Abstract
Objectives:
This study aimed to examine the real-world healthcare resource utilization (HCRU) and direct costs among chronic bronchitis (CB) patients treated with chronic obstructive pulmonary disease (COPD) maintenance medications.
Methods:
This retrospective analysis utilized administrative claims data from 14 US commercial managed care plans. Eligible patients were ≥40 years old, had ≥2 years of continuous enrollment, ≥1 CB (ICD-9-CM code 491.xx) hospitalization or emergency department (ED) visit or ≥2 office visits between 1/1/2004 and 5/31/2011, and had ≥2 pharmacy fills for COPD medications during follow-up (first fill served as the index date). All-cause and COPD-related HCRU and costs were assessed during follow-up. Multivariate models were utilized to identify predictors of total costs.
Results:
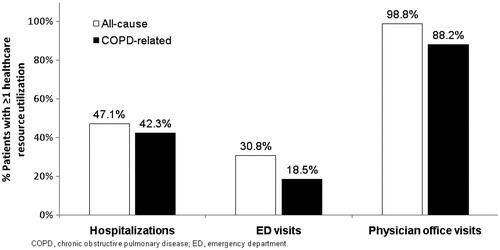
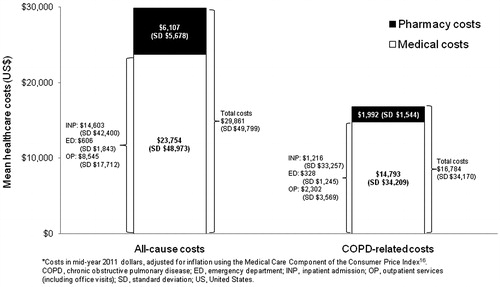
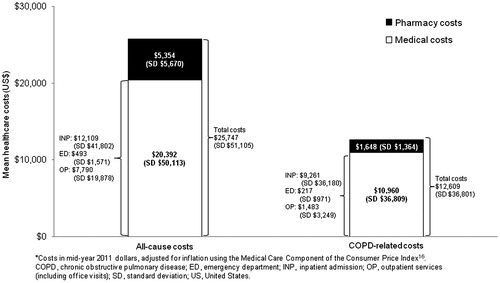
Treated CB patients (n = 17,382; 50.6% female; mean age 66.7 (SD = 11.4) years) had a mean of 7.6 (SD = 6.3) COPD maintenance medication fills during follow-up. Overall, 32.6% of patients had ≥1 COPD-related inpatient hospitalizations, 12.9% had ≥1 ED visit, and 81.8% had ≥1 office visit. Mean all-cause and COPD-related total costs were $25,747 (SD = $51,105) and $12,609 (SD = $36,801), respectively, during follow-up. Among the sub-group with ≥1 exacerbation during baseline year, 42.3% had ≥1 COPD-related inpatient hospitalization, 18.5% had ≥1 ED visit, and 88.2% had ≥1 office visit. Mean follow-up all-cause and COPD-related total costs were $29,861 (SD = $49,799) and $16,784 (SD = $34,170), respectively. The number of baseline exacerbations was a significant predictor of all-cause and COPD-related total costs during follow-up.
Limitations:
This study lacked standard measures of CB severity; however, severity proxies were utilized.
Conclusion:
HCRU and costs among CB patients were substantial during follow-up, despite treatment with COPD maintenance medications. Additional interventions aiming to prevent or reduce HCRU and costs among CB patients warrant exploration.
Introduction
Chronic obstructive pulmonary disease (COPD) is a progressive disease characterized by persistent airflow limitation, chronic and progressive dyspnea, cough, and sputum productionCitation1. It is one of the leading causes of morbidity and mortality worldwide that results in a substantial economic burden on individuals and societyCitation2. In the US, COPD affects ∼24 million adults—half of them (12 million) are undiagnosedCitation3. COPD is currently the third leading cause of death in the US, accounting for ∼138,000 deaths in 2010Citation4. COPD is a broad term that includes two conditions: chronic bronchitis (CB) and emphysema; and many patients with COPD suffer from both conditionsCitation5. COPD also commonly occurs with other chronic co-morbid conditionsCitation6. The mean cost among COPD patients in the US has risen sharply over the last 20 yearsCitation7, with annual cost estimated at $49.9 billion in 2010, of which $29.5 billion are attributable to direct healthcare costsCitation5.
