Abstract
Objective:
This investigation estimated medical costs attributable to treatment of patients diagnosed with atherosclerosis in routine US clinical practice.
Methods:
Using Medstat MarketScan claims data, direct costs of care and rates of cardiovascular (CV) events (i.e., myocardial infarction, stroke, revascularization) were examined for patients ≥18 years of age with and without a diagnostic code for atherosclerosis from 1/1/2002 through 12/31/2004. Patients with an atherosclerosis ICD-9 code who had no history of CV events in the preceding 12 months (n = 75,469) were evaluated. A comparison cohort (n = 238,702) was matched on age, gender, geographic region, enrollment time period, and Charlson comorbidity index to estimate incremental costs attributable to atherosclerosis. Differences between patient groups were tested for CV event rates per 1,000 patients and monthly costs for 6 and 12 months before and after diagnosis.
Results:
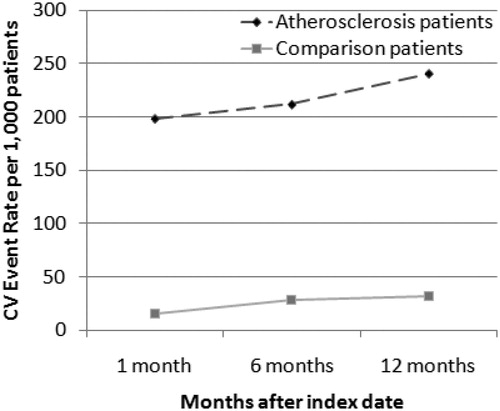
Patients had a mean age of 58 years, 52% men, and a comorbidity index of 0.49. Patients diagnosed with atherosclerosis had significantly higher (p < 0.001) rates of CV events (240/1000) after diagnosis, compared with patients without atherosclerosis (32/1000). Mean direct cost of care for patients diagnosed with atherosclerosis was $579/month for 12 months before and $1,074/month for 12 months after diagnosis, an 85% increase. Change in mean annual costs pre/post-index date was $5,232 ($436/month) higher among patients with than those without atherosclerosis (p < 0.001).
Limitations:
The study population was restricted to patients with diagnosed clinical atherosclerosis based on specific ICD-9 codes. Matching of the patient cohorts was based on observed characteristics and other unobserved differences may exist.
Conclusions:
Patients with diagnosed atherosclerosis incur significant clinical and economic burden, indicating a need for earlier diagnosis and treatment of atherosclerosis to help in reducing this burden.
Introduction
Atherosclerosis, the underlying cause of cardiovascular events, is a chronic, progressive, inflammatory disease with a long asymptomatic phaseCitation1. As atherosclerosis progresses, it can lead to the occurrence of cardiovascular events including myocardial infarction (MI), sudden cardiac death, and strokeCitation1. Atherosclerosis is widely prevalent throughout the worldCitation2,Citation3. Each year approximately 700,000 American men and women have their first coronary event (e.g., myocardial infarction), and an additional 500,000 have a recurrent eventCitation2.
Atherosclerotic disease places a substantial economic burden on society. Total annual costs for coronary heart disease in the US are estimated at $151.6 billionCitation2. When other types of cardiovascular disease are included, the total annual costs rise to $431.8 billionCitation2. These costs are largely driven by the hospital care provided to patients with MI, stroke, or revascularization proceduresCitation2. The REACH registry (Reduction of Atherothrombosis for Continued Health) demonstrated the high cost of hospitalization and medications for patients with atherothrombosisCitation4,Citation5. However, little is known about the actual costs of care incurred at the health plan, patient or employer level for patients diagnosed with atherosclerosis. The purpose of the present study was to determine the incremental cost of atherosclerosis among patients treated in routine clinical practice by comparing costs with patients not diagnosed with atherosclerosis after matching for age, gender, geographic region, enrollment time period, and comorbidity from a payer (e.g., health plan, employer, government) perspective.
Methods
A retrospective cohort study was conducted of patients with a diagnostic code for atherosclerosis and matched to a comparison cohort of patients without an atherosclerosis diagnostic code using administrative claims data from the Medstat MarketScan databases. The MarketScan databases include the Commercial Claims and Encounter database and Medicare Supplemental and Coordination of Benefit database of healthcare claims from large employers, managed-care organizations, and Medicare across the US (all 50 states). The data include the working population as well as those receiving Medicare supplemental insurance paid for by employers throughout the US. More than 35 million patients are included in the databases, encompassing employees, their spouses and dependents who are covered by employer-sponsored private health insurance including fee-for-service and managed care plans (preferred provider organizations, point of service plans, indemnity plans, and health maintenance organizations).
