Abstract
Objective:
This study compared differences in healthcare costs and resource utilization for acute coronary syndrome (ACS) patients with and without diabetes mellitus (DM).
Methods:
A retrospective cohort study of a large, US employer-based claims database identified adults hospitalized for ACS between 01/01/2005 and 12/31/2006 and categorized them based on DM status. Resource utilization and costs during the index hospitalization and in the 12-month follow-up period were compared for ACS patients with and without DM using the propensity score stratification bootstrapping method, adjusting for differences in demographic and clinical characteristics.
Results:
Of 12,502 patients who met selection criteria, 3,040 (24%) had a history of DM and 9,462 (76%) did not. Patients with DM were older, female, and had higher rates of previous cardiovascular and renal diseases. After the propensity score stratification, patients with DM incurred higher index hospitalization costs ($32,577 vs. $29,150, p < 0.01) as well as higher total follow-up healthcare costs ($35,400 vs. $24,080, p < 0.01), including higher inpatient ($17,278 vs. $11,247, p < 0.01), outpatient ($12,357 vs. $8,853, p < 0.01), and pharmacy costs ($5,765 vs. $3,980, p < 0.01).
Limitations:
General limitations exist with any retrospective claims database analysis including potential diagnostic or procedural coding inaccuracies. Additionally, the patient population was representative of a working-age population with employer-sponsored health insurance and results may not be generalizable to other patient populations.
Conclusions:
DM is significantly associated with increased healthcare resource utilization and costs for ACS patients.
Introduction
Acute coronary syndrome (ACS) results from acute obstruction of the coronary artery. Clinical manifestations of ACS include unstable angina (UA), non-ST-segment elevation myocardial infarction (NSTEMI), ST-segment elevation myocardial infarction (STEMI), and sudden cardiac deathCitation1. Acute treatment strategies for ACS include medical management only or an interventional approach with revascularization procedures including percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG)Citation2.
According to the American Heart Association's Heart Disease and Stroke Statistical Update for 2009, almost 1.4 million hospital discharges in the US were due to ACS in 2006Citation3. The economic burden of ACS is great, costing more than $150 billion each year in the USCitation2. Retrospective analyses of US claims databases have demonstrated the substantial burden of new-onset ACS to employers and health plansCitation4–6.
During the first year following an initial ACS-related hospitalization, the majority of healthcare costs are due to hospitalizationCitation4 and rehospitalization is frequentCitation6. While studies have shown that newly diagnosed ACS patients have significantly higher costs in the year following the index event, recurrent ACS patients still utilize many healthcare resources and incur high medical costsCitation7.
Diabetes mellitus (DM) is a frequent comorbidity among patients with ACSCitation8–16 and its prevalence is increasing among these patientsCitation11,Citation17. ACS patients with DM are often older, female, and have more comorbidities compared to patients without DMCitation16,Citation18,Citation19. DM has been identified as an independent risk factor for adverse outcomes of ACS including heart failure, renal failure, cardiogenic shock, and deathCitation9,Citation13,Citation15,Citation16,Citation20 during index hospitalizationsCitation9 and after dischargeCitation20. Additionally, DM increases the risk of long-term negative outcomes in patients with UA/NSTEMI including significantly greater rates of new myocardial infarction compared to individuals without DMCitation13.
A number of comorbidities, including diabetes, have been found to predict high ACS-related costsCitation21. A Swiss study found that treatment costs among ACS patients were independently associated with age, gender, and comorbidities including cerebrovascular disease and diabetes (p < 0.01). These comorbidities were found to increase hospitalization costs by 20–40%Citation22. An Italian study also found that ACS patients with DM had more clinical complications resulting in greater resource use compared to patients without DMCitation23. Additionally, Epstein and colleagues found DM to be a contributing factor to increased mean 5-year costs among ACS patientsCitation24. However, the impact of comorbid DM on ACS-related costs has not been fully investigated and there is a need to quantify the potential cost difference between ACS patients with and without DM.
