Abstract
Objective:
Between 2.7 and 3.9 million people are currently infected with the hepatitis C virus (HCV) in the United States. Although many studies have investigated the impact of HCV on direct healthcare costs, few studies have estimated the indirect costs associated with the virus using a nationally-representative dataset.
Methods:
Using data from the 2009 United States (US) National Health and Wellness Survey, patients who reported a hepatitis C diagnosis (n = 695) were compared to controls on labor force participation, productivity loss, and activity impairment after adjusting for demographics, health risk behaviors, and comorbidities. All analyses applied sampling weights to project to the population.
Results:
Patients with HCV were significantly less likely to be in the labor force than controls and reported significantly higher levels of absenteeism (4.88 vs. 3.03%), presenteeism (16.69 vs. 13.50%), overall work impairment (19.40 vs.15.35%), and activity impairment (25.01 vs. 21.78%). A propensity score matching methodology replicated many of these findings.
Conclusions:
While much of the work on HCV has focused on direct costs, our results suggest indirect costs should not be ignored when quantifying the societal burden of HCV. To our knowledge, this is the first study which has utilized a large, nationally-representative data source for identifying the impact of HCV on labor force participation and work and activity impairment using both a propensity-score matching and a regression modeling framework.
Limitations:
All data were patient-reported (including HCV diagnosis and work productivity), which could have introduced some subjective biases.
Introduction
The hepatitis C virus (HCV) is a blood-borne illness which typically manifests as fever, fatigue, abdominal pain, and jaundice (among other symptoms), though as many as 80% of the newly infected are asymptomaticCitation1. The incidence of HCV has declined in recent decades, with the current rate estimated at 0.3 cases per 100,0002. It is believed that between 2.7 and 3.9 million people are currently infected with HCV in the United StatesCitation3. In the later stages of infection, patients with HCV are at increased risk for the development of cirrhosis and hepatocellular carcinoma which are associated with high morbidity and mortality ratesCitation4. HCV is the primary contributor to deaths from liver diseaseCitation5.
A number of studies have evaluated the impact of HCV on healthcare costsCitation6–8. Previous studies have estimated direct healthcare costs associated with HCV to be $2,070 per patient in 1997Citation6 and $2,470 per patient during the time period from 1997–1999Citation8. However, direct medical costs represent only part of the societal burden of HCV infection. Indirect costs, the costs attributed to work impairment (either through health-related absences or health-related impairment while working), are also important to consider, but have been largely ignored in the HCV literature.
Previous cost-effectiveness models have left out work impairment altogetherCitation9 or have measured productivity losses only in the form of premature mortality and disability as a result of projected late stage liver diseaseCitation7. One of the only studies to analyze current (rather than projected) costs related to HCV found total indirect costs of $3.66 billion in 1997, though the algorithms used focused exclusively on wages, fringe benefits, and home productionCitation6. A review of the literature yielded only one study each that assessed the impact of HCV on labor force participationCitation10, employability in a welfare populationCitation11, and the impact of HCV on absenteeism and presenteeismCitation12. Apart from these studies, the only assessments of HCV impact on workplace activity have been within the context of clinical trialsCitation13.
To fully understand the societal impact of HCV, the association between the virus and both labor force participation and work productivity loss must be considered. It is also crucial to investigate potential confounding variables that may contribute to a relationship between HCV status and workplace activity. A variety of studies have documented the impact comorbidities and health behaviors may have on health outcomes among HCV patients, including psychiatric illnessesCitation14–16, advanced fibrosisCitation17, fatigueCitation18, and depressive symptomsCitation19,Citation20. As these variables all may plausibly affect labor force participation and work productivity, they should be considered as potential confounders. As such, the present study attempts to determine the incremental effect of HCV on labor force participation, work productivity loss, and activity impairment using a large, nationally-representative database, and accounting for many of the differences between the groups that were previously ignored. These results will help provide a robust estimate of the contribution of HCV to indirect costs.