While there is currently no cure for COPD, maintenance medications are available. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines recommend that an effective disease management plan should include assessment and monitoring of the disease, reduction in risk factors, management of stable COPD, and management of exacerbationsCitation1—COPD exacerbation is defined as a change in the patient’s COPD-related baseline dyspnea, cough, and/or sputum that is beyond normal day-to-day variationsCitation8,Citation9. Depending on patient risk and disease activity, the GOLD guidelines recommend maintenance pharmacotherapy whereby long-acting β2-agonists (LABA) and long-acting muscarinic antagonists (LAMA) are preferred over short-acting β2-agonists (SABA) and short-acting muscarinic antagonists (SAMA). The GOLD guidelines further recommend that combined use of LABA + LAMA may be considered if symptoms are not improved with single agents. Inhaled corticosteroids (ICS), phosphodiesterase-4 (PDE4) inhibitors, or theophylline may also be added for severely ill patients.
While limited COPD-related economic data are available in the literatureCitation2,Citation10, there appears to be even fewer data on healthcare utilization and costs among CB patientsCitation11. Additionally, available CB economic studies fail to incorporate COPD-related healthcare resource utilization and costs resulting from the common overlap between CB and emphysema. Furthermore, few studies have examined the predictors of healthcare costs among treated CB patients using real-world data. In particular, few studies have explored the role of COPD exacerbations in predicting overall costs, despite the fact that exacerbations have been found to be the most frequent cause of hospital admission and death among COPD patientsCitation12.
This study addressed the aforementioned limitations in the literature by incorporating COPD-related healthcare resource utilization and costs among patients with CB and by assessing the association between prior exacerbations and healthcare utilization and costs during follow-up. Specifically, this study aimed to (1) estimate the real-world annual total all-cause and COPD-related costs for actively treated CB patients; and (2) examine the association between the number of exacerbations during a one-year baseline period and total all-cause and COPD-related costs during a one-year follow-up period.
Patients and methods
This retrospective observational study utilized data from the HealthCore Integrated Research Database (HIRDSM), which consists of longitudinal medical, pharmacy, and enrollment claims data from 14 major commercial health plans across the US representing ∼45 million commercially insured lives. All study data and materials were handled in compliance with the Health Insurance Portability and Accountability Act (HIPAA), and a limited dataset was used for this analysis.
Sample selection
Patients were required to meet the following criteria to be included in the study: (1) at least one inpatient hospitalization or emergency department (ED) visit or at least two physician office visits with an International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis code of 491.xx (CB) between January 1, 2004 and May 31, 2011; (2) at least two pharmacy fills for COPD medication(s) (i.e., LAMA, LABA, ICS, fixed dose LABA + ICS inhaler, SABA, or SAMA), with at least one fill being a COPD maintenance medication (i.e., LAMA, LABA, ICS, or fixed dose LABA + ICS inhaler) during the follow-up period; (3) continuous health insurance enrollment during two calendar years (one before and one after the index date). The index date was defined as the first fill of COPD medication within 18 months of the most recent CB diagnosis. This index date definition was chosen to capture the most recent treatment patterns among eligible study patients. The 1-year period prior to the index date was defined as the ‘baseline year’ and was used to measure patient baseline characteristics, whereas the 1-year period after the index date was defined as the ‘follow-up year’ and was used to measure follow-up healthcare resource utilization and costs. Patients were excluded from the study if they met any of the following criteria: (1) were aged less than 40 years on the index date; (2) had at least one medical claim for a potential COPD confounding condition (asthmaCitation13, cystic fibrosis, respiratory tract cancer, tuberculosis, interstitial lung diseases, α1-antitrypsin deficiency, or a malignant neoplasm of the thymus, heart, or mediastinum) during the study period; and (3) were long-term oral corticosteroid (OCS) users (had a day supply of 182 days or longer any time during the study periodCitation13).
