Abstract
Background:
Exacerbations are a major contributor to the large burden of treating chronic obstructive pulmonary disease (COPD). Estimates of exacerbation costs in the United States are limited.
Objective:
To estimate incremental costs associated with COPD exacerbation, particularly severe exacerbation, in the United States.
Methods:
COPD patients with at least one exacerbation were identified in the Thomson Reuters MarketScan administrative claims database. A COPD exacerbation was defined as patient use of oral or parenteral corticosteroids on the same day or within 7 days following a claim with a COPD diagnosis. Severe exacerbation was further defined if the exacerbation was associated with hospitalization or death. Healthcare costs and exacerbations were evaluated at quarterly intervals starting from patients’ first observed claim with COPD diagnostic code in the database. Incremental costs associated with exacerbation were estimated as cost differences between quarters with exacerbation and quarters without exacerbation.
Results:
A total of 2644,174 patient-quarters, derived from 228,978 COPD patients, were included in the analysis. The average patient was followed an average of 2.9 years. The mean total cost was $17,016 per patient-quarter with severe exacerbation, $6628 per patient-quarter with non-severe exacerbation, an average of $8726 per patient-quarters with any exacerbation compared to $4762 per patient-quarter with no exacerbation. After adjusting for patient demographics, the mean incremental total cost was $11,261 per patient-quarter with severe exacerbation, $1509 per patient-quarter for non-severe exacerbation, and $3439 per patient-quarter with any exacerbation compared with patient-quarters with no exacerbation.
Limitations:
The method used for defining exacerbations does not capture mild exacerbations. Additional limitations exist due to the nature of claims data.
Conclusions:
Exacerbations, especially severe ones, result in a significant economic burden for third-party payers. Effective management of COPD and prevention of exacerbations may lead to improved patient outcomes and reduction in total healthcare costs for long-term management of COPD.
Introduction
Chronic obstructive pulmonary disease (COPD) is a progressive disease, characterized by chronic airflow obstruction and pathological changes in the lungCitation1. Chronic lower respiratory disease, primarily consisting of COPD, is the fourth leading cause of death in the United StatesCitation2, and is the only disease among the top five leading causes of death with a rising mortality rateCitation3. In 2006, an estimated 12.1 million American adults were diagnosed with COPDCitation4. The annual cost of COPD in the US is projected to reach $49.9 billion in 2010, including $29.5 billion in direct healthcare expenditures and $20.4 billion in indirect costs due to morbidity and mortalityCitation5.
COPD exacerbations are inflammatory events characterized as recurrent episodes of acute worsening of COPD symptoms such as increased dyspnea, cough, and sputum production that often require an adjustment to the patient’s prior pharmacotherapy regimenCitation1,Citation6. Exacerbations are associated with high rates of hospitalization and mortality as well as reduced quality of lifeCitation1,Citation5,Citation7,Citation8. Exacerbations are a major contributor to the large economic burden of COPDCitation8–11, and have been shown to account for 35–45% of the total cost of COPD treatmentCitation12. Published cost estimates of exacerbation vary widely due to differences in data used, definition of exacerbations, and study populationsCitation12–15. A prospective Spanish study reported a cost of $159 per episode of COPD exacerbationCitation13. Hospitalizations accounted for 58% of the total cost. Similarly, in a Swedish study which identified exacerbations by using patient surveys, the estimated cost to treat an exacerbation ranged from SEK120 (approx. $12) for a mild event to SEK21,852 (approx. $2128) for a severe eventCitation12. Oostenbrink et al. estimated that a severe exacerbation cost €4007 (approx. $5046), dramatically higher than a moderate event (€579; approx. $729)Citation15. Finally, a recent Canadian study derived from a prospective trial of COPD patients estimated the average healthcare cost to be CAN$641 (approx. $649) per non-severe exacerbation and CAN$9557 (approx. $9672) per severe exacerbationCitation14.
