Abstract
Objectives:
Heart failure is an increasing burden for all healthcare systems with prevalence reaching over 20 million patients worldwide and direct costs of disease requiring ∼1% of healthcare budget expenditures. Beyond traditional pharmaceutical treatment, medical devices and remote monitoring tools were introduced to ensure a closely managed control of patients. In this context, a decision-maker needs to know whether the new technology provides clinical benefit towards patients and what resource use is attached to them.
Methods:
Health services research is a complementary approach to clinical trials providing results to the impact of the technology in real life settings. As an example this study reports of a secondary data analysis of one of the largest health insurance companies in Germany, comparing resource use of heart failure patients receiving a cardiac resynchronization therapy (CRT) device coupled with a fluid status monitoring and alert function with patients receiving conventional CRT, ICD (implantable cardioverter defibrillator), or no intervention.
Results:
Disease-associated expenses can be attributed to far more than 50% to heart failure. Although implementation of the CRT device with alert function was most expensive (31,794 Euros compared to 27,659 Euros in the conventional CRT group, 24,128 Euros in the ICD group, and 3735 Euros in the no intervention group) in the first year after implementation, the least costs have been caused in this group (7000 Euros compared to more than 11,000 Euros in all other groups).
Conclusion:
This article highlights potential health services research approaches focusing on the example of a CRT device coupled with a pulmonary diagnostic and alert function. Although this retrospective analysis holds a number of limitations (e.g., small number of patients in intervention group, cost calculations only from the payer perspective), and despite the need for randomized controlled trials, it was shown that secondary data research in this field is a valuable approach.
Introduction
Heart failure specified by the ICD 10 Code I50 is the second most common reason for hospitalization in GermanyCitation1. Since 2000 the number of hospitalizations increased 1.5-fold from 239,694 to 363,662 casesCitation1. Worldwide over 20 million, in Germany ∼1.6–2 million people suffer from heart failure, with prevalence being strongly associated with ageCitation2,Citation3. While 2% of the overall population is estimated to be affected by heart failure, in patients aged 65 years and older already 5–10% suffer from this diseaseCitation2. Every year in Germany ∼200,000–300,000 new cases are diagnosedCitation3. Heart failure is defined as the inability of the heart to supply the organism with sufficient blood and oxygenCitation2,Citation4. Typical symptoms are dyspnoea, fatigue and fluid retention leading to repeated hospitalization, reduced quality-of-life, and life expectationCitation2,Citation4. In Western countries in 60–75% of cases the cause of heart failure can be attributed to coronary heart disease and/or arterial hypertension, in ∼20–30% of cases aetiology is not clearCitation2.
Therapy aims primarily at treatment of the underlying cause of the disease: Besides pharmacological therapy, also surgical therapy, including pacemaker (CRT, cardiac resynchronisation therapy) and cardioverter defibrillator (ICD, implantable cardioverter defibrillator) are applied depending on severityCitation5. The severity of heart failure is classified in the four stages of the New York Heart Association (NYHA I–IV) where in NYHA I the patient is not impaired in daily life, in NYHA II high physical stress and in NHYA III already little physical stress causes symptoms while in NYHA IV the patient perceives symptoms even at restCitation5.
Despite therapeutic advances prognosis of heart failure remains poor. About 60–70% of patients die in the first 5 years after diagnosis, mainly due to progressive disease or arrhythmia with sudden cardiac deathCitation2. With a total of 48,954 cases of deaths heart failure was the fourth most common cause of death in Germany in 2009 after chronic ischemic heart disease, acute myocardial infarction and lung cancerCitation6. High number of hospitalizations, considerably rising number of future patients and cost-intensive therapy options result in heart failure being one of the most cost intensive diseases. According to an analysis of the official German statistics in 2006, ∼1.2% of the total direct disease costs of all diagnoses were caused by heart failure, amounting to 2.9 billion EurosCitation7,Citation8. Thereof ∼45%, 1.3 billion Euros, were estimated to be spent on hospitalizationsCitation7. The outpatient sector caused costs of ∼784 million Euros, including pharmaceuticals (287 million Euros), ambulatory care (239 million Euros), and physician visits (162 million Euros) as major cost factorsCitation7. A study performed in co-operation with the competence network of heart failure analysing 2710 patients related 74% of total costs to hospitalizationsCitation9.
