Abstract
Objective:
To estimate the annual incremental per-patient and overall payer burden (2012USD) of venous leg ulcers (VLU) in the US.
Methods:
Beneficiaries with and without VLU were identified using two de-identified insurance claims databases: aged 65+ from a 5% random sample of Medicare beneficiaries (2007–2010: n ∼ 2.3 million); and aged 18–64 from a privately-insured population (2007–2011: n ∼ 8.4 million). The index date was selected as the date of a VLU claim with no other VLU diagnoses in the preceding 12 months for the VLU cohort and as the date of a random medical claim for the non-VLU patients. These groups were matched using propensity scores to account for differences in demographics, comorbidities, resource utilization, and costs in the 12 month pre-index period. Medical resource use and costs incurred during the 12 month follow-up period were calculated for both payers. Drug costs and indirect work-loss due to disability and medically-related absenteeism were estimated for the privately-insured sample only. Annual VLU incidence rates were also estimated for both payers.
Results:
Data for 58,672 matched VLU/non-VLU pairs of Medicare and 22,476 matched pairs of privately-insured patients were analyzed. Relative to matched non-VLU patients, VLU patients used more medical resources and incurred annual incremental medical costs of $6391 in Medicare ($18,986 vs $12,595), and $7030 ($13,653 vs $6623) in private insurance ($7086 including drug costs). Compared with non-VLU patients, privately-insured VLU patients had more days missed from work (14.0 vs 10.0), resulting in 29% higher work-loss costs (comparisons significant at p < 0.0001). The average annual incidence rate of VLU was 2.2% in Medicare and 0.5% in private insurance.
Limitations:
Findings did not account for out-of-pocket payments or other indirect costs (e.g., lost productivity), and relied on accuracy of diagnosis and procedure codes contained in claims data.
Conclusion:
These findings suggest an annual US payer burden of $14.9 billion.
Introduction
Venous leg ulcers (VLU) are the most frequently occurring type of chronic woundCitation1. VLU have been estimated to affect millions of patients in the US at any given time, and account for up to 90% of lower extremity ulcersCitation1–3. A variety of factors have been associated with the development of VLU, including venous insufficiency, obesity, and deep vein thrombosisCitation4,Citation5. Treatment of VLU includes compression therapy, local wound management (e.g., debridement, moist dressings), and more sophisticated treatments such as bioengineered cellular technologies and negative pressure therapy. VLUs often require extensive healing time and are associated with increased risk for infections and other sequelae that can increase the morbidity of the diseaseCitation5,Citation6. Due to pain, mobility limitations, and other consequences, presence of VLU has been associated with increased rates of depression and substantial decreases in patient quality-of-lifeCitation5,Citation7,Citation8.
Little is known, however, about the burden of VLU, both in terms of the overall costs borne by public and private US payers and the incidence of the disease itself. In fact, while reported estimates of the costs of VLU in the US range from $1.9 billion to $2.5 billionCitation5, few studies have estimated the medical resource use and costs of VLU using real world data in the US. One such study relied on data from the 1990s using a small group of patients (i.e., 78 Cleveland Clinic patients)Citation2. Furthermore, the analysis was conducted without attention to a reference population (e.g., non-VLU patients). Nor did it adjust for underlying differences in patient characteristics, such as age, gender, and disproportionate presence of comorbid conditions (e.g., congestive heart failure, peripheral vascular disease, diabetes), that may contribute to overall costs. As a result, it was unable to separate costs of VLU from costs of other conditions. Moreover, little research has been done to assess costs associated with workplace productivity declines due to missed work and/or disability leave among patients with VLU.
Similarly, while the prevalence of VLU in the US has been reported to range from 0.05–1.52%Citation9, to our knowledge, there have been limited attempts to estimate the annual incidence of venous ulcers in the USCitation9. One such study estimated the annual incidence of VLU in the US to be 18.0 in 100,000 person yearsCitation9; however, this study was based on data from the 1990s and a localized population residing in Olmsted County, Minnesota, which is not necessarily generalizable to a national population given current medical technologies.
