Abstract
Objective:
This study quantified the direct healthcare costs and major cost drivers among patients with Huntington’s disease (HD), by disease stage in commercial and Medicaid databases.
Methods:
This retrospective database analysis used healthcare utilization/cost data for HD patients (ICD-9-CM 333.4) from Thomson Reuters’ MarketScan Commercial and Medicaid 2002–2009 databases. Patients were classified by disease stage (Early/Middle/Late) by a hierarchical assessment of markers of disease severity, confirmed by literature review and key opinion leader input. Costs were measured over the follow-up time of each patient with total costs per patient per stage annualized using a patient-year cost approach.
Results:
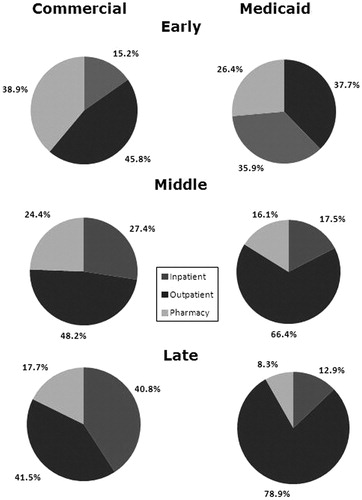
Among 1272 HD patients, the mean age was similar in commercial (752 patients) and Medicaid (520 patients) populations (48.5 years (SD = 13.3) and 49.3 years (SD = 17.2), respectively). Commercial patients were evenly distributed by stage (30.5%/35.5%/34.0%; Early/Middle/Late). However, most (74.0%) Medicaid HD patients were classified as Late stage. The mean total annualized cost per patient increased by stage (commercial: $4947 (SD = $6040)–$22,582 (SD = $39,028); Medicaid: $3257 (SD = $5670)–$37,495 (SD = $27,111). Outpatient costs were the primary healthcare cost component. The vast majority (73.8%) of Medicaid Late stage patients received nursing home care and the majority (54.6%) of Medicaid Late stage costs were associated with nursing home care. In comparison, only 40.6% of commercial Late stage patients received nursing home care, which contributed to only 4.6% of commercial Late stage costs.
Conclusions:
The annual direct economic burden of HD is substantial and increased with disease progression. More late stage Medicaid HD patients were in nursing homes and for a longer time than their commercial counterparts, reflected by their higher costs (suggesting greater disease severity). Key limitations include the classification of patients into a single stage, as well as a lack of visibility into full long-term care/nursing home-related costs for commercial patients.
Introduction
Huntington’s disease (HD) is a rare, autosomal dominant, neurodegenerative disorder caused by an expanded CAG trinucleotide repeat in the huntingtin (HTT) gene, with an estimated prevalence of 7 per 100,000 in the Western HemisphereCitation1,Citation2. Early symptoms of HD include cognitive and behavioral alterations and psychiatric disturbancesCitation3. Formal clinical diagnosis currently relies upon significant motor dysfunction and confirmation through genetic testingCitation4. HD is marked by adult onset, with a mean age of onset between 30–50 years and with a mean duration of disease between 17–20 years; however, age of onset and rate of disease progression are variable from person to personCitation5–7.
To date there are no disease-modifying therapies that can slow the progression of HD, although some therapeutic approaches (such as movement-suppressing drugs, antidepressants, and physical therapy) may ameliorate symptoms. However, HD inexorably causes significant progressive motor, cognitive, and psychiatric impairment, decreasing an individual’s independence and the ability to carry out activities of daily living, with long-term nursing home care a potential necessary optionCitation6,Citation8.
HD has a substantial economic impact on patients, caregivers, and the healthcare system; however, this impact has not been quantified. Very few studies have assessed the cost of care for HD, and none have attempted to evaluate how costs vary with disease progression. The few studies that have assessed costs have done so via a survey of either patients with HD or other neurological disease, or their caregivers, while only one study has assessed direct costs, limited to HD hospitalizationsCitation9–11. No studies have assessed the comprehensive and direct medical costs of HD. Given the paucity of relevant economic data, there is a need for a study, based on a representative sample of the United States (US) population, to assess the current costs of comprehensive HD direct medical care.
