Abstract
Objective:
To examine the daily functioning, diabetes management, and economic burden of non-severe nocturnal hypoglycemic events (NSNHEs) in Canada and differences in impacts by diabetes type.
Research design and methods:
A 20-min web-based survey, with items derived from the literature, expert and patient interviews, assessing the impact of NSNHEs, was administered to patients with self-reported diabetes aged ≥18 having an NSNHE in the past month.
Results:
Two thousand, two hundred and seventy-nine Canadian persons with diabetes were screened with 200 respondents meeting criteria and included in the analysis sample. Out of 87 working respondents, 15 reported on average 3.5 h of lost work (absenteeism). The reduction in work productivity (presenteeism) reported was comparable to the impact of arthritis. Other functional impacts included sleep and daily activities. Additionally, respondents’ increased their usual blood sugar monitoring practice, on average, 4.2 (SD = 7.5) extra tests were conducted in the week following the event and reduced their insulin over the following 4.8 days. Increased healthcare utilization was also reported. Increased costs as a result of NSNHE for lost work productivity, increased diabetes management, and resource utilization was CAD 70.67 per person per year in this sample. Limitations of the study include the biases which are associated with a web-based survey and self-reported data.
Conclusions:
NSNHEs have serious consequences for patients and diabetes management practices. Greater attention to treatments which reduce NSNHEs can have a major impact on improving functioning while reducing the economic burden of diabetes.
Introduction
Non-severe hypoglycemic events are defined as hypoglycemic events in which the person experiencing the symptoms does not require the assistance of another personCitation1. They have been shown to occur in over one-third (36%) of persons with diabetesCitation2 with frequency of events as often as several times a weekCitation3. These events can occur at any time of day or night while patients are at rest or engaged in activitiesCitation2–4 and represent a major challenge for both patients and clinicians, interfere with optimal long-term diabetes control, and contribute to excess morbidity and mortalityCitation5–7. Additionally, non-severe hypoglycemia has been shown to have an economic burden for patients, employers, and healthcare payer systemsCitation8, increased blood glucose (BG) monitoring, healthcare resource utilization, and patient out-of-pocket expensesCitation8–10.
Recent studies have suggested that the impacts that non-severe hypoglycemic events have on patients’ lives and diabetes management may be different for type 1 vs type 2 patientsCitation3,Citation4,Citation6. The frequency of mild-to-moderate events has been found to be significantly greater (p < 0.05) for type 1 than type 2 patientsCitation6,Citation11. The duration of nocturnal events is longer for type 2 (1.3 h) than type 1 (1.0 h), and recovery time following an NSNHE (non-severe nocturnal hypoglycemic event) was longer for type 2 (18.9 h) vs type 1 (13.9 h)Citation3. Additionally, following an event, fear of future hypoglycemia was greater for type 1 (37.8%) than type 2 (29.9%) patientsCitation6. Further, more type 2 patients (8% T1 vs 15% of T2) mentioned the mild or moderate hypoglycemic event to their doctor at their next doctor visitCitation6, and that type 1 patients more often modify their insulin dose after an event (74.1% of the time in T1 vs 43.3% in T2, p < 0.001)Citation6.
When examining the differences between the economic impacts of non-severe hypoglycemic events, type 2 patients missed school, work, or activities more often (6.7% T1 vs 10.3% T2), and have greater lost work time the day after an event (9.3% T2 vs 1.6% for T1, p < 0.01)Citation6. However, the annual out-of-pocket treatment costs for minor hypoglycemia were slightly higher for patients with type 1 diabetes (CAD 122.08 vs insulin treated type 2 patients, CAD 70.06)Citation10.
Literature specifically examining the impacts of non-severe nocturnal hypoglycemic events, or those events which occur while someone is sleeping, is limited although NSNHEs have been shown to have a greater impact than daytime events on lost work productivity due to both absenteeism as well as presenteeismCitation8. Additionally, night-time events disrupt both sleep quality and quantity resulting in impaired functioning and well-being the following dayCitation9. Type 2 patients also have been found to require significantly more time than type 1 patients to recognize and respond to an NSNHE (1.5 vs 1.1 h) and decreased their normal insulin dose less than type 1 patients (25.7% T1 vs. 18.5% T2, p = 0.006) after an NSNHE. NSNHEs were also associated with a higher proportion of type 2 patients contacting a healthcare professional (18.6% T1, 27.8% T2, p < 0.001), although both type 1 and type 2 patients reported similar rates of not being able to return to sleep at night and tiredness on the following day. Of the respondents working for pay, type 2 patients reported significantly greater absenteeism from work or missing a meeting or work appointment or not finishing a task on time after an NSNHECitation3.