The primary objective of this study was to provide a robust, current estimate of the healthcare resource use and costs associated with VLU in the US. To do so, the analysis used de-identified administrative claims records for Medicare and privately-insured populations. In each database, resource use and costs incurred during a recent time period (1/2007–9/2011) were estimated for VLU patients and a similar population without VLU. Incremental medical resource use and cost of VLU (including healthcare and work-loss costs) were assessed using a matched cohort study design to account for differences in age, gender, rates of underlying comorbidities, availability of work-loss data (for privately-insured only), prior healthcare resource, and prior healthcare costs. The secondary objective of this analysis was to estimate the annual incidence of VLU for both Medicare (aged 65 years and older) and privately-insured populations (aged 18–64 years).
Patients and methods
Data sources
This study used administrative claims from two de-identified databases. Outcomes for Medicare patients were identified using Standard Analytical Files, which include data for a 5% random sample of Medicare beneficiaries (n ∼ 3.6 million, available through December 2010). Privately-insured patients were identified using OptumHealth Reporting and Insights, a database containing ∼16 million beneficiaries (employees, spouses, children, and retirees) of 60 large self-insured companies with locations across the US (available through September 2011). These databases contain information regarding patient age, gender, enrollment history, medical diagnoses, procedures performed, dates and place of service, and payment amounts (including amounts paid by insurers to providers and patients’ out-of-pocket costs). Additionally, the private insurance data include prescription drug claims (including fill dates, national drug codes, and payment amounts including amounts paid by insurers to providers and patients’ out-of-pocket costs) for all beneficiaries, and information about wages and work-loss due to disability for a subset of employees.
Sample selection
Patients from Medicare (1/2007–12/2010) and private insurance (1/2007–9/2011) databases were divided into two mutually exclusive groups: patients diagnosed with VLU (n = 137,664 Medicare, n = 118,557 private insurance) and without VLU (n = 2,147,354 Medicare, n = 8,279,840 private insurance). VLU patients were required to have at least one diagnosis of the following International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9 CM) codes at any time in the study period: 454.0x, 454.1x, 454.2x, 459.11, 459.13, 459.31, 459.33, and 459.81.
The index date for the VLU cohort was selected as the start of an ulcer episode, identified as the date of a leg ulcer claim with no other leg ulcer diagnoses in the preceding 12 months. In the event that a patient had multiple new VLU episodes, the analysis was focused on the most recent episode to capture the outcomes associated with current treatment patterns. Because the non-VLU patients did not have a VLU diagnosis, the index date for this cohort was selected as the date of a random medical claim in 2007–2011 (2010 for Medicare). Finally, to ensure that all relevant information on diagnoses and costs were observable in the data, the analytical sample was restricted to patients aged 65+ for Medicare, and aged 18–64 for private insurance with continuous (non-HMO) coverage throughout the 12 months prior to (‘pre-index’) and 12 months following the index date (‘follow-up’).
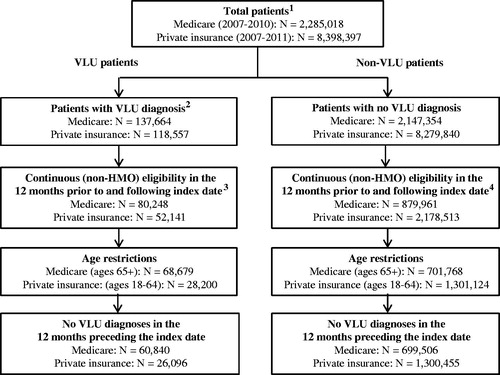
These criteria resulted in a final sample of 760,346 Medicare patients, 60,840 of whom were identified as VLU patients; the remaining 699,506 comprised the potential non-VLU comparator population. For private insurance, 1,326,551 patients met the sample selection criteria. Of these, 26,096 were identified as VLU patients and 1,300,455 as potential comparators (). Because of computational complexities associated with such large comparator populations, random samples of the potential comparators (∼5-times the VLU patients in each database) were used for estimation purposes (Medicare: 50% sample, n = 349,753; private: 10% sample, n = 130,045).
