Abstract
Objective:
To assess the economic impact of initial and repeat hospitalizations associated with acute coronary syndrome (ACS) over 1 year (2009).
Design and methods:
National- and state-level data on length of stay (LOS) and related charges for ACS-associated hospital admissions were assessed using two Healthcare Utilization Project databases. The first, the Nationwide Inpatient Sample (NIS), provided clinical and resource use information from ∼8 million hospital stays, representing a 20% stratified sample of ∼40 million annual hospital stays in the US in 2009. The second, the State Inpatient Databases, provided 100% of inpatient data from nine states that included both patient age and linked information on multiple patient admissions within the same calendar year. For patients with repeat admissions, the LOS, primary diagnosis, and total charges between the first and subsequent admissions were evaluated. All patients ≥18 years of age with at least one diagnosis of ACS, defined using the International Classification of Diseases, 9th Revision, were included (code 410.xx [except 410.x2], 411.1x and 411.8x). Variables evaluated for each discharge included demographics, cardiovascular events and procedures, LOS, discharge status, and total charges.
Results:
The NIS reported 1,437,735 discharges for ACS in 2009. In this dataset, mean LOS for an initial ACS event was 5.56 days. Patients >65 years of age had the highest numbers of admissions; this group also had the most comorbidities. Approximately 40% of ACS patients with data on repeat visits had more than one admission, >70% of these within 2 months of the primary discharge. Mean charges were $71,336 for the first admission and $53,290 for the second admission.
Conclusion:
Despite a variety of new therapies to prevent ACS, it remains a common condition. Better therapies are called for if the clinical and cost burden of ACS is to be alleviated.
Introduction
Acute coronary syndrome (ACS), a common clinical presentation of cardiovascular disease, encompasses a range of acute ischemic cardiac conditions, including unstable angina, ST-segment elevation myocardial infarction (STEMI) and non-STEMICitation1. In the US, the American Heart Association reported ∼1.2 million hospital discharges with a diagnosis of ACS in 2009Citation2. ACS is the leading cause of death in developed countriesCitation3. Despite improvements in treatment, rates of death and myocardial infarction (MI) remain high, as do repeat admissions for ACSCitation3. Healthcare costs for ACS are estimated at ∼$150 billion, ∼60% of which represent re-hospitalization costs after the initial dischargeCitation4.
This study was conducted to assess the economic impact of ACS-associated initial and repeat hospitalizations during 1 year using national- and state-level data on length of stay (LOS) and related charges for ACS-associated hospital admissions. The characteristics and demographics of this patient population were also examined.
Methods
Data sources
The Healthcare Cost and Utilization Project (HCUP) is a family of healthcare databases and related software tools sponsored by the Agency for Healthcare Research and Quality. HCUP databases bring together the data collection efforts of state and private data organizations, hospital associations, and the federal government to create a national information resource of patient-level inpatient healthcare data.
The HCUP reports clinical and non-clinical information on all patients, regardless of payer. Resource use information, such as would be included in a typical discharge abstract, is reported. Safeguards protect the privacy of patients, physicians, and hospitals; e.g., data that could identify individuals, directly or indirectly, are excluded.
The HCUP includes discharge data from two databases, the Nationwide Inpatient Sample (NIS) and the State Inpatient Databases (SID). Our study comprised separate analyses from each of these databases. The re-visit analysis, described below, was conducted on the SID dataset; all other analyses and data reported are based on the NIS data.
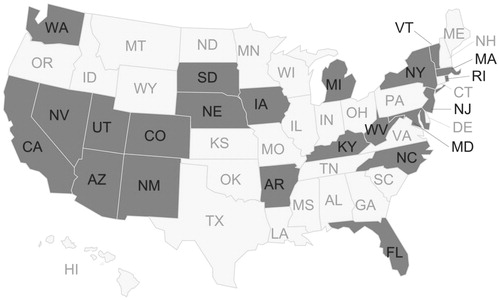
The NIS contains the largest collection of longitudinal hospital data in the US. The 2009 sample contained data from more than 1000 hospitals in 44 states. The ∼8 million hospital stays reported in the NIS represent a 20% stratified sample of the ∼40 million annual hospital stays in the US (). Clinical and resource use information is included for all patients covered by Medicare, Medicaid, and private insurance, as well as the uninsured. Safeguards protect the privacy of hospitals, physicians, and patients included in the NIS.
Figure 1. States participating in the Nationwide Inpatient Sample. Shading denotes different regions.