Our study sought to quantify the direct economic burden of manifest HD and identify major cost drivers among HD patients, overall and by disease stage, utilizing both commercial and Medicaid claims databases. Given the lack of general knowledge of the direct costs of HD or the association between direct costs and HD disease progression, our study sought to investigate how costs vary by disease stage, with the intent of highlighting the economic consequences of HD and disease progression and raising awareness of the unmet treatment needs in HD and the importance of further research.
Patients and methods
Data source
Data were obtained from the MarketScan® Medicaid and Commercial Databases (now Truven Health Analytics)Citation12. Both databases were chosen due to the payer mix of HD patients; patients most commonly transition from commercial insurance to Medicaid once they lose employment and/or spend down (i.e., patients have too much income to qualify for Medicaid and spend their excess income in order to qualify) when they require funding for long-term care. However, there is a 2 year waiting period for Medicaid for HD patients, following the determination of HD disability; therefore, Medicaid-eligible patients may have substantially worse disease progression when compared with/to commercial-insurance patients. The MarketScan Commercial Database contains information on employees and their dependents from the private health insurance plans of over 100 employer-sponsored and private health plans throughout the US. The Multi-State Medicaid database contains claims data from 9–12 unidentified states (depending upon the year). These databases provide fully integrated, adjudicated, de-identified, patient-level healthcare claims data, reflecting real-world treatment patterns and costs. They provide information from inpatient and outpatient settings, and prescription drug claims, allowing for longitudinal tracking of healthcare utilization and costs of enrolled individuals. Complete payment information, both what the plan and patient paid, are captured.
Sample selection
Claims from the time period 2002–2009 were assessed to identify HD patients. Patients were selected based upon having a claim with at least one ICD-9-CM diagnosis code of 333.4 (Huntington’s chorea)Citation13.
Stage cohorts
HD disease progression post-diagnosis is traditionally divided into five stages based upon clinical assessment using the Total Functional Capacity (TFC) scale which measures functioning in five areas: occupation, finances, domestic chores, activities of daily living, and level of careCitation5. As a patient progresses through the stages, their ability and independence in these areas decline. Since the claims data do not allow for the identification of these traditional five stages, we identified claims to be used as ‘disease markers’ (either diagnoses or services received; see ) to distinguish between the stages of disease progression. We developed an algorithm based upon these disease markers to assign disease stages and categorize clinically diagnosed HD patients into Early, Middle and Late stages of HD. There can be great variability in clinical characteristics at each stage by patient; we attempted to identify the defining characteristics of these stages. The algorithm and markers were validated based upon a review of the clinical literature, an exploratory analysis of the data, and key opinion leader (KOL) clinical input (authors Dr Anderson and Dr Langbehn).
Table 1. Disease markers of Huntington’s disease stage.
We followed a hierarchical assessment in which we first identified patients in Late stage due to the presence of any Late stage marker. Late stage patients have multiple and severe clinical characteristics, such as residence in a nursing home or use of a feeding tube. We then worked backwards and, for patients with no markers of Late stage, we identified those in Middle stage based upon the presence of any Middle stage marker. Middle stage patients also have a number of definitive clinical characteristics such as the use of physical therapy or home assistance. All remaining patients were classified as Early stage based on the absence of Late or Middle stage markers. Due to the progressive nature of HD in which patients transition between stages slowly over a gradual period of time, we did not attempt to identify patients who transitioned between stages, or to separate their observed time into their respective stages.
Enrollment requirements
The first observed HD claim was termed the index date. A 180-day pre-index period was imposed prior to the index HD claim for patients classified as Early stage, to ensure a long enough period of continuous enrollment without any identified Middle or Late stage markers. No pre-index period was imposed for Middle or Late stage patients. For all stages, we imposed a minimum of 6 months continuous enrollment post-index, in order to maximize patient sample size, as well as to add confidence to our annualized cost calculations (described below).
