Abstract
Objective:
To define the in-hospital and 6-month post-discharge resource use, following Transcatheter Aortic Valve Implantation (TAVI) and conventional Aortic Valve Replacement (AVR) surgery within a single UK hospital.
Methods:
A local service evaluation of patients undergoing TAVI or AVR between January 2011 and May 2012 captured data until 6-months post-procedure, collected from hospital records and via a General Practitioner questionnaire. The main end-points were mortality, time in ITU/HDU, hospital length of stay (LoS), discharge destination, re-admission, and post-discharge primary/secondary care resource use. Sub-group analyses were performed for AVR patients aged ≥80 (AVR ≥ 80) and with EuroSCORE of ≥10 (AVR ES ≥ 10) to allow more direct comparison with ‘TAVI type’ patients.
Results:
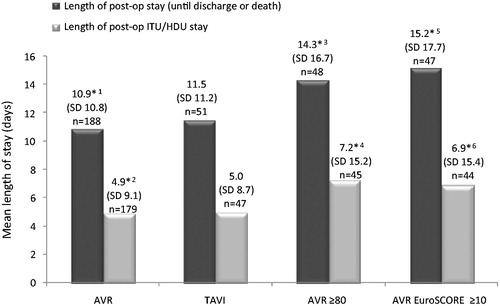
Results are given as means (standard deviation) for TAVI (n = 51), AVR (n = 188), AVR ≥ 80 (n = 48), and AVR ES ≥ 10 (n = 47), respectively, unless otherwise stated. Age in years was 83.0 (8.1), 71.2 (13.1), 84.1 (2.7), 79.4 (7.1); EuroSCORE was 24.7 (11.9), 8.1 (6.4), 12.0 (6.0), and 16.5 (6.6); post-operative LoS (days) was 11.5 (11.2), 10.9 (10.8), 14.3 (16.7), and 15.2 (17.7). For discharged patients, 0%, 7%, 13%, and 9% had unplanned cardiac-related re-admissions within 30-days of discharge. Time to first readmission was 74.6 (34.0), 35.0 (34.2), 20.8 (9.7), and 22.6 (14.3) days.
Limitations:
This was a single-center retrospective evaluation, not prospectively powered to confirm differences in outcomes.
Conclusions:
Despite TAVI being performed in an older, higher risk population, LoS was similar to AVR. Most strikingly there were no cardiac-related re-admissions within 30-days for TAVI and time to first re-admission was significantly longer. This evaluation suggests that TAVI is clinically appropriate and provides economic advantages in both the hospital and post-discharge setting in this high risk group. Many patients undergoing TAVI are considered unfit for surgery and, hence, TAVI offers a treatment that delivers similar results to traditional AVR without the high risk associated with surgery.
Introduction
Aortic stenosis is a degenerative disease that involves thickening and stiffening of the aortic valve cusps leading to progressive restriction of valve opening. Prevalence increases with age and in individuals aged 85 years and over it is at least 4%Citation1. Symptoms include chest pain, breathlessness, dizziness, and fainting, generally on exertion. Untreated symptomatic aortic stenosis is associated with a poor prognosis with median survival somewhere between 1–5 years, depending on the mode of presentation.
The current standard treatment of aortic stenosis is surgical aortic valve replacement (AVR)Citation2. This involves replacing the diseased valve with a biological or mechanical prosthetic valve typically via a median sternotomy under general anesthesia using cardiopulmonary bypass. In elderly patients and in those with significant co-morbidities, however, this operation entails an elevated risk as well as prolonged post-operative inpatient stay and rehabilitation.