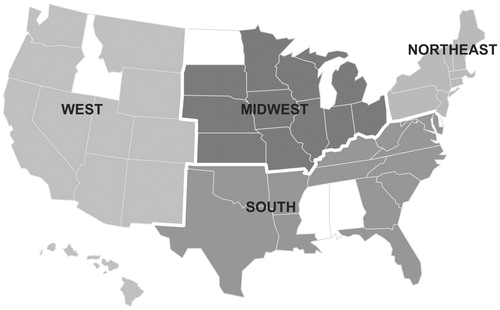
The SID, the second database, contains 100% of inpatient data from the 22–27 states that contribute to it each year, encompassing ∼90% of all US community hospital discharges (). These data are translated into a uniform format to facilitate multi-state comparisons. States that do not provide data on patients’ ages were not included in the analysis for this study. Some states that contribute to the SID include a unique identifier that links multiple visits for the same patient in a calendar year. In 2009, nine states (Arkansas, California, Florida, Hawaii, Iowa, Nebraska, New Mexico, North Carolina, and Utah) included both a patient age field and data on re-admissions and were included in the SID repeat admission analysis.
Study design for the NIS analysis
Using the HCUP ACS Impact Hospital Discharge Analysis Tool, a Web-based tool for summarizing ACS hospital discharge data, we analyzed data for all patients 18 years of age or older with at least one diagnosis of ACS according to the International Classification of Diseases, 9th Revision (ICD codes 410.xx [except 410.x2], 411.1x, and 411.8x). Variables evaluated for each discharge included patient demographics, cardiovascular events and procedures, LOS, discharge status, and total charges.
The data were weighted according to the HCUP survey methodology; detailed technical specifications are publicly available on the HCUP website (http://www.hcup-us.ahrq.gov/). Briefly, to obtain nationwide estimates, HCUP developed discharge weights using the American Hospital Association Annual Survey Database universe as the standard. These were developed separately for hospital- and discharge-level analyses. Hospital-level weights were developed to extrapolate NIS hospitals to the hospital universe. Similarly, discharge-level weights were developed to extrapolate NIS sample discharges to the discharge universe.
Study design for the SID repeat admission analysis
Using data from the nine visit-linked states in the SID that provided patient age information, we analyzed hospital re-admissions during calendar year 2009. For those patients with repeat admission, the LOS, primary diagnosis, and total charges between the first and subsequent admissions were evaluated.
Results
NIS analysis
There were ∼40 million hospital discharges in the US in 2009. The NIS included discharge data from a 20% sample of the national data. In this group, there were 1,367,942 discharges for ACS. The majority of patients discharged with a diagnosis of ACS were males (58%) and at least 65 years of age (59.6%). Among patients with ACS, the majority (67%) had an MI, 32.3% had unstable angina, and 5.8% had a stroke. Categories representing ACS events were not mutually exclusive. The most common co-morbidities across discharges included hypertension (52.5%), hyperlipidemia (45.8%), diabetes (35.3%), and congestive heart failure (29.6%). Cardiovascular events and common co-morbidities among ACS patients by sex and age group are shown in . Of patients with ACS, 6.1% died in the hospital. Additionally, 8.8% were discharged to a skilled nursing facility, 7.4% to another short-term hospital, and 9.1% to home healthcare. The mean LOS was 5.56 days (median = 3 days), with a mean charge of $63,578 (median = $41,816) per ACS discharge. Discharge status, LOS, and hospitalization charges for ACS patients by sex and age group are shown in .
Table 1. Type of event and common co-morbidities among patients with acute coronary syndrome.
Table 2. Discharge status, length of stay, and hospitalization charges for patients with acute coronary syndrome.
SID analysis
In the sub-set of 244,817 patients with a diagnosis of ACS from the nine states that provided visit-linked data, ∼40% had more than one admission; of these, 71.8% were re-admitted within the same or the following month. A breakdown of the sub-set of patients with multiple admissions for ACS by sex and age group is shown in . Categories representing numbers of admissions are mutually exclusive. In the sub-set of patients with visit-linked data, the top three primary diagnoses associated with the second admission were cardiovascular-related: acute MI, chronic ischemic heart disease, and heart failure.
Table 3. Patients with multiple admissions by number of admissions and time of repeat admission.
The median LOS did not differ between the first and subsequent admissions (5.6 vs 5.4 days). Mean charges, however, were greater for the first compared with the second admission ($71,336 vs $53,290, respectively). LOS and corresponding charges by sex, age, and primary diagnosis (cardiovascular-related or not cardiovascular-related) are shown in .
