Abstract
Objective:
Human papillomavirus (HPV) has an important role in the aetiology of a range of diseases, including cervical, other anogenital, and head and neck cancers, genital warts and recurrent respiratory papillomatosis. This literature review was conducted to identify the available cost data for non-cervical HPV-related cancers (anal, penile, vulvar, vaginal, head and neck) in Europe and to inform discussion of methodological challenges for future economic research.
Methods:
The literature search was conducted using Medline and key words to identify papers published in English or French between 1 January 2000 and 31 December 2011. Abstracts of major conferences were searched to identify relevant information. Structured methods were used to select references that focused on overall disease management for inclusion in the review.
Results:
A total of 21 references from seven countries (Denmark, France, Germany, Greece, The Netherlands, Portugal, and the UK) were selected, including 11 references relating to head and neck cancers, five to anogenital cancers, and five to more than one HPV-related disease. Non-cervical cancers accounted for a substantial proportion of the economic burden of HPV-related cancers, and this burden was mainly driven by men (∼70%). A wide range of costs were reported for each disease, particularly head and neck cancers, predominantly due to disease complexity and variation in study design.
Limitations:
The main limitation of this study was in the search strategy, which was constrained by the key words, the database searched, and the restriction on language (English/French).
Conclusions:
Non-cervical cancers attributable to HPV impose a substantial economic burden in Europe, and the burden is greater in men than in women. This review provides useful information for future health-economic studies assessing the impact of HPV vaccination on all HPV-related diseases.
Introduction
Persistent infection with human papillomavirus (HPV) plays an important role in the aetiology of a wide range of diseases, most notably cervical cancer, but also a proportion of other anogenital neoplasias, such as anal, penile, vulvar, and vaginal cancer, as well as some head and neck cancers, genital warts, and recurrent respiratory papillomatosis (RRP)Citation1,Citation2. While persistent HPV infection is implicated in the development of virtually all cervical cancersCitation3, genital wartsCitation4, and cases of RRPCitation5, it is estimated that persistent HPV infection is associated with 80–85% of anal cancers, ∼50% of penile cancers, 36–40% of vulvar cancers, 70% of vaginal cancers, and 20–60% of head and neck cancers (especially tonsillar cancers)Citation6–8.
Over 130 HPV types have been identifiedCitation9, but only a few are responsible for the majority of the medical, psychological, societal, and economic burden of HPV-related disease. The majority of HPV-related cancers are due to types 16 and 18Citation10–12, while types 6 and 11 cause 90% of genital wartsCitation13, over 95% of RRP casesCitation14, and ∼10% of early cervical lesionsCitation15.
The epidemiological burden of HPV-related pre-malignant cervical lesions and cervical cancer has been widely describedCitation16,Citation17. Similarly, economic studies of HPV-related cancers in Europe have focused primarily on cervical cancer and its precursor lesionsCitation18–20. Non-cervical HPV-related cancers have received less attention, particularly from an economic viewpoint, although their incidence in Europe, notably of anal cancer and oropharyngeal cancers, has been rising in both sexes in recent yearsCitation21–25. The estimated burden of non-cervical HPV-related cancers in Europe is higher in men than in women, and is driven primarily by head and neck cancersCitation26. It has been estimated that 17,403 cancer cases attributable to HPV (15,497 attributable to HPV 16/18) occur each year in men in EuropeCitation26. This compares with an estimated 9308 non-cervical cancer cases attributable to HPV 16/18 each year in women in EuropeCitation26.
The main objectives of this literature review were: (1) to identify the best available cost evidence on non-cervical cancers potentially attributable to HPV in Europe; (2) to estimate the associated societal costs and/or lifetime cost per case; and (3) to highlight methodological challenges to be considered for further research into non-cervical HPV-related cancers cost-of-illness studies.
Literature search methodology
A literature search was conducted using Medline to identify papers published in English or French presenting cost data for non-cervical cancers (anal, vulvar, vaginal, penile, and head and neck cancers) potentially attributable to HPV in Europe. The search was performed between 1 January 2000 and 31 December 2011 using the Medical Subject Headings (MeSH) thesaurus, different combinations of economic terminology and disease-specific key words (see Appendix). The literature search focused on papers that provided or allowed determination of societal costs at the country level and/or per-patient costs presented as the cost of an ‘episode of care’ (defined as the period from diagnosis to resolution of the case). Although this review focused on the burden of disease (i.e., cost-of-illness analyses), references utilizing other analytical methods (cost-effectiveness, cost-utility) were included if they considered relevant cost-of-illness data.
Selection of relevant papers was performed by two reviewers who independently assessed the titles and abstracts. Papers were excluded because of irrelevance or similarity with another article. Final selection of papers was based on reviewer consensus. The reference lists of selected papers were checked to identify additional relevant articles, but none were found.
Data from the selected papers were entered into pre-defined data extraction tables, which captured the country, cancer type, patient population, study objectives, design and timeframe, type of economic evaluation, analytical method, results, and data sources. The papers were evaluated by considering study characteristics, type of economic evaluation, analytical method, and the cost focus (societal/per-patient).
Abstracts of major conferences known to the authors in the fields of oncology, gynaecology, or health economics (2008–2011) were searched to identify information not yet published in peer-reviewed journals.
Results
A total of 21 references from seven European countries (Denmark, France, Germany, Greece, The Netherlands, Portugal, and the UK) were selected for inclusion in the review (, ). These included 13 published papers describing economic studies and three published economic review articles. Just over half (11/21) of the references provided economic data for head and neck cancers, five were specific to anogenital cancers (anal, penile, vulvar, and vaginal), and five covered more than one HPV-related disease. In addition to the 11 selected references specific to head and neck cancers, 13 references focusing on European studies were identified during the literature search but were excludedCitation48–60. The main reasons for exclusion were because they focused on costs associated with specific dimensions of the disease management (e.g., screening and diagnosis, treatment options, complications, or clinical care pathways) rather than on overall costs related to the disease (diagnosis, treatment, and follow-up). Similarly one reference presenting cost data on vulvar and vaginal pre-cancerous lesions was identified but excluded from the review as it did not present any cancer dataCitation61.
