <30% unless CHD rates exceed stroke rates. Other recently updated guidelines such as those produced by the European Society of Hypertension (ESH) or the Canadian Hypertension Education Program have produced more general statementsCitation20,Citation21. The ESH recommend aspirin in hypertensive patients with high cardiovascular risk, and the Canadian guidelines recommend aspirin once blood pressure is well controlled.
Primary prevention in diabetes
The use of aspirin as primary prevention in patients with diabetes is controversial. The ADA guidelines recommend that aspirin is considered as primary prevention in patients with diabetes and a 10-year cardiovascular risk >10% (level C recommendation)Citation22. The guidelines acknowledge the disappointing results of the Japanese Primary Prevention of Atherosclerosis With Aspirin for Diabetes (JPAD) and Prevention Of Progression of Arterial Disease And Diabetes (POPADAD) studiesCitation23,Citation24, which failed to show significant effects of aspirin on CVD end-point reductions in Japanese populations, but add that the ATC meta-analysis included almost 4000 patients with diabetesCitation16. Disappointing outcomes were also observed in a recent study from China, and in two meta-analysesCitation25–27, although one concluded that based on a cohort of 11,618 individuals, aspirin had sex-specific effects on MI and stroke in patients with diabetesCitation27. Another meta-analysis found that the relative benefit of aspirin was comparable in patients with and without diabetesCitation28. The Fremantle Diabetes study, which included 651 patients with type 2 diabetes and no prior cardiovascular disease history showed that aspirin reduced all-cause mortality in men aged >65 yearsCitation29.
Cost effectiveness of aspirin in the prevention of primary cardiovascular events
European perspective
An economic analysis using data from five of the studies included in the meta-analysesCitation10–12,Citation14,Citation15 has shown that aspirin is cost effective in the prevention of cardiovascular disease in patients with a ≥1% annual risk of CHD (corresponding to a 10-year CHD risk of 10%)Citation30. In this analysis, low-dose aspirin (mean dosage: 166 mg/day) was assessed in four European countries (UK, Germany, Spain and Italy) using direct costs from the healthcare payers’ perspective (2003 values); the cost analysis was based on a state transition model, which included the country-specific costs of aspirin and no aspirin in primary and secondary prevention (i.e., history or no history of cardiovascular disease) with the ultimate transition being death. Although cost savings started from an annual CHD risk of 0.236% in the UK, 0.324% in Germany, 0.244% in Spain and 0.560% in Italy, the risk of gastrointestinal bleeds outweighed the number of events avoided in patients with an annual risk <0.6%. For patients with an annual CHD risk of 1.5%, the mean 10-year savings/patient associated with low-dose aspirin use were €201 in the UK, €281 in Germany, €797 in Spain and €427 in Italy; these savings refer to direct drug costs associated with the condition including follow-up, and include aspirin versus no aspirin use. These cost savings are likely to increase over longer time-periods (i.e., 15 and 20 years), and in Spain, which had the greatest cost-saving per patient over 10 years, treating all individuals with an annual CHD risk >1.5% would save the Spanish national healthcare system €26.5 million in total costs over 10 years; this value includes the cost of aspirinCitation31.
Asian perspective
In a cost analysis conducted in Japan, in which five key primary-prevention studies were usedCitation10–12,Citation14,Citation15, aspirin was found to be cost effective in patients with an annual CHD risk >1.5% (corresponding to a 10-year risk >15%)Citation32. Low-dose aspirin was associated with a mean direct saving/patient of €889 at this risk level, and aspirin was dominant to no aspirin from an annual risk of 0.2%. Aspirin versus no aspirin use was included in the transition model.
US perspective
An analysis in the USA, which used a model population with the characteristics of the National Health and Nutrition Examination Survey (NHANES) database, showed that 557,470 patients from a sample of 1 million patients were eligible for low-dose aspirin (eligibility was defined as a 10-year risk of cardiovascular disease >10% according to Framingham risk equations); however, 301,658 of these patients were not using aspirinCitation33. Eligibility was based on an assessment of cardiovascular disease risk profile using the Framingham risk equations; the risk was then translated into the number of events expected, taking into account age-adjustments over a 10-year period. Using this approach, the model showed that the appropriate use of aspirin in this population would prevent 1273 MIs, 2184 angina episodes and 565 ischaemic strokes in patients without previous events and would lead to an overall cost saving of $79.6 million (€54.7 million, 2010 values) in primary prevention over a 10-year period; this cost saving refers to the direct costs associated with treatment of these conditions based on the estimated numbers, but includes the cost of aspirin treatment for the population.