The medical aspects as well as the health economic relevance elicit the need for better management of heart failure patients. Disease management programmes (DMPs) and remote monitoring is introduced to ensure a closely-managed control of patients.
A recent systematic Cochrane review and meta-analysis including studies between 2006 and 2008 suggests that patients with heart failure benefit from telemonitoring, for example in terms of a substantial reduction in all-cause mortality and a substantial reduction in the risk of hospitalization due to heart failure and leading to improved quality-of-life and reduced costsCitation10. A significantly lower number of deaths and hospitalizations have also been reported by the authors of another meta analysis including studies between 2000 and 2008Citation11. However, three large randomized multi-centre trials, the Tele-HF, the TIM-HF and the HHH study, did not find significant differences between the intervention and control group regarding hospitalization or mortalityCitation12–14. The Home-HF study performed in London, UK, did not find differences due to telemonitoring in days alive and out of hospital as well as no significant differences in mean direct health services costs, but significantly fewer unplanned hospitalizations and a reduction in clinic and emergency room visitsCitation15.
A specific example in heart failure treatment with remote monitoring is a CRT device coupled with an intra-thoracic impedance monitoring and alert function. The OptiVol System (Medtronic GmbH, Germany) introduced in 2004 is remotely monitoring the fluid status in the lung and warning at an early stage against pulmonary congestion that may lead to hospitalization and progress of heart failure.
A decision-maker needs to know whether, first, new technologies improve the clinical benefit towards patients and, second, at what costs. The contribution of new technologies such as the fluid status monitoring device to the medical benefit or economic implications in routine care might also be scrutinized based on health services research. This article analyses approaches to answer this question.
Health services research and secondary data analysis
According to the German Medical Association (Bundesärztekammer), health services research is defined as scientific analysis of care of individuals or a population with products or services under conditions of daily practiceCitation16. Analysis of the needs for health services (input), structures and processes of health services (throughput), provided services (output), gain in quality-of-life and health (outcome), as well as the direct relevance for health policy are characteristics of health services researchCitation17. For answering this diversity of questions health services research uses different quantitative and qualitative, descriptive, analytical, and evaluative methodsCitation18. Thus, a specific scientific method is not required, but rather defined by the research question. In general, different study types are applicable, including cross-sectional studies, case-control studies, cohort studies, randomized as well as non-randomized interventional studies; collection of primary data as well as secondary data analyses are suitableCitation19. Secondary data analysis is defined as scientific analysis of data not directly based on the primary reason of data collectionCitation20. Secondary databases include claim databases, patient registries, electronic medical record databases and other routinely collected health care dataCitation21, for example routine data of the statutory health insurances (SHI) primarily collected for accounting.
Due to the provided information routine SHI data are suitable for analysis of utilization of medical services, resource use, and costs as well as outcome researchCitation22. Main advantages of routine data are availability of a longer time frame allowing analyses of retrospective as well as prospective research questions, low costs due to the routine collection of data and high granularity of individual patient level dataCitation23. Main disadvantages are collection of data only from the health insurance perspective, i.e., no inclusion of self-pay patients, no specific data collection for a scientific question, unknown validity as well as a potential for selection bias due to a restriction to only a few insurance companiesCitation23.
In order to elucidate the above-mentioned situation in heart failure patients managed with a remote monitoring device secondary data could be used to generate hypotheses on the current medical and economic implication of a new technology, which in turn can then be used as a basis for further confirmatory research with more refined research technologies. The following example highlights a first exploratory study based on secondary data with regard to usage and cost information for further hypothesis generation and study planning.
