Abstract
Objective:
To compare the healthcare costs of pre-dialysis chronic kidney disease (CKD) patients cared for in a nephrology clinic setting versus other care settings.
Methods:
An analysis of health claims between 01/2002 and 09/2007 from the Ingenix Impact Database was conducted. Inclusion criteria were ≥18 years of age, ≥1 ICD-9 claim for CKD, and ≥1 estimated glomerular filtration rate (eGFR) value of <60 mL/min/1.73 m2. Patients were classified in the nephrology care cohort if they were treated in a nephrology clinic setting at least once during the study period. Univariate and multivariate analyses were conducted to compare average annualized healthcare costs of patients in nephrology care versus other care settings.
Results:
Among the 20,135 patients identified for analysis, 1,547 patients were cared for in a nephrology clinic setting. Nephrology care was associated with lower healthcare costs with an unadjusted cost savings of $3,049 ($11,303 vs. $14,352, p = 0.0014) and a cost ratio of 0.8:1 relative to other care settings. After adjusting for covariates, nephrology care remained associated with lower costs (adjusted cost savings: $2,742, p = 0.006).
Limitations:
Key limitations included potential inaccuracies of claims data, the lack of control for patients’ ethnicity in the calculation of eGFR values, and the presence of potential biases due to the observational design of the study.
Conclusions:
The current study demonstrated that pre-dialysis CKD patients treated in nephrology clinics were associated with significantly lower healthcare costs compared with patients treated in other healthcare settings.
Introduction
Chronic kidney disease (CKD) affects an increasing number of people and the cost of treatment is a significant contributor to health-related expenditures. In 2007, costs for Medicare patients with CKD reached $57.5 billion – more than five times greater than costs in 1993Citation1. Although the absolute amount is lower for end-stage renal disease (ESRD), with Medicare total expenditure of approximately $24 billion in 2007, the per-patient-per-month costs are much higher at nearly $15,000 during the transition phase to ESRD, as opposed to $2,202 for pre-dialysis CKD patientsCitation1. As such, treatment of CKD has been shown to be cost effective as it slows disease progression and prevents the development of comorbiditiesCitation2,Citation3. In 2007, per patient per month costs were $688 for Medicare patients with CKD alone, but rose to $2,558 in patients with CKD, diabetes, and cardiovascular diseaseCitation1.
CKD is also associated with multiple comorbidities and complications including cardiovascular disease, hypertension, anemia, malnutrition, and metabolic bone diseaseCitation4. To assist healthcare providers managing these comorbidities and complications of CKD, the Kidney Disease Outcomes Quality Initiative (KDOQI) developed a series of evidence-based guidelines to improve patient outcomesCitation4. These guidelines include CKD stage-specific recommendations to screen for and treat the complications of CKD if they are present.
CKD patients are managed in several care settings such as primary care, internal medicine, endocrinology, and nephrology specialty care. Because comorbidities and hospitalizations constitute the main healthcare costs of CKD, it might be possible to achieve better economic and clinical outcomes if patients are referred early to nephrologistsCitation2,Citation5. Patients with late nephrologist referral have greater short-term morbidityCitation6,Citation7, greater rate of dialysis initiationCitation7–10, and prolonged initial hospitalizationCitation7–9,Citation11,Citation12. Too often, patients are referred to nephrologists when renal failure is already advancedCitation13.
It is hypothesized that more advanced CKD patients not treated by nephrologists would incur greater healthcare costs. Despite available information regarding the cost burden associated with CKD, no study has of yet considered the potential cost impact associated with nephrology care versus care from other practitioners in CKD patients. The objective of this study was to compare the healthcare costs from a managed care perspective for patients cared for in nephrology clinic settings (nephrology care) versus other care settings.