Study measures
Baseline characteristics included patient characteristics (age, gender, US residence region), health plan type (i.e., preferred provider organization (PPO), health maintenance organization (HMO), or other health insurance type), and major patient comorbidities. Comorbidity burden was measured using the Deyo-Charlson Comorbidity Index (DCI)Citation14—COPD diagnosis was excluded from the calculation of this score. Proportions of patients with COPD medication class use on the index date were described. Fill counts for COPD maintenance medications were assessed. Also, fills for short-acting relief medications (SABA/SAMA) during the follow-up year were used as proxies for CB severity in this study. The number of COPD exacerbations during the baseline year was measured as the total number of events meeting one of the following two criteria: (1) a hospitalization with primary COPD diagnosis (ICD-CM diagnosis codes: 491.xx, 492.xx, or 496.xx), (2) an ED visit with a primary COPD diagnosis, or a fill of an OCS within seven days of the date of an office visit with COPD diagnosis. Further, the following rules were applied to measure discrete COPD exacerbation events: (1) exacerbations were measured for up to 14 days from the date of an exacerbation eventCitation15; (2) a maximum of one exacerbation of the most severe type was recorded during any 14-day window; and (3) a new 14-day window was triggered by an exacerbation of any type occurring after the end date of the previous exacerbation time windowCitation15. More detail about measurement of COPD exacerbations is under review elsewhere. Total baseline all-cause costs were measured by summing health-plan-allowed costs for all medical and pharmacy claims available for all patients during the baseline year. Allowed costs included the allowed charges on each administrative claim, including the amounts paid by the insurer plus the amounts paid by the health plan members (copayment, deductible, and coinsurance amounts). Total baseline COPD-related total medical costs were measured by summing health-plan-allowed costs for all medical claims associated with a COPD diagnosis (ICD-CM diagnosis codes: 491.xx, 492.xx, or 496.xx in any position of the medical claim) and the costs of any COPD-related maintenance medications, if applicable, among all patients during the baseline year.
Outcomes assessment
Healthcare utilization and total costs were the outcomes used in this study. Healthcare utilization included the frequency of inpatient hospitalizations, ED visits, and physician office visits during follow-up year. All-cause healthcare utilization was identified by use of any medical care, regardless of diagnosis, whereas COPD-related healthcare utilization was identified by a medical claim associated with any of the following ICD-CM diagnosis codes: 491.xx, 492.xx, or 496.xx (in any position on the claim). Length of stay (LOS) for both all-cause and COPD-related inpatient hospitalizations was measured among patients with at least one admission during the follow-up year.
Total all-cause costs were measured by summing health-plan-allowed costs for all medical and pharmacy claims available for all patients during the follow-up year. COPD-related total medical costs were measured by summing health-plan-allowed costs for all medical claims associated with a COPD diagnosis and the costs of COPD-related maintenance medications among all patients. Outcomes were assessed among the overall population and the sub-groups of patients with at least one exacerbation during the baseline year.
Statistical analysis
Key baseline patient characteristics were summarized using mean (SD) for continuous outcomes and counts and proportions for categorical variables. The proportions of patients with at least one record of healthcare resource utilization (inpatient hospitalization, ED visit, or physician office visit) during the follow-up year were measured for both all-cause and COPD-related utilization. Mean (SD) of hospital LOS among patients with at least one inpatient hospitalization during the follow-up year was calculated. Total all-cause and COPD-related costs were described using means (SDs). Costs were adjusted to mid-year 2011 figures using the medical care component of the Consumer Price IndexCitation16. The proportion of patients with at least one exacerbation during the baseline year was calculated. Separate generalized linear models (GLM) with a log-link function (gamma distribution) were fitted to model total all-cause and COPD-related costs during follow-up year as a function of baseline exacerbations, controlling for baseline demographic, health plan, and clinical characteristics. All statistical analyses were conducted in SAS® version 9.2 (SAS Institute; Cary, NC).
Results
Study population
An initial sample of 48,397 patients met study inclusion criteria. Of those, the following numbers of patients were excluded: 2770 (5.7%) aged less than 40 years on the index date; 21,154 (43.7%) had at least one exclusionary condition (20081 [80.8%] asthma; 1764 [3.6%] were long-term OCS users; 5327 [11.0%] had no fills for COPD maintenance medications during follow-up year). A total of 17,382 patients were used in analyses.