Cost effectiveness of aspirin in developing countries
Cardiovascular disease is predicted to increase dramatically in low- to middle-income countries; therefore, it is important to identify cost-effective strategies for disease prevention in these regions. In one analysis, primary prevention with aspirin, a calcium-channel blocker, an angiotensin-converting enzyme inhibitor and a statin was determined in six developing regions (East Asia and Pacific, East Europe and central Asia, Latin America and Caribbean, Middle East and North Africa, South Asia and Sub-Saharan Africa) according to differing risks for cardiovascular diseaseCitation34. When the 10-year absolute risk of cardiovascular disease was >25%, the ICER/QALY gained was in the range of $746–890 (€514–613, 2010 values), and $1039–1221 (€715–840) when the risk was >5%. Across these levels, the ICER/QALY gained was <3 times the gross national income/head in that country, which is the World Health Organization (WHO)-recommended threshold for interventions. These findings suggest that effective and cost-effective strategies could be implemented across developing countries.
Another analysis performed in Tanzania determined the cost effectiveness of 14 interventions including aspirin, a diuretic, a beta-blocker, a calcium-channel blocker and a statinCitation35. This analysis showed that the diuretic was the most cost-effective option in very high-risk patients (US$85–143 [€58–98, 2010 values] per DALY avoided). Combination therapy with hydrochlorothiazide and aspirin was associated with a cost of $143–317 (€98–218) per DALY avoided, triple combination with a hydrochlorothiazide, aspirin and atenolol cost $317–999 (€218–687) per DALY avoided, and the combination of hydrochlorothiazide, aspirin, atenolol and lovastatin cost $999–1476 (€687–1016) per DALY avoided. The use of such combinations will depend on the willingness-to-pay per DALY avoided in each country. However, preventative strategies could result in gains in life expectancyCitation34,Citation35.
Cost effectiveness of aspirin according to age, sex and risk level
Using a population from the Netherlands, the cost effectiveness of low-dose aspirin usage (2007 values) was found to be dependent on age, sex and risk levelCitation36. In males aged 55, 65, and 75 years with five times the normal 10-year cardiovascular disease risk (cardiovascular disease risk was estimated from the expected number of events in the ‘no aspirin’ arm divided by the number of simulated persons), the ICER of aspirin treatment compared with no aspirin treatment was €1753, €34, and €562 per QALY gained, respectively. The corresponding values in women aged 55, 65 and 75 years were €114,356, €5747 and €−4465. In women aged 75 years with twice the 10-year cardiovascular disease risk, the ICER per QALY gained was €5791. Given that the willingness-to-pay for an additional QALY in the Netherlands was set at €20,000, the analysis shows that aspirin is cost effective in men aged >55 years and in women aged >65 years with high risk, and in women >75 years with moderate riskCitation37. The authors also concluded that age, cardiovascular risk, cardiovascular risk reductions for stroke and MI with aspirin, risk of gastrointestinal bleeds, haemorrhagic stroke and adherence to aspirin medication may affect the results of cost-effectiveness analyses.
However, the recently published ATC meta-analysisCitation16 suggested that the aggregate reduction in serious vascular events was unaffected by age, sex, or cardiovascular risk level (low, moderate or high), and these authors did not differentiate in their recommendations between men and women. Algra and GrevingCitation38 argue that sex, age and cardiovascular risk level do matter when cost effectiveness of aspirin is being considered and, based on the findings of the recent ATC meta-analysis, have published a revised analysis indicating when aspirin is cost effective (in this analysis, aspirin is recommended when the ICER is <€20,000/QALY). However, these authors used different risk : benefit ratios for cardiac events (vs. haemorrhagic stroke) and ischaemic stroke (vs. haemorrhagic stroke) in men and women than those used in the ATC meta-analysisCitation16, but used the risk of bleeding that was based on the new ATC observations. As a result, the ICER/QALY gained is at a much higher vascular risk and age threshold for both men and women; for example, aspirin is recommended in men aged 50–59 years with a 10-year vascular risk >34% (ICER/QALY, €6000), and in women, aspirin is recommended in women aged 60–69 years with a 10-year vascular risk >34% (ICER/QALY, €3000).