Figure 1. Results of the literature search and evaluation of identified studies. Three conference abstracts are now published/accepted for publicationCitation62–64. EU, European Union; H&N, head and neck.
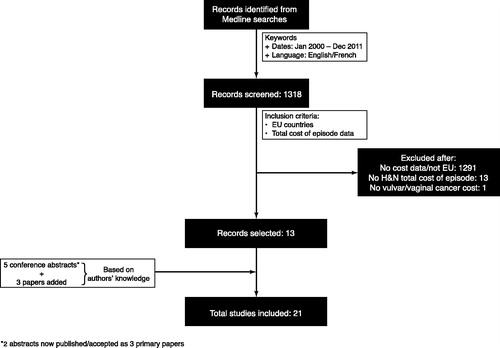
Table 1. Selected references by country and cancer type.
In addition, five conference communications were identified; at the time of the publication of this review article three have been publishedCitation62–64. Three other published papers were added to the review based on the authors’ knowledge. One paper was not retrieved from the search as the journal was not indexed in MedlineCitation31 and the other two papers did not include any disease-specific keywordsCitation44,Citation45.
While some studies included in our review provided costs for the proportion of non-cervical anogenital cancers and head and neck cancers estimated to be associated with HPV, other papers provided costs for the cancers regardless of aetiology. In the latter situation, we did not estimate the proportion of the cases/costs related to HPV. Data were extracted and described exactly as presented in the papers.
Anal cancer
An overview of health economic references for anal cancer is presented in .
Table 2. Overview of health economic references for anal cancer.
Three European publications on anal cancer specifically were selected: two of these papers by Karnon et al.Citation27 and Czoski-Murray et al.Citation28 were from the same UK research group and described cost-utility analyses of screening for anal cancer in high-risk groups, whereas the third paper by Abramowitz et al.Citation29 assessed the economic burden of anal cancer in men and women hospitalized in France in 2006. In addition, anal cancer was one of the diseases covered in two papers, namely the papers of Borget et al.Citation45 and Jit et al.Citation44 describing economic analyses including multiple HPV-related diseases.
Karnon et al.Citation27 developed a cohort-based Markov model using an annual cycle to represent the natural history of anal cancer, alongside the natural history of human immunodeficiency virus (HIV) infection, in a population of men who have sex with men (MSM) in the UK. Czoski-Murray et al.Citation28 developed two decision-analytical models to analyse cost-effectiveness of screening for anal cancer in HIV-positive and HIV-negative MSM and HIV-positive women in the UK. In both studies, costs were estimated from a UK National Health Service perspective. The mean lifetime treatment costs per patient used in the analyses were £8895 and £13,334 for screen-detected and non-screen-detected anal cancer, respectivelyCitation27,Citation28. However, these lifetime costs were based on US clinical care algorithms.
The cost-of-illness study of Abramowitz et al.Citation29 estimated costs from the French healthcare-payer perspective and involved retrospective analysis of data extracted from a French national hospital database (Programme de Médicalisation des Systèmes d’Information [PMSI]). In 2006, 3711 patients with anal cancer were treated in hospitals in France and total annual management costs (hospitalization, outpatient, and daily allowance costs) were €38.2 million. Based on the estimation that 88% of anal cancers are attributable to HPV infection, total management costs for HPV-related anal cancers were €33.7 million. Hospital costs were based on Diagnosis Related Group (DRG) tariffs, outpatient costs on those for colorectal tumours, and indirect costs (daily allowance) on the mean number of workdays lost for any type of cancer. Use of DRG tariffs may under-estimate hospitalization costs because expensive drug and patient rehabilitation expenditure is not included. Furthermore, the costs of managing side-effects of anal cancer treatment (e.g., anal incontinence), which are common and debilitating, were not included. Although the estimation of daily allowance was based on payments to patients from the National Sickness Fund to offset any loss of income, it did not take into account costs that patients may have to cover themselves, such as travel expenses, and indirect costs due to loss of productivity or premature death were not considered. Another limitation of this study is the time horizon. The PMSI database does not allow patients to be followed for more than 1 year, and incident cases cannot be identified. The estimated mean cost per hospitalized patient (€6228 in public sector; €4695 in private sector), therefore, reflects the average management cost for all cases admitted to hospital. This may be lower than the management cost for a new case, as more resources are likely to be used in the first year of treatment than in subsequent years. This study was further discussed in the paper of Borget et al.Citation45.
The paper of Jit et al.Citation44 described a cost-effectiveness analysis of HPV transmission and disease and the effects of vaccinating girls in the UK, and utilized lifetime treatment costs for various HPV-related cancers that were derived from comparisons with cervical cancer and direct medical costs in the US. The lifetime treatment cost per case of anal cancer was estimated at £13,050.
Three conference communications reporting cost-of-illness studies for multiple cancer types provided costs for anal cancer in GermanyCitation46, DenmarkCitation43, and PortugalCitation47. These studies involved retrospective analysis of data extracted from healthcare insurance databases. Hospital costs in all three studies were based on DRG tariffs, with the inherent limitations discussed above. Rémy et al.Citation46 reported total annual societal costs (hospitalization, inpatient rehabilitation [e.g., anal sphincter training after surgery] and sick leave costs) of anal cancer in Germany of €34.1 million, although several cost components were not included (e.g., outpatient management, expensive chemotherapy, premature retirement, long-term care costs). Total annual societal costs for HPV-related anal cancer were €28.7 million in GermanyCitation46. The studies of OlsenCitation43 and Santana et al.Citation47 in Denmark and Portugal, respectively, reported costs from the healthcare-payer perspective (hospitalization and outpatient costs). In Denmark, total annual healthcare costs for anal cancers, regardless of aetiology, were €4.28 million, and for the proportion attributable to HPV 16/18 were €3.36 millionCitation43. In Portugal, total annual healthcare costs for HPV-related anal cancers were €3.91 million, and for the proportion attributable to HPV 6/11/16/18 were €2.59 millionCitation47. Although the data used for the Portuguese study came from official sources, the authors commented on evidence of under-reporting of cases and a high proportion of unspecified cancer codingCitation47.