Baseline characteristics
Slightly more than half (53.6%) of the overall study patients were 65 years of age or older on the index date (mean age was 66.7 [SD 11.4]) years) (). South (33.2%) and Mideast (30.6%) regions of the US had the highest proportion of study patients. Most patients (63.5%) had PPO insurance, 22.2% had HMO insurance, and 14.4% had other insurance types (). The mean DCI score during the baseline year was 1.3 (SD = 1.7). Of the select co-morbid conditions included in this study, the following were the most common: hypertension (56.0%), cardiovascular disease (39.9%), acute bronchitis and bronchiolitis (22.1%), diabetes mellitus (21.2%), and acute sinusitis (9.6%). A quarter (n = 4349) of the study patients had at least one exacerbation during the baseline year (exacerbations occurring on the index date were not counted). Total pre-index all-cause costs were $19,872 (SD = $43,165) and total pre-index COPD-related costs were $7840 (SD = $29,058).
Table 1. Patient characteristics during baseline year.
COPD maintenance medications
On the index date, 22.2% of the study patients were prescribed LAMA, 20.5% were prescribed fixed dose ICS + LABA inhalers, 6.0% were prescribed ICS, 2.4% were prescribed LABA, and 5.8% were prescribed combinations of these four maintenance medication classes. While the remaining patients were prescribed SABA (21.9%), SAMA (10.7%), or both (1.4%) on the index date, these patients had at least one COPD maintenance medication fill during the follow-up year. Overall, the mean number of COPD maintenance medication fills was 7.6 (SD = 6.3) during the follow-up year, consisting of the following medications: fixed dose ICS + LABA inhalers (mean = 3.4, SD = 3.8), LAMA (mean = 3.2, SD = 4.2), ICS (mean = 0.7, SD = 2.1), and LABA (mean = 0.4, SD = 1.8). The mean fills for SABA and SAMA were (2.7 [SD = 4.0]) and (1.7 [SD = 3.7]), respectively.
Healthcare resource utilization and cost
A considerable proportion of the overall study patients had at least one all-cause inpatient hospitalization (39.0%), with a mean LOS of 11.7 (SD = 17.6) days. In addition, 26.6% of patients had at least one ED visit, and 98.4% had at least one physician office visit during the follow-up year (), resulting in a total mean follow-up cost of $25,747 (SD = $51,105) per patient. Overall, 32.6% of patients had at least one COPD-related inpatient hospitalization with a mean LOS of 11.2 (SD = 16.9) days, 12.9% had at least one ED visit, and 81.8% had at least one physician office visit. These utilizations resulted in a mean COPD-related total cost of $12,609 (SD = $36,801) during the follow-up year. depicts the mean all-cause and COPD-related total costs and costs per inpatient hospitalization, ED visit, and outpatient services (including physician office visits) among all study patients. Overall, COPD-related costs accounted for 53.7%, 30.8%, and 49.0% of medical, pharmacy, and total all-cause costs, respectively, among all patients.
Figure 1. Proportion of patients with all-cause and COPD-related healthcare utilization during follow-up year (n = 17,382).
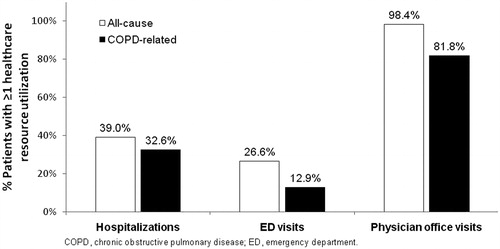
Figure 2. Mean (SD) of all-cause and COPD-related costs* among all patients during follow-up year (n = 17,382).
Among the sub-group of patients with at least one exacerbation during the baseline year, approximately half (47.1%) had at least one all-cause inpatient hospitalization with a mean LOS of 13.2 (SD = 18.7) days. In addition, 30.8% of this sub-group had at least one ED visit and 98.8% had at least one physician office visit during the follow-up year (). These utilizations resulted in a total mean follow-up cost of $29,861 (SD = $49,799) per patient. A large proportion (42.3%) of these patients had at least one COPD-related inpatient hospitalization, with a mean LOS of 12.6 (SD = 17.4) days; 18.5% had at least one ED visit, and 88.2% had at least one physician office visit. These utilizations resulted in a mean COPD-related total cost of $16,784 (SD = $34,170) per patient during the follow-up year. depicts the mean total all-cause and COPD-related costs and costs per inpatient hospitalization, ED visit, and outpatient services (including office visits) among patients with at least one exacerbation during the baseline year. Overall, COPD-related costs accounted for 62.3%, 32.6%, and 56.2% of medical, pharmacy, and total all-cause costs, respectively, among this patient sub-group.