Pilot study example—Methods
Our example of health services research in heart failure patients based on secondary data is a retrospective pilot study comparing the above-mentioned CRT system coupled with a fluid status monitoring and alert function to conventional systems. For generating hypothesis on the technology’s potential to reduce disease costs a database of one of the largest health insurance companies in Germany has been analysed and searched for patients treated due to heart failure NYHA III–IV (ICD code I50.13 and/or I50.14) and/or due to dilated cardiomyopathy (ICD code I42.0). The nationwide operating SHI company is accessible for 90% of the German population and covers more than 8 million lives.
Only patients aged between 5–89 years having received treatment between 01.01.2004 and 31.12.2006 and being diagnosed heart failure at least once in outpatient or inpatient health care were included and classified in four study groups:
Patients having received a CRT (‘CRT only’);
Patients having received a CRT system with the additional fluid status monitoring and alert function. Patients were either identified via OPS codes or probability linkage (‘CRT plus alert’);
Patients having received an ICD (‘ICD’); and
Patients not having received an ICD or CRT (‘No Implantation’).
Additionally, in a comparison group all insurees at the same age but without any evidence of heart failure NYHA III or IV or dilated cardiomyopathy or supply of ICD or CRT systems were included, representing ordinary insurees of a SHI.
Treatment costs in the four study groups have been determined separately for different periods, specific to the single patient and relative to the day of discharge of index hospitalization. Index hospitalization in the device study groups was the hospital stay where the device was implanted, in the ‘No Implantation’ group index was the hospital stay where heart failure and/or dilated cardiomyopathy was named as primary diagnosis.
All expenses of the insurance company regarding medical treatment, medication from pharmacies, adjuvants, remedies, sick pay, rehabilitation, transportation expenses, treatment abroad, social services, home nursing, and additional services were considered. Data were obtained from risk adjustment scheme data (Risikostrukturausgleich–RSA), hospital data, prescription data, and billing data from outpatient care available within the SHI.
As not all costs caused in patients with heart failure are due to heart failure, gender- and age-specific expected non-heart failure costs were calculated in order to identify the exceeding costs attributable to heart failure. For this purpose daily expenses of the comparison group for the specific account groups, separated by gender, and 5-year age groups were determined.
Pilot study example—Results
In the described time-frame in 129 patients with at least one CRT implantation and in 285 patients with ICD implantation heart failure according to ICD codes I42.0, I50.13, or I50.14 was diagnosed, whereas in 22 patients a CRT with additional fluid status monitoring and alert function was implanted. Consequently, 107 patients were included in the ‘CRT only’ group, 22 in the ‘CRT plus alert’ group, and 285 in the ‘ICD’ group. Additionally, 2662 patients with at least one hospitalization due to heart failure but without any device implantation have been identified. These patients, included in the ‘No Implantation’ group, on average were older than patients of the other groups; therewith the 1-year mortality rate with 26.3% was much higher than in the other groups. Socio-demographic characteristics of the study groups are summarized in ; 1.243 million insurees have been included in the comparison group, representing ordinary insurees.
Table 1. Socio-demographic characteristics.
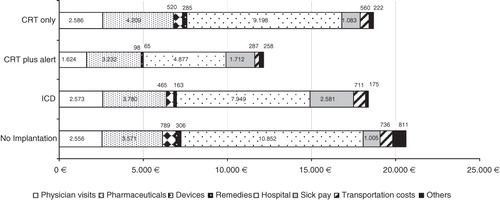
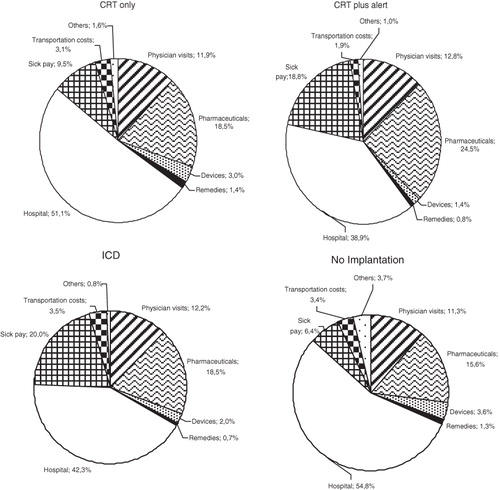
Regarding the cost calculations before index treatment average total costs per quarter in all groups are comparable and range at ∼2000 Euros. In the ‘CRT plus alert’ group the period of index hospitalization was most expensive as for implantation of CRT with additional fluid status monitoring and alert function the health insurance company had to reimburse 31,794 Euros. Index hospital stay in the ‘CRT only’ group accrued to 27,659 Euros, in the ‘ICD’ group to 24,128 Euros and in the ‘No Implantation’ group to 3735 Euros ().