Penile cancer
Only one reference on penile cancer specifically was identified, which was a poster by Rémy and VainchtockCitation30 that was discussed further in the paper of Borget et al.Citation45. This cost-of-illness study assessed the economic burden of penile cancer in men hospitalized in France in 2006 from the French healthcare-payer perspective and employed the same methodology as the anal cancer study of Abramowitz et al.Citation29 described above. Consequently, the same limitations as those described above for the study of Abramowitz et al.Citation29 may have led to under-estimation of the costs associated with penile cancer. In 2006, 678 men with penile cancer were treated in French hospitals. The annual total costs of management (hospitalization, outpatient, and indirect costs) were €5.65 million. Based on the estimation that 55% of penile cancers are attributable to HPV infection, annual total management costs for HPV-related penile cancers were €3.11 million.
The paper of Jit et al.Citation44 (see above for details and limitations) reported a lifetime treatment cost of £11,550 per case of penile cancer in the UK.
Two further conference communications presenting cost data for multiple cancer types provided costs estimated from the healthcare-payer perspective for penile cancer in DenmarkCitation43 and PortugalCitation47. These two studies and their limitations in terms of use of DRG tariffs and under-reporting of cases have been discussed previously in relation to anal cancer. In Denmark, total annual healthcare costs for penile cancer, regardless of aetiology, were €1.03 million, and for the proportion attributable to HPV 16/18 were €353,706Citation43. In Portugal, total annual healthcare costs for HPV-related penile cancers were €499,718, and for the proportion attributable to HPV 6/11/16/18 were €173,281Citation47.
Vulvar and vaginal cancers
One paper by Rémy et al.Citation31 describing a retrospective analysis of data for vulvar and vaginal cancers from the French PMSI database was identified. This cost-of-illness study assessed the economic burden of vulvar and vaginal cancers from the French healthcare-payer perspective in women hospitalized in France during 2006. The study employed the same methodology as the anal cancer study of Abramowitz et al.Citation29 and the penile cancer study of Rémy and VainchtockCitation30 described above. Consequently, similar limitations to those described above for these latter studies may have led to under-estimation of the costs associated with vulvar and vaginal cancers. In 2006, 1965 women with vulvar and vaginal cancers were treated in hospitals in France. The annual total costs of management (hospitalization, outpatient, and indirect costs) were €16.1 million. Based on the estimation that 36% of vulvar cancers and 72% of vaginal cancers are attributable to HPV infection, annual total management costs for HPV-related vulvar and vaginal cancers were €8.19 million. This study was further discussed in the paper of Borget et al.Citation45.
The paper of Jit et al.Citation44 (see above for details and limitations) reported a lifetime treatment cost of £13,650 per case of vulvar or vaginal cancer in the UK.
Two conference communications by OlsenCitation43 and Santana et al.Citation47, presenting cost data for multiple cancer types, provided costs estimated from the healthcare-payer perspective for vulvar and vaginal cancers in DenmarkCitation43 and PortugalCitation47. These two studies and their limitations in terms of use of DRG tariffs and under-reporting of cases have been discussed above in relation to anal and penile cancers. In Denmark, total annual healthcare costs (hospitalization and outpatient costs) for vulvar and vaginal cancer were €2.89 million, and for the proportion attributable to HPV 16/18 were €1.14 millionCitation43. In Portugal, total annual healthcare costs (hospitalization and outpatient costs) for HPV-related vulvar and vaginal cancers were €1.72 million, and for the proportion attributable to HPV 6/11/16/18 were €312,528Citation47.
Head and neck cancers
Compared with non-cervical anogenital cancers, the costs associated with head and neck cancers in Europe are better documented in the published literature. This may be related to the importance of head and neck cancers in terms of incidence and mortality. In 2008, ∼132,000 new cases of head and neck cancer occurred in Europe, and there were 62,800 deaths from the diseaseCitation65. Hartwig et al.Citation26 estimated that 67,354 new cases of head and neck cancer (14,098 [21%] attributable potentially to HPV) occur in men in Europe each year, compared with 2162 anal cancer cases and 3178 penile cancer cases.
An overview of health economic references for head and neck cancers is presented in .
Table 3. Overview of health economic references for head and neck cancers.
Seven published papers and a conference communication on head and neck cancers describing studies conducted in France (n = 2)Citation36,Citation37, Greece (n = 1)Citation42, The Netherlands (n = 3)Citation39–41, and the UK (n = 2)Citation33,Citation34 were selected. Three review articles that provided further cost data for head and neck cancers were also selectedCitation32,Citation35,Citation38.
Head and neck cancers are a heterogeneous group of malignancies affecting various anatomical sites, but there is no consensus regarding the aggregation of anatomical sites and the corresponding International Classification of Diseases (ICD)-10 codes. Consequently, there was no consistency in the anatomical sites represented in the selected references (). In addition, the management and treatment of head and neck cancers involve multiple medical specialities and multiple diagnostic and treatment modalities. This makes disease management cost estimations difficult. The wide range of healthcare costs per patient reported for head and neck cancers across the selected references is likely to be due to differences between studies in anatomical sites, time horizon, disease stage, and costing perspective (e.g., hospital, healthcare payer, society). Time horizons for the economic studies for head and neck cancers varied considerably, ranging from 1–10 years, with only one paper reporting a lifetime costCitation44.