Eligible patients were ≥18 years of age as of January 1, 2001, and were continuously enrolled in the health plan for at least 12 months preceding and 3 months after the index date. At least 3 months of follow-up after the index date was used to reduce selection bias (exclusion of sicker patients who die before end of follow-up period) and to examine costs at 6 and 12 months post-diagnosis. Patients were excluded if they had an acute MI, stroke, transient cerebral ischemia (TIA), coronary artery bypass graft (CABG), or other revascularization procedure in the 12 months prior to the index date. Eligible atherosclerosis patients had at least one medical claim (inpatient or outpatient) for an encounter for coronary or cerebral atherosclerosis (ICD-9 diagnostic code of 414.x, 437.0, 437.1, 437.3, or 440.x) from January 1, 2002 through December 31, 2004. ICD-9 code of 414.x included coronary atherosclerosis, aneurysm of the heart, and ischemic heart disease. ICD-9 code of 437.0, 437.1, and 437.3 included cerebral atherosclerosis and cerebral aneurysm, and ICD-9 code 440.x included atherosclerosis of the extremities and general atherosclerosis. Patients with a diagnosis of ischemic heart disease, peripheral vascular disease, or diabetes without a diagnosis specifically for atherosclerosis were not included in the study. The study included patients with clinically documented and coded (i.e., ICD-9 code) atherosclerosis. The date of the diagnosis of atherosclerosis was the start (index) date. The comparison cohort was patients with no diagnostic code for atherosclerosis in the 12 months before the index date and was matched for age, gender, region, enrollment time period, and comorbidity to eligible atherosclerosis patients.
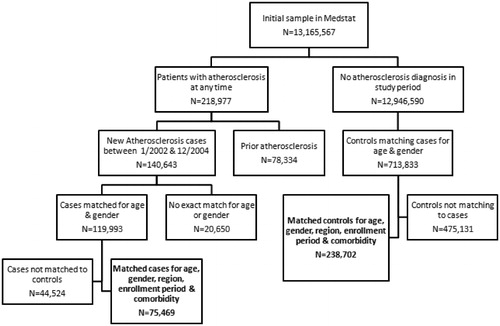
The matching was done in a two-step approach. The first step matched the comparison patients on age (±1 year), gender, geographic region, and enrollment window (±1 month, in the database at the same time). These initially matched comparison patients were then assigned the same start date as their atherosclerosis patient. Using the index date, further matching was done on the Charlson comorbidity index (±0.1)Citation6. Comparison patients were matched to the atherosclerosis patients for up to six matches, with a mean of four comparison patients to one atherosclerosis patient. The inverse of the match rate was used as a sample weight to account for the ‘oversampling’ of comparison patients for easier-to-match atherosclerosis patients. The number of patients included versus excluded and matched versus no match is shown in .
Study outcomes
The primary outcomes of interest were: (1) the rate of cardiovascular events (MI, TIA/stroke, revascularization) for the 12 months of follow-up, and (2) total direct cost of care and incremental cost for up to 24 months of follow-up for atherosclerosis patients and comparison patients. Cardiovascular-related and non-cardiovascular deaths were not included in the analysis because the administrative database did not track and verify patient death. Costs were derived from claims for office/outpatient visits, outpatient prescriptions, laboratory/diagnostic tests, medical procedures, emergency room visits, and hospitalizations. Costs were defined as the allowed charge for hospital, medical (inpatient and outpatient physician, diagnostics, laboratory), and pharmacy claims, comprising the amount paid by the insurance plan plus the patient copayment, deductible, and coinsurance. Payments for all claims were standardized to 2004 dollars based on the value of the Consumer Price Index – Medical Care Services, for the month of payment, relative to the CPI–Medical Care Services annual value for 2004.