Table 2. Average treatment costs in Euros per patient and quarter.
In the first year after index hospitalization costs for the ‘CRT plus alert’ group were lowest, resulting in ∼7000 Euros compared to more than 11,000 Euros in all other groups ( and ). In the second year costs of 10,531 Euros emerged in the ‘CRT plus alert’ group attributable to one single patient only compared to 7219 Euros in the ‘CRT only’ group, 12,660 Euros in the ‘ICD’ group, and 9602 Euros in the ‘No Implantation’ group ( and ). When excluding patients with total costs exceeding 100,000 Euros within the 2 years after index treatment, total expenses per patient in the second year after index treatment resulted in 5648 Euros in the ‘CRT plus alert’ group, 7219 Euros in the ‘CRT only’ group, 8152 Euros in the ‘ICD’ group, and 8412 Euros in the ‘No Implantation’” group ().
Table 3. Average expenses per patient per year in Euros differentiated by accounting groups.
In reporting total patient costs it always has to be taken into account that only a part can be attributed to a certain disease. Therefore, in this study expected costs have been calculated according to specific gender and age characteristics without diagnosis of heart failure. These expected expenses varied between 600–800 Euros per quarter. Disease-associated expenses then resulted from the difference of the expected costs and the calculated total costs. Comparing the disease-associated expenses with the total expenses in nearly all quarters in all four groups more than 50% of total costs can be attributed to heart failure ().
When ranking the cost categories hospitalization after index treatment was the most relevant cost driver, succeeded by medication, medical outpatient treatment, and sick pay in a different order (, and ) This pilot study was exploratory in nature and has to be followed by more refined analytic approaches.
Discussion
When analysing daily clinical practice, it is of interest to determine whether a specific therapy is efficacious for prevention of disease or reduction in resource use. In observational retrospective data analyses in particular in those outlined above, the treatment receipt mechanism is not under control. Furthermore, it can depend on various factors, including the outcome of interestCitation24. This results in differential selection of treatment groups known as selection bias.
A matched pairs analysis of secondary data might serve as an approximation for avoiding bias. In matched pairs analyses, every individual of the study group is matched with a corresponding individual in a control group. Frequently-used matching criteria are age, sex, ethnicity, co-morbidity, severity of disease, and risk factorsCitation25. With longitudinal data available from German SHI healthcare information on demographic characteristics, ambulatory diagnoses, ambulatory drug treatment (only if reimbursed by SHI), hospitalizations including duration of in-hospital stay, main discharge diagnoses, accessory diagnoses, procedures, reason of discharge, etc., data on resource-consumption such as usage of remedies could be used to address selection bias. Insurants with an incident diagnosis of chronic heart failure, CRT implantation, and implementation of a fluid status monitoring in most recent calendar years could then be identified as cases. Controls without the treatment of interest could be matched by sex, year of birth, and clinical severity. Martin et al.Citation26 have shown that the matching correlation must exceed 0.92 when there are only two pairs, 0.51 when there are five pairs, and ∼0.34 when there are 10 pairs before the power of the matched analysis will exceed that of the unmatched analysis. All insurants (intervention group and controls) are required to be continuously insured since index date. In sensitivity analyses, the impact of the clinical definition could be explored by introducing the requirement of more than one diagnosis of heart failure during the respective calendar year to define subjects with heart failure. Cases and controls have to be categorized according to several characteristics that will be assessed in the time period prior to the index date.