Patients and methods
Data source
Health insurance claims data from the Ingenix Impact National Managed Care (IMPACT) database between January 2002 and September 2007 were used to conduct the analysis. This large national database was designed to support benchmarking projects, healthcare outcomes research, and other research initiatives. The IMPACT database includes complete medical and pharmacy claims for more than 80 million managed-care lives, covering all census regions of the US. Data elements used in the present analysis included health-plan enrollment records, patient demographics, inpatient and outpatient medical services, outpatient prescription drug dispensing records, and laboratory results. Laboratory results from the IMPACT database are available for the subset of patients within a given carrier's laboratory network, representing approximately 10% of the IMPACT population. Finally, data included in the IMPACT database are de-identified and comply with the Health Insurance Portability and Accountability Act of 1996.
Study design
Included in the study were patients ≥18 years old, who had ≥1 claim for CKD (ICD-9 codes: 250.4, 285.21, 403–404, 585–586, and 588), ≥1 estimated glomerular filtration rate (eGFR) value of <60 mL/min/1.73 m2, and ≥2 hemoglobin (Hb) assessments. Patients were further required to have continuous health-plan coverage throughout their observation period. Patients with cancer, lupus, or those who had received an organ transplant or chemotherapy were excluded from the analysis. If a patient had received renal dialysis, data were censored 30 days prior to the first date of dialysis to avoid skewed data coming from the period of tests and procedures generally performed prior to renal dialysis initiation.
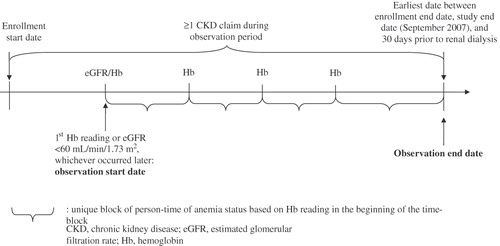
The observation period spanned from the date of first Hb reading or eGFR reading <60 mL/min/1.73 m2, whichever occurred later, until the end of the health-plan enrollment, the defined study end date of September 2007, or 30 days prior to renal dialysis, whichever occurred first ().
Definition of CKD Based on eGFR
Glomerular filtration rate values were estimated based on serum creatinine value, age, gender, and ethnicity, using the Modification of Diet in Renal Disease (MDRD) study abbreviated equationCitation14.
where SCr = serum creatinine value. Since the patients’ ethnicity is not available in the IMPACT database, this variable was not included in the calculation. This missing information has the effect of underestimating eGFR by 21% for black patients.
Definition of study groups
Patients were considered part of the nephrology care cohort if they were treated in a nephrology care setting at least once during the study period. Patients treated in primary care and/or other settings, including internal medicine and endocrinology settings comprised the other care cohort. Patients’ observation periods were further stratified into anemia versus non-anemia periods based on their Hb values. A retrospective open-cohort design approach was adopted, allowing a patient's anemia status to change over time, which reflects real-world situations (). Based on the value of the closest Hb reading to the beginning of the observation period, patients were classified as either anemia or non-anemia up to the following reading where patients were re-classified based on the new Hb value. Anemia status was defined as Hb <11 g/dL, as the 2007 KDOQI guidelines for anemia in CKD recommend that Hb levels be maintained between 11 g/dL and 12 g/dL for dialysis and non-dialysis CKD patientsCitation15. Patients were also stratified according to their CKD stage at baseline: patients with eGFR between 30.0 and 59.9 were classified in CKD stage 3, between 15.0 and 29.9 in CKD stage 4, and <15.0 in CKD stage 5.
Statistical analysis
Both univariate and multivariate analyses were conducted to compare weighted average annualized healthcare costs between patients cared for in a nephrology care setting versus other care settings, and to compare weighted average annualized healthcare costs for these two cohorts stratified by anemia status and baseline CKD stage. The healthcare costs were composed by three mutually exclusive components: (1) outpatient services, (2) inpatient services, and (3) pharmacy costs. Average weighted annualized direct costs were reported to adjust for different lengths of patients’ observation duration. The observation period of each patient was used as the weight; therefore, the normalized per-patient cost represents the mathematical equivalent of a standard per-patient-per-year value (i.e., aggregated costs divided by aggregated years, with both values summed across all patients), but with a value for each patient, allowing for statistical testing.