Table 4. Anatomical sites for head and neck cancers represented in selected references.
Seven of the selected references described cost-of-illness studies using retrospective data from hospital databasesCitation34,Citation36,Citation37,Citation39–42, and one described a cost-effectiveness study using modelling techniques and retrospective hospital dataCitation33. Some of these papers, describing studies conducted in Greece, The Netherlands, and the UK, reported estimated hospital costs per patient that varied depending on the stage of disease or the treatment utilizedCitation33,Citation34,Citation40–42. Lacau St Guily et al.Citation37 estimated the total annual management costs (hospitalization, expensive drug, outpatient and indirect costs) for head and neck cancers in France at €530 million, which corresponded to an annual cost of €14,629 per hospitalized patient. On the basis that 26% of head and neck cancers are attributable to HPV, total annual management costs for HPV-related head and neck cancers in France were estimated at €138 millionCitation37. This study was discussed further in the paper of Borget et al.Citation45. Kim et al.Citation36 estimated the cost of post-operative healthcare (hospitalization, outpatient, homecare, and rehabilitation costs) per patient with head and neck cancer in France at €14,500 in the first year and €6800 in the second year. A retrospective analysis by Kim et al.Citation34 estimated that the mean costs of post-operative healthcare utilization for patients with squamous cell carcinoma of the head and neck in the UK was £23,212 over 5 years. The mean cost per year was £19,778 in the first year, and £455 for the fifth year. Over 10 years following diagnosis, van Agthoven et al.Citation39 estimated direct healthcare costs (hospitalization and outpatient costs) at €31,829 per patient with head and neck cancer in The Netherlands. Jit et al.Citation44 (see above for details and limitations) reported a lifetime treatment cost of £15,000 per case of oropharyngeal cancer.
Three conference communications presenting cost data for several cancers included costs for head and neck cancers in GermanyCitation46, DenmarkCitation43, and PortugalCitation47. Total annual costs of management of patients with head and neck cancers were estimated at €366 million from the societal perspective (hospitalization, inpatient rehabilitation, and sick leave costs) in GermanyCitation46, and €28.1 million from the hospital perspective (hospitalization and outpatient costs) in DenmarkCitation43. For HPV-related head and neck cancers only, the total estimated costs were €78.2 million in Germany and €5.81 million in DenmarkCitation43,Citation46. In Portugal, the total annual costs of management (hospitalization and outpatient costs) of patients with HPV-related head and neck cancers were €3.81 millionCitation47.
The majority of the selected references for head and neck cancers estimated costs from the healthcare-payer perspective and focused predominantly on hospital costs. However, notable healthcare costs (e.g., expensive drugs, radiotherapy) were excluded in several studies. The study of Rémy et al.Citation46 was the only study to estimate costs for head and neck cancers from a societal perspective, although the review article of Ruff et al.Citation38 considered smoking-attributable costs of head and neck cancers from a societal perspective. Rémy et al.Citation46 included hospitalization, inpatient rehabilitation (e.g., speech therapy, learning how to care for a stoma), and sick-leave costs. However, several cost components were not included, such as outpatient management, expensive chemotherapy, premature retirement, long-term care costs, and premature death. The absence of a comprehensive assessment of the indirect costs associated with head and neck cancers in Europe in the published literature was a noticeable omission. Head and neck cancers are associated with a range of indirect costs, including loss of productivity and income during hospitalization and recovery, potential inability to perform everyday tasks because of deformity and functional problems, potential inability to return to work, reduced quality-of-life, and premature death. In addition, because patients with head and neck cancers often experience devastating physical and functional changes as a result of their disease and treatment, rehabilitation care plays an important role in attempts to restore function and improve quality-of-life. Other costs that were excluded from studies included the costs of managing side-effects of treatment and complications (e.g., dysphagia, mucositis, nosocomial infections, and pneumonia following surgery)Citation66.
Key cost findings for non-cervical HPV-related cancers
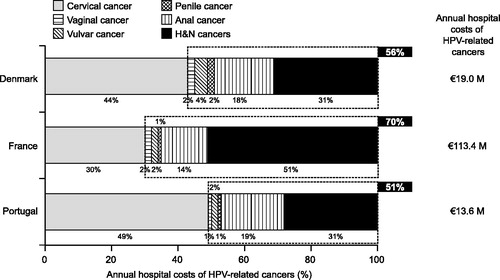
In comparing available evidence on the cost of HPV-related diseases from various sources using different methods, this review showed that non-cervical cancers contribute substantially to the economic burden of HPV-related cancers. Combining data from studies using similar methodology from DenmarkCitation43, FranceCitation45, and PortugalCitation47 showed that non-cervical cancers generate the majority of hospital costs associated with HPV-related cancers (51–70% depending on the country) (). As an example, the total annual cost of managing HPV-related cancers from a healthcare payer perspective in France was estimated to be ∼€240 million in 2006, whereas cervical cancer incurred costs of ∼€84 million (35% of total cost)Citation45.
Figure 2. Estimated annual hospital costs of cancers attributable to HPV in DenmarkCitation43, FranceCitation45, and PortugalCitation47 by type of cancer. Country (year): France (2006–2007); Denmark (2008); Portugal (2009). Burden approach: societal hospital economic burden; Perspective: hospital perspective; Type(s) of costs: hospital costs (attributable to HPV-16 &18); Analytical method: retrospective analysis of national hospital database or cancer registry (incident or prevalent patients); Time horizon: cross-sectional (yearly basis). H&N, head and neck; HPV, human papillomavirus.