Methods reducing the selection bias seek to properly adjust known and observed confounders via e.g., stratification, standardization, or adjustment. In a prospective research setting where neither a randomized pragmatic trial nor a cluster randomization is feasible, a sequential control design could be applied. This was applied in the GERSHWIN study in 952 consecutively recruited patients with coronary artery disease to be treated with a stent for the reduction of coronary restenosisCitation27. The distribution of potential bias factors like sociodemographic factors, cardiac status, and risk factors between the two patients groups were tested by χ2-test (categorical variables) or t-test (metric). Based on these results the researcher adjusted for age, gender, household status, three-vessel disease, and number of stents in a multiple logistic regression analysis, indicating a clinical benefit with increased direct costsCitation27.
In patients with heart failure, relevant factors to be controlled for comprise the following: pre-existing conditions, hospitalization for cardiac decompensation in a period prior to the analytic index date, already implanted cardiac assist system, heart failure related diseases such as unstable angina pectoris, congenital heart defect, as well as comorbidities such as chronic renal insufficiency or liver cirrhosis and medical treatment for chronic heart failure (ß-blocker, ACE-inhibitor/ARB, diuretics) including ICD/CRT.
The above-outlined prospective and secondary data analytic approaches could support the hypothesis that the new technology is expected to reduce costs. However, SHI routine data as well as non-randomized prospective research hold limitations with regard to causal inference. Therefore, in order to causally confirm resource use hypotheses based on exploratory research randomized controlled study designs are of importanceCitation19.
One influential example for a randomized clinical trial meeting randomization requirements in analysing medical devices provides the prospective BASKET trial (Basel Stent Kosten-Effektivitäts Trial)Citation28. This trial was introduced after the GERSHWIN trial in a setting already prepared for randomization obtaining similar results. With regard to fluid monitoring in heart failure an ongoing randomized study might serve as a further example: With the hypothesis that remote fluid status monitoring and alert function contribute to improved clinical outcomes and reduced resource use a randomized clinical trial called the OptiLink HF Study (Optimization of Heart Failure Management Using Medtronic OptiVol Fluid Status Monitoring and Medtronic Care Link Network) is currently recruiting subjects at risk for pulmonary congestion secondary to heart failureCitation29. The specific research question of this study is to demonstrate that the use of event-triggered heart failure disease-management through a fluid status monitoring device with automatically generated wireless alerts of the clinician can prolong the time to hospitalization, reduce the number of hospitalizations, deaths and all other interventions for worsening of heart failure in a subject population with heart failure and ICD treatment as compared to standard clinical assessment alone (control arm). As the study is planned to be completed in 2013 no results are available so farCitation29. A major challenge is the multi-centre recruitment of a sufficient patient number in this controlled service setting.
Another challenge is the replication of positive effects in different healthcare settings: Despite positive results with regard to telemonitoring in the US the TIM-HF trial (Telemedical Interventional Monitoring in Heart Failure) could not reach significance in its primary end-point of reducing resource consumption with telemonitoring in GermanyCitation13,Citation30.
Running pragmatic trials allowing for clear causal inference is very elaborate, cost-intensive (the TIM-HF trial required an investment of ∼5 million Euro) and feasibility in a routine real life setting may be questionableCitation31. Hence, only in rare cases, institutions or manufacturers are willing to implement such sophisticated randomized study approaches in settings of daily practice. Although analyses based on secondary end-points are scientifically less rigid, they are very often the only alternative to answer questions on clinical and economic implications of new technologies.