The current study compared real-world healthcare utilization and healthcare costs for ACS patients with and without DM in a large, privately insured, US population. The primary objective of this study was to evaluate differences in healthcare costs and resource utilization for ACS patients with and without DM. A secondary objective of this study was to determine if differences in resource utilization and costs exist for DM patients versus non-DM patients who undergo different revascularization procedures including PCI, CABG, or no revascularization (medical management only) during the index hospitalization.
Patients and methods
A retrospective cohort study was conducted using the MarketScan Commercial Claims and Encounters (CCAE) database. The MarketScan CCAE database is an employer-based claims database in the US representing approximately 100 contributing employers and 12 contributing health plans. It includes 10 million covered lives per year and provides integrated drug and medical claims covering all plan designs.
Inclusion criteria
Patients aged 18–65 years who were hospitalized with a primary diagnosis of ACS based on International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes 410.xx and 411.1 between January 1, 2005 and December 31, 2006 were included in the analysis. The first ACS hospitalization during the study period was considered the “index hospitalization.” Patients included in the analysis were required to have continuous medical and prescription drug coverage for the 12 months prior to the index hospitalization. This was defined as the baseline period. Additionally, patients were also required to have continuous medical and prescription drug coverage during the 12 months following the index ACS-related hospitalization, which was defined as the follow-up period.
Two mutually exclusive groups of ACS patients with and without DM were created using information regarding patients’ DM status extracted from their medical claims data during the 12 months prior to and during the index hospitalization. ACS patients were categorized as having DM if they had at least two outpatient office visits or one hospitalization with a primary diagnosis of DM (250.xx) during the baseline period. Patients with ACS were categorized as not having DM if they had no DM-related medical claims at any time during the 12-month period prior to and following the index hospitalization. Patients with a new diagnosis of DM during the 12-month period following the index hospitalization were excluded from the analysis.
Study endpoints
Healthcare resource utilization during the index hospitalization and over the 12-month period following the index hospitalization was compared for ACS patients with and without DM. Measures of resource utilization included index hospitalization length of stay (LOS), all-cause hospitalization rates, ACS-related rehospitalization rates, rehospitalization LOS, and rates of emergency department (ED) utilization.
Total direct healthcare costs during the index hospitalization and the 12-month follow-up period were estimated in 2008 US dollars and compared for ACS patients with and without DM. Indirect costs were not included in this analysis. The 12-month follow-up healthcare costs, including pharmacy, outpatient, and inpatient costs, were broken into two categories: all-cause and ACS-related follow-up costs. ACS-related follow-up healthcare costs were defined as: (1) medical costs from inpatient/outpatient claims having an ICD-9 diagnosis code of 410.xx, 411.1x; and (2) pharmacy costs for use of lipid lowering agents, antiplatelets, anticoagulants, antiarrhythmic agents, β-blockers, calcium channel blockers, angiotensin converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBS), antihypertensive agents, and nitrates (see ). Total healthcare costs were also calculated for patients with and without DM by the type of revascularization technique received during the index hospitalization (i.e., PCI, CABG, or no revascularization). PCI was identified using ICD-9-CM procedure codes: 36.01, 36.02, 36.05, 00.66, 36.06, 36.07, Current Procedural Terminology (CPT) codes: 92982, 92984, 92995, 92996, 92980, 92981, 92975, 92973, 92974, 92978, 92979, and Healthcare Common Procedure Coding System (HCPCS) codes: G0290, G0291, C1753. CABG was identified using ICD-9-CM procedure ode 36.1x, CPT codes: 33510, 33511, 33512, 33513, 33514, 33516, 33533, 33534, 33535, 33536, 33517, 33518, 33519, 33521, 33522, 33523, and HCPCS codes: S2205, S2206, S2207, S2208, S2209.