Analyses
For the commercial and Medicaid populations, patients were characterized by demographic characteristics, as well as cumulative time enrolled in the database, overall and by stage. HD-related comorbidities were identified based on the presence of associated ICD-9-CM diagnosis codes. Healthcare costs were classified by type of service (inpatient, outpatient, or pharmacy). Outpatient care was further sub-divided by service type (ancillary, ER visits, radiology, physical therapy, GP, etc.). Additionally, characteristics and costs of long-term care/nursing home utilization were assessed. However, long-term care/nursing home care (inclusive of room and board, medical services received, etc.) is not able to be stratified by mutually exclusive cost groups (i.e., inpatient, outpatient, or pharmacy) as a function of the databases. Costs were calculated as the amounts paid by primary and secondary insurers and by patients (i.e., copayments and deductibles), and updated to 2011 values using the Medical Component of the CPI IndexCitation14. All dollar figures represent US dollars (USD), denoted as $. Costs were evaluated on a per cohort member basis, as has been done in other burden of illness studies in comparable diseasesCitation15. Thus, the denominator includes all patients in a cohort whether they experienced utilization in a service category or not (for example, a patient who had no inpatient stays would contribute a cost of $0 for inpatient stay costs).
The average annual cost per patient was calculated. Each patient’s cost was measured over the time enrolled and then allocated to their assigned stage. Total costs per patient, by stage, were annualized using a patient-year cost approach; time less than or greater than 1 year was weighted accordingly to provide an average cost per year. For example, for a patient with 9 months of continuous enrollment post-index, his/her costs would be multiplied by 4/3 to arrive at annualized costs, while a patient with 1 year and 8 months would have his/her costs multiplied by 3/5 to arrive at annualized costs. Costs were reported descriptively for the overall population and by stage, for both the commercial and Medicaid databases. Because HD-related morbidity increases with disease progression, no attempts were made to control for baseline characteristics. Statistical analyses were not conducted between Medicaid and commercial patients, nor internally between stages within a plan, given the separate databases and inherent differences between commercial and Medicaid insurance.
All analyses were conducted using SAS® Release 9.2 (SAS Institute Inc., Cary, NC).
Results
Study sample
A total of 1272 patients (752 from the commercial and 520 from the Medicaid MarketScan 2002–2009 databases) were identified (see ) based upon an ICD-9-CM diagnosis code of 333.4 (Huntington’s chorea) and who met the other enrollment requirements. Overall, there was a similar mean age in the commercial and Medicaid populations (48.5 years (SD = 13.3) and 49.3 years (SD = 17.2), respectively). The majority of patients in both populations were female, with a slightly higher female representation among Medicaid patients (60.8% vs 54.1%). There was a fairly even distribution of patients by disease stage in the commercial population (30.5% classified as Early stage, 35.5% Middle stage, and 34.0% Late stage). In the Medicaid population, the vast majority (74.0%) was classified as Late stage. This is likely a function of the Medicaid insurance system, whereby patients with advanced disease only become eligible for Medicaid after exhausting all other resources and following a 2 year waiting period for the determination of disability. Additionally, more Medicaid Late stage patients were 65 years of age or older compared to commercial Late stage patients (21.3% vs 1.2%), further suggesting the greater disease progression among Medicaid patients.
Table 2. Demographic and clinical characteristics by stage for the commercial and Medicaid Huntington’s disease population, overall and by stage.
Some demographic variables are only available for one population. For the commercial population, half of patients (49.9%) were the employee who was the primary insurance holder, while 42.4% were the spouse. Among Medicaid patients, the vast majority were White (77.1%) and 17.5% were Black.