Cost effectiveness of aspirin in diabetes
Aspirin has been shown to be cost effective in patients with diabetes irrespective of the level of cardiovascular risk. A state transition model has recently compared the cost (2005 values) of low-dose aspirin with placebo in the primary prevention of cardiovascular disease in patients with diabetes stratified according to low (7.5%), intermediate (15%) and high cardiovascular risk (20%) of developing cardiovascular disease over a 10-year periodCitation39. Even at the low-risk level, aspirin was dominant over placebo in more than 85% of cases. In low-risk diabetic patients, the QALY gained over 10 years with aspirin usage was 8.10 and the cost was US$3102 (€2135 [2010 values]). In comparison, the QALY gained with no aspirin use was 8.08 and the cost was US$3750 (€2580). In high-risk diabetic patients, the QALY gained with aspirin use was 7.56 and the cost was US$6842 (€4708); the corresponding values with no aspirin use were 7.53 and US$8473 (€5831). In high-risk non-diabetic patients, the QALY gained with aspirin use was 7.67 at a cost of US$5518 (€3797); the corresponding values with no aspirin use were 7.64 and US$6822 (€4695). However, given the negative results of the latest studiesCitation23,Citation24, further clarification on diabetes definition, background level of cardiovascular risk, and factors such as sex and ethnicity are warranted to address the role of aspirin in primary prevention, and a reliable estimation of its cost effectiveness in this subset of patients.
Comparisons between aspirin and other agents
A number of analyses have compared the cost effectiveness of aspirin with statins, smoking cessation and antihypertensives in the primary prevention of cardiovascular diseaseCitation40–44. One analysis determined the costs (2003 values) associated with aspirin, antihypertensives, statins and clopidogrel per coronary event prevented in patient with a 5-year coronary risk of 10%Citation44. This analysis found that aspirin was the most cost-effective option costing £3500 (€3896, 2010 values [1 GB£ = €1.11]) per coronary event prevented. The costs associated with the other options were £12,500 (€13,914) (initial antihypertensive treatment), £18,300 (€20,369) (intensive antihypertensive treatment), £60,000 (€66,784) (clopidogrel) and £61,400 (€68,342) (simvastatin). These authors concluded that aspirin and initial antihypertensive treatment should be offered to all patients with a 5-year coronary risk of 7.5% or more, whereas statins and clopidogrel should be used in high-risk patients with a 5-year coronary risk of 15% or more.
In another analysis, which used the population from the Framingham Heart Study (n = 5209) and the Framingham Offspring study (n = 5214), estimated the transition rates for non-fatal CHD, fatal primary CHD, secondary fatal CHD, stroke and death over a 10-year period in patients using aspirin, antihypertensives, statins and in those on smoking cessation programmes (primary-care physician advice, nicotine substitutes, bupropion)Citation40. The model was based on the healthcare system and direct medical costs in the Netherlands. These authors showed that smoking cessation was the most cost-effective treatment, but least effective option and statins were the least cost-effective option, but the most effective as shown in . Depending on cardiovascular risk (moderate or high) and age (>50 or >60 years), the cost per years of life saved (YLS) ranged from €73,971 to 190,276 for statins/population; the cost/YLS ranged from €28,187 to 79,843 for antihypertensives/population, and from €2263 to 16,949 for aspirin/population; smoking cessation was a cost-saving option in all scenarios. These authors concluded that smoking cessation should be offered to all smokers, but aspirin treatment remains the most cost-effective option in the primary prevention of cardiovascular disease. Statins are expensive and should be used in patients with a 10-year CHD risk >30%. Another analysis, which explored the primary prevention of CHD in men, also concluded that aspirin was effective and less costly than no treatment in patients with a 10-year CHD risk >7.5%Citation41. The addition of a statin was cost effective in high-risk patients (those with a 10-year CHD risk >10%).
Table 3. Cost effectiveness of primary prevention of cardiovascular disease with nicotine substitutes, aspirin, antihypertensives and statins in a population at moderate risk (i.e., 10-year CHD risk 10–20%) or high risk (i.e., 10-year CHD risk ≥20%). Adapted with permission from Franco OH, et al. Primary prevention of cardiovascular disease: cost-effectiveness comparison. Int J Technol Assess Health Care 2007;23:71–79.