Statistical analysis
Baseline characteristics between DM and non-DM patients were compared using chi-square tests for categorical variables and t-tests for continuous variables. To assess the prevalence of comorbidities, both inpatient and outpatient medical claims from the baseline period were reviewed. A total of 17 dichotomous variables were created, each corresponding to a chronic disease contained in the Charlson Comorbidity IndexCitation25. The method of Deyo et al.Citation26,Citation27, which establishes ICD-9-CM codes for each of these 17 conditions, was used to create the dichotomous comorbidity variables from the claims database. Finally, the sum of weighted scores of all of the comorbid conditions was used to create a single Charlson Comorbidity Index. Healthcare costs and resource utilization were compared between DM and non-DM patients using a propensity score stratification bootstrapping approachCitation28–30. Specifically, the propensity score method was performed first to calculate the logit score for each patient based on patient demographics (i.e., female gender, age at index hospitalization), the presence or absence of comorbidities (i.e., transient ischemic attack [TIA]/stroke, peripheral artery disease [PAD], peptic ulcer disease [PUD], congestive heart failure [CHF], atrial fibrillation, renal disease, chronic obstructive pulmonary disease [COPD], hypertension, hyperlipidaemia, neoplasms, or depression), the presence or absence of hospital admissions in pre-index period, the presence or absence of specific index ACS diagnoses (i.e., STEMI, NSTEMI, UA), and the presence or absence of each type of revascularization technique received during the index hospitalization (i.e., PCI, CABG) as dichotomous covariates. All patients were then stratified into quintiles based on the predicted propensity score, and the bootstrap re-sampling method was performed within each quintile to compare their cost differences. After 10,000 times of repeated sampling, statistical tests were conducted and two-tailed p-values were calculated. SAS version 9.1 was used to perform all statistical analyses, with all effects tested at a two-sided α level of 0.05.
Results
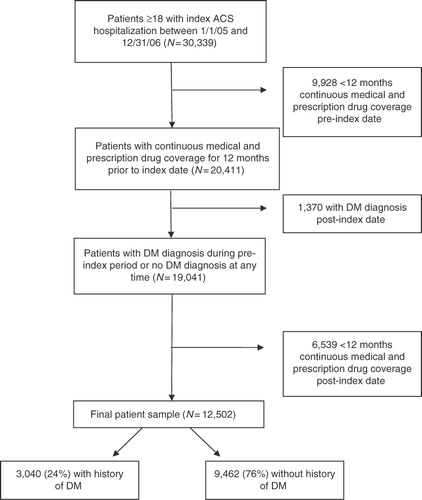
More than 30,000 patients were hospitalized for ACS during the study period (). Of these, 12,502 patients with ACS were identified and had both continuous medical and prescription drug coverage in the 12 months prior to and following the index hospitalization. Among these patients, 3,040 (24%) had a history of DM and 9,462 (76%) had no history of DM.
Figure 1. Patient disposition. Patients were included in the analysis if they were 18–65 years old and had an ACS-related hospitalization during the study dates. Patients were required to have 12 months of continuous enrolment and pharmacy data prior to and following the index hospitalization. Of the more than 12,500 patients included in the analysis, 24% had a history of DM. ACS, acute coronary syndrome; DM, diabetes mellitus.
ACS patients with DM were more likely to be older and female (). Patients with DM also had significantly higher Charlson Comorbidity Index scores compared to those without DM and were significantly more likely to have higher rates of most comorbidities evaluated including congestive heart failure, peripheral artery disease (PAD), transient ischemic attack/stroke, hypertension, hyperlipidaemia, and renal disease (p < 0.01 for each comparison). Significantly more patients with DM had a hospitalization due to any cause during the pre-index period compared to those without DM (24.2 vs. 10.7%, p < 0.01). They were also more likely to have a previous ACS-related hospitalization during the pre-index period compared to patients without DM (7.5 vs. 3.2%, p < 0.01).
Table 1. Demographic and clinical characteristics of ACS patients with and without diabetes mellitus (N = 12,502).