Figure 1. Selection of VLU patients and non-VLU patients. Notes: 1. Total patient population includes all beneficiaries with at least one medical claim in years evaluated. 2. VLU patients defined as those with at least one claim with ICD-9-CM: 454.0x, 454.1x, 454.2x, 459.11, 459.13, 459.31, 459.33, and 459.81 in years evaluated. 3. Index date defined as the most recent VLU diagnosis date meeting all sample selection criteria. 4. Index date defined as the date of a random medical claim in years evaluated.
Propensity score matching
To account for observable differences in pre-index characteristics between VLU and non-VLU patients, VLU patients were matched one-to-one to non-VLU patients with the same gender, year of index date, pre-index healthcare costs (±10%), availability of work-loss data (privately-insured patients only), and propensity scores (calipers equal to ¼ standard deviation) using greedy matchingCitation10. Propensity scores were calculated for patients in each database using a logistic regression with cohort assignment as the dependent variable and covariates for age, underlying medical conditions that can affect leg ulcer healing rates, other conditions that can affect healthcare costs, pre-index medical resource use, and pre-index prescription drug use (private insurance only)—see and for the complete list of these covariates.
Table 1. Patient characteristics, resource utilization, and healthcare costs during the 12 months prior to the index date—Medicare.
Table 2. Patient characteristics, resource utilization, and healthcare costs during the 12 months prior to the index date—Private insurance.
Calculation of medical resource utilization and costs
Total and incremental all-cause healthcare resource utilization and costs (2012USDCitation11, as measured by payments made by third-party payers) in the 12-month follow-up period were calculated for both VLU and non-VLU patients. These measures were broken out by place of service, with categories for hospitalizations, outpatient/physician office, home health, emergency department (ED), and other (e.g., skilled nursing facilities, durable medical equipment (DME)), in order to identify sources of utilization that comprise the cost differential. Medical costs were identified as ‘VLU-related’ if the claim included at least one diagnosis for a venous ulcer or ulcer-related infection (e.g., cellulitis, osteomyelitis) of the lower limb “where applicable”, or a procedure related to ulcer treatment (i.e., compression therapy, debridement, drainage, skin substitute use, and hyperbaric oxygen therapy (HBO)).
Additionally, for the subset of privately-insured patients with available wage and disability information (work-loss data were not available in the Medicare data), total and incremental indirect work-loss costs (2012USD) due to disability and medically-related absenteeism were estimated during both the baseline and follow-up periods. Days and cost of short- and long-term disability leave were obtained directly from the database and include actual employer payments. Medically-related absenteeism days were estimated using medical claims occurring during the workweek. Days with a hospitalization or ED visit were counted as a full day of missed work, and all other visits were counted as a half day of absenteeismCitation12. Costs due to medically-related absenteeism were calculated per beneficiary by multiplying the number of medically-related absenteeism days by the employee’s wage.
Incidence estimates
The annual incidence of VLU was calculated based on the total sample of patients identified in each database. Specifically, annual incidence was calculated as the number of patients with new VLU episodes in each calendar year divided by the total number of patients in the database who had at least one medical claim, met the age restrictions, and were continuously enrolled in non-HMO plans. A ‘new’ VLU episode was defined as a VLU diagnosis with no other VLU diagnosis in the preceding 12 months. As a result, patients included in this estimation were required to have two calendar years of continuous non-HMO enrollment (i.e., for both the calendar year for incidence estimation and the preceding year) and meet corresponding age criteria in both years.