When the data were extrapolated to a model in BelgiumCitation40,Citation41, which included the cheapest statin (<€90 medication cost/year), the ICER per life-year gained (LYG) ranged from €29,173 to 87,022 (depending on age and cardiovascular risk) with the statin and from €3854 to 29,509 with aspirin. These authors concluded that low-cost options such as aspirin are important for the majority of the population. An analysis of patients from the Health Survey of EnglandCitation42, found that 1540/5603 patients were eligible for at least one primary-prevention intervention treatment, and 940 were eligible for three treatments. When the Joint British recommendations were applied, these authors concluded that aspirin plus two antihypertensives were more cost-effective than using four antihypertensives or statins.
Cost effectiveness of aspirin in relation to safety
Like any drug, the benefits of aspirin should be weighed against potential risks such as gastrointestinal bleeding. In patients at low-to-moderate risk of cardiovascular complications, the risk of bleeding may outweigh the benefits gained; however, in high-risk patients, the opposite seems to be true when considering aspirin monotherapy. In one analysis, aspirin was dominant from an annual cardiovascular risk of 0.2%Citation32. However, the risk : benefit ratio is likely to be an issue at such a low annual cardiovascular risk level, and the cost of treating any gastrointestinal bleeding is likely to define the cost at which low-dose aspirin becomes cost effectiveCitation45. In the ATC meta-analysis of primary-prevention trials, aspirin reduced serious vascular events by 12%, but was associated with an increased risk of gastrointestinal and extracranial bleeds compared with control (0.10 vs. 0.07% per year, respectively; p < 0.0001); these authors concluded that reduction in events needs to weighed against the risk of bleeding. The lowest risk thresholds (the risk level at which cardiovascular events prevented exceed any potential gastrointestinal harm) recommended by the USPSTF (2009) guidelines are a 10-year CHD risk ≥4% in men and a 10-year stroke risk ≥3% in womenCitation8, but these exact thresholds have not yet been examined in cost analyses.
Compared with other agents, a systematic review of aspirin and clopidogrel trials has shown that from a cost-effectiveness point of view, 833 patients would need to be treated with clopidogrel rather than aspirin to prevent one major gastrointestinal bleed per year; this would translate into an estimated $1 million (€0.7 million, 2010 values) additional direct costs/year for treatment with clopidogrel (assuming an incremental retail cost of $1460 for clopidogrel versus aspirin therapy for 1 year), which is not considered cost effectiveCitation46. A recent analysis showed that proton pump inhibitors (PPIs) which can reduce gastrointestinal bleeds are cost effective in high-risk patients using lifelong aspirin at prescription costCitation47; however, the costs associated with co-administering PPIs or H2-receptor antagonists needs to be fully explored in primary prevention.
Cost effectiveness in relation to aspirin utilisation
Underutilisation of prophylactic agents can have a major impact on long-term cost effectiveness, particularly regarding costs associated with poor prognosis. An analysis of the 1993–2003 US National Ambulatory Medical Care Survey (NAMCS) and National Hospital Ambulatory Medical Care Survey (NHAMCS), which estimated aspirin use by cardiovascular risk (high risk was defined as having cardiovascular disease, intermediate/multiple risk was defined as having diabetes mellitus, age >40 years or additional cardiovascular risk factors, and patients without these risks were defined as low risk)Citation48, showed that aspirin was underutilised in all risk categories. Aspirin was shown to be more underused than statins, despite a more favourable cost-effectiveness profile. The survey showed that use of aspirin had increased over the decade, but was still relatively low. In 2003, aspirin was used in 32.8%, 11.7% and 1–3% of high-, intermediate- and low-risk patients, respectively. Aspirin use tended to be greater in older patients, males, in hospital outpatient departments and in patients being treated by a cardiologist.
Strengths and weaknesses of this current critique
Cost-effectiveness models are an important way of making informed choices about long-term treatment strategiesCitation49; however, there is no universally agreed standard for the definition of cost effectiveness. The published aspirin models are robust – they include key trials data published to date, and indicate that prevention of first events with aspirin is cost effective for a 10-year follow-up period once risk surpasses a certain threshold. However, the main limiting factor appears to be gastrointestinal bleedsCitation45, which indicates that cost analyses should use bleeds as a threshold for treatment use in addition to 10-year risk estimates. There is also the question of what constitutes cardiovascular riskCitation50; different analyses use different criteria to define the threshold for risk, and this is confounded by controversy over sex and age effects. Using the thresholds described in guidelines may not be helpful, as this is also a grey area where differences occur. There are also some areas where further analyses are needed, such as in subgroups (defined according to risk), in women, and in individual low- to middle-income countries according to healthcare policies.