ACS patients with DM were more likely to present with NSTEMI compared to those without DM, who were more likely to present with STEMI at the index hospitalization (). Rates of UA and other symptoms of ACS were similar between study groups. During the index hospitalization, ACS patients with DM underwent less PCI (48.7 vs. 59.3%, p < 0.01), but received more CABG (13.1 vs. 8.9%, p < 0.01), and were more likely to receive no revascularization (38.3 vs. 31.7%, p < 0.01). However, regardless of DM status, PCI was the most frequently performed revascularization procedure during the index hospitalization.
Healthcare resource use
During the index hospitalization for ACS, patients with DM had a significantly longer LOS compared to those without DM (p < 0.01) (). Regardless of whether a patient received PCI, CABG, or no revascularization during the index hospitalization, LOS was significantly greater for ACS patients with DM compared to those without DM (p < 0.01 for each comparison).
Table 2. Resource utilization in patients with and without diabetes mellitus* (N = 12,502).
During the 1-year period following the index hospitalization, ACS patients with DM used significantly more healthcare resources compared to those without DM (). Rates of all-cause hospitalizations, mean LOS during rehospitalizations, ED utilization, and mean number of office visits were all significantly higher for ACS patients with DM compared to those without DM (p < 0.01 for each comparison). Similar patterns of greater resource use among patients with DM were seen in those who received PCI, CABG, or no revascularization during the index hospitalization.
Similarly, diabetic patients had significantly greater ACS-related healthcare resource utilization including higher ACS-related rehospitalization rates with greater mean LOS (p < 0.01 for each comparison). However, the mean number of outpatient office visits was slightly lower for ACS patients with DM compared to those without DM (p < 0.05). There was no difference in the frequency of ED visits between patients with or without DM. A similar pattern of greater ACS-related resource use among patients with DM was seen in those who received PCI, CABG, or no revascularization during the index hospitalization. However, the mean number of office visits per patient was not significantly different between patients with or without DM in those who received PCI, CABG, or no revascularization during the index hospitalization. Additionally, among patients who underwent CABG during the index hospitalization, there was no significant difference in rehospitalization LOS between patients with or without DM.
Healthcare costs
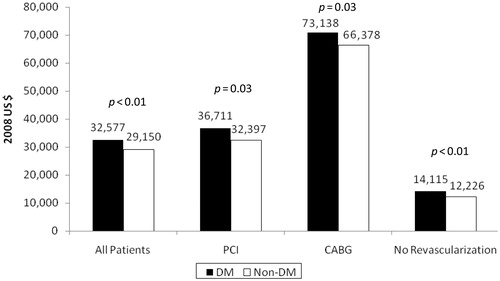
ACS patients with DM had significantly greater total direct index hospitalization costs compared to patients without DM ($32,577 [SE $1,157] vs. $29,150 [SE $298], p < 0.01) (). In addition, regardless of the type of revascularization patients received during the index hospitalization, ACS patients with DM had significantly higher total index hospitalization costs compared to patients without DM (PCI: $36,711 [SE $2,072] vs. $32,397 [SE $339], p = 0.03; CABG: $73,138 [SE $2,617] vs. $66,378 [SE $1,454], p = 0.03; No revascularization: $14,115 [SE $543] vs. $12,226 [SE $257], p < 0.01).
Figure 2. Mean total index hospitalization costs for ACS patients with DM versus without DM (US$ 2008). Total direct index hospitalization costs were significantly greater for patients with DM compared to those without DM among all ACS patients and regardless of the type of revascularization patients received during the index hospitalization. ACS, acute coronary syndrome; CABG, coronary artery bypass graft; DM, diabetes mellitus; PCI, percutaneous coronary intervention.