Overall, the prevalence of HD-related comorbidity was higher in the Medicaid population, which also had a greater proportion of Late stage patients (see ). HD-related psychiatric comorbidity was high in both populations and depression and anxiety were the most prevalent comorbidities (37.4% and 21.1% in the commercial population, and 46.3% and 25.6% in the Medicaid population, respectively). The prevalence of many HD-related comorbidities increased by stage in both populations, including depression and confusion.
Inpatient admissions
For inpatient admissions, the mean total annualized cost per patient increased greatly from Early to Late stage, ranging from $754 (SD = $2452) to $9218 (SD = $29,701) in the commercial population and $1229 (SD = $5173) to $4830 (SD = $10,006) in the Medicaid population (see ). Mean total costs more than doubled between Middle and Late stages. Costs were almost twice as high for Late stage commercial patients than for their Medicaid counterparts.
Table 3. Annualized direct medical costs (2011 US$) per patient for the commercial and Medicaid Huntington’s disease population, by stage and by service type.
Outpatient services
For outpatient services, the mean total annualized cost per patient increased from Early to Late stage, and in the commercial population ranged from $2268 (SD = $2487) to $9365 (SD = $14,423), and in the Medicaid population ranged from $1168 (SD = $2139) to $29,572 (SD = $24,452) (see ). Outpatient costs more than tripled between Middle and Late stages for Medicaid patients. Among Late stage patients, costs for Medicaid patients were 3-times the costs of commercial patients. The bulk of outpatient costs came from ancillary services (diagnostic or treatment-related procedures). Ancillary costs represented a higher proportion of outpatient costs for the Medicaid population than the commercial population and increased from Early to Late stage (66.1% to 96.6% vs 48.5% to 69.5%, respectively).
Pharmacy
The mean total annualized pharmacy cost per patient increased from Early to Late stage and ranged from $1925 (SD = $3803) to $3999 (SD = $5739) in the commercial population and $860 (SD = $1149) to $3094 (SD = $3338) in the Medicaid population (see ). Pharmacy costs approximately doubled between Early and Middle stage. For all stages, pharmacy costs were higher for the commercial population than for their Medicaid counterparts.
Overall
Overall, the mean total annualized cost per patient increased from Early to Late stage and ranged from $4947 (SD = $6040) to $22,582 (SD = $39,028) in the commercial population, and $3257 (SD = $5670) to $37,495 (SD = $27,111) in the Medicaid population (see ). Costs more than tripled between Early and Middle stage for both the commercial and Medicaid populations. Between Middle and Late stage, costs increased by ∼50% in the commercial population, whereas costs more than tripled in the Medicaid population. Outpatient services were the primary component of total costs for commercial patients, ranging from 42–48% (see ). Among Medicaid patients, inpatient admissions were the primary cost component for Early stage (37.7%; however the sample size of 38 patients was limited), while the vast majority of Middle and Late stage costs were attributed to outpatient services (66.4% and 78.9%, respectively).
Long-term care/nursing home
Long-term care/nursing home costs for Late stage patients in both the commercial and Medicaid populations (see ) are not exclusive of the cost service types above (e.g., a patient receiving physical therapy in a nursing home would have a physical therapy outpatient claim associated with nursing home care). Almost twice as many Medicaid Late stage patients had at least one claim for long-term care/nursing home compared to their commercial counterparts (73.8% vs 40.6%, respectively) and spent twice as much time there (1213.8 days (SD = 1142) vs 528.5 days (SD = 617.7), respectively). This is reflected in the mean total annualized cost per patient for Medicaid patients, which was 20-times higher than for commercial patients ($20,455 (SD = $21,501) vs $1039 (SD = $3611), respectively). Long-term care/nursing home costs were associated with more than half (54.6%) of total Late stage Medicaid costs, but only 4.6% of Late stage commercial costs. However, it is likely that, for commercial patients, we lack visibility into receipt of long-term care/nursing home care, as commercial insurance does not typically reimburse such care, and patients must fund their care through a long-term care-focused insurer.