Conclusion
Overall, published models that utilise the aspirin trials show that aspirin is cost effective in preventing cardiovascular disease. In developed countries, the cost of treating gastrointestinal bleeds is the main limiting factor when considering the direct costs of aspirin in primary prevention. In European countries, the mean 10-year direct cost savings/patient associated with low-dose aspirin use is €201 (UK), €281 (Germany), €797 (Spain) and €427 (Italy) for patients with an annual CHD risk of 1.5%Citation30. In Japan, aspirin was associated with a direct cost saving/patient of €889 in patients with an annual CHD risk >1.5%Citation31. In the US, the appropriate use of aspirin in primary prevention would lead to an overall saving of direct costs of $79.6 million (€54.7 million, 2010 values) over a 10-year periodCitation33. Overall, the models show that there is a risk : benefit threshold (i.e., from low- to high-risk patients), indicating the level at which aspirin becomes cost effective; this is illustrated in .
Table 4. Cost of aspirin use (€ per country or ICER/QALY gained) according to cardiovascular risk level.
Compared with other agents, aspirin is the most cost-effective option in primary prevention, costing £3500 (€3896, 2010 values) per coronary event prevented compared with initial antihypertensive treatment (£12,500, €13,914), intensive antihypertensive treatment (£18,300, €20,369), clopidogrel (£60,000, €66,784), and simvastatin (£61,400, €68,342)Citation44. In developing countries, the use of aspirin in primary prevention will depend on the willingness of a healthcare system to pay. Estimates suggest that when the 10-year absolute risk of cardiovascular disease is >25%, the ICER/QALY gained is in the range of $746–890 (€514–613, 2010 values)Citation34. Non-adherence may also have a counterproductive role in all patients in terms of costs associated with poor prognosis and repeat medications.
Although the majority of the models explored are robust in terms of patient numbers and validated approaches, they do have a number of limitations. The models are based on a range of clinical trials, which could result in different baseline risks, and different aspirin doses. There is also the necessity for assumptions; for example, the number of patients that will transition to death. They are also confounded by controversy over factors such as sex and age. Overall, aspirin is a cost-effective option, and is likely to meet the willingness of a healthcare system to pay for any additional QALY gained in the majority of healthcare systems.
Transparency
Declaration of funding
This work was funded by an educational grant from Bayer Schering Pharma AG, Berlin, Germany.
Declaration of financial/other relationships
L.A. has disclosed that he has received consulting fees and honoraria from Bayer. K.W-J. has disclosed that he is an employee of Bayer. H.B. has disclosed that he has received consulting fees and honoraria from Bayer.
References
- Leal J, Luengo-Fernandez R, Gray A, et al. Economic burden of cardiovascular diseases in the enlarged European Union. Eur Heart J 2006;27:1610-1619
- Lloyd-Jones D, Adams R, Canethon M, et al. Heart disease and stroke statistics 2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2009;119:e21-181
- Luengo-Fernández R, Leal J, Gray A, et al. Cost of cardiovascular diseases in the United Kingdom. Heart 2006;92:1384-1389
- Pestana JA, Steyn K, Leiman A, et al. The direct and indirect costs of cardiovascular disease in South Africa in 1991. S Afr Med J 1996;86:679-684
- Azambuja MI, Foppa M, Maranhão MF, et al. Economic burden of severe cardiovascular diseases in Brazil: an estimate based on secondary data. Arg Bras Cardiol 2008;91:148-155, 163-171
- Zhai Y, Hu JP, Kong LZ, et al. [Economic burden of coronary heart disease and stroke attributable to hypertension in China]. Zhonghua Liu Xing Bing Xue Za Zhi 2006;27:744-747
- Abegunde DO, Mathers CD, Adam T, et al. The burden and costs of chronic diseases in low-income and middle-income countries. Lancet 2007;370:1929-1938