Multivariate analysis results
GLM multivariate regression results of follow-up all-cause costs () showed that, controlling for other covariates examined in this study, the number of exacerbations in the baseline year was significantly associated (β = 0.0924, p < 0.0001) with greater overall costs. Among the control variables, DCI score (β = 0.1982, p < 0.0001), being from west (β = −0.2126, p < 0.0001) and northeast regions (β = −0.1382, p < 0.0001), having other health plans (β = 0.1558, p < 0.0001), and female gender (β = −0.0909, p < 0.0001) had the highest associations with total all-cause costs.
Table 2. GLM regression model of total all-cause healthcare costsa during the follow-up year (n = 17,382).b
GLM multivariate regression results of COPD-related costs during the follow-up year () showed that the number of exacerbations in the baseline year (β = 0.1862, p < 0.0001) was a strong predictor of greater COPD-related costs, controlling for other covariates. Among COPD maintenance medication classes, only the number of fills for fixed dose ICS + LABA (β = −0.0130, p < 0.0001) and ICS (β = −0.0241, p < 0.0001) were associated with lower total COPD-related costs. As expected, the number of fills for SABA (β = 0.0231, p < 0.0001) and SAMA (β = 0.0253, p < 0.0001) were associated with higher total COPD-related costs. Among other covariates, DCI score (β = 0.1370, p < 0.0001), northeast region (β = −0.3108, p < 0.0001), west region (β = −0.1879, p < 0.0001), other health plan type (β = 0.1348, p < 0.0001), and female gender (β = −0.1280, p < 0.0001) were associated with total COPD-related costs.
Table 3. GLM regression model of total COPD-related healthcare costsa during the follow-up year (n = 17,382).b
Discussion
This study of relatively well-treated CB patients (7.6 [SD = 6.3] COPD maintenance medication fills during follow-up) found that COPD-related healthcare utilization was substantial—32.6%, 12.9%, and 81.8% had at least one COPD-related inpatient hospitalization, ED visit, or physician office visit, respectively, during the follow-up year. These COPD-related utilizations accounted for 83.6%, 48.5%, and 83.1% of all-cause inpatient hospitalizations, ED visits, and physician office visits, respectively. This finding underscores the predominance of COPD care in healthcare utilization during the follow-up period.
Among the overall CB patients, the mean total all-cause costs estimated in this study ($25,747) are higher than estimates previously reported in the literature ($19,882)Citation11. The previous study was limited to newly diagnosed CB patients, whereas the present study included both incident and prevalent CB patients. Since a previous study suggested that increased progression of COPD disease is also associated with higher healthcare utilization and costsCitation17, the higher costs found in this study are likely due to the fact that the patients within our cohort had a comparatively longer CB duration at the time of healthcare utilization and cost measurement. As expected, DCI score was associated with both all-cause and COPD-related costs. The finding that the number of exacerbations during the baseline year is a significant predictor of both all-cause and COPD-related costs is also supported by previous claim-based studies showing that exacerbations contribute to considerable healthcare costsCitation18,Citation19.
The finding that COPD patients with at least one exacerbation during the baseline year had higher medical, pharmacy, and total direct healthcare costs compared to the overall CB patients (by 25.9%, 17.3%, and 24.9%, respectively) highlights the fact that this sub-group of patients has unmet needs and should be targeted for interventions intended to improve outcomes and decrease healthcare costs.
This study has several strengths. First, it focused on managed care CB patients treated with COPD maintenance medications, including adults aged 40 years and over and excluded major respiratory-related CB confounders, such as asthma. Given that CB is a long-term, progressive condition, our choice to focus on patients who were exposed to COPD maintenance medications makes it more likely that we included more severe CB patients. The results of this study will be most generalizable to CB patient populations with similar characteristics to this cohort. Second, this study provided real-world estimates of both all-cause and COPD-related healthcare utilization and costs among treated CB patients, which are currently lacking in the literature. This study included the number of exacerbations during baseline as a predictor of total costs in addition to conventional demographic and other clinical measures of co-morbidity burden.