Although the incidence of hypoglycemic events may be lower for patients on orals than on insulinCitation12, studies have shown that rates may be as high as 38% for patients on oral agents confirmed by BG readingCitation13 and between 57.2–74% of T2 patients on oral treatments showed signs/symptoms of hypoglycemiaCitation13,Citation14. The impact of NSNHEs on work productivity has been shown to be significantly lower (better) for patients on insulin than those on oral treatment (p < 0.001)Citation15. Further, patients on insulin were shown to have a higher percentage of work absence (66.7%) than those on oral treatment (33.3%) due to an NSNHE (p = 0.076). The total yearly cost of lost work productivity was estimated to be higher for those on insulin, $520.4 (insulin = $452.7, oral = $586.0, p = 0.277) per working person. Additionally, subjects on oral treatments only had a significantly higher rate of contacting a primary care doctor or clinic than those on insulin (22.3% vs 12.3%, respectively, p < 0.01) as a result of an NSNHE, and subjects on insulin reported fewer trips/falls than subjects on orals only (6.1% vs 9.2%, p < 0.05).
Thus, previous research has begun to suggest that NSNHEs are consequential contributors to increasing healthcare costs as well as the overall burden on disease management and functioning of diabetes patients. Further, although these events may not be as common in type 2 patients or for those on orals, the evidence suggests that non-severe events are also a concern to type 1 patients or those on insulin.
The purpose of this study is to further explore the burden of NSNHEs in terms of daily functioning, diabetes management, and economic impacts on patients in Canada as well as examine the differences in impacts between type 1 and type 2 diabetes patients. This information is critical data which can be instrumental in helping to manage and contain costs associated with these events and reduce the overall cost of care while at the same time improving patient functioning and well-being.
Patients and methods
Survey development and conduct
A survey assessing the impact of non-severe nocturnal hypoglycemic events (NSNHEs) was developed based on the literature, expert input, and interviews with 78 persons with diabetes in nine focus groups in four countries (US, UK, Germany, and France) who recently had experienced an NSNHE. The survey items were developed based on a qualitative analysis of the expert input and the persons’ with diabetes interviews, and cognitively debriefed and pilot tested in English in nine persons who met the same eligibility criteria as the focus groups. These steps were conducted to ensure content validity (relevant questions) and to ensure that the questions had face-validity with the respondents (e.g., no unfamiliar/strange words or concepts)Citation9. The final questionnaire was translated into all relevant languages using a forward and backward translation process. The survey was administered via a secure internet server in the US, UK, Germany, Canada, France, Italy, Spain, Netherlands, and SwedenCitation16. This study was reviewed and approved by Independent Review Consulting (# 09033-01), and this paper presents the results for the Canadian sample.
NSNHEs were defined for the respondent as:
night-time hypoglycemic episode that happened while you were sleeping and did not require medical attention (such as needing to call an ambulance, go to the emergency room/hospital) or did not require help from anyone else to manage the hypo. You knew that you were having this hypoglycemic episode because you had symptoms like sweating and/or confusion or perhaps you experienced no symptoms, but noted the hypoglycemic episode when measuring your blood sugar.
Respondents were asked questions regarding reasons for the event, length of time of the event, impact on productivity, daily functioning, and well-being. Survey respondents were asked to recall NSNHEs which occurred during the previous month; they were not asked to report nightly hypos on a routine basis. The survey took ∼20 min to complete and respondents were remunerated US $10.00 or less depending on the data source. The survey had several real-time validation steps (e.g. plausible min–max input values) and skip-patterns depending on the respondents reply. Prior to database-release, additional cross-checks were performed.