Discussion
We comprehensively examined the direct annual medical costs of HD in commercially-insured and Medicaid populations, and found increasing costs with HD disease progression ($4947 (SD = $6040) to $22,592 (SD = $39,028) and $3257 (SD = $5670) to $37,495 (SD = $27,111), respectively). Late stage costs were substantial, and Medicaid Late stage costs were more than 66% higher than their commercial counterparts. Costs associated with long-term care/nursing home care contributed to more than half of Medicaid Late stage costs; however, more Medicaid Late stage patients were in long-term care/nursing home and, for a longer time, compared to their commercial counterparts. However, it is uncertain whether Medicaid Late stage patients have higher overall and long-term care/nursing home costs due to more advanced disease or whether the commercial database lacks full visibility into long-term care/nursing home use, or a combination of the two.
Our average yearly pharmacy costs were higher for commercial patients compared to Medicaid patients, and may be partly explained by Medicaid pharmacy discounts. It is important to note that tetrabenazine (Xenazine®), the only FDA-approved treatment for chorea associated with Huntington’s disease, was approved in the US in August 2008 and therefore only patients followed through 2009 would reflect the substantial costs of tetrabenazine to the payer. While we did not examine annual cost trends between 2002–2009, it is likely pharmacy costs will have increased in recent years with the approval of this drug.
Our study is the only one to our knowledge which assesses the comprehensive, direct costs of HD among a large, representative sample of US patients. Only one study has provided direct cost data related to HD, using the 1996–2002 Nationwide Inpatient Sample, with scope limited to inpatient costs of HD patients by admission diagnosisCitation11. Two studies have assessed HD costs through survey methods, however only one was conducted in the USCitation9,Citation10. This study surveyed healthcare utilization in neurological illnesses, including HD, as reported by caregivers, in 1996Citation9. Based on healthcare utilization, the authors estimated a total annual adjusted direct cost for HD including long-term care, hospital care, and paid home care of ∼$17,614 (updated to 2011 dollars) for the 51 HD patients, of whom 42% had reported long-term care utilization. This annual cost is between our comprehensive commercial Middle and Late stage costs. It is likely that the survey study was skewed toward more late-stage HD patients, as these patients had caregivers and 42% utilized long-term care.
Since we are unable to compare our findings to any other comprehensive direct medical cost analyses in HD, we identified claims database studies which assessed the direct cost of illness in other progressive neurological illnesses: Alzheimer’s disease (AD), multiple sclerosis (MS), and Parkinson’s disease (PD). Our HD cost burden may be considered relative to the costs of these other illnesses which have established costs (which we have updated to 2011 USD), and which are in some aspects comparable to HD. A study using comprehensive claims data found annualized costs for Medicare patients with AD in the pre-index year (prior to the first AD claim) of $15,305 and the post-index year of $28,263Citation16. These costs are comparable to our HD Middle and Late stage costs, respectively. The direct costs of MS were assessed using commercial and public claims data and an annual cost of $16,425 was found, comparable to our Middle stage costsCitation17. The annual cost of PD among both commercial and Medicaid patients was found to be $31,849, which is within the range of our Late stage costsCitation18. The major cost drivers varied in these studies: inpatient care (inclusive of nursing home costs) for AD, pharmacy for MS, and outpatient care for PD costs (as was the case for our HD costs, for the most part). Additionally, a few analyses have classified patients into stage and demonstrated increased cost with disease progression. Annual costs of later-stage was considerably higher than earlier-stage among Medicare AD patients ($9860 and $46,952, respectively)Citation19. Among Medicare MS patients, higher annual costs were found for pre-existing primary progressive MS than pre-existing relapsing-remitting MS (RRMS) ($27,903 and $6,952, respectively)Citation20.
We identified the costs for a reference cohort of healthy patients from Thomson Reuters’ MarketScan commercial and Medicaid databases to provide a comparator group in order to assess the incremental costs which may be attributable to HDCitation21. Average total annual costs (updated to 2011 USD) were $4067 and $5191 for commercial and Medicaid healthy controls, respectively. For the commercial population, this mean reference cost is slightly lower than the cost for our Early stage commercial patients. Our small sample of Early stage Medicaid patients (n = 38) limits comparisons; however our Middle and Late stage HD costs are considerably higher than these reference costs, with excesses of $18,526 and $32,304, respectively.