Costs during follow-up were also stratified by the primary diagnosis to determine which costs were cardiovascular related. Claims with a primary diagnosis of atherosclerosis (same ICD-9 codes as listed above) were classified as atherosclerosis related. Claims with a primary diagnosis of cardiac event or intervention (ICD-9 and CPT codes for aortic aneurysm, MI, coronary angioplasty, coronary endarterectomy, rechanneling of artery, atherectomy, angiectomy, CABG) were classified as cardiovascular related. Claims with a primary diagnosis of cerebrovascular event or intervention (ICD-9 and CPT codes for carotid endarterectomy, occlusion of precerebral and cerebral arteries, TIA, and cerebrovascular disease) were classified as cerebrovascular related. In a subgroup analysis, patients with atherosclerosis and diabetes were compared with their matched comparison cohort with diabetes and no atherosclerosis diagnosis.
Statistical analysis
The cumulative rate of cardiovascular events (number of events/number of patients at specified time period/per 1,000 patients) occurring up to 12 months of follow-up (1, 6, and 12 months) was calculated for atherosclerosis and comparison patients. Monthly direct costs of care, including inpatient, outpatient, pharmacy, and total costs, were computed per patient because patients had variable lengths of follow-up. The monthly costs were tabulated only for those patients with complete follow-up for the specified time period. Monthly costs of care were computed for patients who had complete follow-up data for 6 months, 12 months, and 24 months after the index date. To estimate the incremental cost of care attributable to atherosclerosis, the difference in pre- versus post-index date costs was computed and then the pre–post difference among atherosclerosis patients was subtracted from the pre–post difference among the comparison patients. Mean and median costs were calculated.
Results
A total of 75,469 patients with a diagnostic code for atherosclerosis from January 1, 2002, through December 31, 2004, and no history of a cardiovascular event (i.e., MI, TIA/stroke, revascularization) in the previous 12 months were matched to 238,702 comparison patients who had no diagnosis of atherosclerosis. The matching resulted in similar characteristics for the comparison group on age, gender, region, enrollment time period, and Charlson comorbidity index ().
Table 1. Characteristics of atherosclerosis patients (ICD-9 diagnostic code for coronary or cerebral atherosclerosis) and matched comparison patients.
Cardiovascular event rates
Overall, there were 240 cardiovascular events per 1,000 patients diagnosed with atherosclerosis compared with 32 cardiovascular events per 1,000 comparison patients in the 12 months after diagnosis (). At 1 month after diagnosis of atherosclerosis, there were 22.4 MIs per 1,000 patients with atherosclerosis and 0.9 per 1,000 comparison patients. The higher MI rate among patients with atherosclerosis compared with patients without atherosclerosis continued through 12 months after diagnosis, with 26.4 MIs per 1,000 patients with atherosclerosis and 1.9 MIs per 1,000 comparison patients. A similar pattern of significantly higher TIA/stroke rates among patients diagnosed with atherosclerosis compared with patients without atherosclerosis was evident throughout the 12 months, 106.4 strokes per 1,000 patients with atherosclerosis versus 23.2 strokes per 1,000 comparison patients. At 12 months after diagnosis, there was a very low rate of revascularization among comparison patients (7 per 1,000) versus a rate of 107 procedures per 1,000 patients diagnosed with atherosclerosis. The incidence rate per 1,000 patients was significantly higher at 1 month of follow-up than the rate at 6 months and 12 months of follow-up (p < 0.0001).
Cardiovascular events in patients with diabetes
Patients with diabetes in both the diagnosed atherosclerosis and the comparison cohorts were identified for a subgroup analysis. For the subgroup of patients with diagnosed atherosclerosis and diabetes mellitus (very high CHD risk), there were 10,842 patients with both conditions (10% of total atherosclerosis group) who were matched (original matching on age, gender, region, enrollment time period, and comorbidity) to 14,188 comparison patients with diabetes (4% of comparison cohort). No additional matching was done; only the subset of patients with diabetes was selected. The subgroup of patients with diabetes was similar in age and gender to the total sample but had a higher Charlson comorbidity index due to the diabetes diagnosis. The cardiovascular event rate at 12 months of follow-up for this subgroup was 239 events per 1,000 patients with atherosclerosis and diabetes versus 39.8 events per 1,000 comparison patients with diabetes but no atherosclerosis.