Sample
To be eligible to complete the survey, the respondent had to have a self-reported diagnosis of diabetes and experienced at least one NSNHE in the past month, be over 18 years of age, and be able to read the predominant language of the country they were living in. The screener did not ask respondents if their NSNHE had impacted them in any way so as to ensure that those with ‘non-problematic events’ were as likely to complete the survey as those with ‘problematic events’. In order to ensure the generalizability of the results from the panel, the panel structure and recruitment used the following strategies: the panel used for the survey was multi-sourced; panelists were mainly recruited online via a wide range of permission e-mail recruitment, affiliate networks, and website advertising, avoiding potential bias associated with single source recruitment methodology. Patients were recruited from more than 100 websites as well as from face-to-face and telephone surveys where appropriate to include members who were not frequent online users. Additionally, the panel was used for research only; panelists were not exposed to third party advertising or direct marketing campaigns, nor were their personal data sold to third parties. The panel was also frequently refreshed to ensure that the panel was dynamic in nature and reflected any changes in the online population that might be occurring. Lastly the incentive was very low to help ensure that there was not undue incentive to participate in the panel.
The selection process used a sampling frame in a pre-existing panel of persons with self-reported type 1 or type 2 diabetes. All respondents went through a healthcare profiler (screening questions) to ensure that their diabetes had been diagnosed by a physician and that a relevant treatment was initiated. A stratified sampling procedure was employed using invitation selection criteria to account for disproportional response rates between stratification categories. Stratification variables were age (18–29 years, 30–49 years, 50–64 years, and ≥65 years), diabetes type (type 1 diabetes and type 2 diabetes), gender, and working status (working and non-working).
Results are presented via frequencies or descriptives (means and standard deviations) with differences in diabetes type explored using analysis of variance (ANOVA) for continuous variables and Pearson chi-square for proportions. For results that include cost comparisons, the human capital approach using average wages to estimate productivity was used. To estimate input for the human capital method, an average of 35.7 working hours per week (corresponding to the self-reported working hours in ) with an estimated 47 working weeks per year (a total of 1678 working hours per year). The 2011 gross domestic product per capitaCitation17 was used as an estimate for annual income. An estimated average income of CAD 23.53/hCitation17 was used to estimate the value of the lost productivity. The estimated productivity loss per NSNHE because of absenteeism was calculated based on the proportion of persons reporting missed work multiplied with the hourly income multiplied with the hours missed. The costs for blood glucose testing strips were based on each strip being CAD 0.799, computed at CAD 0.729 for the strip plus a pharmacy fee of CAD 0.070Citation18.
Table 1. Sample demographic characteristics.
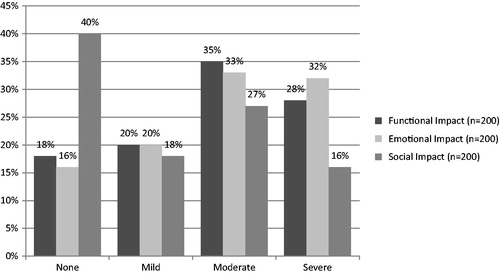
Analyses were conducted to characterize and assess the impact of the respondents last NSNHE on diabetes management, work productivity, and economic burden. For questions with a 0–10 response scale assessing the impact of events on functioning, where 0 is no impact and 10 being extremely impacted, scores were presented as means (with standard deviations) and also categorized as none (0), mild (1–2), moderate (3–6), and severe (7–10).
Presenteeism was assessed by the Endicott Work Productivity Scale (EWPS)Citation19 as well as a patient reported Likert scale assessment. The EWPS is a 25-item measure assessing the impact of a disease/event on a person’s ability to perform their work functions due to behaviors and subjective feelings or attitudes (e.g., ability to concentrate or impatience or annoyance with others at work). For the 0–10 scale rating ‘how much this hypo impacted productivity at work’, where 0 represented ‘My hypo did not impact my productivity at work at all’ and 10 represented ‘My hypo had an extremely negative impact on my productivity at work’, mirroring the standard interpretations of Cohen’s effect sizeCitation20 classifications of mild, moderate, and severe. Thus, mean scores were collapsed to ‘no impact’ (score 0), ‘a little impact’ (scores 1–2), ‘moderate impact’ (3–6), and ‘high impact’ (scores 7–10).
Results
The sample
A total of 2279 Canadian respondents with self-reported diabetes were screened. Of these, 239 respondents reported an NSNHE during the previous month and were eligible for the study (10.5% prevalence rate). Of those eligible, 200 completed the survey for a response rate of 83.7%. The mean diabetes duration was 14.4 (SD = 10.7) years. As per the stratified inclusion criteria, 150 (75.0%) of the sample had type 2 diabetes. The majority of the sample used insulin (69.5%) with the remainder on oral treatments only. Eighty-seven of the respondents (43.5%) reported working for pay. Respondents reported approximately two additional co-morbid conditions along with diabetes (range = 0–9).