Descriptive univariate statistics were used to summarize annualized healthcare costs. Both cost differences and cost ratios were reported. Cost difference was defined as the average annualized cost of patients cared for in nephrology care settings minus the average annualized cost of patients cared for in other care settings. Cost ratio was defined as the ratio of the average annualized cost of patients in nephrology care settings and the average annualized cost of patients cared for in other care settings.
Multivariate analyses were performed using linear regressions to control for potential confounding factors in the estimation of the cost associated with nephrology-care settings. Because of the non-normality of the healthcare cost outcome variables, which are truncated at zero and positively skewed, standard errors associated the parameter estimates from a linear regression may be biased. To this effect, statistical inference for adjusted cost difference estimates was based on the permutation test, a non-parametric approach. The permutation test is similar to the bootstrap test in its iterative process; however, as opposed to the bootstrap method where replications are computed on resample with replacements, the permutation replications are computed without replacement. Patients are reallocated to either one of the two groups at each replication. The permutation test is thus performed under the null hypothesis that there is no difference in the distribution of healthcare costs between patients cared for in nephrology clinic settings versus other care settings. Variables of control used in the regression were age, gender, baseline eGFR (except for the analyses stratified by CKD stage at baseline) and Hb, presence of hypertension, diabetes, cardiac arrest, cardiac arrhythmia, congestive heart failure, stroke, coronary artery disease, acute myocardial infarction, and left ventricular hypertrophy. A two-sided alpha error of 0.05 was used to declare statistical significance. All statistical analyses were performed using SAS version 9.1 (SAS Institute Inc., Cary, NC, USA).
Results
presents the patients' disposition chart. A total of 20,135 patients met the inclusion/exclusion criteria and formed the study population. Of these patients, 1,547 (8%) were treated in a nephrology care setting at least once during the observation period, and 5,701 (28%) had at least one period of anemia (Hb level <11 g/dL). presents the study population characteristics for the nephrology care cohort and the other care cohort. The nephrology care cohort comprised of fewer women (38.2% vs. 43.5%, p < 0.0001) and were slightly younger (years, 59.6 vs. 61.2, p < 0.0001) compared with the other care cohort. A greater proportion of patients cared for in nephrology clinics had more advance CKD stage (4 and 5) compared with those treated in other care settings (p < 0.0001). Except for hypertension, which was more prevalent in the nephrology care cohort, patients in the other care cohort had more comorbidities (diabetes, coronary artery disease, left ventricular hypertrophy, myocardial infarction, p < 0.05 for all) at baseline.
Figure 2. Patients’ disposition. *Defined as ≥1 CKD claim + ≥1 eGFR <60 mL/min/1.73 m2 + ≥2 Hb readings; †Categories not mutually exclusive. CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate; Hb, hemoglobin.
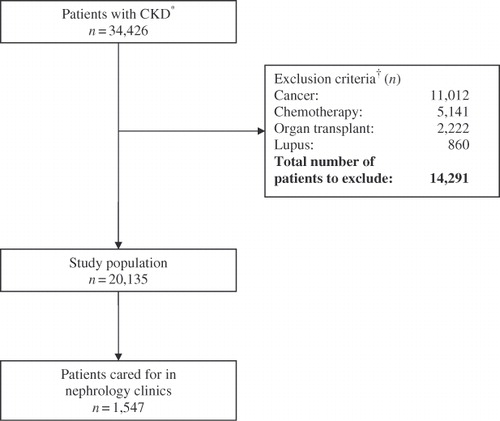
Table 1. Study population characteristics.
summarizes the unadjusted and adjusted healthcare costs associated with patients cared for in nephrology clinics versus other care settings for the overall study population. The nephrology care cohort was associated with lower medical costs with an unadjusted annualized cost savings of $3,049 ($11,303 vs. $14,352, p = 0.0014) and a cost ratio of 0.8:1 relative to patients treated in other care settings. The largest driver of healthcare cost differences between nephrology clinics and other care settings was hospitalization costs (unadjusted cost difference: $1,442, p = 0.0524). After adjusting for covariates, the nephrology care cohort remained associated with statistically significantly lower healthcare costs (adjusted cost savings: $2,742, p = 0.006).