- US Preventive Services Task Force (USPSTF). Aspirin for the prevention of cardiovascular disease: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med 2009;150:396-404
- Graham I, Atar D, Borch-Johnsen K, et al. European guidelines on cardiovascular disease prevention in clinical practice: executive summary. Eur Heart J 2007;28:2375-2414
- Steering Committee of the Physicians’ Health Study Research Group. Final report on the aspirin component of the ongoing Physicians’ Health Study. N Engl J Med 1989;32:1129-1135
- Peto R, Gray R, Collins R, et al. Randomised trial of prophylactic daily aspirin in British male doctors. Br Med J (Clin Res Ed) 1988;296:313-316
- Hansson L, Zanchetti A, Carruthers SG, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomized trial. Lancet 1998;351:1755-1762
- Ridker PM, Cook NR, Lee IM, et al. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med 2005;352:1293-1304
- The Medical Research Council’s General Practice Research Framework. Thrombosis prevention trial: randomized trial of low-intensity oral anticoagulation with warfarin and low-dose aspirin in the primary prevention of ischaemic heart disease in men at increased risk. Lancet 1998;351:233-241
- Sacco M, Pellegrini F, Roncaglioni MC, et al. Primary prevention of cardiovascular events with low-dose aspirin and vitamin E in type 2 diabetic patients: results of the Primary Prevention Project (PPP) trial. Diabetes Care 2003;26:3264-3272
- Antithrombotic Trialists’ (ATT) Collaboration. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomized trials. Lancet 2009;373:1849-1860
- Bartolucci AA, Howard G. Meta-analysis of data from the six primary prevention trials of cardiovascular events using aspirin. Am J Cardiol 2006;98:746-750
- Berger JS, Roncaglioni MC, Avanzini F, et al. Aspirin for the primary prevention of cardiovascular events in women and men: a sex-specific meta-analysis of randomized controlled trials. JAMA 2006;295:306-313
- World Health Organization. Prevention of Cardiovascular Disease. Guidelines for assessment and management of cardiovascular risk. 2007. Available at: http://www.who.int/cardiovascular_diseases/guidelines/Prevention_of_Cardiovascular_Disease/en/index.html. Last Accessed 01 March, 2010
- Mancia G, Laurent S, Agabiti-Rosei E, et al. Reappraisal of European guidelines on hypertension management: a European Society of Hypertension Task Force document. J Hypertens 2009;27:2121-2158
- Khan NA, Hemmelgarn B, Herman RJ, et al. The 2009 Canadian Hypertension Education Program recommendations for the management of hypertension: Part 2—therapy. Can J Cardiol 2009;25:287-298
- American Diabetes Association. Standards of Medical Care in Diabetes—2010. Diabetes Care 2010;33(Suppl 1):S11-61
- Ogawa H, Nakayama M, Morimoto T, et al. Low-dose aspirin for primary prevention of atherosclerotic events in patients with type 2 diabetes: a randomized controlled trial. JAMA 2008;300:2134-2141
- Belch J, MacCuish A, Campbell I, et al. The prevention of progression of arterial disease and diabetes (POPADAD) trial: factorial randomised placebo controlled trial of aspirin and antioxidants in patients with diabetes and asymptomatic peripheral arterial disease. BMJ 2008;337:a1840
- Leung WY, So WY, Stewart D, et al. Lack of benefits for prevention of cardiovascular disease with aspirin in type 2 diabetic patients—a longitudinal observational study. Cardiovasc Diabetol 2009;8:57
- De Berardis G, Sacco M, Strippoli GF, et al. Aspirin for primary prevention of cardiovascular events in people with diabetes: meta-analysis of randomised controlled trials. BMJ 2009;339:b4531
- Zhang C, Sun A, Zhang P, et al. Aspirin for primary prevention of cardiovascular events in patients with diabetes: a meta-analysis. Diabetes Res Clin Pract 2010;77:211-218
- Calvin AD, Aggarwal NR, Murad MH, et al. Aspirin for the primary prevention of cardiovascular events: a systematic review and meta-analysis comparing patients with and without diabetes. Diabetes Care 2009;32:2300-2306
- Ong G, Davis TM, Davis WA. Aspirin is associated with reduced cardiovascular and all-cause mortality in type 2 diabetes in a primary prevention setting: the Fremantle Diabetes Study. Diabetes Care 2010;33:317-321