Statistical analyses
For categorical variables, statistical significance was assessed using chi-squared tests for comparisons between pre-match VLU patients and non-VLU patients, and McNemar tests for the matched cohort. For continuous variables, statistical significance was assessed using Wilcoxon rank-sum tests (pre-match) and Wilcoxon signed-rank (post-match) tests. The claims data analyses were conducted using SAS version 9.2 (SAS Institute Inc., Cary, NC).
Results
Pre-index characteristics
VLU patients were significantly different from the non-VLU comparator population on nearly every characteristic examined during the pre-index period (i.e., in the 1-year period prior to the index date). For the Medicare sample (), VLU patients were older (77.9 (SD = 7.4) vs 75.7 (SD = 7.1)), and had at least twice the rates of peripheral vascular disease, congestive heart failure, diabetes with complications, obesity, deep vein thrombosis, and phlebitis in the 12 months prior to the index date. In addition, VLU patients had higher rates of other comorbidities including infections of lower limbs and depression. The results were similar for the privately-insured samples, with VLU patients being older (50.6 (SD = 9.3) vs 44.5 (SD = 12.2)), and having at least twice the rates of diagnoses for 18 of the 24 comorbid conditions evaluated ().
In addition, compared with the non-VLU population, both Medicare and privately-insured VLU patients had more hospitalization days (+85.7% Medicare, +158.3% private), ED visits (+100.0% Medicare, +50.0% private), and outpatient/physician office visits (+54.5% Medicare, +83.1% private) prior to the index date. These differences resulted in baseline healthcare costs among VLU patients that were approximately twice that of the comparator population ( and ). (All comparisons for resource use were significant at p < 0.0001.)
Despite these baseline differences in the overall VLU and non-VLU patient populations, the matching process resulted in a matched sample of 117,344 Medicare patients (58,672 matched VLU/non-VLU pairs) and 44,952 privately-insured patients (22,476 matched VLU/non-VLU pairs) with similar baseline demographics, comorbidities, and healthcare costs ( and ). Although some differences remained statistically significant post-match, the incremental healthcare cost estimates (reported below) were robust to a sensitivity analysis, which estimated healthcare costs in matched VLU and non-VLU patients controlling for the few pre-index variables that remained statistically significant (p < 0.05) after matching.
Direct medical resource use and costs during the follow-up period
As seen in and , the VLU groups used significantly (p < 0.0001) more medical resources and incurred more costs during the 12-month follow-up period than the matched non-VLU patients. Among Medicare patients, VLU patients had 0.7 (77.8%) more hospitalization days, 0.3 (50.0%) more ED visits, 10.4 (27.4%) more outpatient/physician office visits, and 0.3 (60.0%) more days of home healthcare. The privately-insured cohorts exhibited similar results, with matched VLU patients having had 3.2 (88.9%) more hospitalization days, 0.2 (50.0%) more ED visits, 4.2 (41.6%) more outpatient/physician office visits, and 1.0 (250.0%) more days of home healthcare. All comparisons were significant at p < 0.0001.
Figure 2. Components of per-patient all-cause healthcare cost differential during the 12-month follow-up period (VLU—matched non-VLU patients). Notes: 1. Percentages reflect the share of excess costs attributable to the place of service. 2. Prescription drug claims were not available for Medicare.
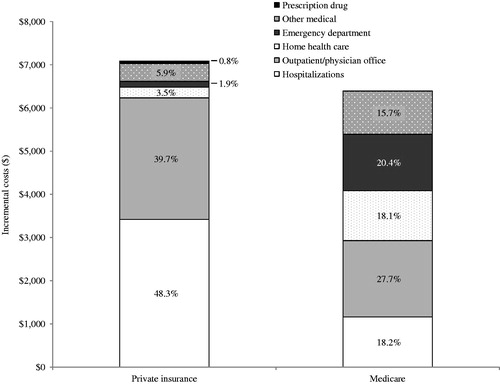
Table 3. Healthcare resource utilization and direct costs during the 12 months following the index date among matched VLU and non-VLU patients*.