Nonetheless, the following limitations to this study are noted. First, the study was limited, by design, to treated CB patients. Because untreated patients were not extracted from the database, it is not possible to compare the characteristics of these excluded patients to the study patients, and therefore the findings of this study may not be generalizable to untreated patients. Second, this study did not include clinical variables, such as smoking history and forced expiratory volume in 1 s (FEV1), which were found significant of CB costsCitation20, etc., which are likely to be relevant in predicting costs. Thirdly, this study lacked CB severity measures because no such standard measures exist in the claims-based literature; nonetheless, severity proxiesCitation6 such as number of exacerbations in the previous year and number of fills for SABA and SAMA were used in the regression models. Fourthly, this study excluded patients with concomitant asthma, which may limit the generalizability of these results to patients who have both diagnoses. Finally, estimates in this study are limited to direct healthcare costs and, therefore, do not reflect the full societal burden of CB on patients and their informal caregivers.
Despite the limitations, the findings of this study are notable. They suggest that, despite treatment with COPD maintenance medications, this real-world CB population had substantial COPD-related costs that accounted for the majority of all-cause costs. The number of baseline exacerbations was a significant predictor of both all-cause and COPD-related costs. These findings underscore the potential importance of more effective treatment options for this CB patient population. For example, more effective disease management programs have been recommendedCitation21. Major features of effective disease management programs include adherence to treatment guidelines, use of a nurse with special training in the disease condition (CB in this case), co-ordination of care between providers, and patient-centered care programs. Additionally, one strategy to lower costs among the high-risk CB patients is to prevent or reduce the rate of exacerbations. Therefore, the use of more aggressive add-on treatments in severe and very severe patients who experience COPD exacerbations, as suggested by the GOLD guidelinesCitation1, can potentially improve the management of the CB disease and, therefore, reduce related costs. Finally, more efforts directed to health education and prevention of major CB risk factors, such as smoking, along with early detection and management of the disease, can prevent or slow the progression of the disease.
Future studies are warranted to estimate longitudinal healthcare utilization and costs among treated CB patients, since this study was limited to 1 year of follow-up data. Furthermore, future studies that incorporate indirect costs from the client and informal caregiver perspective would contribute to the growing body of literature on the economic and humanistic burden of COPD. Particular attention is also required to differentiate the impact of exacerbations on total COPD-related costs. Due to the high prevalence of chronic diseases in this patient population, more research is also needed to differentiate the impact of these major co-morbid conditions on the outcomes of this study.
Conclusion
The results of this study provide new insight regarding the real-world healthcare utilization and costs among the CB population, which are not typically assessed apart from the umbrella COPD term in the literature. This study found that, despite treatment with various COPD maintenance medications during the follow-up year, patients had considerable healthcare utilization and costs; most of which were COPD-related. The study also identified the number of exacerbations during the baseline year as a significant predictor of both all-cause and COPD-related costs and found that healthcare costs were higher among patients with baseline history of exacerbation compared to the overall treated CB patients. Recommendations for managing COPD-related healthcare costs and needed future research are provided.
Transparency
Declaration of funding
This research project was funded by Forest Research Institute (Jersey City, NJ), a wholly owned subsidiary of Forest Laboratories, Inc. (New York, NY).
Declaration of financial/other relationships
SXS is an employee of Forest Research Institute. The other authors (AA, HT, CTS) report no relationship or financial interest with any entity that would pose a conflict of interest with the subject matter of this article. The funding sponsor had no role in data collection, interpretation, or analysis, nor did the sponsor influence the manuscript or the decision to publish. AA and HT are employees of HealthCore, Inc. (Wilmington, DE), an independent outcomes research organization. CTS is an employee of Pharmerit North America (Bethesda, MD), an independent outcomes research organization. Both HealthCore, Inc. and Pharmerit North America received consulting fees from Forest Research Institute for research related to this manuscript. JME peer reviewers on this manuscript have no relevant relationships to disclose.