Table 4. Length of stay and charges for first and second hospital admission.
Discussion
The results of our study suggest that ACS-related hospital stays remain lengthy and costly, despite improvements in the management of ACS. Several recent studies have confirmed our findings that patients with ACS remain at increased risk for recurrent events, with attendant increases in the costs of patient care. Most of these studies have focused on particular agents or management strategies, such as percutaneous coronary angioplasty and coronary artery bypass graftCitation5–8. An exception is a 2011 retrospective study that found that, of the conditions that impose direct and indirect costs on employers, ACS is the most costly, with re-hospitalization representing a large portion of the costCitation9. Our study found a re-admission rate of almost 40%, with approximately three quarters of these re-admissions occurring within the first 2 months. This rate of re-admission of ACS patients represents a substantial cost burden to the healthcare system.
The death rate from ACS has declined in recent decadesCitation10. Nevertheless, 25% of men and 30% of women aged 65 years or older will die within a year of their first ACS eventCitation2. In a randomized clinical trial of patients with non-STEMI, rates of 30-day mortality or MI were 14%Citation11. In a non-selected population of patients with STEMI undergoing lytic therapy, 30-day mortality was at least 10%Citation12. In our analysis, ∼6% of patients died in the hospital from ACS-related causes.
Anti-platelet agents, including acetylsalicylic acid, thienopyridines such as clopidogrel and ticlopidine, and glycoprotein IIb/IIIa inhibitors, were recommended by the 2007 and 2008 American College of Cardiology/American Heart Association guidelines for the management of patients with non-STEMI and STEMI and are the standard of care in ACSCitation13,Citation14. However, despite improvements in long-term therapyCitation13, patients with ACS remain at high risk of repeat events, with risk rates for repeat events reported to be as high as 10%Citation15. Our data suggest that these rates may be significantly higher, specifically within the first 2 months post the previous event.
Because preventing recurrent ACS events and re-hospitalizations is so critical to the healthcare system, the National Quality Forum endorses measures designed to encourage collaboration among all stakeholders to reduce rates of unplanned readmissionsCitation16. Further, in October 2012, the Centers for Medicare and Medicaid Services began to fine hospitals for preventable re-admissions due to complications within 30 days of dischargeCitation17. However, preventing recurrent ACS events is particularly challenging, because the coagulation system remains hyperactive long after the initial acute eventCitation18,Citation19. Long-term dual anti-platelet therapy has proven to be highly effective; nevertheless, re-admission rates remain high, suggesting that a therapeutic plateau has been reachedCitation18. A more comprehensive approach to long-term therapy could include an anticoagulant that prevents thrombin generation, which persists long after an acute eventCitation19. Guidelines recognize the potential for dual pathway treatment for ACS patients that includes thrombin-directed therapy in patients with ACSCitation20. The individual risk profile of each patient should be considered when balancing the risks and benefits of the potential addition of anticoagulant treatment. Given the rate of re-hospitalization observed in ACS patients, further research into this is warranted.
The limitations of our study reflect limitations inherent in the two databases. Only variables available through the NIS and SID were included, and any inaccuracies in coding could not be detected or verified. Data were aggregated to the level of the inpatient stay; therefore, a patient could have been included in the dataset more than once. Data from Veterans Affairs and Department of Defense hospitals were not included. Clinical data were limited. While hospital charges were available, these may be higher than what was actually paid, and cost information was lacking. With respect to the SID, re-admissions data came from nine states and might not be generalizable to the entire US population. The linked database contained the admission month but not the date. Therefore, it was not possible to determine whether patients were re-admitted within 30 days (as opposed to within 60 days) of the first admission (e.g., if the first admission was in January 2009 and the second was in February 2009, a patient could have been admitted on January 30 and re-admitted on February 10; thus, re-admission would have been within 30 days. However, if a patient was admitted on January 1 and re-admitted on February 28, almost 60 days would have elapsed). Readmissions could have been significantly under-estimated if the second admission was to a different hospital than the first, or if the initial admission took place earlier or the re-admission took place later than the calendar year assessed. This is important, since, based on this analysis, most re-admissions happen within the first 60 days after discharge.
Conclusions
Findings from this national inpatient care database highlight the significant clinical and economic impact of ACS in the US. In this study, the number of repeat inpatient admissions was high, with approximately three quarters occurring within 60 days of the primary discharge. Better therapies/interventions are required, in view of this continued unmet need.