Direct cost of care
Including patients with complete follow-up for each time period, total monthly direct cost of care was estimated for 6 and 12 months prior to the index date and for 6, 12, and 24 months after the index date. Overall cost of care among patients diagnosed with atherosclerosis was significantly higher through 12 months after diagnosis compared with patients without atherosclerosis (p < 0.001) (). Among patients diagnosed with atherosclerosis, mean monthly costs were $835 over the 6 months before diagnosis and $1,522 over the 6 months after diagnosis, an 82% increase. An 85% increase for 12 months and 200% increase for 24 months were observed for total monthly costs for patients diagnosed with atherosclerosis. For comparison patients, total monthly costs were higher after the index date, but the increase was small: 20% for 6 months, 28% for 12 months, and 41% for 24 months.
Figure 3. Overall monthly pre- and post-index date direct cost of care at 6 and 12 months for atherosclerosis patients and comparison cohort. Each time period includes those patients with complete follow-up for the specified period.
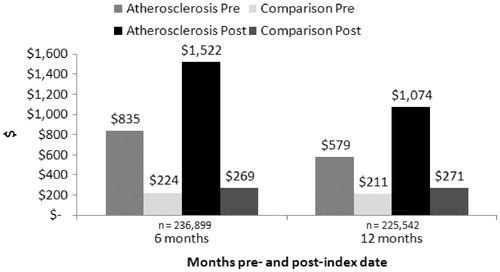
Comparing monthly costs between patients with and without atherosclerosis, patients diagnosed with atherosclerosis had significantly higher costs before and after the index date (p < 0.001). The incremental, attributable cost of atherosclerosis was $643 per month at 6 months after the index date, taking into account the difference between costs before and after the index date (). At 12 months, the incremental cost was $436 per month, or an additional $5,232 spent on patients with atherosclerosis compared with patients of similar age and health status. Inpatient costs accounted for a large portion of the incremental costs. The incremental cost for inpatient care was $429 per month and outpatient care incremental cost was $165 per month at 6 months ().
Table 2. Component costs of care and cost difference for 6 and 12 months before and after the index date for atherosclerosis patients and comparison cohort.
Cost of care among patients with diabetes
The very high-risk patients with atherosclerosis and diabetes had significantly higher costs before and after the index date compared with the matched comparison cohort (p < 0.001) (). The incremental, attributable cost of atherosclerosis among this diabetes cohort was $627 per month at 12 months of follow-up, an additional $7,524 for that time period. Patients with diabetes, both with and without atherosclerosis, had higher cost of care than the total sample of patients.
Table 3. Total costs of care and cost difference at 12 months before and after the index date for patients with diabetes mellitus.
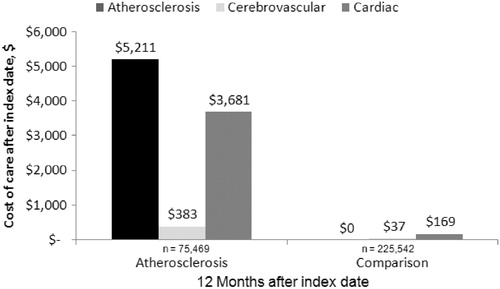
Cardiovascular-related costs
The cost of care was stratified for the total sample into four categories by the primary diagnosis provided when the services were rendered: atherosclerosis, cerebrovascular, cardiac, or other. This stratification was performed to determine what proportion of the total costs was cardiovascular related. At 12 months of follow-up, $9,275 of the total cost of care ($13,879) was cardiovascular-related for patients diagnosed with atherosclerosis. Approximately 56% of the cardiovascular-related costs were for atherosclerosis, and 40% were for cardiac care (). For comparison patients, $206 of the $3,102 total costs were cardiovascular-related costs, significantly lower than those for patients with atherosclerosis. A similar pattern was observed at 24 months of follow-up, yet cardiovascular-related costs were higher at 24 months compared with 12 months of follow-up for patients with ($11,766) and without atherosclerosis ($353).
Discussion
Atherosclerosis condition is costly for employers, Medicare, and health plans. After accounting for the cost of care among matched comparison patients without atherosclerosis, the 12-month cost differential was $5,232 more among patients diagnosed with atherosclerosis. Overall, patients with atherosclerosis cost $12,888 in the 12 months after diagnosis. The incremental cost is largely driven by the cardiovascular-related costs and events. The rate of cardiovascular events was significantly higher among patients diagnosed with atherosclerosis over the 12 months after diagnosis. This same pattern of higher costs and substantial incremental costs attributable to atherosclerosis also was found in the group with diabetes. To the authors’ knowledge, this is the first study examining the cost of atherosclerosis (as opposed to cost of cardiovascular events) among patients treated in routine clinical practice.