While international economic evaluations are useful in showing that the magnitude of exacerbation related costs are large, it is difficult to directly link the costs from other countries to costs in the United States due to differences in the COPD treatment strategy and in the overall healthcare systems. To our knowledge, there are only few studies conducted in the United States that attempted to quantify the cost of COPD exacerbation using real-world data. One is a prospective study by Connors et al., published more than 10 years ago, which estimated the median cost of a hospitalization due to exacerbation at approximately $7100Citation1Citation6. Other manuscripts were published while this manuscript was in preparation, such as work by Mapel and colleagues which estimated that the median 6-month costs of severe exacerbation ranged from $11,016 to $12,349 depending on disease complexityCitation17. However, these study findings may not be generalizable to the larger COPD population, as the Connors study is limited to severe COPD patients admitted to the hospital and the Mapel study is based on patients from a single health plan. Additionally, Dalal and colleagues recently published several papers estimating the costs for COPD-related outpatient services, emergency department (ED) visits, and inpatient admissionsCitation18–20. These studies provide good estimates of the total costs incurred by COPD patients if they have ED and hospitalization due to exacerbations. However, since COPD patients generally require maintenance medications and often have significant comorbidities that may result in emergency care and hospitalizationsCitation21–23, the estimates from the above studies may be confounded by the general COPD maintenance cost and costs for treating comorbidities.
The objective of the current retrospective, observational study was to estimate the incremental costs associated with COPD exacerbation, particularly severe exacerbation, in the United States using a large claims database. As the prevention and reduction of exacerbations is an important endpoint for the outcomes of COPD management, accurate and current estimates of COPD exacerbation costs are warranted to better understand the economic benefits of reducing exacerbations. The present analysis was performed from the third-party payer perspective.
Methods
Data source
De-identified healthcare service claims and cost data of COPD patients were extracted from Thomson Reuters MarketScan database, combining the Commercial Claims and Encounter database and the Medicare Supplemental and Coordination of Benefits database. The former data source aggregates healthcare claims from approximately 100 third-party payers, including self-insured employers and health insurance plans. The latter data source houses healthcare claims for patients aged 65 and older who have employer-sponsored Medicare plans.
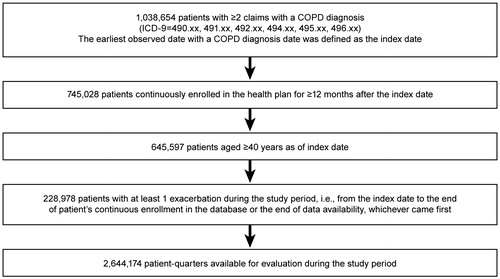
Patient population
Patients were included in the study if they had at least two claims associated with a COPD diagnostic code (International Classification of Diseases, 9th Revision, Clinical Modification [ICD-9-CM] codes: 490.xx–492.xx, 494.xx–496.xx) and experienced at least one episode of COPD exacerbation within the time frame of January 1, 2004 and December 31, 2008. The date on which the first claim with a COPD diagnostic code occurred was defined as the index date. Patients were 40 years and older on the index date and had continuous eligibility for at least 12 months following their index date. A COPD exacerbation was identified if a patient had a claim for oral or parenteral corticosteroids on the same day or within 7 days following a COPD claim. Exacerbations were further categorized as being severe or non-severe. A severe exacerbation was defined as an exacerbation involving either a hospitalization on the same day or death (identified by a discharge status of died or by ICD-9 codes of 798) within 7 days of the COPD diagnosis, otherwise, the exacerbation was defined as non-severe.
Study design
This study used a longitudinal analytical approach in which patient-quarters, instead of individual patients, were the unit of evaluation. A similar design was used by Delea and colleagues in a study of asthma patientsCitation24. For the current study, each patient was followed from the index date through the end of his or her plan eligibility in the database. Each patient’s follow-up period was divided into quarters with 90 days in each quarter. Each quarter was marked as a patient-quarter with severe exacerbation, non-severe exacerbation, or no exacerbation based on whether an exacerbation occurred in that quarter and the severity of the event. If both severe and non-severe exacerbations occurred for a particular patient-quarter, that patient-quarter was labeled as a patient-quarter with severe exacerbation.
Outcome measures
The endpoint measured in this study was the quarterly incremental cost associated with COPD exacerbation, calculated as the difference in mean cost between the patient-quarters with exacerbation and patient-quarters without exacerbation.