Total direct all-cause healthcare costs over the 12-month period following the index hospitalization were significantly higher for ACS patients with DM compared to those without DM ($35,400 [SE $1,001] vs. $24,080 [SE $371], p < 0.01) (). Significant differences in each cost component were seen between patients with and without DM including pharmacy ($5,765 [SE $96] with DM vs. $3,980 [SE $35] without DM, p < 0.01), outpatient care ($12,357 [SE $529] with DM vs. $8,853 [SE $154] without DM, p < 0.01), and inpatient care ($17,278 [SE $743] with DM vs. $11,247 [SE $296] without DM, p < 0.01). Inpatient costs were the largest component of the costs over the 12 months following the index hospitalization regardless of DM status. A similar pattern of significantly greater all-cause total, pharmacy, outpatient, and inpatient costs among patients with DM was also seen in patients who received PCI, CABG, or no revascularization during the index hospitalization (p < 0.05 for each comparison) ().
Figure 3. Mean total direct all-cause and ACS-related costs during the 12 months following the index ACS-related hospitalization in patients with and without diabetes mellitus (N = 12,502). Total direct all-cause costs were significantly greater for patients with DM compared to those without DM. Patients with DM had significantly higher all-cause pharmacy, outpatient, and rehospitalization costs compared to those without DM. Similar findings were seen with ACS-related total costs. Patients with DM had significantly higher pharmacy and rehospitalization costs compared to those without DM. However, ACS-related outpatient costs were higher for those without DM compared to those with DM. *p < 0.01; †p < 0.05. ACS, acute coronary syndrome; DM, diabetes mellitus.
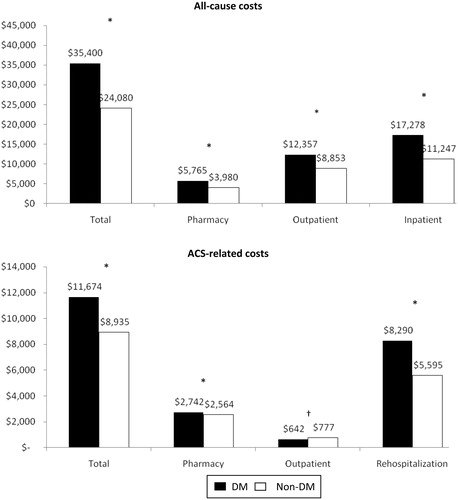
Figure 4. Mean total direct all-cause and ACS-related costs during the 12 months following the index ACS-related hospitalization in patients with and without diabetes mellitus by revascularization technique received (N = 12,502). All-cause and ACS-related healthcare costs for the 12-month period following the index hospitalization data were stratified by the type of revascularization procedure received during the index ACS-related hospitalization. Regardless of index revascularization procedure received, ACS patients with DM had significantly greater all-cause total healthcare costs compared to those without DM. Total ACS-related healthcare costs were generally greater for patients with DM compared to those without DM. However, in patients who underwent CABG during the index hospitalization, ACS-related total costs were not significantly different between patients with DM and those without DM. *p < 0.01; †p < 0.05. ACS, acute coronary syndrome; CABG, coronary artery bypass graft; DM, diabetes mellitus; PCI, percutaneous coronary intervention.