Acknowledgments
The authors thank Rebecca Cobb for programming efforts and Cheryl Jones for editorial assistance in preparing this manuscript. Assistance with preparation of the manuscript for submission by Prescott Medical Communications Group (Chicago, IL) was made possible by funding from Forest Research Institute. Data presented in this manuscript were previously presented in part as a poster at the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) 17th Annual International Meeting; June 2–6, 2012; Washington, DC.
References
- Vestbo J, Hurd SS, Agusti AG, et al. Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease, GOLD Executive Summary. Am J Respir Crit Care Med 2012Aug 9. [Epub ahead of print]
- Sullivan SD, Ramsey SD, Lee TA. The economic burden of COPD. Chest 2000;117:5S-9S
- Minino SL, Xu JQ, Kochanek KD. Deaths: preliminary data for 2008. National Vital Statistics Reports 2010;59:1-52
- Murphy SL, Xu JQ, Kochanek KD. Deaths: preliminary data for 2010. National Vital Statistics Reports 2012;60:1-69
- National Heart, Lung, and Blood Institute (NHLBI). Morbidity and mortality: 2009 chart book on cardiovascular, lung, and blood diseases. Bethesda, MD: National Heart, Lung, and Blood Institute, 2009. http://www.nhlbi.nih.gov/resources/docs/2009_ChartBook.pdf Accessed October 23, 2012
- Dalal AA, Shah M, Lunacsek O, et al. Clinical and economic burden of patients diagnosed with COPD with comorbid cardiovascular disease. Respir Med 2011;105:1516-22
- Blanchette CM, Dalal AA, Mapel D. Changes in COPD demographics and costs over 20 years. J Med Econ 2012;15:1176-82 [Epub 1 August 2012]
- Rodriguez-Roisin R. Toward a consensus definition for COPD exacerbations. Chest 2000;117:398S-401S
- Burge S, Wedzicha JA. COPD exacerbations: definitions and classifications. Eur Respir J Suppl 2003;41:46s-53s
- Gagnon YM, Levy AR, Spencer MD, et al. Economic evaluation of treating chronic obstructive pulmonary disease with inhaled corticosteroids and long-acting β2-agonists in a health maintenance organization. Respir Med 2005;99:1534-45
- Blanchette CM, Roberts MH, Petersen H, et al. Economic burden of chronic bronchitis in the United States: a retrospective case-control study. Int J Chron Obstruct Pulmon Dis 2011;6:73-81
- Donaldson GC, Wedzicha JA. COPD exacerbations. 1: epidemiology. Thorax 2006;61:164-8
- Blais L, Forget A, Ramachandran S. Relative effectiveness of budesonide/formoterol and fluticasone propionate/salmeterol in a 1-year, population-based, matched cohort study of patients with chronic obstructive pulmonary disease (COPD): effect on COPD-related exacerbations, emergency department visits and hospitalizations, medication utilization, and treatment adherence. Clin Ther 2010;32:1320-8
- Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 1992;45:613-9
- Mapel DW, Dutro MP, Marton JP, et al. Identifying and characterizing COPD patients in US managed care. A retrospective, cross-sectional analysis of administrative claims data. BMC Health Serv Res 2011;11:43
- Bureau of Labor Statistics, US Department of Labor. Measuring price change for medical care in the CPI. Last updated April 12, 2010. http://www.bls.gov/cpi/cpifact4.htm. Accessed October 1, 2011
- Akazawa M, Halpern R, Riedel AA, et al. Economic burden prior to COPD diagnosis: a matched case-control study in the United States. Respir Med 2008;102:1744-52
- Mapel DW, Schum M, Lydick E, et al. A new method for examining the cost savings of reducing COPD exacerbations. Pharmacoeconomics 2010;28:733-49
- Yu AP, Yang H, Wu EQ, et al. Incremental third-party costs associated with COPD exacerbations: a retrospective claims analysis. J Med Econ 2011;14:315-23
- Mapel DW, McMillan GP, Frost FJ, et al. Predicting the costs of managing patients with chronic obstructive pulmonary disease. Respir Med 2005;99:1325-33
- Seemungal TA, Hurst JR, Wedzicha JA. Exacerbation rate, health status and mortality in COPD–a review of potential interventions. Int J Chron Obstruct Pulmon Dis 2009;4:203-23