The pilot study reported here also holds a number of limitations. First of all the reported pilot study indicates that analysing maintenance and resource use of patients receiving new products not frequently used in clinics is difficult, as small groups do not have the confirming value they should have. In our example the ‘CRT plus alert’ group only included 22 patients, due to the restricted nature of the underlying usage of the new technology. Outliers in such small groups have a strong impact and results are difficult to interpret. The new introduction of a technology (here ‘CRT plus alert’) requires in addition reliable approaches to identify patients of interest, as OPS coding might not have been used by all providers right away. Secondly, the reported pilot study aimed to analyse treatment costs caused by heart failure patients within a maximum of 2 years after implementation of a cardioverter/defibrillator. As routine data of health insurances are collected for determination of resource use it is a good alternative if primary data is not available. However, it has to be taken into account that only costs from the perspective of the payer are covered. All direct costs borne by the patients and other insurances as well as indirect costs are not included. Furthermore, accountability of resource use to specific services or diseases is difficult, as recently concluded by Bowles et al.Citation32. Besides, a selection of patients due to choice of the insurance company has to be considered. Thirdly, the diagnoses in the ‘No Implantation’ group have to be interpreted carefully. Hoffmann et al.Citation33 cited the positive predictive value of diagnosis, i.e., proportion of patients really suffering from the disease diagnosed, in the General Practice Research Database (GPRD), a physician-based database, varying between 99% and only 27%.
The utilization of secondary data in health sciences increased considerably, and recommendations for analysis were publishedCitation20. One important point is related to internal validity: BusseCitation18 emphasized that for matching relevant parameters it is important to adjust for confounders, mainly demography, co-morbidity, and severity of disease. In this study this was partly taken into account by considering difference to expected costs caused by the control group adjusted to age group, sex, and time frame. However, information about the NYHA functional states in different study groups as well as comorbidity ideally should be taken into account, although not being available in SHI data routinely.
Analysing impact of technologies and related management in a longitudinal time frame following the index hospitalization, as performed in the reported pilot study, is a reasonable method to compare costs before and after implementation of a programme or a new product. Quality of medical care may be judged regarding hospital costs over time, i.e., reduced hospital costs may be an indication for improved medical care. However, beyond using secondary data or non-randomized prospective data, the ultimate approach to confirm the contribution of new technologies is, if being feasible to be implemented, a randomized study approach.
Conclusion
In this paper we discuss the importance of and differences in methods for health services research in patients with heart failure subject to remote monitoring. After introducing a retrospective study in heart failure patients based on secondary data, we discuss alternative designs and provide an approximation for hypothesis testing based on SHI data as well as for prospective health service research.
In conclusion this report emphasizes the diversity of approaches in health services research and the variety of methods. Depending on the research question secondary data analysis can provide valuable information for assessing impact of new technologies in treating heart failure patients bearing in mind its advantages and limitations.
Transparency
Declaration of funding
This publication was supported by an unconditional grant from Medtronic GmbH.
Declaration of financial/other relationships
The authors have disclosed that they received a grant from Medtronic to conduct this study. They have no other relevant relationships to disclose.
Acknowledgements
The exploratory secondary research study was commissioned by Medtronic Deutschland GmbH and executed by the Institut für Sozialmedizin, Epidemiologie und Gesundheitssystemforschung e.V. (ISEG). Publication rights are held by Medtronic Deutschland GmbH.