The majority of respondents (51.0%) reported experiencing an NSNHE with regularity. Of these, 35% experienced an NSNHE at least several times a month, 8.5% about once a week, 7.0% not daily but more than 1 a week, and 0.5% daily. The remainder of the sample (49.0%) reported having NSNHEs once a month to very rarely. The overall recall period for when the event occurred was short, with 73.5% (n = 147) reported having an NSNHE within the last 2 weeks.
There were significant differences between diabetes type for age (T2 older, p < 0.001), duration of diabetes (T1 longer, p < 0.001), work for pay (T1 worked more, p < 0.01), and frequency of NSNHE (T1 more frequent, once a month or more often, p < 0.01). Respondents on insulin and oral treatments showed significant difference with regard to duration (years) of diabetes (insulin longer, p < 0.01) and number of medical complications (insulin greater number, p < 0.01). There were no significant differences in frequency of events between patients on insulin compared to oral treatments, gender, or for those with more co-morbid conditions.
Characteristics of the last NSNHE
The majority of respondents (85.0%) were aware that they were experiencing their NSNHE because they had hypoglycemic symptoms (self-identified or noticed by someone else) and more than half of events (60.0%) were also confirmed by blood glucose tests. Of note, 11.5% of respondents did not wake up during the event, but believed they had experienced a nocturnal hypoglycemic event based on how they felt or their blood glucose reading upon awakening the next day.
It took an average of 5.2 min for respondents to realize they were having an NSNHE (after waking up) and another 4.4 min to do something about it (monitoring blood sugar, going to get something to eat or drink, and then eating or drinking it), then 17.1 min for the acute hypoglycemic symptoms to go away after eating or drinking something. Thus, the acute period of experiencing and managing the event took, on average, approximately half an hour. During the NSNHE, 3.0% (n = 6) of the respondents reported either tripping or falling.
It took substantially more time on average (2.9 h or 171 min) before respondents felt like they were functioning again at their usual or normal levels (see ). Thus, the recovery phase for the event impacted the patient considerably longer than the acute phase.
Figure 1. Recovery time from an event. A = After you woke up that night, how long did it take to realize you were having a hypo before you did something about it? B = After you woke up that night, how long did it take after realization to do something about the hypo, including monitoring your blood sugar, going to get something to eat or drink, and then eating or drinking it? C = After you woke up that night, how long did it take for all of your acute hypoglycemic symptoms to go away after you had something to eat or drink? D = After you woke up that night, how long did it take before you felt like you were functioning again at your usual or normal level after you had something to eat or drink?
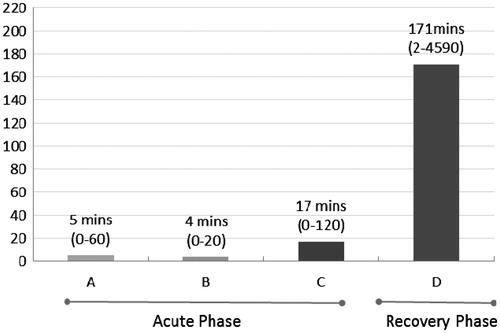
There were no significant differences with regard to diabetes type, gender, or co-morbid conditions for the average length of time either the acute or recovery phase lasted or the total time it took for respondents until they felt like they were functioning again at their normal level. With respect to acute and recovery times, respondents on oral treatment took longer to realize they were having an NSNHE vs insulin users (7.2 vs 4.3, p < 0.05).
Impact of NSNHE on diabetes management
Compared to respondents’ usual blood sugar monitoring practice, on average, 4.2 (SD = 7.5) extra tests were conducted in the week following the event. Additionally, 23.7% (n = 33) of respondents reduced their insulin dose following the event and reported keeping it lower than normal for up to 4.8 days.
There was an increase in health services utilization reported, with 14.5% (n = 29) of the respondents contacting their primary care doctor, hospital/diabetes clinic, or another healthcare professional (by telephone, in-person visit, or e-mail) as a result of having an NSNHE. No significant differences were found between diabetes types, gender, oral compared to insulin users, or number of co-morbid conditions for number of extra blood sugar tests conducted, length of time insulin use was reduced, or health services utilization ().