Methods
National Health and Wellness Survey
The current study used data from the 2009 wave (N = 75,000) of the US National Health and Wellness Survey (NHWS; Kantar Health, New York, NY, USA), an annual, cross-sectional study of adults aged 18 years or older. The NHWS includes epidemiological data, treatment information, information on health risk behaviors, and health-related outcome data. Potential respondents to NHWS are recruited through an existing consumer panel. The consumer panel recruits its panel members through opt-in emails, co-registration with panel partners, e-newsletter campaigns, and banner placements. All panelists must explicitly agree to be a panel member, register with the panel through a unique email address, and complete an in-depth demographic registration profile. Using a stratified random sample framework (with quotas based on gender, age, and race/ethnicity), the demographic composition of the 2009 US NHWS sample is comparable to that of the US adult population as described by the March 2008 Current Population Survey of the US Census BureauCitation21. Additional comparisons with NHWS and NHIS have been made elsewhereCitation22. All subjects provided informed consent and the study was approved by Essex Institutional Review Board (Lebanon, NJ, USA). In the NHWS study, 501,239 subjects were contacted, out of whom 92,759 responded (18.5% response rate). Of those who responded, 75,000 patients gave informed consent, met inclusion criteria, and completed the survey. Patients diagnosed with hepatitis B, HIV, or AIDS (n = 966) were excluded from the sample, leaving a total sample size of 74,034. Because the base rates of these conditions are low among the general population yet relatively high among the HCV population, patients diagnosed with these conditions were excluded to ensure any observed differences between HCV diagnosed patients and controls were not due to HCV-related comorbidities. This has also been done in prior researchCitation21. Of the total 74,034 respondents, 695 reported being diagnosed with HCV and 73,339 reported not being diagnosed with HCV.
Labor force and work productivity variables
The potential impact of HCV was assessed in terms of the following five workplace and associated characteristics: (1) labor force participation (whether or not the respondent is employed/actively seeking work); (2) absenteeism (percentage of work time missed due to health); (3) presenteeism (degree of impairment experienced at work due to health); (4) overall work impairment (a total percentage of missed work time due to either absenteeism or presenteeism); and (5) activity impairment (degree of impairment experienced during non-work activities).
Labor force participation
All respondents reported their current workforce status. Those who reported being employed full-time, employed part-time, self-employed, or unemployed but looking for work were considered to be in the labor force. All others were not considered to be in the labor force.
Work productivity and activity impairment
The Work Productivity and Activity Impairment (WPAI) questionnaire was used to measure the impact of health on employment-related activitiesCitation23. WPAI is a 6-item validated instrument that consists of four metrics: absenteeism (the percentage of work time missed because of one’s health in the past 7 days), presenteeism (the percentage of impairment experienced while at work in the past 7 days because of one’s health), overall work productivity loss (an overall impairment estimate that is a combination of absenteeism and presenteeism), and activity impairment (the percentage of impairment in daily activities because of one’s health in the past 7 days). Only respondents who reported being employed full-time, employed part-time, or self-employed provided data for absenteeism, presenteeism, and overall work impairment. All respondents provided data for activity impairment. The validity and accuracy of the instrument has been established in a number of disease states, included HCVCitation13.
Absenteeism was calculated by dividing the number of work hours a patient missed in the past week because of his or her health by the total number of hours a patient could have worked (the number of hours he/she did work plus the number of hours missed because of his/her health) and converting this proportion into a percentage. Presenteeism was measured by a patient’s rating of his or her level of impairment experienced while at work in the past 7 days (from 0 to 10, with higher numbers indicating greater impairment), which was then multiplied by 10 to create a percentage, with a range from 0% to 100%. Overall work impairment was measured by adding absenteeism and presenteeism to determine the total percentage of lost work time. Activity impairment was measured by a patient’s rating of the level of impairment experienced in daily activities in the past 7 days (from 0 to 10, with higher numbers indicating greater impairment), which was then multiplied by 10 to create a percentage, with a range from 0 to 100%.