References
- Robert Koch-Institut and Statistisches Bundesamt. Gesundheitsberichterstattung des Bundes – Diagnosedaten der Krankenhäuser. http://www.gbe-bund.de/oowa921-install/servlet/oowa/aw92/dboowasys921.xwdevkit/xwd_init?gbe.isgbetol/xs_start_neu/&p_aid=3&p_aid=37122806&nummer=564&p_sprache=D&p_indsp=-&p_aid=20349829. Accessed April 1, 2011
- Rokita AG, Sag CM, Maier LS. [Heart failure: excitation-contraction coupling and novel therapeutic options.]. Herz 2011;36(2):94–101
- Dietz R, Rauch B. Chronische Herzinsuffizienz, eine verkannte Gefahr? J Public Health: Zeitschrift für Gesundheitswissenschaften 2004;12(1 Suppl):S25
- Hoppe UC, Böhm M, Dietz R, et al. Leitlinien zur Therapie der chronischen Herzinsuffizienz. Zeitschrift für Kardiologie 2005;94:488-509
- Bundesärztekammer (BÄK), Kassenärztliche Bundesvereinigung (KBV), Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF). Nationale Versorgungsleitlinie Chronische Herzinsuffizienz – Langfassung Version 1.3 November 2010. http://www.versorgungsleitlinien.de/themen/herzinsuffizienz. Accessed April 19, 2011
- Robert Koch-Institut and Statistisches Bundesamt. Gesundheitsberichterstattung des Bundes – Sterbefälle für die 10 häufigsten Todesursachen. http://www.gbe-bund.de/oowa921-install/servlet/oowa/aw92/dboowasys921.xwdevkit/xwd_init?gbe.isgbetol/xs_start_neu/&p_aid=i&p_aid=79445342&nummer=517&p_sprache=D&p_indsp=-&p_aid=73584246. Accessed April 1, 2011
- Neumann T, Biermann J, Neumann A, et al. Herzinsuffizienz: häufigster grund für krankenhausaufenthalte - medizinische und ökonomische aspekte. Deutsches Ärzteblatt 2009;106:269-75
- Robert Koch-Institut and Statistisches Bundesamt. Gesundheitsberichterstattung des Bundes – Krankheitskosten in Mio. € für Deutschland. http://www.gbe-bund.de/oowa921-install/servlet/oowa/aw92/dboowasys921.xwdevkit/xwd_init?gbe.isgbetol/xs_start_neu/&p_aid=3&p_aid=5064231&nummer=553&p_sprache=D&p_indsp=-&p_aid=48037634. Accessed April 1, 2011
- Biermann J, Neumann T, Angermann C, et al. Resource use and costs in heart failure. Presentation DGGÖ – annual conference 2011 Bayreuth 22-3-2011
- Inglis SC, Clark RA, McAlister FA, et al. Which components of heart failure programmes are effective? A systematic review and meta-analysis of the outcomes of structured telephone support or telemonitoring as the primary component of chronic heart failure management in 8323 patients: Abridged Cochrane Review. Eur J Heart Fail 2011;13:1028-40
- Klersy C, De Silvestri A, Gabutti G, et al. A meta-analysis of remote monitoring of heart failure patients. J Am Coll Cardiol 2009;54:1683-94
- Chaudhry SI, Mattera JA, Curtis JP, et al. Telemonitoring in patients with heart failure. N Engl J Med 2010;363:2301-9
- Koehler F, Winkler S, Schieber M, et al. Impact of remote telemedical management on mortality and hospitalizations in ambulatory patients with chronic heart failure: the telemedical interventional monitoring in heart failure study. Circulation 2011;123:1873-80
- Mortara A, Pinna GD, Johnson P, et al. Home telemonitoring in heart failure patients: the HHH study (Home or Hospital in Heart Failure). Eur J Heart Fail 2009;11:312-8
- Dar O, Riley J, Chapman C, et al. A randomized trial of home telemonitoring in a typical elderly heart failure population in North West London: results of the Home-HF study. Eur J Heart Fail 2009;11:319-25
- Bundesärztekammer (BÄK). Definition der Versorgungsforschung. 2006. http://www.bundesaerztekammer.de. Accessed April 1,2011
- Zentrum für Versorgungsforschung Köln. Was ist Versorgungsforschung. 2008. http://www.zvfk.de/content/e2996/index_ger.html. Accessed May 1, 2011