The present study confirms the high medical and economic burden of atherosclerosis and cardiovascular disease as reported in other studiesCitation4,Citation5,Citation7,Citation8. The Reduction of Atherothrombosis for Continued Health (REACH) registry found high costs of hospitalization and medications that increased as the number of affected arterial beds increasedCitation4. Mean annual hospitalization costs were reported as $2,864 per patient with one affected arterial bed. The present study expands on this knowledge by comparing costs with patients without a diagnosis of atherosclerosis to provide the incremental cost burden of atherosclerosis. Also, the present study did not include cardiovascular deaths which have a different clinical and economic impact which makes the findings different from studies like the REACH registry that used a composite measure of CV death, MI, stroke, or hospitalization for revascularizationCitation4,Citation5.
The higher rate of CV events among patients with a diagnosis of atherosclerosis was expected. However, the majority of the cardiovascular events that occurred after a diagnosis of atherosclerosis took place shortly after the diagnosis was recorded (1 month). Thus, the cost of care for patients diagnosed with atherosclerosis was greatest in the short term. This pattern may indicate that the diagnosis of atherosclerosis may be made late, when a cardiovascular event is imminent, limiting the time frame for preventive action. This pattern also indicates that therapies that work in the short term to slow the progression of atherosclerosis may be desirable.
To put the cost of atherosclerosis into context with other chronic health conditions, retrospective managed care database studies have found the cost of type 2 diabetes mellitus to be between $3,385 and $9,031, with higher costs among patients with diabetes and cardiovascular comorbidity (total 12-month costs between $10,450 and $12,550)Citation9,Citation10. Mean respiratory-related healthcare costs were $7,240 for patients in a Medicare Advantage population with chronic obstructive pulmonary disease (COPD) and asthma and $5,158 for patients with COPD without asthmaCitation11. Mean all-cause cost for patients with bipolar disorder was $6,826 in the year following the first bipolar-related claimCitation12. Differences in the study populations, databases, and analytic approach will produce different cost estimates. The current study findings put atherosclerosis in line with common diseases and conditions widely viewed as economically burdensome within the healthcare payer community.
The matching of patients diagnosed with atherosclerosis with patients without atherosclerosis in the present study allowed for the computation of incremental cost due to atherosclerosis rather than making assumptions about whether a claim was disease related or not. Other retrospective database studies have not used a comparison cohort but rather utilized the diagnosis code associated with the claimCitation11,Citation13,Citation14. This method requires assumptions to be made based on using the primary diagnosis or all diagnoses and may assign a cost as disease related when it may not be, thus overestimating the cost attributable to the disease. In the present study, the matching of the comparison cohort to the patients with atherosclerosis allowed for computing the attributable cost of atherosclerosis (subtracting any non-atherosclerosis-related costs). In addition, the subtraction of the difference between pre- and post-index date costs within each group (atherosclerosis and comparison groups) before computing the incremental cost adjusted for any difference in costs before and after diagnosis.
The study findings should be interpreted in light of several limitations. Patients included in the study were required to have an ICD-9 diagnosis of atherosclerosis because imaging studies were not routinely done and the results of the imaging tests were not available in the administrative claims database. Therefore, we were able to study only patients with known clinical atherosclerosis. Patients with clinical atherosclerosis who did not receive a specific diagnostic code for atherosclerosis (ICD-9 code = 414, 440, 437) were excluded from this study. Also, the specificity of the atherosclerosis diagnosis was limited to the specificity of the ICD-9 codes. It is possible that some of the ICD-9 codes used in the study for revascularization could have been for peripheral vascular disease. Clinicians may have recorded the cardiovascular event (e g., MI or stroke) without recording an atherosclerosis diagnosis code, and these patients were excluded from the analysis. In addition, atherosclerosis often presents in an advanced stage upon diagnosisCitation15, but severity of atherosclerosis is unknown in this study because data were not available from diagnostic tests. To address this limitation of the atherosclerosis diagnosis, a subgroup analysis was conducted of patients diagnosed with atherosclerosis who had a cardiac diagnostic test within the 3 months prior to their diagnosis. The results of the cardiac testing were not available, but it was assumed that these patients had clinical symptoms leading the physician to perform angiography, cardiac stress test, or cardiac imaging. A similar pattern of cardiovascular event rates (224 events per 1,000 patients at 12 months of follow-up) was observed among the 14,563 patients with diagnosed atherosclerosis and a prior cardiac diagnostic test as was observed for the total sample. Comparing monthly costs, patients diagnosed with atherosclerosis who had a prior cardiac diagnostic test had significantly higher costs before and after the index date (p < 0.001). These consistent results support the validity of the study findings from the total sample.