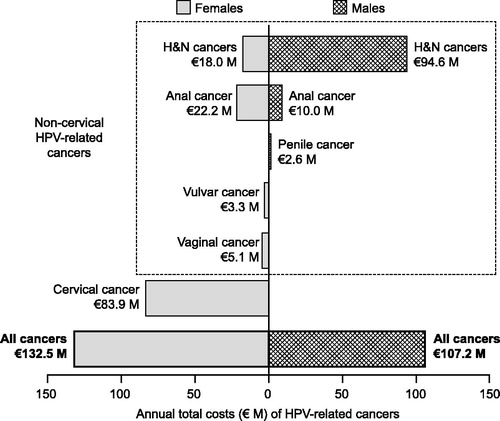
The economic burden of non-cervical cancers potentially attributable to HPV in Europe is mainly driven by males (∼70%), as illustrated by data from France ()Citation45. In Germany, a study estimated that the annual cost of managing HPV-related head and neck and anal cancers was €106.9 million in 2008, with HPV-related head and neck cancers accounting for €78.2 millionCitation46. Males accounted for ∼80% of the costs of HPV-related head and neck cancers (€62.4 million)Citation46. Consequently, when all HPV-related cancers are included, the economic burden of HPV-related cancers in males approaches that for females.
Figure 3. Estimated annual total costs of HPV-related cancers attributable to HPV in males and females in FranceCitation45. Reprinted from Borget I, Abramowitz L, Mathevet P. Economic burden of HPV-related cancers in France. Vaccine 2011;29:5245–9, with permission from Elsevier. Country (year): France (2006–2007). Burden approach: per-patient economic burden; Perspective: healthcare payer perspective; Type(s) of costs: hospital, outpatient, and daily allowance costs (attributable to HPV all types); Analytical method: retrospective analysis of national hospital database (prevalent patients); Time horizon: cross-sectional (yearly basis). H&N, head and neck; HPV, human papillomavirus.
For each disease, a wide range of costs per patient were reported (shown for anal cancer and head and neck cancers in and , respectively), particularly for head and neck cancers, which can be explained largely by disease complexity and variation in study design as explained above.
Discussion
This study provides an overview of available evidence for the substantial economic burden of non-cervical HPV-related cancers in Europe. The distribution of references across cancer types was not homogeneous, and half of the references retrieved were specific to head and neck cancers. This may be related to the importance of head and neck cancers in terms of incidence; overall (both sexes combined) and in men alone, head and neck cancers are the fifth most frequent cancer in EuropeCitation65. In addition to the papers selected for head and neck cancers, a number of other papers on these cancers were identified during the search but were excluded because they focused on a specific dimension of the disease management.
This review is of particular interest because it is one of few studies to have considered all cancers known to have an association with HPV and involved a wide search of the European literature. Although there was less evidence for anal, penile, vulvar, and vaginal cancers than for head and neck cancers, the diversity of references allowed comparison of the economic burden of these diseases with that of cervical cancer. This allows estimation of the costs that could be avoided by an HPV prevention programme that had the potential to prevent all HPV-related cancers.
The economic picture of HPV-related disease emerging from this review is not complete, however, because non-malignant diseases attributable to HPV such as genital warts, RRP, and pre-cancerous lesions, which have also been shown to impose substantial economic costs, were not included. A study estimated the economic burden of non-cervical HPV 6/11/16/18-related disease in the US in 2003 at $418 million, and reported that HPV 6 and 11-related diseases (genital warts and RRP) may account for more than 60% of this burdenCitation67. This adds weight to the importance of considering all HPV-related diseases when considering the potential benefits of HPV-preventive interventions.
Another important point highlighted by this review is that the economic burden of HPV is very significant in males and, in fact, is driven by males when focusing on non-cervical HPV-related cancers. This economic burden is far higher than usually perceived because HPV tends to be associated with women and cervical cancer. This emphasizes the importance of considering both males and females when assessing the impact of HPV.
A number of methodological issues were identified while reviewing the selected references. Some of these issues were related to clinical aspects of study design as illustrated by the variability in design (i.e., the ICD-10 codes considered) of head and neck cancer studies described above. The majority of studies described in the selected references adopted a cross-sectional approach on a 1-year basis. Some studies of head and neck cancers evaluated costs over 2–5 years, but only one Dutch study evaluated the course of disease over an extended period of up to 10 yearsCitation39. A longitudinal approach is preferred over a cross-sectional approach for capturing costs incurred by cancers because of their chronicity, and future studies should adopt an adequate time horizon to capture the vast majority of costs. To improve consistency in future economic studies, an ‘episode of care’ would be a useful standard framework for defining costs during the course of a cancer.
In most of the studies, costs reported were not specific to HPV-related cancers. HPV-related costs were extrapolated from other information sources by considering the proportion of the specific cancer type reported to be associated with HPV. This could be a limitation of this review as it is unclear whether the aetiology of the cancer has an impact on the cost of management. There were no data retrieved suggesting that there is a difference in economic outcome for HPV- versus non-HPV-attributable cancers. Some studies indicated that patients with HPV-attributable cancers have a better prognosis than patients with cancers attributable to other factors (e.g., smoking)Citation68, which could mean that reports of costs associated with HPV-attributable cancers might be over-estimated. However, as patients with HPV-related cancers tend to be younger than patients with non-HPV-related cancersCitation69, they may live longer and, as a result, experience more recurrences and side-effects of treatment, thereby incurring higher costs.
Several other criticisms may be levelled at the economic methodology used in selected references. Each study reported only a fraction of the true economic burden of the cancer under investigation because incomplete costs were included. Most studies reported direct medical costs, but these were frequently under-estimated because studies did not consider all types of medical cost (i.e., outpatient costs were often not included). Few studies reported indirect costs and, where this occurred, most included daily allowance payment to patients but did not include true indirect costsCitation29–31,Citation37,Citation45. Costs associated with productivity losses were only considered in one review article of smoking-attributable head and neck cancersCitation38. The economic burden of HPV-related cancers is therefore invariably under-estimated as the cost associated with productivity losses due to illness or early mortality are rarely considered. Comparisons of costs across studies and countries were often hampered by differences in the costing perspective and the variety of data sources (ad-hoc study, administrative databases/registries, expert opinion, literature, clinical practice guidelines). The country with the largest number of selected references was France, where a series of economic studies for the different diseases employed the same methodology to estimate hospitalization, outpatient, and indirect (daily allowance) costsCitation29–31,Citation37.