Healthcare costs were analyzed in terms of all-cause costs and COPD-related costs. All-cause costs comprised all medical claims regardless of diagnosis and all prescription drug claims. COPD-related costs consisted of only those medical claims associated with a COPD diagnosis and prescription drug claims for the following COPD-related medications: short-acting and long-acting β2-adrenergic agonists, anticholinergic bronchodilators, methylxanthines, corticosteroids, and COPD-related antibioticsCitation1. All costs were inflation-adjusted to the 2008 US dollar value.
Statistical analysis
Patient demographics were collected on the index date. The number of patient-quarters with severe, non-severe, any (a combination of severe and non-severe exacerbations), or no exacerbation observed during the study period were reported. Costs were calculated for patient-quarters as stratified by exacerbation severity. Incremental costs were calculated in four separate comparisons: (1) difference between the mean cost of patient-quarters with any exacerbations and patient-quarters with no exacerbations; (2) difference between patient-quarters with severe exacerbations and those with no exacerbations; (3) difference between patient-quarters with severe exacerbations and those with non-severe exacerbations; and (4) difference between patient-quarters with non-severe exacerbations and no exacerbations. Unadjusted costs between patient-quarters were compared using Wilcoxon rank-sum test. Adjusted incremental costs were calculated using generalized estimating equation (GEE) methods controlling for age, gender, region of residence, type of insurance plan, index year, and the time of each quarter from the index date (expressed as sequential quarterly indicator). The GEE method accounts for the potential correlations between multiple observations from the same patient. All statistical analyses were performed using SAS 9.2 (SAS Institute, Inc., Cary, NC, USA).
Results
A total of 228,978 COPD patients who experienced at least one exacerbation met the inclusion criteria (). As presented in , the average age of the study patients was 65.7 (SD 12.0) years, and 43.1% were male. The mean duration of follow-up was 2.9 (SD 1.3) years (). Severe exacerbation occurred at least once to 66,680 (29.1%) patients. Collectively, a total of 2644,174 patient-quarters were included in the analyses. Among them, 446,690 (16.9%) patient-quarters contained at least one COPD exacerbation, including 90,210 (3.4%) patient-quarters in which at least one severe exacerbation occurred.
Table 1. Patient demographics.
Table 2. Patient characteristics during follow-up study period.
Based on unadjusted analysis, the average all-cause total cost per patient-quarter with any COPD exacerbation was $8726 (SD $20,108), which was higher than the cost per patient-quarter with no exacerbation of $4762 (SD $13,082) (p < 0.0001, ). There was a large difference between the all-cause total cost per patient-quarter with severe $17,016 (SD $24,675) and non-severe $6628 (SD $18,188) exacerbations (p < 0.0001). The COPD-related total cost was higher per patient-quarter with any exacerbation at $2631 (SD $12,087) than that with no exacerbation, which was $658 (SD $3336) (p < 0.0001). The COPD-related total cost per patient-quarter with severe exacerbation was $7014 (SD $13,278) higher than the cost per patient-quarter with non-severe exacerbations of $1522 (SD $11,505) (p < 0.0001).
Table 3(a). Quarterly healthcare costs by exacerbation (US$ 2008).
Table 3(b). Quarterly healthcare costs by exacerbation (US$ 2008) – unadjusted incremental cost.
After controlling for patient characteristics, the adjusted all-cause incremental total cost associated with any COPD exacerbation, as compared with no exacerbation, was $3439 per patient-quarter (p < 0.0001, ). The adjusted all-cause incremental total cost was particularly high for patient-quarters with severe exacerbations: $11,261 per patient-quarter compared with no exacerbation (p < 0.0001) and $10,257 per patient-quarter compared with non-severe exacerbation (p < 0.0001). The incremental inpatient cost associated with severe exacerbation was the predominant contributor to the high incremental total cost incurred during these quarters. The adjusted all-cause incremental total cost associated with non-severe exacerbation, as compared with no exacerbation, was $1509 per patient-quarter (p < 0.0001, ), mainly comprised of the incremental outpatient cost of $786 (p < 0.0001).
Table 4. Quarterly healthcare costs by exacerbation (US$ 2008) – adjusted incremental cost.