Control variables
A wide array of predictor variables that have previously been shown to have a potential impact on both labor force participation as well work productivity loss was evaluated. These variables were grouped into socio-demographic variables, health-risk behaviors, and morbidity/comorbidity status variables. The socio-demographic variables included gender, race/ethnicity (white, black, Hispanic, Asian, or other), marital status (married/living with partner vs. all else), educational attainment (college degree vs. all else), and annual household income (<$25,000, $25,000 to <$50,000, $50,000 to <$75,000, $75,000 or more, decline to answer). Health-risk behaviors included tobacco smoking, alcohol consumption, body mass index (BMI) and physical exercise. For the assessment of morbidity/comorbidity status, both the number of comorbid conditions and, separately, the self-reported presence of anxiety and depression were assessed.
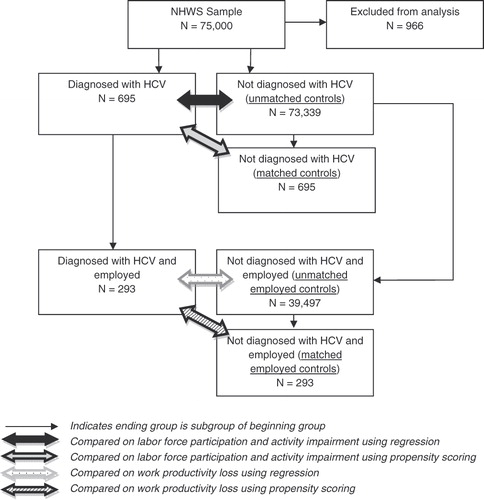
Statistical analysis
Initial bivariate comparisons between HCV and controls were made using chi-square tests for categorical outcomes and independent-samples t-tests for continuous outcomes. Because some of the outcomes were available for all respondents (labor force participation and activity impairment) and some outcomes were only available for those who were employed (absenteeism, presenteeism, and overall work impairment), different analysis groups were created (see ). The primary analytical approach was regression modeling. The regression modeling approach included patients diagnosed with HCV and controls. Age, gender, race/ethnicity, education, income, health insurance, presence of anxiety, presence of depression, number of comorbidities, smoking status, exercise behavior, alcohol use, BMI and group membership (HCV group vs. control group) were included in a series of generalized linear models (specifying a negative binomial distribution and a log-link function) to predict work productivity and activity impairment metrics. A log-link function was selected because of the pronounced non-normality of the dependent variables (high positive skew) and the negative binomial distribution was selected because it best modeled the dispersion. A thorough discussion of these approaches is made elsewhereCitation24. A logistic regression model (with the same independent variables) was used to predict labor force participation (yes vs. no). The formula for these models is as follows (with a log or logit depending upon the outcome):
Regression techniques used in situations such as this do present some disadvantages. The analysis groups are of vastly different sizes and the characteristics of the HCV group may be so meaningfully different that the extrapolation conducted during the regression process may not be an accurate estimate of the effect of HCV. To combat these limitations, and provide a more robust analysis of HCV, a propensity score modeling approach was also used to replicate the findings.
Two separate propensity score matching procedures were used. In the first matching procedure, all HCV patients were matched to a subset of all controls. Age, gender, race/ethnicity, education, income, health insurance, presence of anxiety, presence of depression, number of comorbidities, smoking status, exercise behavior, alcohol use, and BMI were entered in a logistic regression to predict group membership (HCV group vs. unmatched control group) in order to obtain propensity score values. Next, each HCV patient was matched with the control patient with the closest propensity score using a greedy-matching algorithmCitation25. Post-match, these groups were compared on labor force participation and activity impairment (the two outcomes that were answered by all respondents).