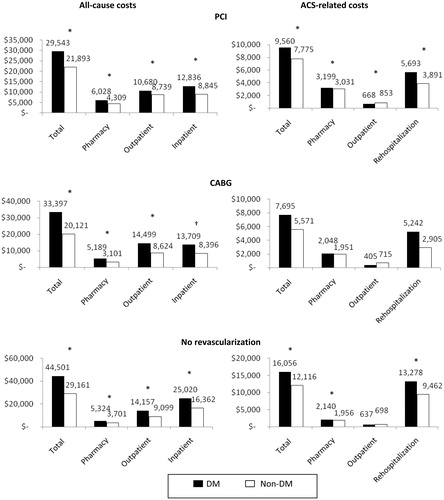
Total ACS-related costs for the 12-month period following the index hospitalization were significantly greater for patients with DM compared to those without DM ($11,674 [SE $531] vs. $8,935 [SE $191], p < 0.01) (). When only ACS-related costs were considered, patients with DM had significantly higher pharmacy costs ($2,742 [SE $33] vs. $2,564 [SE $16], p < 0.01) and rehospitalization costs ($8,290 [SE $526] vs. $5,595 [SE $184], p < 0.01) compared to patients without DM during the 12-month follow-up period. However, patients without DM had higher costs for outpatient care compared to those with DM during the follow-up period ($777 [SE $36] vs. $642 [SE $42], p < 0.05). Similar to all-cause costs, ACS-related rehospitalization cost was the largest cost component following the index hospitalization. Among ACS patients who received PCI or no revascularization during the index hospitalization, the pattern of differences in ACS-related costs between DM and non-DM patients was similar to that seen in all ACS patients; however, in patients who received no revascularization, ACS-related outpatient costs were not significantly different between those with or without DM (). Among patients who received CABG during the index hospitalization, there were no significant differences in ACS-related total, pharmacy, outpatient, or rehospitalization costs between patients with and without DM.
Discussion
This study compared resource utilization and healthcare costs during the index hospitalization and 12-month follow-up period for ACS patients with or without DM. In the current analysis, 24% of patients with ACS had known DM upon index admission. Similar prevalence rates can be found in previous studies of large clinical survey and registry dataCitation9,Citation18. DM patients with ACS were older, more likely to be female, and had a less-favorable risk profile, with higher rates of previous cardiovascular and renal disease, compared to their non-DM counterparts. Again, these findings are similar to several studies in the medical literatureCitation9,Citation15. Upon index hospital admission, patients with DM were more likely to present with NSTEMI and were less likely to present with STEMI, compared to ACS patients without DM.
After adjusting for differences in demographic and clinical characteristics, ACS patients with DM had higher index hospitalization costs and longer mean LOS compared to those without DM. As expected, ACS patients with DM were also more likely to use healthcare resources in the 12 months following the index hospitalization compared to patients without DM, including higher rates of all-cause rehospitalization, outpatient doctor office visits, and ED visits. As a consequence, total healthcare costs during the 12-month follow-up period were also significantly greater for ACS patients with DM compared to those without DM. The differences in follow-up healthcare resource utilization and costs between patients with and without DM were seen among all ACS patients, regardless of revascularization strategy received during the index hospitalization.
Among all patients, ACS-related resource utilization and costs during the follow-up period were greater for those with DM compared to without DM except for the frequency of ED visit. However, the differences in office visit use were not statistically significant when the revascularization strategy received during index hospitalization was considered. Additionally, diabetic patients who underwent PCI or no revascularization during the index hospitalization had greater ACS-related total, pharmacy, and rehospitalization costs. However, patients who underwent CABG during the index hospitalization had no differences in ACS-related follow-up costs based on DM status.
While several papers have quantified the cost of ACSCitation4–6, comparison of healthcare costs for ACS patients with and without DM is infrequent. The findings of the current study are supported by a retrospective analysis of inpatient resource use in Italy, which also found that ACS patients with DM had more clinical complications (41.1 vs. 17.9%, p < 0.01) and longer hospitalizations, which resulted in greater management costs, compared with patients without DMCitation23. However, this study focused on inpatient resource use and costs only, unlike the current study, which also evaluated total inpatient and outpatient costs during the 12 months following the index hospitalization. To the authors’ knowledge, the current study is the first to evaluate the differences in healthcare costs for ACS patients with and without DM in the US.
In the current study, total all-cause treatment costs among ACS patients with DM were approximately $11,000 (47%) greater than those for patients without DM. This magnitude of difference is similar to a comparison of costs in patients with cardiovascular disease, where patients with DM had average annual medical care costs that were approximately 59% higher than those without DMCitation31. However, the magnitude of difference in the current study is less than that seen in a comparison of end-stage renal disease-associated costs, which estimated that adjusted total annual costs per patient were between 69% and 79% greater in those with DM compared to nondiabeticsCitation32.