Table 2. Impact of NSNHE on diabetes management.
Impact of NSNHE on work productivity: absenteeism and presenteeism
Of working respondents, 17.2% (n = 15) reported missing work time, 4.6% (n = 4) missed a full day, while 12.6% (n = 11) missed a partial day (either going late to work the next day or leaving early) due to the NSNHE. For those missing work, the average working time lost was 3.5 (SD = 3.3) hours. A third of these (33.3%) reported that the NSNHE had a high impact on productivity at work the following day, 33.3% reported moderate impact, 17.2% reported a little impact, and 16.1% reported no impact of the NSNHE on their work productivity. Of those who worked the next day (n = 87), the impact of the previous night’s event was apparent, with 44.8% of respondents reporting they had trouble focusing or concentrating the next day at work, 24.1% not completing work tasks on time, and 18.4% needing to re-schedule their work day
Based on EWPS scores, the impact of the NSNHE on presenteeism had a mean score of 24.1 (SD = 21.6), which is significantly higher than groups defined as normal controls in two recent studies (ranging from mean = 3.54Citation21 and mean = 15.6 (SD = 11.7)–18.2 (SD = 10.7)Citation22), comparable to the score among patients with arthritis (mean = 21.5, SD = 14.3)Citation23, and lower than patients reporting psychiatric disorders (mean = 40.8, SD = 21.6)Citation24.
There were no significant differences for reported missed work time between diabetes type, oral vs insulin treatment, gender, or number of co-morbid conditions ().
Table 3. Impact of an NSNHE on work productivity.
Impact of NSNHE on daily dunctioning
Impact on sleep
Respondents reported a moderate impact (mean = 5.2 on 10-pt scale, with 10 being prevented from going back to sleep) of the NSNHE on their sleep the night of the event. For those who woke up due to the NSNHE (88.5%, n = 177), the average time it took people to fall back to sleep was 58.0 min, and 12.5% (n = 25) never went back to sleep, remaining awake for the remainder of the night. A small number of respondents (2.5%, n = 5) gave themselves some type of sleeping medication to help them go back to sleep.
On the night of the NSNHE, 52.5% (n = 105) of the respondents indicated having a bed partner who was woken up either intentionally (7.0%, n = 14) or unintentionally (18.5%, n = 37) due to the NSNHE. This suggests that these NSNHEs impact not only the person having the event, but also those they sleep with.
There were no significant differences between diabetes types for the impact of NSNHE on their sleep the night of the event, but the average time it took people to fall back to sleep was higher for type 2 than type 1 respondents (p < 0.036). There were no significant differences in sleep for oral compared to insulin treatment or gender.
Impact on next day functioning
It was reported by 82.0% (n = 164) of respondents that the NSNHE impacted their overall functioning the following day: 43.0% (n = 86) reported feeling emotionally low, 21.5% (n = 43) reported that they avoided driving or drove less, 47.5% (n = 95) found it difficult to concentrate, and 49.5% (n = 99) restricted their household chores or errands as well as 30.5% (n = 61) restricting social activities. The next day impact of poor sleep the previous night was evident in that 75.0% (n = 150) reported being tired or fatigued, 133 (66.5%) of respondents reported wanting to take a nap or rest the following day (42.0% of the 133 did take a nap), and 42.5% (n = 85) reported wanting to go to bed earlier than usual the following night, with 29.5% of these respondents actually going to bed earlier.
When asked how much their lives were impacted the day after their NSNHEs, moderate-to-severe impact was reported by 62.5% of respondents for their next day functioning, 64.5% for emotional functioning, and 43.0% for social functioning.
There were no significant differences between diabetes type, gender, or oral compared to insulin treatment for next day functioning, emotional functioning, and social functioning (). With regards to co-morbid conditions, there were no significant differences of the impact on next day functioning, and emotional functioning; however, respondents with no co-morbid conditions reported a significantly greater impact on social functioning than those with co-morbidities (p = 0.05).
Economic burden and costs of NSNHE
The economic burden of NSNHE was calculated for lost work time, changes in diabetes management, and resource utilization. Out of the 87 working respondents, 15 reported an average of 3.5 h of lost work time (absenteeism). This represents an average cost of lost work time for the working respondents of CAD 14.20 per event. The total yearly cost of lost work productivity due to working either a partial day or missing a full day of work for the working sample, based on the number of reported events, was estimated to be CAD 282.10.