- Lamotte M, Annemans L, Evers T, et al. A multi-country economic evaluation of low-dose aspirin in the primary prevention of cardiovascular disease. Pharmacoeconomics 2006;24:155-169
- Lamotte M, Pinol C, Brotons C, et al. [Health economic evaluation of low-dose acetylsalicylic acid in the primary prevention of cardiovascular disease]. Rev Esp Cardiol 2006;59:807-815
- Tsutani K, Igarashi A, Fujikawa K, et al. A health economic evaluation of aspirin in the primary prevention of cardiovascular disease in Japan. Intern Med 2007;46:157-162
- Benedict A, Manson SC, Pan F, et al. US budget impact of increasing low dose aspirin usage for primary and secondary prevention of cardiovascular disease. Presented at the American Heart Association Quality of Care and Outcomes Research in Cardiovascular Disease and Stroke Conference, Washington, DC, Apr 23--25, 2009, Poster 75
- Gaziano TA, Opie LH, Weinstein MC. Cardiovascular disease prevention with a multidrug regimen in the developing world: a cost-effectiveness analysis. Lancet 2006;368:679-686
- Robberstad B, Hemed Y, Norheim OF. Cost-effectiveness of medical interventions to prevent cardiovascular disease in a sub-Saharan African country – the case of Tanzania. Cost-Eff Resour Alloc 2007;5:3
- Greving JP, Buskens E, Koffijberg H, et al. Cost-effectiveness of aspirin treatment in the primary prevention of cardiovascular disease events in subgroups based on age, gender, and varying cardiovascular risk. Circulation 2008;117:2875-2883
- Pignone M, Earnshaw S, Pletcher MJ, et al. Aspirin for the primary prevention of cardiovascular disease in women: a cost-utility analysis. Arch Intern Med 2007;167:290-295
- Algra A, Greving JP. Aspirin in primary prevention: sex and baseline risk matter. Lancet 2009;373:1821-1822
- Moeremans K, Lamotte M, Wittrup-Jensen K. The health economic value of aspirin in the primary prevention of cardiovascular disease in diabetic patients. Presented at the 69th Scientific Sessions of the American Diabetes Association, New Orleans, LA, Jun 5--9, 2009. Abstract 44-OR
- Franco OH, der Kinderen AJ, De Laet C, et al. Primary prevention of cardiovascular disease: cost-effectiveness comparison. Int J Technol Assess Health Care 2007;23:71-79
- Pignone M, Earnshaw S, Tice JA, et al. Aspirin, statins, or both drugs for the primary prevention of coronary heart disease events in men: a cost-utility analysis. Ann Intern Med 2006;144:326-336
- Marshall T. The cost-effectiveness of drug treatments for primary prevention of cardiovascular disease: a modeling study. Eur J Cardiovasc Prev Rehab 2006;13:523-528
- Neyt M, De Laet C, Van Brabandt H, et al. Cost-effectiveness of statins in the primary prevention of cardiovascular disease: a systematic review and economic analysis for Belgium. Acta Cardiol 2009;64:1-10
- Marshall T. Coronary heart disease prevention: insights from modeling incremental cost effectiveness. BMJ 2003;327:1264
- Annemans L, Lamotte M, Kubin M, et al. Which patients should receive aspirin for primary prevention of cardiovascular disease? An economic evaluation. Int J Clin Pract 2006;60:1129-1137
- McQuaid KR, Laine L. Systematic review and meta-analysis of adverse events of low-dose aspirin and clopidogrel in randomized controlled trials. Am J Med 2006;119:624-638
- Saini SD, Schoenfeld P, Fendrick AM, et al. Cost-effectiveness of proton pump inhibitor cotherapy in patients taking long-term, low-dose aspirin for secondary cardiovascular prevention. Arch Intern Med 2008;168:1684-1690
- Stafford RS, Monti V, Ma J. Underutilization of aspirin persists in US Ambulatory Care for the Secondary and Primary Prevention of Cardiovascular Disease. PLoS Med 2005;12:e353
- Gaziano TA. Reducing the growing burden of cardiovascular disease in the developing world: disease burden can be lowered with cost-effective interventions, especially by reducing the use of tobacco around the world. Health Aff (Millwood) 2007;26:13-24
- Sartore ME, Kamal KM. Costs and thresholds in cost-effectiveness analysis. Aliment Pharmacol Ther 2007;26:1455-1456