General limitations exist with any retrospective database analysis including potential diagnostic or procedural coding inaccuracies, and incomplete dataCitation33. A claim does not guarantee service was provided or provided correctly. Additionally, with most claims databases, there is a lag time between when a claim occurs and when data are available for analysis. This study included data from 2005 and 2006 because these were the latest data available upon initiation of this study. Thus, results presented here reflect practice patterns that occurred during the study period. To our knowledge, there has not been a more recent assessment of resource use and costs of treatment by DM status published in the medical literature.
The large sample sizes provided by a database lead to great statistical power, which may yield differences that are statistically significant, but not clinically or practically meaningful. Since individual outcome is our primary focus, all the p-values in this study are not adjusted for multiplicityCitation34.
The patient population included in this database analysis was representative of a working-age population with employer-sponsored health insurance. Thus, there is a lack of generalizability to individuals beyond this patient population, including older patients. Results may not be generalizable to other patient populations including beneficiaries of Medicare or Medicaid. Additionally, this analysis captured all costs and co-payments incurred by ACS patients, which is reflective of total costs to the healthcare system.
Conclusion
In conclusion, ACS patients with DM were significantly more likely to use healthcare resources and have higher total all-cause and ACS-related follow-up healthcare costs compared to those without DM. ACS patients with comorbid DM represent more complex and resource intensive patients compared to those without DM. Finding ways to manage costs in ACS patients with DM may have a substantial impact on controlling the escalating costs associated with ACS in the US.
Transparency
Declaration of funding
This study was funded by Daiichi Sankyo, Inc., and Eli Lilly and Company.
Declaration of financial/other relationships
At the time of this study, all authors were employed by Eli Lilly and Company.
Acknowledgments
The authors wish to acknowledge technical writing support from Dr Susan L. Dennett of Strategic Health Outcomes, Inc. Technical writing support was funded by Eli Lilly and Company.
Notes
*The type of revascularization technique received during the index hospitalization was excluded from the model for sub group analysis for CABG, PCI and no revascularization patients.
References
- Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction — executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction): developed in collaboration with the American College of Emergency Physicians, American College of Physicians, Society for Academic Emergency Medicine, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol 2007;50:652-726
- Kolansky DM. Acute coronary syndromes: morbidity, mortality, and pharmacoeconomic burden. Am J Manag Care 2009;15:S36-41
- Lloyd-Jones D, Adams R, Carnethon M, et al. Heart disease and stroke statistics—2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2009;119:e21-181
- Etemad LR, McCollam PL. Total first-year costs of acute coronary syndrome in a managed care setting. J Manag Care Pharm 2005;11:300-306
- McCollam P, Etemad L. Cost of care for new-onset acute coronary syndrome patients who undergo coronary revascularisation. J Invasive Cardiol 2005;17:307-311
- Menzin J, Wygant G, Hauch O, et al. One-year costs of ischemic heart disease among patients with acute coronary syndromes: findings from a multi-employer claims database. Curr Med Res Opin 2008;24:461-468
- Shetty S, Halpern R, McCollam PL. Cost of care for new versus recurrent acute coronary syndrome patients. J Med Econ 2008;11:81-99
- Norhammar A, Tenerz A, Nilsson G, et al. Glucose metabolism in patients with acute myocardial infarction and no previous diagnosis of diabetes mellitus: a prospective study. Lancet 2002;359:2140-2144