The estimated yearly healthcare utilization cost due to diabetes management as a result of NSNHEs for increased BG monitoring, assuming CAD 0.799 cost per BG monitoring stripCitation18, was CAD 54.84 (SD = 107.30).
Cost comparison between diabetes type showed no significant differences for lost work time, changes in diabetes management, or resource utilization (). There were also no cost differences with regard to insulin compared to oral treatments, gender, or number of co-morbid conditions.
Table 4. Economic burden of NSNHEsa.
Discussion
This study has confirmed that NSNHEs are common in both type 1 and type 2 patients on insulin as well as for those taking only oral agents, occurring at least monthly in ∼10.5% of patients, and as found in previous research, are experienced more frequently in type 1 patientsCitation8. However, in contrast to previous research which identified significant differences between diabetes type in impact of events on diabetes management, daily functioning, work productivity, and costsCitation8, this study found no significant differences in Canada between diabetes type in regard to these impacts (with the exception of time to get back to sleep after an event). Most importantly, this evidence should further dispel the myth that non-severe events are only a concern for type 1 patients or only for patients on insulin.
The longer term impacts of these events, such as poor concentration, lasts far longer than the immediate experience of the acute symptoms of the NSNHE (shaking, sweats, etc.) and can impact next day functioning at work as well as daily functioning and well-being. These findings are consistent with previous findings showing that the impact of these events often continues into the next dayCitation3. It is of note that the impact of NSNHEs on work productivity (presenteeism) is similar to that of arthritis, a major debilitating disease with major impact on patient functioning and well-being as well as economic costs of careCitation25–28. Clearly, these events are not ‘minor’ or ‘non-severe’, and labeling these events as such is a serious misnomer and may contribute to the lack of attention or appreciation of the importance of NSNHEs.
The total economic burden of NSNHEs must include not only lost work productivity, but also costs incurred for increased diabetes management and healthcare resource utilization. The total yearly cost for all reasons as a result of NSNHEs for all participants in this study is estimated to be CAD 15,193 (CAD 70.7 per person). This figure is less than reported in previous research which found an average annual cost for all NSHEs (both daytime and nighttime events) of between CAD 2012.74 and CAD 3099.76 per patientCitation8. This may be due to the lower prevalence of events in this Canadian sample than the previous study (10.5% vs 13.2%)Citation8. However, given that there are ∼3 million persons with diabetes in CanadaCitation29 and assuming, as found here, that ∼10.5% of these individuals experience on average 20 NSNHEs in a year, the annual economic burden of these events in Canada would be substantial.
This survey also identified a previously undiscussed economic impact of NSNHEs, namely falls due to the event. Falls and potential subsequent visits to healthcare providers due to falls are not only frightening to patients but also represent an additional healthcare cost. Given that the elderly are more prone to fallsCitation30, that the prevalence of diabetes increases with ageCitation31, and that there is a 47% increased risk of recurrent fallsCitation32, one can assume that the economic burden for this population is even greater than for younger persons with diabetes. Further research is needed to better understand the prevalence and economic implications for these falls and injuries as a consequence of NSNHEs.
Further, these costs may be an under-estimation for several reasons. First, the full extent of the economic burden of these NSNHEs on work productivity does not include the impact of the NSNHE on the ability to be productive at work (presenteeism) and the cost of reduced focus or concentration at work. Second, the increased healthcare resource utilization costs due to additional contacts with healthcare providers (additional phone calls, visits or questions to healthcare providers reported in this survey by 14.5% of respondents) could not be calculated, as the type and length for each contact is unknown. Third, the calculations for the annual costs of these events in Canada only assumed that 10.5% of people with diabetes would have an event. However, this percentage is based on only those who have had an event in the previous month of the survey, and does not include costs for all patients who have less than one event a month. Fourth, the total economic burden as a result of NSNHE should also include the additional out-of-pocket costs of the individual patient to manage these eventsCitation10. This was not assessed in this study, although previous studies have found these costs to be considerable; the average dollar amount spent per year per person to manage non-severe hypoglycemic events was $25/month for purchases such as food more substantial than just a sugar packet or juiceCitation8. Finally, in response to a minor hypogylcemic event, these patients were found to reduce their insulin dosage. As found in other research, insulin reduction due to NSHE is common and reduction in insulin use may in fact sometimes also precede an event in an attempt to avoid a future eventCitation2. These alterations to insulin regimes may negatively influence gylcemic control over time, leading to complications and increased cost of care not considered in this study.