VLU patients had ∼50% higher medical costs than matched non-VLU patients in Medicare ($18,986 (SD = $29,642) vs $12,595 (SD = $22,464); p < 0.0001), and more than twice the costs of matched non-VLU patients in private insurance ($13,653 (SD = $39,342) vs $6623 (SD = $19,658); p < 0.0001) (). Considering both medical and prescription drug costs, privately-insured VLU patients had an average of $7086 in total incremental direct healthcare costs ($15,296 (SD = $40,071) vs $8210 (SD = $20,756); p < 0.0001). The incremental all-cause healthcare costs resulting from a multivariate analysis controlling for pre-index patient characteristics that remained statistically significant (i.e., p < 0.05) after matching, were within 5% of those reported here (model results are available upon request).
Each place of service (i.e., hospitalization, ED, outpatient/physician office, home healthcare, and other) accounted for ∼20% of the excess costs incurred by Medicare VLU patients. For the privately insured, however, increased hospitalization and outpatient/physician office costs were responsible for ∼90% of the cost differential (). A relatively small proportion of patients were treated with advanced therapies such as skin substitutes, which were received by 0.9% and 0.1% of Medicare and privately-insured VLU patients, respectively (data not shown).
Disability and medically-related absenteeism during the follow-up period
reports results on work-loss due to disability and medically-related absenteeism for the subset of privately-insured patients for whom this information was available in the data. Despite having similar pre-index work-loss days, employees with VLU missed significantly more days of work during the 12-month follow-up period compared with matched non-VLU patients. Mean time missed due to disability leave was 4.5 days (SD = 25.5) for the VLU group, compared with 3.3 (SD = 23.6) for the matched non-VLU population (p < 0.0001). Because of greater utilization of medical services, VLU employees also had higher medically-related absenteeism than did the matched non-VLU patients (9.5 (SD = 11.4) vs 6.7 (SD = 8.3); p < 0.0001). Overall, VLU employees had ∼40% more estimated total work-loss days compared with matched non-VLU patients (14.0 (SD = 27.5) vs 10.0 (SD = 24.7); p < 0.0001).
Table 4. Disability, absenteeism, and related costs among matched VLU and non-VLU patients—privately-insured primary beneficiaries onlya.
The increased number of work-loss days led to ∼29% higher total annual indirect costs during the study period for employees with VLU ($2481 (SD = $4667)) compared with matched non-VLU patients ($1924 (SD = $3736)), with a total cost differential of $557 (p < 0.0001) ().
Incidence estimates
reports the results of the VLU incidence estimates. In Medicare, our results suggest an annual incidence of VLU that was similar across years, ranging from 2.1–2.2%, with an average of 2.2% across all years examined. Among the privately-insured patient population, estimates similarly had low variation across time, with annual incidence rates ranging from 0.4–0.6%, with an average of 0.5% across all years examined.
Table 5. Estimated annual incidence of VLU in Medicare and private insurance.
Burden of VLU in the US
As shown in , extrapolating the incidence and cost estimates of this study to a national population using publicly available statistics on the number of individuals by type of insuranceCitation13–16 suggests combined potential annual burden to Medicare and private payers of $11.6 billion ($5.9 billion for Medicare and $5.7 billion for private insurance). Moreover, while the above analysis was unable to consider other payers (e.g., self-insured, Medicaid), applying the average incidence and cost estimates developed in this study to these other payers suggests an additional annual burden of $3.3 billion. Thus, based on these estimates the total economic burden in terms of healthcare costs across all payers is $14.9 billion (ranging as high as $17.4 billion depending on the incidence and cost estimates applied to the “other” payer population).
Table 6. Estimated economic burden of VLUs in the US—by payer type.