In the second matching procedure, employed HCV patients were matched to a subset of employed controls. The same variables noted above were entered in a logistic regression to predict group membership (employed HCV group vs. unmatched employed control group) in order to obtain propensity score values. Next, each employed HCV patient was matched with the employed control patient with the closest propensity score using a greedy-matching algorithmCitation25. Post-match, these groups were compared on absenteeism, presenteeism, and overall work impairment (the three outcomes that were answered by only those who were employed).
Generalized linear models, specifying a negative binomial distribution and a log-link function, were used to analyze group differences on work and activity impairment variables because of the pronounced non-normality of the data. Since employed HCV patients differed from matched employed controls on prevalence of smoking, this variable was controlled for when predicting absenteeism, presenteeism, and overall work impairment. A logistic regression was used to analyze group differences on labor force participation.
All analyses applied sampling weights (calculated using data from the NHWS and the US Bureau of the Census) to project the results to the US population, though bivariate comparisons also include unweighted statistics (i.e., frequencies and means with applying a sampling weight). The a priori cutoff for statistical significance was set as p < 0.05. All analyses were conducted using SAS 9.1 (SAS Institute, Inc., Cary, NC, USA)
Results
Sociodemographic and health risk behavior differences
compares respondent characteristics by the HCV status. Subjects with HCV diagnosis were older (50.4 vs. 46.0 years; p < 0.0001) and less likely to be female (41.9 vs. 52.2%; p < 0.0001) compared to those without HCV. Fewer HCV subjects were married (54.5 vs. 59.4%, p = 0.017) or college-educated (22.6 vs. 36.1%, p < 0.0001). The proportion of those with an annual income of less than $25,000 was lower in the HCV group (31.8 vs. 18.9%, p < 0.0001) relative to controls. Those with HCV were more likely to smoke, less likely to have exercised in the past month, and less likely to currently consume alcohol. In addition, the prevalence of anxiety and depression was more than twice as high in the HCV group than in the control group.
Table 1. Demographic and health history differences of hepatitis C patients compared to both unmatched and matched controls.
Labor force participation
Using a regression modeling approach, HCV patients were found to be significantly less likely to be in the labor force than unmatched controls (unstandardized regression estimate (b) = −0.32, odds ratio (OR) = 0.73, p < 0.0001), even after adjusting for sociodemographic, health risk, and comorbidity variables, many of which were significantly associated with labor force participation (see ). In particular, young age, male gender, Hispanic ethnicity, black ethnicity, unmarried status, college education, high household income, health insurance, smoking status, exercise, alcohol consumption, overweight BMI, fewer comorbidities, and lack of depression were all significantly predictive of labor force participation.
Table 2. Predictors of labor force participation.
Work productivity loss
Among those who were currently employed (full-time, part-time, or self-employed), the effect of HCV was examined on absenteeism, presenteeism, and overall work impairment after adjusting for sociodemographics, health risk behaviors, and comorbidity status (see ). Interestingly, those over the age of 70 generally had lower levels of impairment relative to other age groups. Although seemingly counterintuitive, an apparent self-selection bias may be present. Past retirement age, employment is less likely to be a necessity, thus workers over 70 still remain in the work force largely by choice and may be relatively healthier after adjusting for all other sociodemographic, health risk behavior, and comorbidity variables. White ethnicity, college education, and high household income were associated with lower levels of impairment. In regards to health risk behaviors and comorbidities, smoking, obesity, depression (though not anxiety), and a high comorbidity status were associated with more impairment while exercise was associated with less impairment.
Table 3. Generalized linear model regression estimates when predicting each of the work productivity and activity impairment metrics.
Of primary interest, the effect of HCV was significantly associated with presenteeism (b = 0.21, p = 0.02), overall work impairment (b = 0.23, p = 01), and marginally related to absenteeism (b = 0.48, p = 0.05). After controlling for the set of covariates outlined above, patients with HCV reported absenteeism levels of 4.88% (compared with 3.03% for unmatched controls), presenteeism levels of 16.69% (compared with 13.50%), and overall work impairment levels of 19.40% (compared with 15.35%).