There are some limitations inherent to retrospective database analyses, as well as to our analysis of HD patients and our algorithm for assigning HD stage. We are unable to track patients who move from commercial to Medicaid insurance due to database limitations. Our algorithm classified patients into a single stage, based on the severity of disease markers present, potentially allowing for misclassification of some costs. For patients who transitioned between stages within their time enrolled in the database, our algorithm classified these patients (and all their costs) into the more advanced stage, potentially under-estimating the costs of the more advanced stage. However, because patients progress gradually through disease stages, we were less concerned about this, and, furthermore, thought it impossible to identify the exact point of transition. We required a 6 months minimum of follow-up time in order to maximize patient sample for patients with less than 12 months continuous enrollment post-index, as well as to be able to utilize the entire available time for patients with greater than 12 months post-index. While the annualized cost method may both over- and under-estimate the actual cost, this likely averages out. We miss an important aspect of the overall burden of HD by not capturing indirect costs (absenteeism, under-employment, informal caregiving, etc.). Also, there is a possibility that HD patients who have not received a diagnosis code of 333.4 due to their physicians’ respect for their privacy have not been captured in our cohorts. However, this issue is more problematic for patients in Early stage, where fear of job loss or insurance denial may be a concern, while for later stages, use of the diagnosis code of 333.4 for insurance claims is likely necessary due to reimbursement needs. Our sample includes 4.6% of patients who were younger than 18. Juvenile HD has a different pattern of disease progression and symptoms as compared to adult onset HDCitation22. Another limitation is that the small number of patients in our Medicaid Early stage limits comparisons and identification of trends by stage. A final limitation is that commercial insurance does not traditionally cover long-term care/nursing home. It is possible that we do not capture all long-term care/nursing home-related costs for commercial patients and lack visibility into any out-of-pocket or supplemental LTC insurance purchased. Additionally this limits cost comparisons between commercial and Medicaid Late stage patients.
Conclusions
In conclusion, our retrospective database analysis of HD commercial and Medicaid patients uncovered a substantial economic burden of HD, which increased greatly by stage. The mean total annualized cost per patient ranged from $4947 (SD = $6040) to $22,582 (SD = $39,028) with median $3397–$12,618 for commercial patients, and $3257 (SD = $5670) to $37,495 (SD = $27,111) with median $1688–$35,925 for Medicaid patients. The vast majority of Late stage Medicaid patients received nursing home care, and were in a nursing home for a longer duration than Late stage commercial patients. Late stage Medicaid costs were much higher than their commercial counterparts, and the majority of Late stage Medicaid costs were associated with nursing home care, suggesting further disease progression.
Given the unmet treatment needs in HD, and the high costs of HD disease progression, there is a great need for an effective treatment. Delaying or preventing disease progression in HD would result in considerable cost savings and a disease modifying therapy which would stabilize a patient in Early stage could potentially save annual total costs of up to ∼$17,500 and $34,000 per patient for commercial and Medicaid populations, respectively (Late stage costs minus Early stage costs). A forthcoming study will incorporate these direct cost estimates along with indirect cost estimates, obtained through patient and caregiver surveys, into a comprehensive model of the burden of HD at the national US level.
Given the limited understanding of the costs of HD, as well as the association between costs and HD stage, it is our hope that quantifying the economic consequences of HD, which increase with disease progression, will raise awareness of the unmet need of HD among clinical and managed care decision-makers, as well as highlight the need for continued research into therapies which may effectively delay or prevent disease progression.
Transparency
Declaration of funding
This study was funded by the CHDI Foundation, Princeton, NJ.