Table 2. Unadjusted and adjusted healthcare cost difference between CKD patients cared for in nephrology clinics and other care settings: all patients.
As expected, stratified analyses by CKD stages () showed a cost escalation associated with more advanced stages of CKD. The results also revealed that annualized healthcare costs in the nephrology care cohort were significantly lower in patients with CKD stages 3 and 4, compared with those cared for in other care settings (CKD stage 3: $10,132 vs. $14,000, p = 0.0006; CKD stage 4: $12,386 vs. $16,545, p = 0.025). The opposite situation was observed in those with CKD stage 5, where patients cared for in nephrology clinics were associated with increased healthcare costs (CKD stage 5: $23,445 vs. $18,522, p = 0.2385). After adjusting for confounders, only the cost difference of the nephrology care cohort with CKD stage 3 remained significantly lower compared with patients cared for in other care settings (adjusted cost savings: $3,259, p = 0.002). Adjusted healthcare costs in the nephrology care cohort remained lower compared with other care settings for CKD stage 4 patients, but the difference was not statistically significant (adjusted cost savings: $2,766, p = 0.0699).
Table 3. Unadjusted and adjusted healthcare cost difference between CKD patients cared for in nephrology clinics and other care settings by CKD stage at baseline.
presents the unadjusted and adjusted annualized healthcare costs associated with anemia and non-anemia periods for patients cared for in nephrology clinics versus other care settings. The cost savings associated with nephrology care relative to other care settings was more pronounced in periods of anemia ($14,963 vs. $21,112; cost difference: $6,149, p = 0.0022), compared with periods of non-anemia ($10,669 vs. $13,545; cost difference: $2,875, p = 0.0046), and remained statistically significant after adjusting for covariates (adjusted cost savings associated with nephrology care settings: anemia periods: $4,401, p = 0.026; non-anemia periods: $2,278, p = 0.006).
Table 4. Unadjusted and Adjusted Healthcare Cost Difference between CKD Patients Cared for in Nephrology Clinics and Other Care Settings by Anemia Status.
Discussion
The objective of this study was to evaluate, from a managed-care perspective, the healthcare cost of patients treated in nephrology care settings versus other care settings. From a sample of 20,135 pre-dialysis CKD patients observed over a period of 5 years, both unadjusted and adjusted results revealed that healthcare costs were lower among patients cared for in a nephrology care setting compared with patients who received care from other settings, with the exception of stage 5 CKD patients, where the situation was reversed. The largest driver of medical cost differences between the nephrology care cohort and the other care cohort was hospitalization-associated costs. Results also revealed that the cost difference between the nephrology care cohort and the other care cohort was increased during periods of anemia. Only patients with CKD stage 5 treated in nephrology clinics showed greater healthcare costs compared with those treated in other care settings. This situation is likely due to the numerous additional tests and heavier treatments administered to patients by nephrologists prior to their complete kidney failure, highlighting the importance of early referral. Additionally, in patients with advanced CKD not referred for nephrology care, it is possible that a decision was made to withhold dialysis due to several reasons, including patient or family refusal or severe comorbid conditionsCitation16. In patients with advanced CKD, where the decision has been made not to undergo dialysis and the associated preparations prior, the healthcare goals are different from those in a patient electing to undergo dialysisCitation17,Citation18. On the other hand, patients with advanced CKD not referred for nephrology care could possibly increase costs in the other care settings where the clinics have to manage more advanced disease without that modality of nephrology treatments.
Previous research has shown that both more advanced CKD and anemia in CKD patients are associated with significant increases in healthcare costsCitation19–21. In addition, previous studies have observed that delayed referral of CKD patients to nephrologists was associated with negative clinical outcomes such as prolonged initial hospitalizationCitation7–9,Citation11,Citation12, inadequate treatment for comorbiditiesCitation22,Citation23, greater incidence of dialysisCitation7–10, and higher probability of early death following dialysis initiationCitation5,Citation24,Citation25. Recent studies comparing nephrology care with non-nephrology care reported greater conformance to guidelines for the monitoring and treatment for comorbidities and complications of CKDCitation26–29.