A range of costing approaches was applied in the selected references, including macro- and micro-costing. Macro-costing is the least accurate method and involves identifying and measuring intermediate resource consumption units (e.g., hospital stay). Micro-costing is the most accurate method and involves identifying and measuring the components of a resource consumption unit (e.g., consultation, diagnostics, surgery, etc.) and combining these to estimate the composite intermediate resource consumption unit. Some selected references, notably those describing studies of head and neck cancers conducted in The NetherlandsCitation39–41, adopted a micro-costing approach. In contrast, other studies, including several conducted in France, used a macro-costing approach, basing hospitalization costs on DRG tariffs that do not include the cost of expensive drugsCitation29–31,Citation37,Citation43,Citation46. Consequently, the direct medical costs reported in these latter studies were under-estimated. In order to provide comprehensive cost data from the broadest societal perspective, future studies should focus on the micro-costing approach and include direct and indirect costs. This will allow identification and comparison of specific costs, and enable cost data to be tailored for the interested stakeholder (hospital, third-party payer, society, etc.).
Conclusion
Considerable challenges are associated with estimating the healthcare costs of cancerCitation70. Cancers are complex diseases involving interdisciplinary diagnostic and treatment approaches. In addition, cancers are associated with frequent side-effects of treatment, complications arising from treatment and the disease itself, and a chronic disease course with the risk of recurrence; these factors complicate the capture of all relevant costs. The increasing incidence of cancers as the population in Europe ages, the development of new and expensive treatments, and an emphasis on the containment of healthcare costs make the economics of cancer care a focus for healthcare payers.
Evidence for the involvement of HPV in cancers is increasing, and questions are being raised about the potential benefits of HPV vaccination on the incidence of non-cervical cancers. Estimations of the costs to healthcare systems and society associated with all cancers attributable to HPV 16/18 are important for assessing the economic impact of HPV vaccination programmes. This review shows that non-cervical cancers account for a major part of the economic burden of cancers potentially attributable to HPV and that this burden is mainly driven by males. This highlights the importance of considering all diseases attributable to HPV when assessing the potential benefits of preventive interventions such as HPV vaccination programmes, and raises questions about the benefits of HPV vaccination beyond those observed in the current target population of young girls.
Priorities for future research are refinement of cost estimates by including all identifiable direct and indirect costs and utilization of a time horizon that encompasses the majority of costs associated with each cancer type. Inclusion of cost data for HPV-related pre-cancerous lesions, genital warts and RRP would allow a more complete estimate of the economic impact of HPV-related diseases in Europe.
Transparency
Declaration of funding
This review was performed by Sanofi Pasteur MSD.
Declaration of financial/other relationships
Emmanuelle Préaud and Nathalie Largeron are employees of Sanofi Pasteur MSD. JME Peer Reviewers on this manuscript have no relevant financial relationships to disclose.
Acknowledgements
The authors take full responsibility for the content of this contribution and thank Claire Takizawa and Lionel Moro (former employees of Sanofi Pasteur MSD) for their involvement in specific steps of the literature review, and Communigen Limited, Oxford, UK (supported by Sanofi Pasteur MSD) for their assistance in preparing the manuscript.
References
- von Krogh G. Management of anogenital warts (condylomata acuminata). Eur J Dermatol 2001;11:598-603
- Parkin DM, Bray F. Chapter 2: the burden of HPV-related cancers. Vaccine 2006;24(3 Suppl):S3/11-25
- Wallboomers JM, Jacobs MV, Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol 1999;189:12-19
- Aubin F, Prétet JL, Jacquard AC, et al. Human papillomavirus genotype distribution in external acuminata condylomata: a Large French National Study (EDiTH IV). Clin Infect Dis 2008;47:610-5
- Donne AJ, Hampson L, Homer JJ, et al. The role of HPV type in recurrent respiratory papillomatosis. Int J Pediatr Otorhinolaryngol 2010;74:7-14
- De Vuyst H, Clifford GM, Nascimento MC, et al. Prevalence and type distribution of human papillomavirus in carcinoma and intraepithelial neoplasia of the vulva, vagina and anus: a meta-analysis. Int J Cancer 2009;124:1626-36
- Gillison M. HPV and its effect on head and neck cancer prognosis. Clin Adv Hematol Oncol 2010;8:680-2
- Giuliano AR, Tortolero-Luna G, Ferrer E, et al. Epidemiology of human papillomavirus infection in men, cancers other than cervical and benign conditions. Vaccine 2008;26(10 Suppl):K17-28
- de Villiers EM, Fauquet C, Broker TR, et al. Classification of papillomaviruses. Virology 2004;324:17-27
- Kirrander P, Kolaric A, Helenius G, et al. Human papillomavirus prevalence, distribution and correlation to histopathological parameters in a large Swedish cohort of men with penile carcinoma. BJU Int 2011;108:355-9
- Smith JS, Lindsay L, Hoots B, et al. Human papillomavirus type distribution in invasive cervical cancer and high-grade cervical lesions: a meta-analysis update. Int J Cancer 2007;121:621-32
- Acay R, Rezende N, Fontes A, et al. Human papillomavirus as a risk factor in oral carcinogenesis: a study using in situ hybridization with signal amplification. Oral Microbiol Immunol 2008;23:271-4
- Yanofsky VR, Patel RV, Goldenberg G. Genital warts: a comprehensive review. J Clin Aesthet Dermatol 2012;5:25-36
- Sanchez GI, Jaramillo R, Cuello G, et al. Human papillomavirus genotype detection in recurrent respiratory papillomatosis (RRP) in Colombia. Head Neck 2013;35:229-34
- Clifford GM, Rana RK, Franceschi S, et al. Human papillomavirus genotype distribution in low-grade cervical lesions: comparison by geographic region and with cervical cancer. Cancer Epidemiol Biomarkers Prev 2005;14:1157-64.