Discussion
The analyses above examined the incremental, per-patient, annual cost of VLU, including both direct healthcare costs and indirect work-loss costs. To our knowledge this is the first study to assess the excess costs of VLU by employing robust methods to account for underlying differences between patients with and without VLU. Moreover, the study is the first to use data from large and geographically-diverse samples of Medicare and privately-insured beneficiaries, to not only capture recent and actual real-world healthcare resource utilization and costs, but also to evaluate annual incidence of VLU in the US.
Although the study estimates document substantial burden of VLU, they likely understate the true economic burden of this condition in the US. This is because the incremental costs included in the calculation include neither work-loss costs nor prescription drug costs for Medicare patients, which would impose additional burden of treating VLU patients on the US payers. Additionally, the matching process disproportionately removed relatively-high cost VLU patients, and relatively low-cost non-VLU patients, as these ‘outliers’ could not be matched. Including these patients in the analyses resulted in total all-cause costs in the year following the index date of $20,223 for Medicare patients and $20,923 for privately-insured patients, and incremental costs that were almost 2-times higher than the incremental costs calculated using matched pairs; $11,360 for Medicare patients (vs $6391) and $14,655 for privately-insured patients (vs $7086) (data not shown). Finally, this analysis assesses the costs of VLU from a payer perspective only and, therefore, does not account for a number of additional costs, such as patients’ out-of-pocket costs and costs associated with the impact of VLUs on a patient’s quality-of-life.
While a population-based incidence of VLU in the US has not been estimated previously, aspects of our findings related to incidence of VLU are consistent with prior research. For instance, despite differences in study populations and methodology, our finding that 2.2% of patients aged 65 years and older developed new VLU each year is consistent with the reported incidence rate among elderly in other researchCitation17,Citation18.
This study had a number of limitations. First, as with any claims data analysis, this analysis relied on the measures in the database to evaluate the resource use and cost information in the follow-up period. Moreover, any miscoding of diagnoses related to VLU or patients’ comorbidity profiles would affect our results, although we have no reason to believe that any inaccuracies in the data may have affected the VLU and non-VLU groups differently. Second, the per-patient costs and incidence estimates (and corresponding burden calculation) are based on patients with diagnosed VLU who met our sample selection criteria. To the extent that some patients with VLU go undiagnosed or did not meet the criteria, they would not be accounted for in this study.
Third, we only captured costs associated with work time lost due to illness or medical treatment; therefore, the work-loss costs calculated potentially understate actual costs due to missed work for other reasons such as sick time at home, reduced on-the-job productivity (i.e., ‘presenteeism’), and administrative and training expenses for replacement workers. In addition, because work-loss information could only be estimated for a subset of primary beneficiaries, the calculation by definition is limited to the employed population only. Additionally, this analysis does not account for unemployment costs potentially related to VLU.
Fourth, the calculation of incremental healthcare costs and VLU incidence estimates were based on patients with 2 years of continuous eligibility. Although this requirement was necessary to properly identify recent VLU episodes and account for underlying differences between the VLU and non-VLU populations, it is unknown what impact this has on the generalizability to other patients who may be enrolled in their plans for shorter time periods.
Finally, while the propensity score matching led to matched cohorts with similar baseline characteristics in terms of magnitude, the results were robust (within 5%) to multivariate analyses that controlled for the few measures for which statistically significant differences remained after matching. The matching approach could not control for clinical detail regarding wound-specific information (e.g., presence of a single vs multiple VLU), as this information was not available in the claims data. Further research is warranted to examine the costs of VLU accounting for these characteristics.
Conclusions
The findings of this study highlight the substantial annual payer burden of VLU of $14.9 billion by quantifying the incremental resource use and costs of treating these patients ($6391 per Medicare patient, $7086 per privately-insured patient). In addition, it quantifies the proportions of patients affected by this condition each year for two types of payers in the US. Such knowledge may enhance awareness of the often under-appreciated burden of this disease among health plans and providers, which, in turn, may encourage better monitoring as well as targeted early intervention with the aim of reducing cost and improving outcomes.