Periods of anemia were associated with increased healthcare costs compared with periods of non-anemia; however, the absolute magnitude of the costs and the cost difference between periods of anemia and non-anemia were both reduced when patients were receiving care in a nephrology care setting compared with other care settings. Therefore, early referral of pre-dialysis CKD patients -- especially those with anemia-- to a nephrologist may contribute to reduced healthcare costs. Despite previous evidence that early intervention by a nephrologist is associated with better outcomes in CKD patientsCitation5,Citation30, only 1,547 (8%) patients in the present analysis were seen in a nephrology clinic setting during their observation period.
In 2006, per-patient-per-month healthcare expenditure in the pre-dialysis CKD population ranged from $1,902 to $2,609Citation1. These costs sharply increased in the month following ESRD to reach $14,461 to 28,718, depending on the specific population, and can be highly exacerbated by comorbiditiesCitation1,Citation15,Citation31. In light of these numbers, management of pre-dialysis CKD patients through earlier nephrology referral might have several advantages from a payer perspective. First, based on the findings of the current study, early treatment of CKD may prevent significant healthcare costs, especially with regard to inpatient services and disease-related comorbiditiesCitation4,Citation32. Second, timely and appropriate treatment of anemia may delay CKD progression, thus postponing the important costs brought by ESRD and the initiation of dialysisCitation33–38.
This study had several limitations. First, claims data may have inaccuracies in billing diagnoses, costs, and missing data on laboratory results. Although not rare, it would be unlikely that these inaccuracies have significantly affected the results considering the large sample size. Second, because the patient ethnicity was not available in the database used, eGFR values for black patients were under estimated by 21%. It is not possible to assess the extent of this bias on the stratification of patients according to their CKD stage, because the proportion of black patients in the studied population is unknown. Third, the study evaluated only the direct healthcare costs. Information to determine the indirect costs of CKD, such as work productivity loss and reduced quality of life, was not available. Fourth, the observational design was susceptible to various biases. The authors recognize that a randomized trial may be the ideal way of addressing this question; however, randomized trials focusing on economic end points are seldom undertaken because economic behaviors can still be influenced in a controlled setting. In the absence of such randomized trials, well-designed observational studies with appropriate statistical techniques adjusting for confounding factors provide valuable information with real-life scenarios and high generalizability. Fifth, the current study may also suffer from detection bias. Indeed, because laboratory results and diagnoses were not collected at pre-specified intervals as in randomized clinical trials, false negatives of CKD and anemia could have occurred in patients who did not seek care (especially those who did not have symptomatic manifestations). Sixth, it is possible that whether or not a patient was cared for in a nephrology clinic was influenced by the presence of such a clinic in the area where the patient lives and not solely by random factors. The authors acknowledge that such bias could have impacted the results as healthcare may differ from one region to the other, but the direction of such impact is undetermined. Moreover, it was not possible from the IMPACT database to determine if nephrology care was available in the region where each patient lived. Finally, it was not possible to capture the entire continuum of care of patients, as the IMPACT database does not include information from long-term nursing home care.
Despite these limitations, this research has several advantages, including the important advantage of relying on real-world data, a relatively large sample size, the availability of laboratory results to ascertain CKD stage and anemia status, and multivariate adjustments to control for confounders. To the authors’ knowledge, this research is the first to assess directly the economic impact of nephrology care on pre-dialysis CKD patients.
Conclusion
The current study based on real-life practice data demonstrated that patients with pre-dialysis stage 3 or 4 CKD treated in nephrology care setting were associated with significantly lower medical costs compared with those cared for in other healthcare settings. The current results also revealed that treatment of CKD patients in nephrology clinics was associated with healthcare cost savings regardless of their anemia status. Early identification of CKD and referral of pre-dialysis CKD patients to a nephrologist have the potential to decrease healthcare costs.