The adjusted COPD-related incremental costs showed similar patterns. The adjusted COPD-related incremental total cost associated with any exacerbation, compared with no exacerbation, was $1831 per patient-quarter (p < 0.0001). The adjusted COPD-related incremental total cost associated with severe exacerbation was $6116 (p < 0.0001) and $5461 (p < 0.0001) per patient-quarter compared with no exacerbation and non-severe exacerbation, respectively. Again, incremental inpatient costs accounted for nearly all of the incremental total costs associated with severe exacerbation. The adjusted COPD-related incremental total cost per patient-quarter for non-severe exacerbation was $775 compared with no exacerbation (p < 0.0001).
Discussion
This study was designed to estimate the economic impact of COPD exacerbations costs associated with management of COPD in the United States. The current study has estimated that COPD patients will incur healthcare savings of $3439 per quarter by preventing any exacerbation and of $11,261 by preventing severe exacerbations (). These results confirm the findings of several previous studies that costs associated with COPD exacerbations are high and vary greatly by the severity of the episode. Therefore, effective treatments that prevent and reduce the severity of exacerbations can be expected to not only provide clinical benefitsCitation9 for patients but also reduce the economic costs associated with COPD management.
In this study, the COPD-related incremental total costs per patient-quarter for any exacerbation, compared with no exacerbation, were approximately half of the all-cause incremental total costs ( and ). This observation may be explained by the systemic nature of COPD in that these patients’ comorbidities, such as cardiovascular disease and osteoporosis, may also worsen as a consequence of COPD exacerbation and require additional treatmentCitation21–23. However, such occurrences of medical resource use might not be coded with a COPD diagnosis code. Therefore, COPD-related total incremental costs may be an under-estimation of the economic burden of COPD exacerbations. This is consistent with a previous study based on Medicaid claims data, in which the excess cost of COPD patients compared to non-COPD controls was nearly two to three times of the COPD-related costCitation25. The all-cause incremental total cost of $3439 per patient-quarter (any exacerbation vs. no exacerbation) is likely to be a more accurate estimation of the economic burden of COPD exacerbation than the COPD-related incremental total cost of $1831 ().
Although exacerbations are an important clinical endpoint, it is challenging to estimate the actual per-episode cost because there is no standard definition of an exacerbation episode. As stable COPD patients often experience day-to-day variations in symptoms, it is difficult to: (a) clearly identify an exacerbation, (b) determine the duration of an episode, or (c) distinguish a new exacerbation episode from a relapse of the original episodeCitation26. Previous economic studies have used a variety of methods to identify the presence and duration of an exacerbation episode. Andersson and colleagues collected data for their analyses from telephone interviews with patients relying on recall of their COPD symptoms and treatments received in the previous 4 monthsCitation12. A prospective UK study by O’Reilly and colleagues used patient diaries over 12 months to compare symptom defined exacerbations with healthcare resource use defined exacerbations. Approximately 41–54% of exacerbations could be identified using both criteriaCitation27. In the previously mentioned Canadian study, clinical details were reviewed to identify exacerbation as the worsening of COPD symptoms. Moderate and severe exacerbations were further defined as events associated with an alteration of medications and visits to medical facilitiesCitation14. The current study used a claims database which contained limited clinical information. The data did not allow for the use of specific clinical assessments, nor did it allow for clearly defining the start, end, and duration of an exacerbation episode. Similar to other claims studies of COPD exacerbations, in this study exacerbation was identified by using healthcare resource useCitation6,Citation27,Citation28. Severity was further defined using a criterion previously used by Calverley and colleaguesCitation29.
The current study has estimated that the all-cause incremental total cost associated with severe exacerbation was $11,261 per patient-quarter. This estimate takes into account that patients in this study experienced, on average, approximately 1.15 episodes of exacerbations per patient-quarter among quarters with exacerbation (estimated using the assumptions that two exacerbations within 2 weeks of each other were considered as one episode). Therefore, our cost estimates could be loosely interpreted as the cost per exacerbation episode. This estimate for severe exacerbation was similar to the cost of CAN$9557 (approx. $9672) per severe episode reported in a Canadian studyCitation14, but higher than other studiesCitation12,Citation15, which is likely due to differences in study design, patient populations, and healthcare systems.