Several limitations with this study should be mentioned. First, accuracy of reporting, as with any survey, is a consideration as recall bias may have influenced findings. However, recall of episodes of NSHEs up to a week can be considered relatively accurateCitation33 and recall of longer durations was considered to be accurate as reported by focus group participants in the groups conducted to generate items for this survey. The recall period for most of the sample (73.5%) was within the last 2 weeks and no recall period was longer than 1 month. The fact that this study collected data via an internet-based survey may also introduce a selection bias in the respondents who are able to participate (i.e., only literate respondents with access to a computer). However, the proportion of internet users in Canada based on total population is 78.6%Citation34, which should mitigate the impact of this bias. Also, accuracy may be impacted by any incentives given the respondents for completion of the survey, although in this case the amount of the incentive was minimal and should not have affected responses or decisions to participate in the study. Lastly, given the panel nature of the survey it was not possible to have a physician confirmed diagnosis. However, it was not known to the patients who completed the screener beforehand that only those with diabetes would be administered the survey. In the screener, the subjects were provided with several medical conditions and asked to check which they had been diagnosed with by a physician. Only those who checked diabetes, among the multiple possibilities, were invited to complete the full survey. It is possible that some patients did misrepresent their diagnosis; however, it is unlikely that this group was large enough to influence findings. Lastly, the effect of specific types of treatment regime as well as level of education the patient has received by their healthcare provider regarding NSNHEs, was not examined in this study. Further examination of these influences would be of interest.
Conclusions
This study strongly suggests that NSNHEs are significant events for patients, regardless of diabetes type, and represent an important economic burden in terms of both lost work productivity and increased healthcare resource utilization. These events should not be considered ‘minor’ or ‘non-severe’, and incorporating a discussion of these events and optimal corrective action strategies into all diabetes management treatment plans should facilitate reducing the economic burden of NSNHEs.
Transparency
Declaration of funding
This study was funded by Novo Nordisk A/S.
Declaration of financial/other relationships
MB and DB are consultants/paid advisors to Novo Nordisk. MW and DG are employees of Novo Nordisk.
Previous presentation
Portions of this study were previously presented at the 15th Annual Canadian Diabetes Association conference in Vancouver, BC 2012.
References
- Canadian Diabetes Association Clinical Practice Guidelines Expert Committee. Hypoglycemia. Can J Diabetes 2008;32:S62-4
- Brod M, Christensen T, Bushnell DM. The impact of non-severe hypoglycemic events on daytime function and diabetes management among adults with type 1 and type 2 diabetes. J Med Econ 2012;15:869-77
- Brod M, Rana A, Barnett AH. Impact of self-treated hypoglycaemia in type 2 diabetes: a multinational survey in patients and physicians. Curr Med Res Opin 2012;28:1947-58
- Brod M, Christensen T, Bushnell DM. Impact of nocturnal hypoglycemic events on diabetes management, sleep quality, and next-day function: results from a four-country survey. J Med Econ 2012;15:77-86
- Unger J. Uncovering undetected hypoglycemic events. Diabetes Metab Syndr Obes 2012;5:57-74
- Leiter LA, Yale JF, Chiasson JL, et al. Assessment of the impact of fear of hypoglycemic episodes on glycemic and hypoglycemia management. Can J Diabetes 2005;29:186-92
- Gerstein HC, Miller ME, Genuth S, et al. Long-term effects of intensive glucose lowering on cardiovascular outcomes. N Engl J Med 2011;364:818-28
- Brod M, Christensen T, Thomsen TL, et al. The impact of non-severe hypoglycemic events on work productivity and diabetes management. Value Health 2011;14:665-71
- Brod M, Pohlman B, Wolden M, et al. Non-severe nocturnal hypoglycemic events: experience and impacts on patient functioning and well-being. Qual Life Res 2012;22:997-1004