Transparency
Declaration of funding
This research was supported by Centocor Ortho Biotech Services, LLC.
Declaration of financial/other interests
F.V., N.D.Y., and P.L. have disclosed that they are employees of Analysis Group, Inc., a consulting company that has received research grants from Centocor Ortho Biotech Services, LLC. R.A.B., R.S.M., and C.T.P. have disclosed that they are employees of Centocor Ortho Biotech Services, LLC.
Acknowledgment
Parts of this work were presented at the American Society of Nephrology 2008 Renal Week, Philadelphia, PA, November 4–9, 2008.
References
- U.S. Renal Data System. USRDS 2009 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2009. Available at: http://www.usrds.org/adr_2009.htm. Accessed June 30, 2010
- Khan S, Amedia CA Jr. Economic burden of chronic kidney disease. J Eval Clin Pract 2008;14:422-434
- Trivedi H. Cost implication of caring for chronic kidney disease: are interventions cost-effective? Adv Chronic Dis 2010;17:265-270
- National Kidney Foundation. Kidney Disease Outcomes Quality Initiative (KDOQI) Clinical practice guidelines for chronic kidney disease: evaluation, classification and stratification. Am J Kidney Dis 2002;39(Suppl 1):S1-S66
- Khan SS, Xue JL, Kazmi WH, et al. Does predialysis nephrology care influence patient survival after initiation of dialysis? Kidney Int 2005;67:1038-1046
- Jungers P. Late referral: loss of chance for patient, loss of money for society. Nephrol Dial Transplant 2002;17:371-375
- Roubicek C, Brunet P, Huiart L, et al. Timing of nephrology referral: influence on mortality and morbidity. Am J Kidney Dis 2000;36:35-41
- Lorenzo V, Martin M, Rufino M, et al. Predialysis nephrologic care and a functioning arteriovenous fistula at entry are associated with better survival in incident hemodialysis patients: an observational cohort study. Am J Kidney Dis 2004;43:999-1007
- Dogan E, Erkoc R, Sayarlioglu H, et al. Effects of late referral to a nephrologist in patients with chronic renal failure. Nephrology (Carlton) 2005;10:516-519
- Schmidt RJ, Domico JR, Sorkin MI, et al. Early referral and its impact on emergent first dialysis, healthcare costs, and outcome. Am J Kidney Dis 1998;32:278-283
- Goransson LG and Bergrem H. Consequences of late referral of patients with end-stage renal disease. J Intern Med 2001;250:154-159
- Stoves J, Bartlett CN, Newstead CG, et al. Specialist follow up of patients before end stage renal failure and its relationship to survival on dialysis. Postgrad Med J 2001;77:586-588
- Boulware LE, Troll MU, Jaar BG, et al. Nephrology referral of patients with progressive CKD: a national study. Am J Kidney Dis 2006;48:192-204
- Levey AS, Coresh J, Balk E, et al. National Kidney Foundation: National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med 2003;139:137-147
- National Kidney Foundation. Kidney Disease Outcomes Quality Initiative (KDOQI), Clinical Practice Guideline and Clinical Practice Recommendations for Anemia in Chronic Kidney Disease, 2007 Update of Hemoglobin Target. Available at: http://www.kidney.org/professionals/KDOQI/guidelines_anemiaUP/index.htm. Accessed June 30, 2010
- Sekkarie MA, Moss AH. Withholding and withdrawing dialysis: the role of physician specialty and education and patient functional status. Am J Kidney Dis 1998;31:464-472
- Smith C, Da Silva-Gene M, Chandna S, et al. Choosing not to dialyze: Evaluation of planned non-dialytic management in a cohort of patients with end-stage renal disease. Nephron Clin Pract 2003;95:c40-c46
- Murtagh FE, Marsh JE, Donohue P, et al. Dialysis or not? A comparative survival study of patients over 75 years with chronic kidney disease stage 5. Nephrol Dial Transplant 2007;22:1955-1962