One limitation of this study is that the exacerbation criterion used here was representative of moderate and severe exacerbations, but not mild exacerbations. However, it has been shown that mild exacerbations pose a small costCitation17, possibly due to the fact that patients are not as likely to seek treatment, or are treated with an increase in the dose and frequency of general daily medicationsCitation30. Additionally, our study selected patients who had experienced at least one exacerbation and may not include COPD patients with milder symptoms. Further, the data used for this study were recorded from 2004 to 2008, thus the study results may not be generalizable to more recent years where the introduction of new and more costly treatments for exacerbations might further increase the cost. Furthermore, with respect to identifying COPD exacerbations the study uses a claims database to identify exacerbation which, due to the potential for missing information in the claims could omit certain exacerbations from being identified. This is especially possible for a severe exacerbation with hospitalization. However, the authors feel confident though that the method used in this study is more conservative than other approaches that have been used in the past to identify exacerbations in claims data. Finally, due to the nature of claims data, it is likely that not all deaths will be captured, especially those which occurred in outpatient settings.
Despite these limitations, this study provides one of the first practical, comprehensive, and large-scale quantitative analyses of the costs of treating COPD exacerbations in the United States. The use of claims data allows for the study of a large and diverse group of patients over a longer period of time than is typically available in prospectively defined research using data collected directly from patients. Therefore, the sample used here may be more reflective of general COPD populations in the United States. As exacerbation becomes more consistently defined and accurately measured, future research may be able to better delineate the components of healthcare costs of treating exacerbation and help clinicians, policy makers, and managed care organizations to more effectively predict costs and allocate resources.
Conclusions
The economic burden of treating exacerbations in the management of COPD patients is significant, and the incremental cost of treating severe exacerbations is far greater than that of non-severe episodes. The findings suggest that effective prevention and reduction of exacerbations would lead to substantial cost reduction in the management of COPD.
Transparency
Declaration of funding
This study was carried out by Analysis Group, Inc. Funding for this study was provided by Forest Research Institute. A.P.Y., E.Q.W., H.Y., J.S., M.M., and S.B. contributed to the conception and design of this study; H.Y. and A.P.Y. performed data analysis; A.P.Y., E.Q.W., H.Y., J.S., M.M., and S.B. provided data interpretation; and A.P.Y., E.Q.W., H.Y., J.S., M.M., and S.B. wrote and approved the manuscript.
Declaration of financial/other relationships
A.P.Y., H.Y., and E.Q.W. are employees of Analysis Group Inc., which has received consulting fees from Forest Research Institute for research related to this manuscript. J.S. was an employee of Forest Research Institute when this study was conducted. M.M. and S.B. are employees of Forest Research Institute.
Acknowledgments
A prior version of this study was presented in poster form at the 15th annual international meeting of the International Society for Pharmacoeconomics and Outcomes Research, May 15–19, 2010, in Atlanta, GA, USA. Prescott Medical Communications Group (Chicago, IL, USA) provided editorial assistance funded by Forest Research Institute.