Transparency
Declaration of funding
This study was funded by Organogenesis, Inc., Canton, MA.
Declaration of financial/other relationships
JBR, UD, AKGC, and HGB are employees of Analysis Group, Inc., a company that received funding from Organogenesis, Inc. to conduct this study. MS and NP are employees of Organogenesis, Inc. JME peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Acknowledgments
No assistance in the preparation of this article is to be declared. Abstracts containing results from this analysis were presented at 2013 Spring Symposium for Advanced Wound Care (SAWC) in Denver, CO, ISPOR 18th Annual International Meeting in New Orleans, Louisiana, and 2013 Fall SAWC in Las Vegas, NV.
References
- Phillips TJ, Dover JS. Leg ulcers. J Am Acad Dermatol 1991;25:965-87
- Olin JW, Beusterien K, Childs MB, et al. Medical costs of treating venous stasis ulcers: evidence from a retrospective cohort study. Vasc Med 1999;4:1-7
- Sen CK, Gordillo GM, Roy S, et al. Human skin wounds: a major and snowballing threat to public health and the economy. Wound Repair Regen 2009;17:763-71
- Robertson L, Evans C, Fowkes FGR. Epidemiology of chronic venous disease. Phlebology 2008;23:103-11
- Valencia IC, Falabella A, Kirsner RS, et al. Chronic venous insufficiency and venous leg ulceration. J Am Acad Dermatol 2001;44:401-21
- Nelzén O, Bergqvist D, Lindhagen A. Long term prognosis for patients with chronic leg ulcers: a prospective cohort study. Eur J Vasc Endovasc Surg 1997;13:500-8
- Phillips T, Stanton B, Provan A, et al. A study of the impact of leg ulcers on quality of life: financial, social, and psychologic implications. J Am Acad Dermatol 1994;31:49-53
- Green J, Jester R. Health-related quality of life and chronic venous leg ulceration: part 1. Wound Care 2009;December:S12-S17
- Heit JA, Rooke TW, Silverstein MD, et al. Trends in the incidence of venous stasis syndrome and venous ulcer: a 25-year population-based study. J Vasc Surg 2001;33:1022-7
- Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res 2011;46:399-424
- US Bureau of Labor Statistics. Consumer Price Index. Washington DC, 2013. Available at: http://www.bls.gov/cpi/home.htm [Last accessed 2 February 2013]
- Birnbaum HG, Barton M, Greenberg PE, et al. Direct and indirect costs of rheumatoid arthritis to an employer. JOEM 2000;42:588-96
- United States Census Bureau. US Population Clock. Washington DC, 2013. Available at: http://www.census.gov/main/www/popclock.html [Last accessed 1 February 2013]
- United States Census Bureau State & County QuickFacts, Persons under 18 years, percent. 2011. Washington DC: US Census Bureau. Available at: http://quickfacts.census.gov/qfd/states/00000.html. [Last accessed 2 February 2013]
- CMS. Medicare & Medicaid Statistical Supplement. Baltimore, MD., 2013. Available at: http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/MedicareMedicaidStatSupp/2013.html. Accessed Table 2.2 ‘Medicare Enrollment: Hospital Insurance and/or Supplementary Medical Insurance Programs for Total, Fee-for-Service and Managed Care Enrollees, by Demographic Characteristics as of July 1, 2012’.
- Mossavar-Rahmani. Center for Business & Government. Health care delivery customers by market segment: summary of findings. Cambridge, MA: Kennedy School of Government, Harvard University, 2008. [Last accessed 2 February 2013]
- Margolis DJ, Bilker W, Santanna J, et al. Venous leg ulcer: incidence and prevalence in the elderly. J Am Acad Dermatol 2002;46:381-6
- Takahashi P, Chandra A, Cha SS, et al. A predictive model for venous ulceration in older adults: results of a retrospective cohort study. Ostomy Wound Management 2010;56:60-6