- Smith DH, Guillion CM, Nichols G, et al. Cost of medical care for chronic kidney disease and comorbidity among enrollees in a large HMO population. J Am Soc Nephrol 2004;15:1300-1306
- Lefebvre P, Duh MS, Buteau S, et al. Medical costs of untreated anemia in elderly patients with pre-dialysis chronic disease. J Am Soc Nephrol 2006;17:3497-3502
- Nissenson AR, Wade S, Goodnough T, et al. Economic burden of anemia in an insured population. J Manag Care Pharm 2005;11:565-574
- London R, Solis A, Goldberg GA, et al. Health care resource utilization and the impact of anemia management in patients with chronic kidney disease. Am J Kidney Dis 2002;40:539-548
- Robbins JD, Kim JJ, Zdon G, et al. Resource use and patient care associated with chronic kidney disease in a manage care setting. J Manag Care Pharm 2003;9:238-247
- Astor BC, Eustace JA, Powe NR, et al. Timing of nephrologist referral and arteriovenous access use: the CHOICE Study. Am J Kidney Dis 2001;38:494-501
- Winkelmayer WC, Owen WF Jr, Levin R, et al. A propensity analysis of late versus early nephrologist referral and mortality on dialysis. J Am Soc Nephrol 2003;14:486-492
- Patwardhan MB, Samsa GP, Matchar DB, et al. Advanced chronic kidney disease practice patterns among nephrologists and non-nephrologists: a database analysis. Clin J Am Soc Nephrol 2007;2:277-283
- Curtis BM, Barrett BJ, Djurdjev O, et al. Evaluation and treatment of CKD patients before and at their first nephrologist encounter in Canada. Am J Kidney Dis 2007;50:733-742
- Philipneri MD, Rocca Rey LA, Schnitzler MA, et al. Delivery patterns of recommended chronic kidney disease care in clinical practice: administrative claims-based analysis and systematic literature review. Clin Exp Nephrol 2008;12:41-52
- Charles RF, Powe NR, Jaar BG, et al. Clinical testing patterns and cost implications of variation in the evaluation of CKD among US physicians. Am J Kidney Dis 2009;54:227-237
- Levin A. Consequences of late referral on patient outcomes. Nephrol Dial Transplant 2000;15(Suppl 3):8-13
- Ershler WB, Chen K, Reyes EB, et al. Economic burden of patients with anemia in selected diseases. Value Health 2005;8:629-638
- Jungers P, Choukroun G, Robino C, et al. Epidemiology of end-stage renal disease in the Ile-de-France area: a prospective study in 1998. Nephrol Dial Transplant 2000;15:2000-2006
- Jungers P, Choukrun G, Oualim Z, et al. Beneficial influence of recombinant human erythropoietin therapy on the rate of progression of chronic renal failure in pre-dialysis patients. Nephrol Dial Transplant 2001;16:307-312
- Gouva C, Nikolopoulos P, Ioannidis JPA, et al. Treating anemia early in renal failure patients slows decline of renal function: a randomized controlled trial. Kidney Int 2004;66:753-760
- Keith DS, Nichols GA, Gullion CM, et al. Longitudinal follow-up and outcomes among a population with chronic kidney disease in a large managed care organization. Arch Intern Med 2004;164:659-663
- Mohanram A, Zhang Z, Shahinfar S, et al. Anemia and end-stage renal disease in patients with type 2 diabetes and nephropathy. Kidney Int 2004;66:1131-1138
- Dean BB, Dylan M, Gano A Jr, et al. Erythropoiesis-stimulating protein therapy and the decline of renal function: a retrospective analysis of patients with chronic kidney disease. Curr Med Res Opin 2005;21:981-987
- Go AS, Yang J, Ackerson LM, et al. Hemoglobin level, chronic kidney disease, and the risks of death and hospitalization in adults with chronic heart failure: the Anemia in Chronic Heart Failure: Outcomes and Resource Utilization (ANCHOR) Study. Circulation 2006;113:2713-2723