Activity impairment
Among all respondents, the effect of HCV was examined on activity impairment after adjusting for sociodemographics, health risk behaviors, and comorbidities (see ). The same factors as noted above (ethnicity, education, income, etc.) were generally associated with impairment. Much like the other forms of work impairment, there was a significant effect of HCV on activity impairment (b = 0.14, p < 0.01). Respondents with HCV reported significantly higher levels of activity impairment (25.01%) relative to non-HCV subjects (21.78%), after adjusting for the set of covariates.
Propensity scoring
The research questions above were then examined using a propensity matching methodology to replicate the observed regression modeling effects. As expected, post-propensity matching there were no significant differences between the HCV group and the matched control group on any of the variables. Next, employed patients with HCV (n = 293) were compared to matched employed controls (n = 293). These groups were also generally comparable post-match. Although patients with HCV reported a significantly higher rate of smoking (54.1 vs. 43.9%, p = 0.04), no other significant differences were observed.
Using a propensity match approach to estimate the effect of HCV on labor force participation revealed no difference between the groups. Both respondents with HCV and matched controls were equally likely to be in the labor force (52.85 vs. 54.54%, p = 0.55).
Even after accounting for the imbalance of smoking behavior, employed HCV patients reported significantly higher levels of absenteeism (b = 0.64, p = 0.006), presenteeism (b = 0.26, p = 0.009), and overall work impairment (b = 0.30, p = 0.002) relative to matched employed controls. Specifically, HCV patients reported absenteeism levels of 9.27% (compared with 4.87% for matched employed controls), presenteeism levels of 27.23% (compared with 21.00%), and overall work impairment levels of 31.57% (compared with 23.47%). When comparing all patients with HCV and matched controls, there was a significant effect of HCV status on activity impairment (b = 0.17, p < 0.0001). Levels of activity impairment were 47.91% among patients with HCV, compared with 40.22% among matched controls.
Discussion
The aim of this project was to document, using a nationally-representative sample, the effect of HCV on labor force participation and productivity loss. The regression results suggest that patients with HCV are significantly less likely to participate in the labor force and have significantly greater work productivity loss and impairment in daily activities. Using a propensity score methodology to replicate those findings, many of the regression results were corroborated. The lone exception was that labor force participation was not significantly lower in the HCV group using propensity score matching. In part, this may be due to the statistical power discrepancy. Because the regression model approach had a much larger control group, the power to detect small effects was enhanced. It is possible the effect of HCV on labor force is present but relatively modest (indeed, the trend was such that those with HCV had lower labor force participation rates). In contrast, the impact of HCV on productivity loss and activity impairment was detected in both methodologies, highlighting the magnitude of these effects.
These findings have important implications given the limited number of studies investigating the impact of HCV on labor force participation, absenteeism and presenteeism. Indeed, only one national study could be identified that assessed the impact of HCV on employment statusCitation9. This study found that positive HCV status with normal alanine aminotransferase (ALT) levels in males was associated with a 10.7% reduction in labor force participation while positive HCV status and elevated ALT was associated with a 17.5% reduction.
Our results also suggest a detrimental effect of HCV on labor force participation, though only when analyzed using a logistic regression approach. It is important to note that the Jacobs et al.Citation9 analysis controlled for self-perceived health status but not a complete list of comorbidities as done in the present analysis. By demonstrating a significant effect even after controlling for comorbidities, anxiety, and depression, the incremental effect of HCV was more properly isolated (though, as noted above, this effect is likely small).