Declaration of financial/other relationships
JHW and JG have disclosed that they are employees of CHDI Foundation. KEA and DL have disclosed that they are consultants to CHDI. VD, MD, and WCL have disclosed that they are employees of IMS Health Inc., a company that received funding from CHDI to help conduct this study. JME Peer Reviewers on this manuscript have no relevant financial relationships to disclose.
References
- Novak MJ, Tabrizi SJ. Huntington’s disease. BMJ 2010;340:c3109
- Spinney L. Uncovering the true prevalence of Huntington's disease. Lancet Neurol 2010;9:760-1
- National Institute of Neurological Disorders and Stroke. What is Huntington’s Disease? National Institutes of Heath, Bethesda MD, 2012. http://www.ninds.nih.gov/disorders/huntington/huntington.htm. Accessed March 6, 2012
- Cardoso F. Huntington disease and other choreas. Neurol Clin 2009;27:719-36
- Roos RAC. Huntington’s disease: a clinical review. Orphanet J Rare Dis 2010;5:40
- Shoulson IF, Fahn S. Huntington disease: clinical care and evaluation. Neurology 1979;29:1-3
- Rosas HD, Reuter M, Doros G, et al. A tale of two factors: what determines the rate of progression in Huntington's disease? A longitudinal MRI study. Mov Disord 2011;26:1691-7
- Mayo Clinic. Huntington’s disease. Treatment and drugs. Mayo Foundation for Medical Education and Research (MFMER), Rochester, MN, 2011. http://www.mayoclinic.com/health/huntingtons-disease/DS00401/DSECTION=treatments%2Dand%2Ddrugs. Accessed March 6, 2012
- Murman DL, Chen Q, Colucci PM, et al. Comparison of healthcare utilization and direct costs in three degenerative dementias. Am J Geriatr Psychiatry 2002;10:328-36
- McCabe MP, O'Connor EJ. A longitudinal study of economic pressure among people living with a progressive neurological illness. Chronic Illn 2009;5:177-83
- Dubinsky RM. No going home for hospitalized Huntington's disease patients. Mov Disord 2005;20:1316-22
- Thomson Reuters MarketScan Research Database. Thomson Reuters Healthcare, Inc., Ann Arbor, MI, 2012 http://thomsonreuters.com/products_services/healthcare/healthcare_products/pharmaceuticals/epidemiology_res/mktscan_res_db. Accessed on January 12, 2012
- Buck CJ. ICD-9-CM 2011 Professional Edition for Physicians, Vols 1&2: Compact: 1st edn. American Medical Association, Chicago, IL. 2010
- Bureau of Labor Statistics. Consumer Price Index. Washington, DC, 2011. http://www.bls.gov/cpi. Accessed on October 1, 2011
- Costa N, Derumeaux H, Rapp T, et al. Methodological considerations in cost of illness studies on Alzheimer disease. Health Econ Rev 2012;2:18
- Joyce AT, Zhao Y, Bowman L, et al. Burden of illness among commercially insured patients with Alzheimer’s disease. Dement 2007;3:204-10
- Prescott JD, Factor S, Pill M, et al. Descriptive analysis of the direct medical costs of multiple sclerosis in 2004 using administrative claims in a large nationwide database. J Manag Care Pharm 2007;13:44-52
- Huse DM, Schulman K, Orsini L, et al. Burden of illness in Parkinson's disease. Mov Disord 2005;20:1449-54
- Fillit H, Hill JW, Futterman R. Health care utilization and costs of Alzheimer's disease: the role of co-morbid conditions, disease stage, and pharmacotherapy. Fam Med 2002;34:528-35
- Gilden DM, Kubisiak J, Zbrozek AS. The economic burden of Medicare-eligible patients by multiple sclerosis type. Value Health 2011;14:61-9
- Dworkin RH, White R, O'Connor AB, et al. Health care expenditure burden of persisting herpes zoster pain. Pain Med 2008;9:348-53
- van Dijk JG, van der Velde EA, Roos RA, et al. Juvenile Huntington Disease. Hum Genet 1986;73:235-9