- Arbyn M, Castellsagué X, de Sanjosé S, et al. Worldwide burden of cervical cancer in 2008. Ann Oncol 2011;22:2675-86
- Ting J, Kruzikas DT, Smith JS. A global review of age–specific and overall prevalence of cervical lesions. Int J Gynecol Cancer 2010;20:1244-9
- Arveux P, Bénard S, Bouée S, et al. [Invasive cervical cancer treatment costs in France]. Bull Cancer 2007;94:219-24 [Article in French]
- Ricciardi A, Largeron N, Giorgi Rossi P, et al. Incidence of invasive cervical cancer and direct costs associated with its management in Italy. Tumori 2009;95:146-52
- Brown RE, Breugelmans JG, Theodoratou D, et al. Costs of detection and treatment of cervical cancer, cervical dysplasia and genital warts in the UK. Curr Med Res Opin 2006;22:663-70
- Robinson D, Coupland V, Møller H. An analysis of temporal and generational trends in the incidence of anal and other HPV-related cancers in Southeast England. Br J Cancer 2009;100:527-31
- Nielsen A, Munk C, Kjaer SK. Trends in incidence of anal cancer and high-grade anal intraepithelial neoplasia in Denmark, 1978-2008. Int J Cancer 2012;130:1168-73
- Ramqvist T, Dalianis T. An epidemic of oropharyngeal squamous cell carcinoma (OSCC) due to human papillomavirus (HPV) infection and aspects of treatment and prevention. Anticancer Res 2011;31:1515-9
- Attner P, Du J, Näsman A, et al. The role of human papillomavirus in the increased incidence of base of tongue cancer. Int J Cancer 2010;126:2879-84
- Mehanna H, Jones TM, Gregoire V, et al. Oropharyngeal carcinoma related to human papillomavirus. BMJ 2010;340:c1439
- Hartwig S, Syrjänen S, Dominiak-Felden G, et al. Estimation of the epidemiological burden of human papillomavirus-related cancers and non-malignant diseases in men in Europe: a review. BMC Cancer 2012;12:30
- Karnon J, Jones R, Czoski-Murray C, et al. Cost-utility analysis of screening high-risk groups for anal cancer. J Public Health 2008;30:293-304
- Czoski-Murray C, Karnon J, Jones R, et al. Cost-effectiveness of screening high-risk HIV-positive men who have sex with men (MSM) and HIV-positive women for anal cancer. Health Technol Assess 2010;14:1-131
- Abramowitz L, Rémy V, Vainchtock A. Economic burden of anal cancer management in France. Rev Epidemiol Sante Publique 2010;58:331-8
- Rémy V, Vainchtock A. Hospitalisation and management costs of patients with penile cancer in France. Paris, France: European Academy of Dermatology and Venereology (EADV), 2008 [Poster presentation]
- Rémy V, Mathevet P, Largeron N, et al. Cost of management of vulvar and vaginal cancers in France. Journal d’Economie Médicale 2010;28:31-45
- Mignogna MD, Fedele S, Lo Russo L, et al. Costs and effectiveness in the care of patients with oral and pharyngeal cancer: analysis of a paradox. Eur J Cancer Prev 2002;11:205-8
- Speight PM, Palmer S, Moles DR, et al. The cost-effectiveness of screening for oral cancer in primary care. Health Technol Assess 2006;10:1-144
- Kim K, Amonkar MM, Högberg D, et al. Economic burden of resected squamous cell carcinoma of the head and neck in an incident cohort of patients in the UK. Head Neck Oncol 2011;3:1-10
- Selke B, Allenet B, Bercez C, et al. [Economic assessments of head and neck cancers: a review]. Bull Cancer 2001;88:759-64 [Article in French]
- Kim K, Faivre P, Cancalon C, et al. Healthcare utilisation and costs of resected squamous cell carcinoma of head and neck (SCCHN) in France. Barcelona, Spain: European Society for Therapeutic Radiology and Oncology (ESTRO), 2010 [Poster presentation]
- Lacau St Guily JL, Borget I, Vainchtock A, et al. Head and neck cancers in France: an analysis of the hospital medical information system (PMSI) database. Head Neck Oncol 2010;2:22
- Ruff LK, Volmer T, Nowak D, et al. The economic impact of smoking in Germany. Eur Respir J 2000;16:385-90
- van Agthoven M, van Ineveld BM, de Boer MF, et al. The costs of head and neck oncology: primary tumours, recurrent tumours and long-term follow-up. Eur J Cancer 2001;37:2204-11
- Nijdam W, Levendag P, Noever I, et al. Cancer in the oropharynx: cost calculation of different treatment modalities for controlled primaries, relapses and grade III/IV complications. Radiother Oncol 2005;77:65-72
- van Agthoven M, Heule-Dieleman HAG, Knegt PP, et al. Compliance and efficiency before and after implementation of a clinical practice guideline for laryngeal carcinomas. Eur Arch Otorhinolaryngol 2006;263:729-37
- Zavras A, Andreopoulos N, Katsikeris N, et al. Oral cancer treatment costs in Greece and the effect of advanced disease. BMC Public Health 2002;2:12
- Olsen J. Incidence and costs of anal, penile, vaginal, vulva and head and neck cancer in Denmark. Lisbon, Portugal: European Research Organisation on Genital Infection and Neoplasia (EUROGIN), 2011 [Oral presentation]
- Jit M, Chapman R, Hughes O, et al. Comparing bivalent and quadrivalent human papillomavirus vaccines: economic evaluation based on transmission model. BMJ 2011;343:d5775
- Borget I, Abramowitz L, Mathevet P. Economic burden of HPV-related cancers in France. Vaccine 2011;29:5245-9