The literature on the impact of HCV on absenteeism and presenteeism is just as limited with only one study identifiedCitation11. Su et al. utilized employee records from multiple large employers in the US and found (via regression modeling) that employees with HCV had 1.85 times more absence days than controlsCitation11. The number of annual absence days varied by type. The difference was smaller for those taking sick leave and for those on workers’ compensation and greater for those on short-term or long-term disability. Overall, those with HCV recorded 4.15 more days of absence per employee than the control cohort. Productivity was lower with employees with HCV processing 7.5% fewer units per hour than controls. All healthcare benefit costs among employees with HCV were significantly higher than the same costs among employees without HCV.
Our absenteeism results were consistent with Su et al.Citation11, in that levels of absenteeism were 1.61 times higher (4.88 vs. 3.03%) in our regression modeling approach. However, our presenteeism results were much stronger than Su et al.Citation11 in that impairment was 1.24 times higher (16.69 vs. 13.50%) in our regression modeling approach. The difference in effects may be due to the use of employer data versus our use of patient reports; the latter of which may be better suited to picking up more subtle effects of productivity, especially in cases when employee productivity is difficult for employers to quantify. It is also important to note that the Su et al.Citation11 paper used linked employer and claims data, which would have neglected patients whose physician did not code their HCV diagnosis. Further, the sample was skewed towards full-time employees. The Su et al.Citation11 study also neglected those not currently employed. Indeed, the current study was the first of its kind to demonstrate the impact of HCV infection on impairment outside of the workplace.
Limitations
All HCV diagnoses and work productivity measures were patient-reported and may have introduced measurement error. Although the results from the propensity scoring and regression modeling generally coincided in demonstrating the burden of HCV on work productivity, it is possible that there may be additional variables not included, which could explain the observed differences in health outcomes. This is an important limitation. However, it should be noted that the most likely alternative explanations for the relationship between HCV status and work productivity (such as comorbidities, health behaviors, etc) have been accounted for in both a regression modeling and propensity score matching framework. The Internet survey methodology represents another limitation, as certain disenfranchised groups without Internet access would not have been able to participate. Naturally, this study only includes respondents from the US and it is not clear whether these effects generalize to other geographies. It is also important to note that the study was cross-sectional and likely included a mix of HCV patients, from those newly diagnosed to those who are in the later stages of infection. It would be informative, particularly for some employers with a short-term focus, to use a time series approach to document work productivity changes pre- and post-HCV diagnosis. Although using both a regression approach and a propensity score matching approach provided a robust series of results, other methodologies (such as a multi-part model) may be useful, particularly when estimating specific costs associated with HCV.
Conclusions
Although much of the work in the HCV area has focused on direct costs, our results suggest the indirect costs should not be ignored when quantifying the societal burden of HCV. To our knowledge, this is the first study which has utilized a large, nationally-representative data source for identifying the impact of HCV on labor force participation and work and activity impairment using both a propensity-score matching and regression modeling framework. Results from both methodologies converged to indicate that HCV is associated with persistent indirect economic costs from a societal perspective.
Transparency
Declaration of funding
The National Health and Wellness Survey (NHWS) is conducted by Kantar Health. Bristol-Myers Squibb purchased access to the NHWS dataset and funded the analysis for this project.
Declaration of financial relationships
Both M.D. and J.-S.W. of Kantar Health while Y.Y. and G.L. are employees of Bristol-Myers Squibb. P.L. served as a consultant to Kantar Health.
Acknowledgments
No assistance in the preparation of this article is to be declared.
References
- Centers for Disease Control and Prevention. Hepatitis C information for the public. Retrieved on December 12, 2010: http://www.cdc.gov/hepatitis/C/cFAQ.htm#overview
- Centers for Disease Control and Prevention. Surveillance for acute viral hepatitis: United States, 2007. MMWR Surveill Sum 2009;58:SS-3.