- Franklin K, Goldberg RJ, Spencer F, et al. Implications of diabetes in patients with acute coronary syndromes: the Global Registry of Acute Coronary Events. Arch Intern Med 2004;164:1457-1463
- Tenerz A, Lonnberg I, Berne G, et al. Myocardial infarction and prevalence of diabetes Mellitus: Is increased casual blood glucose at admission a reliable criterion for the diagnosis of diabetes? Eur Heart J 2001;22:1102-1110
- Gandhi GY, Roger VL, Bailey KR, et al. Temporal trends in prevalence of diabetes mellitus in a population-based cohort of incident myocardial infarction and impact of diabetes on survival. Mayo Clin Proc 2006;81:1034-1040
- Benjamin SM, Geiss LS, Pan L, et al. Self-reported heart disease and stroke among adults with and without diabetes – United States, 1999–2001. MMWR Weekly 2003;52:1065-1070
- Malmberg K, Yusuf S, Gerstein HC, et al. Impact of diabetes on long-term prognosis in patients with unstable angina and non-Q-wave myocardial infarction: results of the OASIS (Organisation to Assess Strategies for Ischemic Syndromes) Registry. Circulation 2000;102:1014-1019
- Steg PG, Goldberg RJ, Gore JM, et al. Baseline characteristics, management practices, and in-hospital outcomes of patients hospitalized with acute coronary syndromes in the Global Registry of Acute Coronary Events (GRACE). Am J Cardiol 2002;90:358-363
- McGuire DK, Emanuelsson H, Granger CB, et al. Influence of diabetes mellitus on clinical outcomes across the spectrum of acute coronary syndromes. Findings from the GUSTO-IIb study. GUSTO IIb Investigators. Eur Heart J 2000;21:1750-1758
- Hasdai D, Behar S, Boyko V, et al. Treatment modalities of diabetes mellitus and outcomes of acute coronary syndromes. Coron Artery Dis 2004;15:129-135
- Fox CS, Coady S, Sorlie PD, et al. Increasing cardiovascular disease burden due to diabetes mellitus: the Framingham heart study. Circulation 2007;115:1544-1550
- Hasin T, Hochadel M, Gitt AK, et al. Comparison of treatment and outcome of acute coronary syndrome in patients with versus patients without diabetes mellitus. Am J Cardiol 2009;103:772-778
- Zhao Z, Zhu B, Anderson J, et al. Real-world practice patterns in acute coronary syndrome patients with and without diabetes mellitus. Manuscript submitted for publication, 2010
- Donahoe SM, Stewart GC, McCabe CH, et al. Diabetes and mortality following acute coronary syndromes. JAMA 2007;298:765-775
- Etemad LR. McCollam PL. Predictors of high-cost managed care patients with acute coronary syndrome. Curr Med Res Opin 2005;21:1977-1984
- Bramkamp M, Radovanovic D, Erne P, et al. Determinants of costs and the length of stay in acute coronary syndromes: a real life analysis of more than 10,000 patients. Cardiovasc Drugs Ther 2007;21:389-398
- Novo G, Scordato F, Cerruto G, et al. In-hospital stay of patient with acute coronary syndrome with or without diabetes mellitus. Minerva Cardioangiologica 2009;57:159-164
- Epstein DM, Sculpher MJ, Clayton TC, et al. Costs of an early intervention versus a conservative strategy in acute coronary syndrome. Int J Cardiol 2007;127:240–246
- Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373-383
- Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 1992;45:613-619
- Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005;43:1130-1139
- Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika 1983;70:41-55
- Rosenbaum PR, Rubin DB. Reducing bias in observational studies using subclassification on a propensity score. J Am Stat Assoc 1984;79:516-524
- Faries D, Leon A, Haro J, et al. Analysis of Observational Health Care Data Using SAS. 2010. SAS institute
- Nichols GA, Brown JB. The impact of cardiovascular disease on medical care costs in subjects with and without type 2 diabetes. Diabetes Care 2002;25:482-486
- Joyce AT, Iacoviello JM, Nag S, et al. End-stage renal disease–associated managed care costs among patients with and without diabetes. Diabetes Care 2004;27:2829-2835
- Diehr P, Yanez D, Ash A, et al. Methods for analyzing health care utilisation and costs. Annu Rev Public Health 1999;20:125-144
- Feise RJ. Do multiple outcome measures require p-value adjustment? BMC Med Res Methodol 2002;2:2-8
Appendix
Drug classes and specific medications included in pharmacy costs.