- Busse R. Methoden der Versorgungsforschung. In: Hey M, Maschewsky-Schneider U, editors. Kursbuch Versorgungsforschung. Berlin: Medizinisch Wissenschaftliche Verlagsgesellschaft, 2006. p 244
- Glaeske G, Augustin M, Abholz H, et al. [Epidemiological methods for health services research]. Gesundheitswesen 2009;71:685–93
- Arbeitsgruppe Erhebung und Nutzung von Sekundärdaten and Arbeitsgruppe Epidemiologische Methoden. GPS – Gute Praxis Sekundärdatenanalyse: Revision nach grundlegender Überarbeitung. Deutsche Gesellschaft für Sozialmedizin und Prävention, Deutsche Gesellschaft für Epidemiologie, Deutsche Gesellschaft für Medizinische Informatik, Biometrie und Epidemiologie, and Deutsche Gesellschaft für Sozialmedizin und Prävention. 2008. Version 2 http://www.gesundheitsforschung-bmbf.de/_media/GPS.pdf. Accessed April 18, 2011
- Berger ML, Mamdani M, Atkins D, et al. Good research practices for comparative effectiveness research: defining, reporting and interpreting nonrandomized studies of treatment effects using secondary data sources: the ISPOR Good Research Practices for Retrospective Database Analysis Task Force Report–Part I. Value Health 2009;12:1044-52
- Schubert I, Köster I, Küpper-Nybelen J, et al. Versorgungsforschung mit GKV-Routinedaten. Bundesgesundheitsblatt-Gesundheitsforschung-Gesundheitsschutz 2008;10:1095-105
- Hoffmann W, Bobrowski C, Fendrich K. Sekundärdatenanalyse in der Versorgungsepidemiologie. Bundesgesundheitsblatt-Gesundheitsforschung-Gesundheitsschutz 2008;10:1193-201
- Hogan JW, Lancaster T. Instrumental variables and inverse probability weighting for causal inference from longitudinal observational studies. Stat Methods Med Res 2004;13:17-48
- Deutsches Netzwerk Evidenzbasierte Medizin e.V. EbM - Glossar. 2008. http://www.ebm-netzwerk.de/grundlagen/glossar#matched. Accessed May 1, 2011
- Martin DC, Diehr P, Perrin EB, et al. The effect of matching on the power of randomized community intervention studies. Stat.Med. 1993;12(3-4):329-38
- Bruggenjurgen B, McBride D, Bode C, et al. Sirolimus-eluting versus bare-metal stents for the reduction of coronary restenosis: 18-month angiographic results from the GERSHWIN Study. Herz 2007;32:650-5
- Kaiser C, Brunner-La Rocca HP, Buser PT, et al. Incremental cost-effectiveness of drug-eluting stents compared with a third-generation bare-metal stent in a real-world setting: randomised Basel Stent Kosten Effektivitats Trial (BASKET). Lancet 2005;366(9489):921-9
- OptiLink HF Study. Optimization of heart failure management using Medtronic OptiVol Fluid Status Monitoring and Medtronic CareLink Network. 2011. http://clinicaltrials.gov/ct2/show/NCT00769457. Accessed May 1, 2011
- Koehler F, Winkler S, Schieber M, et al. Telemedical Interventional Monitoring in Heart Failure (TIM-HF), a randomized, controlled intervention trial investigating the impact of telemedicine on mortality in ambulatory patients with heart failure: study design. Eur J Heart Fail 2010;12:1354-62
- Koehler, F. Das Forschungs- und Entwicklungsprojekt "Partnership for Heart". 2008. Presentation http://www.dgtelemed.de/downloads/praxisseminar2008/Vortrag-Koehler-240408.pdf. Accessed August 16, 2011
- Bowles D, Damm O, Greiner W. Gesundheitsbezogene Versorgungsforschung mit GKV-Routinedaten – Grenzen am Beispiel der Prophylaxe venöser Thromboembolien in der Hüft- und Kniegelenkendoprothetik. Gesundheitsökonomie und Qualitätsmanagement 2011;16:96-107
- Hoffmann F, Andersohn F, Giersiepen K, et al. [Validation of secondary data. Strengths and limitations]. Bundesgesundheitsblatt-Gesundheitsforschung-Gesundheitsschutz 2008;51:1118–26