- Rémy V, Heitland W, Klussmann J, et al. Economic burden of HPV-related head & neck and anal cancers in Germany. Value Health 2011;14:A443
- Santana R, Lopes S, Costa C. Human papillomavirus disease burden in Portugal. Lisbon, Portugal: European Research Organisation on Genital Infection and Neoplasia (EUROGIN), 2011 [Poster presentation]
- Bongers V, Hobbelink MG, van Rijk PP, et al. Cost-effectiveness of dual-head 18F-fluorodeoxyglucose PET for the detection of recurrent laryngeal cancer. Cancer Biother Radiopharm 2002;17:303-6
- Baujat B, Altabaa K, Meyers M, et al. Medicoeconomic study of microsurgical head and neck reconstructions. Eur Ann Otorhinolaryngol Head Neck Dis 2011;128:121-6
- Hopper C, Niziol C, Sidhu M. The cost-effectiveness of Foscan mediated photodynamic therapy (Foscan-PDT) compared with extensive palliative surgery and palliative chemotherapy for patients with advanced head and neck cancer in the UK. Oral Oncol 2004;40:372-82
- Brown B, Diamantopoulos A, Bernier J, et al. An economic evaluation of cetuximab combined with radiotherapy for patients with locally advanced head and neck cancer in Belgium, France, Italy, Switzerland and the United Kingdom. Value Health 2008;11:791-9
- Lundkvist J, Ekman M, Ericsson SR, et al. Proton therapy of cancer: potential clinical advantages and cost-effectiveness. Acta Oncol 2005;44:850-61
- Bonastre MJ, Noël E, Bensadoun RJ, et al. The cost of intensity modulated radiation therapy in head and neck cancers: results of the 2002 STIC study. Bull Cancer 2006;93:1026-32
- Nijdam W, Levendag P, Noever I, et al. Cost analysis comparing brachytherapy versus surgery for primary carcinoma of the tonsillar fossa and/or soft palate. Int J Radiat Oncol Biol Phys 2004;59:488-94
- Leon X, Quer M, Orus C, et al. How much does it cost to preserve a larynx? An economic study. Eur Arch Otorhinolaryngol 2000;257:72-6
- Watters K, O’Dwyer TP, Rowley H. Cost and morbidity of MRSA in head and neck cancer patients: what are the consequences? J Laryngol Otol 2004;118:694-9
- Penel N, Lefebvre JL, Cazin JL, et al. Additional direct medical costs associated with nosocomial infections after head and neck cancer surgery: a hospital-perspective analysis. Int J Oral Maxillofac Surg 2008;37:135-9
- Bennett CL, Lane D, Stinson T, et al. Economic analysis of amifostine as adjunctive support for patients with advanced head and neck cancer: preliminary results from a randomized phase II clinical trial from Germany. Cancer Invest 2001;19:107-13
- Preuss SF, Quante G, Semrau R, et al. An analysis of surgical complications, morbidity, and cost calculation in patients undergoing multimodal treatment for operable oropharyngeal carcinoma. Laryngoscope 2007;117:101-5
- Braaksma M, van Agthoven AM, Nijdam W, et al. Costs of treatment intensification for head and neck cancer: concomitant chemoradiation randomized for radioprotection with amifostine. Eur J Cancer 2005;41:2102-11
- Hampl M, Huppertz E, Schulz-Holstege O, et al. Economic burden of vulvar and vaginal intraepithelial neoplasia: retrospective cost study at a German dysplasia centre. BMC Infect Dis 2011;11:73
- Olsen J, Jørgensen TR, Kofoed K, et al. Incidence and cost of anal, penile, vaginal and vulvar cancer in Denmark. BMC Public Health 2012;12:1082
- Heitland W, Schädlich PK, Chen X, et al. Annual cost of hospitalization, inpatient rehabilitation and sick leave of anal cancer in Germany. J Med Econom 2013;16:364-71
- Klussmann JP, Schädlich PK, Chen X, et al. Annual cost of hospitalization, inpatient rehabilitation, and sick leave of head and neck cancers in Germany. ClinicoEconom Outcomes Res 2013; accepted for publication
- Ferlay J, Parkin DM, Steliarova-Foucher E. Estimates of cancer incidence and mortality in Europe in 2008. Eur J Cancer 2010;46:765-81
- Brown B, Diamantopoulos A, Bernier J, et al. An economic evaluation of cetuximab combined with radiotherapy for patients with locally advanced head and neck cancer in Belgium, France, Italy, Switzerland, and the United Kingdom. Value Health 2008;11:791-9
- Hu D, Goldie SJ. The economic burden of noncervical human papillomavirus disease in the United States. Am J Obstet Gynecol 2008;198:500-7
- Fakhry C, Westra WH, Li S, et al. Improved survival of patients with human papillomavirus-positive head and neck squamous cell carcinoma in a prospective clinical trial. J Natl Cancer Inst 2008;100:261-9
- Chaturvedi AK, Engels EA, Anderson WF, et al. Incidence trends for human papillomavirus-related and -unrelated oral squamous cell carcinomas in the United States. J Clin Oncol 2008;26:612-9
- Szucs TD, Dedes KJ. Balancing costs and benefits in cancer therapy and prevention. Ann Oncol 2008;19(7 Suppl):vii313-9
- Olsen J, Jorgensen TR, Rubek N. The economic burden of head and neck cancers in Denmark. Int J Otolaryngol Head Neck Cancers 2013 ; accepted for publication
Appendix: Keywords used for the literature search
Table A1. Keywords used for the literature search.