Transparency
Declaration of funding
This research was supported by Janssen Scientific Affairs, LLC.
Declaration of financial/other relationships
J.C.L., C.C., and S.H.M. are employees of Janssen Scientific Affairs and have received stock or stock options from Johnson and Johnson. K.D. was an employee of Janssen Scientific Affairs at the time this study was conducted. O.S. is an employee of TriCore, Inc, to whom Janssen Scientific Affairs provided consulting fees for work on the design of this study and analysis of the data. JME Peer Reviewers on this manuscript have no relevant or other relationships to disclose.
Acknowledgments
The authors would like to acknowledge Ruth Sussman, PhD, who provided editorial support with funding from Janssen Scientific Affairs, LLC.
Previous presentation
Portions of this article were presented as a poster at the ASHP Midyear Clinical Meeting and Exhibition; December 2–6, 2012; Las Vegas, NV.
References
- Grech ED, Ramsdale DR. Acute coronary syndrome: unstable angina and non-ST segment elevation myocardial infarction. BMJ 2003;326:1259-61
- Roger VL, Go AS, Lloyd-Jones DM, et al. Heart and Stroke Statistics–2012 update: a report from the American Heart Association. Circulation 2012;125:e2-220
- Bassand JP, Hamm CW, Ardissino D, et al. Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes. Eur Heart J 2007;28:1598-660
- Kolansky DM. Acute coronary syndromes: morbidity, mortality, and pharmacoeconomic burden. Am J Manag Care 2009;15:S36-41
- Meadows ES, Bae JP, Zagar A, et al. Rehospitalization following percutaneous coronary intervention for commercially insured patients with acute coronary syndrome: a retrospective analysis. BMC Res Notes 2012;5:342
- Bakhai A, Ferrieres J, Iniquez A, et al; APTOR Trial Investigators. Clinical outcomes, resource use, and costs at 1 year in patients with acute coronary syndrome undergoing PCI: results from the multinational APTOR registry. J Interv Cardiol 2012;25:19-27
- Zhao Z, Winget M. Economic burden of illness of acute coronary syndromes: medical and productivity costs. BMC Health Serv Res 2011;11:35
- Berenson K, Ogbonnaaya A, Casciano R, et al. Economic consequences of ACS-related rehospitalizations in the US. Curr Med Res Opin 2010;26:329-36
- Johnston SS, Curkendall S, Makenbaeva D, et al. The direct and indirect cost burden of acute coronary syndrome. J Occup Environ Med 2011;53:2-7
- Ford ES, Ajani UA, Croft JB, et al. Explaining the decrease in US deaths from coronary disease, 1980-2000. N Engl J Med 2007;356:2388-98
- Ferguson JJ, Califf RM, Antman EM, et al. Enoxaparin vs unfractionated heparin in high-risk patients with non-ST-segment elevation acute coronary syndromes managed with an intended early invasive strategy: primary results of the SYNERGY randomized trial. JAMA 2004;292:45-54
- White H. Thrombin-specific anticoagulation with bivalirudin versus heparin in patients receiving fibrinolytic therapy for acute myocardial infarction: the HERO-2 randomised trial. Lancet 2001;358:1855-63
- Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non ST-Elevation Myocardial Infarction): developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. Circulation 2007;116:e148-304
- Antman EM, Hand M, Armstrong PW, et al. 2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2008;51:210-47
- Hamm CW. Current practice and limitations of dual antiplatelet therapy in acute coronary syndrome. Eur Heart J 2009;11(G Suppl):G4-8
- National Quality Forum, 2012. http://www.qualityforum.org/News_And_Resources/Press_Releases/2012/NQF_Endorses_All-Cause_Unplanned_Readmissions_Measures.aspx. Accessed April 19, 2013
- Medicare.gov. 30-day death and readmission measures data. http://www.medicare.gov/hospitalcompare/data/rcd/30-day-measures.aspx. Accessed April 17, 2013
- Wallentin L, Wilcox RG, Weaver WD, et al. Oral ximelagatran for secondary prophylaxis after myocardial infarction: the ESTEEM randomised controlled trial. Lancet 2003;362:789-97
- Merlini PA, Bauer KA, Oltrona L, et al. Persistent activation of coagulation mechanism in unstable angina and myocardial infarction. Circulation 1994;90:61-8
- Hamm CW, Bassand JP, Agewall S, et al; ESC Committee for Practice Guidelines. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2011;32:2999-3054