Selection bias was possible because of the observational nature of the study; however, the data set was a large, national administrative database, which should make the findings generalizable to other large national healthcare plans. The matching of the cohorts was done using observed characteristics; there may have been other unobserved differences between the groups that were not adjusted for in the matching. Costs reported in this study were in 2004 dollars; costs expressed in 2009 dollars would be 23.7% higher, based on the change in the Consumer Price Index – Medical Care Services from 2004 to 2009. The results from our usual-care study approximate the management and treatment patterns in actual clinical practice.
Conclusion
This observational study of patients diagnosed with atherosclerosis showed a significant clinical and economic burden of atherosclerosis. The results indicated a need for earlier diagnosis and treatment of atherosclerosis. Interventions aimed at effectively managing and treating this condition may help to reduce the clinical and economic burden of atherosclerosis for patients and the healthcare system. Further research should examine the cost effectiveness of therapeutic intervention initiated earlier in the course of atherosclerosis development that prevents future cardiovascular events in patients with atherosclerosis.
Transparency
Declaration of funding
This research was supported by funding from AstraZeneca LP.
Declaration of financial/ other relationships
R.L.O. and K.M.F. have disclosed that they have received grants from AstraZeneca LP to conduct this study. S.K.G. and M.F.B. have disclosed that they are employees and stockholders of AstraZeneca LP. M.D. has disclosed that he is a consultant to AstraZeneca LP.
References
- Toth PP. Subclinical atherosclerosis: what it is, what it means and what we can do about it. Int J Clin Pract 2008;62:1246-1254
- American Heart Association. Heart Disease and Stroke Statistics: 2007 Update. Dallas, TX. American Heart Association, 2007
- Coronary Heart Statistics 2008: United Kingdom. Available athttp://www.ws3.heartstats.web.baigent.net/datapage.asp?id=7998 [Accessed October 2009]
- Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373-383
- Bakhai A. The burden of coronary, cerebrovascular and peripheral arterial disease. Pharmacoecon 2004;22(Suppl 4):11-18
- Leys D. Atherothrombosis: a major health burden. Cerebrovasc Dis 2001;11(Suppl 2):1-4
- Mahoney EM, Wang K, Cohen DJ, et al. One-year costs in patients with a history of or at risk from atherothrombosis in the United States. Circ Cardiovasc Qual Outcomes 2008;1:38-45
- Steg PG, Bhatt DL, Wilson PWF, et al. One-year cardiovascular event rates in outpatients with atherothrombosis. JAMA 2007;297:1197-1206
- Gandra SR, Lawrence LW, Parasuraman BM, et al. Total and component health care costs in a non-Medicare HMO population of patients with and without type 2 diabetes and with and without macrovascular disease. J Manag Care Pharm 2006;12:546-554
- Mody R, Kalsekar I, Kavookjian J, et al. Economic impact of cardiovascular co-morbidity in patients with type 2 diabetes. J Diabetes Complications 2007;21:75-83
- Blanchette CM, Gutierrez B, Ory C, et al. Economic burden in direct costs of concomitant chronic obstructive pulmonary disease and asthma in a Medicare Advantage population. J Manag Care Pharm 2008;14:176-185
- Harley C, Li H, Corey-Lisle P, et al. Influence of medication choice and comorbid diabetes: the cost of bipolar disorder in a privately insured US population. Soc Psychiatr Epidemiol 2007;42:690-697
- Etemad LR, McCollam PL. Total first-year costs of acute coronary syndrome in a managed care setting. J Manag Care Pharm 2005;11:300-306
- Margolis J, Barron JJ, Grochulski D. Health care resources and costs for treating peripheral artery disease in a managed care population: results from analysis of administrative claims data. J Manag Care Pharm 2005;11:727-734
- Kiechl S, Willeit J, for the Bruneck Study Group. The natural course of atherosclerosis. Part I: incidence and progression. Arterioscler Thromb Vasc Biol 1999;19:1484-1490