References
- Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (Updated 2009) 2009; http://www.goldcopd.com/download.asp?intId=554. Accessed 6 April, 2010
- Xu J, Kochanek KD, Murphy SL, Tejada-Vera B. Deaths: Final Data for 2007. National Vital Statistics Report 2010; http://www.cdc.gov/nchs/data/nvsr/nvsr58/nvsr58_19.pdf. Accessed 27 August, 2010
- Gudmundsson G, Gislason T, Lindberg E, et al. Mortality in COPD patients discharged from hospital: the role of treatment and co-morbidity. Respir Res 2006;7:109
- American Lung Association. Trends in COPD (Chronic Bronchitis and Emphysema): Morbidity and Mortality. Report 2010; http://www.lungusa.org/finding-cures/our-research/trend-reports/copd-trend-report.pdf. Accessed 6 April, 2010
- National Heart Lung and Blood Institute. Morbidity and Mortality: 2009 Chart Book on Cardiovascular, Lung, and Blood Diseases 2009; http://www.nhlbi.nih.gov/resources/docs/2009_ChartBook.pdf. Accessed 6 April, 2010
- Effing TW, Kerstjens HA, Monninkhof EM, et al. Definitions of exacerbations: does it really matter in clinical trials on COPD? Chest 2009;136:918–23
- Rodriguez-Roisin R. Toward a consensus definition for COPD exacerbations. Chest 2000;117(5 Suppl 2):398–401S
- Simoens S, Decramer M, Laekeman G. Economic aspects of antimicrobial therapy of acute exacerbations of COPD. Respir Med 2007;101:15–26
- Anzueto A, Sethi S, Martinez FJ. Exacerbations of chronic obstructive pulmonary disease. Proc Am Thorac Soc 2007;4:554–64
- Sullivan SD, Ramsey SD, Lee TA. The economic burden of COPD. Chest 2000;117(2 Suppl):5–9S
- Hilleman DE, Dewan N, Malesker M, et al. Pharmacoeconomic evaluation of COPD. Chest 2000;118:1278–85
- Andersson F, Borg S, Jansson SA, et al. The costs of exacerbations in chronic obstructive pulmonary disease (COPD). Respir Med 2002;96:700–8
- Miravitlles M, Murio C, Guerrero T, et al. Pharmacoeconomic evaluation of acute exacerbations of chronic bronchitis and COPD. Chest 2002;121:1449–55
- Mittmann N, Kuramoto L, Seung SJ, et al. The cost of moderate and severe COPD exacerbations to the Canadian healthcare system. Respir Med 2008;102:413–21
- Oostenbrink JB, Rutten-van Molken MP. Resource use and risk factors in high-cost exacerbations of COPD. Respir Med 2004;98:883–91
- Connors AF, Jr., Dawson NV, Thomas C, et al. Outcomes following acute exacerbation of severe chronic obstructive lung disease. The SUPPORT investigators (Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments). Am J Respir Crit Care Med 1996;154(4 Pt 1):959–67
- Mapel DW, Schum M, Lydick E, et al. A new method for examining the cost savings of reducing COPD exacerbations. Pharmacoeconomics. 2010;28:733–49
- Dalal AA, Christensen L, Liu F, et al. Direct costs of chronic obstructive pulmonary disease among managed care patients. Int J Chron Obstruct Pulmon Dis 2010;5:341–9
- Dalal AA, Shah M, D'Souza AO, et al. Costs of inpatient and emergency department care for chronic obstructive pulmonary disease in an elderly Medicare population. J Med Econ 2010;13:591–8
- Dalal AA, Shah M, D'Souza AO, et al. Costs of COPD exacerbations in the emergency department and inpatient setting. Respir Med 2011;105:454–60
- Antonelli Incalzi R, Fuso L, De Rosa M, et al. Co-morbidity contributes to predict mortality of patients with chronic obstructive pulmonary disease. Eur Respir J 1997;10:2794–800
- Adams SG, Melo J, Luther M, et al. Antibiotics are associated with lower relapse rates in outpatients with acute exacerbations of COPD. Chest 2000;117:1345–52
- Rabe KF, Hurd S, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 2007;176:532–55
- Delea TE, Stanford RH, Hagiwara M, et al. Association between adherence with fixed dose combination fluticasone propionate/salmeterol on asthma outcomes and costs. Curr Med Res Opin 2008;24:3435–42
- Marton JP, Boulanger L, Friedman M, et al. Assessing the costs of chronic obstructive pulmonary disease: the state Medicaid perspective. Respir Med 2006;100:996–1005
- Vijayasaratha K, Stockley RA. Reported and unreported exacerbations of COPD: analysis by diary cards. Chest 2008;133:34–41
- O'Reilly JF, Williams AE, Holt K, et al. Defining COPD exacerbations: impact on estimation of incidence and burden in primary care. Prim Care Respir J 2006;15:346–53
- Suh DC, Lau H, La HO, et al. Association between incidence of acute exacerbation and medication therapy in patients with COPD. Curr Med Res Opin 2010;26:297–306
- Calverley PM, Rabe KF, Goehring UM, et al. Roflumilast in symptomatic chronic obstructive pulmonary disease: two randomised clinical trials. Lancet 2009;374:685–94
- Hurst JR, Wedzicha JA. Management and prevention of chronic obstructive pulmonary disease exacerbations: a state of the art review. BMC Med 2009;7:40