- Armstrong GL, Wasley A, Simard EP, et al. The prevalence of hepatitis C virus infection in the United States, 1999 through 2002. Ann Intern Med 2006;144:705-14
- McHutchison JG, Bacon BR, Owens GS. Making it happen: managed care considerations in vanquishing hepatitis C. Am J Manag Care 2007;13:S327-36
- Kim WR. The burden of hepatitis C in the United States. Hepatology 2002;36(5 Suppl 1):S30-4
- Leigh JP, Bowlus CL, Leistikow BN, et al. Costs of hepatitis C. Arch Intern Med 2001;161:2231-7
- Wong JB, McQuillan GM, McHutchison JG, et al. Estimating future hepatitis C morbidity, mortality, and costs in the United States. Am J Public Health 2000;90:1562-9
- Armstrong EP, Charland SL. Burden of illness of hepatitis C from a managed care organization perspective. Curr Med Res Opin 2004;20:671-9
- Salomon JA. Weinstein MC, Hammitt JK, et al. Cost-effectiveness of treatment for chronic hepatitis C infection in an evolving patient population. JAMA 2003;290:228-37
- Jacobs P, Ng YC, Stafinski T, et al. Labour force participation among individuals with hepatitis C in the US. Pharmacoeconomics 2003;21:565-72
- Montoya ID, Atkinson J, Lichtiger B, et al. Prevalence of hepatitis C in a drug using and non-using welfare population. Health Policy 2003;64:221-8
- Su J, Brooks RA, Kleinman NL, et al. The impact of hepatitis C virus on work absence, productivity, and healthcare benefit costs. Hepatology 2010;52:436-42
- Perrillo R, Rothstein KD, Rubin R, et al. Comparison of quality of life, work productivity and medical resource utilization of peginterferon alpha 2a vs the combination of interferon alpha 2b plus ribavirin as initial treatment in patients with chronic hepatitis C. J Viral Hepat 2004;11:157-65
- Lim HJK, Cronkite R, Goldstein MK, et al. The impact of chronic hepatitis C and comorbid psychiatric illnesses on health-related quality of life. J Clin Gastroenterol 2006;40:528-34
- Kwan JW, Cronkite RC, Yiu A, et al. The impact of chronic hepatitis C and co-morbid illnesses on health-related quality of life. Qual Life Res 2008;17:715-24
- Hauser W, Holtmann G, Grandt D. Determinants of health-related quality of life in patients with chronic liver disease. Clin Gastroenterol Hepatol 2004;2:157-63
- Bonkovsky HL, Woolley JM. Reduction of health-related quality of life in chronic hepatitis C and improvement with interferon therapy. Hepatology 1999;29:264-70
- Kallman J, O’Neil MM, Larive B, et al. Fatigue and health-related quality of life (HRQL) in chronic hepatitis C virus infection. Dig Dis Sci 2007;52:2531-9
- Gallegos-Orozco JF, Fuentes AP, Gerado-Argueta J, et al. Health-related quality of life and depression in patients with chronic hepatitis C. Arch Med Res 2003;34:124-9
- Falasca K, Mancino P, Ucciferri C, et al. Quality of life, depression, and cytokine patterns in patients with chronic hepatitis C treated with antiviral therapy. Clin Invest Med 2009;32:E212-18
- DiBonaventura MD, Wagner JS, Yuan Y, et al. Humanistic and economic impacts of hepatitis C infection in the United States. J Med Econ 2010;13:709-718
- Bolge SC, Doan JF, Kannan H, et al. Association of insomnia with quality of life, work productivity, and activity impairment. Qual Life Res 2009;18:415-22
- Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. PharmacoEconomics 1993;4:353-65
- Gardner W, Mulvey EP, Shaw EC. Regression analyses of counts and rates: Poisson, overdispersed poisson, and negative binomial models. Psych Bull 1995;118:392-404
- Parsons LS. Reducing bias in a propensity score matched-pair sample using greedy matching techniques. Proceedings of the Twenty-Six Annual SAS_Users Group International Conference, Cary, NC: SAS Institute Inc., 2004;214–26