- Harris SB, Leiter LA, Yale JF, et al. Out-of-pocket costs of managing hyperglycemia and hypoglycemia in patients with type 1 diabetes and insulin-treated type 2 diabetes. Can J Diabetes 2007;31:25-33
- Willis WD, Diago-Cabezudo JI, Madec-Hily A, et al. Medical resource use, disturbance of daily life and burden of hypoglycemia in insulin-treated patients with diabetes: results from a European online survey. Expert Rev Pharmacoecon Outcomes Res 2013;13:123-30
- UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998;352:837-53
- Garber A, Klein E, Bruce S, et al. Metformin-glibenclamide versus metformin plus rosiglitazone in patients with type 2 diabetes inadequately controlled on metformin monotherapy. Diabetes Obes Metab 2006;8:156-63
- Pollack MF, Purayidathil FW, Bolge SC, et al. Patient-reported tolerability issues with oral antidiabetic agents: associations with adherence; treatment satisfaction and health-related quality of life. Diabetes Res Clin Pract 2010;87:204-10
- Brod M, Wolden M, Christensen T, et al. Understanding the economic burden of non-severe nocturnal hypoglycemic events: impact on work productivity, disease management, and resource utilization. Value Health In press
- Brod M, Wolden M, Christensen T, et al. A Nine-Country Study of the burden of non-severe nocturnal hypoglycaemic events on diabetes management and daily function. Diabetes Obes Metab 2013;15:546-57
- Average hourly wages of employees by selected characteristics and profession, unadjusted data, by province (monthly), February 2012. CANISM tables 282-0069 and 282-0073. Statistics Canada. Ottawa, Ontario: Government of Canada, 2013. www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/labr69a-eng.htm. Accessed March 21, 2012
- Dolovich L, Dahl M. Utilization and expenditure on blood glucose test strips in Canada. Can J Diabetes 2010;34:34-40
- Endicott J, Nee J. Endicott Work Productivity Scale (EWPS): a new measure to assess treatment effects. Psychopharmacol Bull 1997;33:13-16
- Cohen J. A power primer. Psychol Bull 1992;112:155-9
- Roth T, Zammit G, Lankford A, et al. Nonrestorative sleep as a distinct component of insomnia. Sleep 2010;33:449-58
- Low D, Gramlich M, Engram BW. Self-paced exercise program for office workers: impact on productivity and health outcomes. AAOHN J 2007;55:99-105
- Beaton DE, Tang K, Gignac MA, et al. Reliability, validity, and responsiveness of five at-work productivity measures in patients with rheumatoid arthritis or osteoarthritis. Arthritis Care Res (Hoboken) 2010;62:28-37
- Linden M, Baron S, Muschalla B. Relationship between work-related attitudes, performance and capacities according to the ICF in patients with mental disorders. Psychopathology 2010;43:262-7
- da Silva JA, Phillips S, Buttgereit F. Impact of impaired morning function on the lives and well-being of patients with rheumatoid arthritis. Scand J Rheumatol Suppl 2011;125:6-11
- Gettings L. Psychological well-being in rheumatoid arthritis: a review of the literature. Musculoskeletal Care 2010;8:99-106
- Murphy L, Helmick CG. The impact of osteoarthritis in the United States: a population-health perspective. Am J Nurs 2012;112:S13-19
- Fautrel B, Verstappen SM, Boonen A. Economic consequences and potential benefits. Best Pract Res Clin Rheumatol 2011;25:607-24
- The prevalence and costs of diabetes. Toronto, ON: Canadian Diabetes Association, 2012. www.diabetes.ca/diabetes-and-you/what/prevalence/. Accessed December 19, 2012
- Older Adult Falls & Statistics. Atlanta, GA: Centers for Disease Control and Prevention, 2012. www.cdc.gov/homeandrecreationalsafety/Falls/data.html. Accessed September 17, 2012
- The Harsh Reality - Diabetes is a Global Pandemic. Toronto, ON: Canadian Diabetes Association, 2012. www.diabetes.ca/diabetes-and-you/living/harsh-reality/. Accessed December 19, 2012
- Pijpers E, Ferreira I, de Jongh RT, et al. Older individuals with diabetes have an increased risk of recurrent falls: analysis of potential mediating factors: the Longitudinal Ageing Study Amsterdam. Age Ageing 2012;41:358-65
- Pramming S, Thorsteinsson B, Bendtson I, et al. Symptomatic hypoglycaemia in 411 type 1 diabetic patients. Diabet Med 1991;8:217-22
- Canada. The World Factbook. Washington, DC: US Central Intelligence Agency, 2012. www.cia.gov/library/publications/the-world-factbook/". Accessed July 30, 2012