Transcatheter aortic valve implantation (TAVI) is a procedure performed without the use of cardiopulmonary support and can, in some cases, be carried out under local anesthesia or sedation. In terms of evidence of effectiveness, the PARTNER trial was the first randomized controlled trial for TAVI and recruited two primary patient cohorts (A and B). Patients in cohort A were designated high risk for surgery but operable and patients were randomized to TAVI or conventional surgery. Those recruited to cohort B were designated as inoperable, i.e., extreme risk for surgical intervention, and patients were randomized to TAVI or the then current standard of care (primarily pharmacotherapy). For cohort B, TAVI was shown to be associated with significantly reduced mortality vs those in the conservative treatment arm after 1 year of follow-up (30.7% vs 50.7%; p < 0.001)Citation3.
At present in the UK, in keeping with the currently available trial data, TAVI is undertaken principally in patients for whom conventional aortic valve replacement would entail a high risk. UK National Health Service (NHS) providers should systematically review, analyse, and improve their servicesCitation4, a goal which is ever more important within a changing NHS landscape. Whilst some data are available on the time to discharge following surgery with the two techniquesCitation5, although notably nothing directly from UK hospitals, there are no data to describe either the current pathway of care following discharge from hospital or the impact of TAVI on this pathway. There are published economic analyses of TAVI in the UK based on the available clinical data (typically either from the PARTNER study or large observational registries) which overwhelmingly demonstrate that TAVI is a cost-effective treatment optionCitation6–9. However, they are not validated by empirically-derived published UK resource estimates of TAVI. It has been observed that minimally invasive surgery is associated with shorter recovery times, both in the inpatient recovery and the post-discharge periodsCitation10,Citation11. Accordingly, in order to assess the true value of TAVI, it is essential to consider the complete patient pathway. This is particularly important in the current NHS climate where there is a recognized need to consider ways of optimizing complete patient pathways and improving patient outcomes in order to deliver quality care in the most cost-effective way. This study aimed to describe the post-operative NHS care requirements following TAVI and conventional aortic valve replacement in one tertiary care NHS Trust.
The objectives were:
To describe the post-operative resource use for patients undergoing TAVI or AVR during the inpatient stay and over the 6-month period following the procedure.
To describe the post-discharge patient pathway for patients undergoing TAVI or AVR.
Patients and methods
This local service evaluation took place at Barts Health NHS Trust tertiary care center. It included retrospective evaluation of the healthcare resource utilization of patients undergoing TAVI or AVR procedures. Both the inpatient post-operative period and post-discharge follow-up in Barts Health NHS Trust and other healthcare settings were included. The post-discharge care pathway followed by both groups of patients for 6 months post-procedure was also described.
A total of 51 consecutive patients who underwent TAVI from January 1, 2011 and all patients (188) who underwent conventional AVR during this same period were included in the evaluation. Two patients for whom Barts Health NHS Trust hospital records were unavailable were excluded. Patients were identified retrospectively from either the hospital coding system or the cardiology department database.
The following parameters were measured to determine resource use and outcomes in all patients: time in ITU/HDU, overall length of stay, discharge destination, cardiac-related re-admission to hospital within 30 days and 6 months, number of hospital inpatient admissions, visits to hospital accident and emergency departments, outpatient clinic visits, and primary care contacts. Data on inpatient post-operative resource use were collected retrospectively from patient medical records and electronic hospital systems. Data relating to the post-discharge pathway and resource use whether in primary or secondary care were collected from primary care records via a standardized data collection form sent to the patient’s GP. Data on post-discharge resource use up to 6 months post-procedure were also collected from the hospital medical records, when recorded. A ‘re-admission’ was defined as any unplanned inpatient (i.e., length of stay ≥1 day) hospitalization, with an admission date in the 30 days following discharge from Barts Health NHS Trust or in the 6 months post-procedure. Patient mortality data were also collected both from hospital records and GP primary care records.
The dataset was analyzed using Microsoft Excel. All analyses were performed separately for AVR and TAVI. Two further ‘high risk’ AVR sub-groups were also analyzed separately; those aged 80 years or above (AVR age ≥80) and those with a logistic EuroSCORE of 10 or greater (AVR ES ≥10). Where appropriate, the Student’s t-test was used to determine whether there were significant differences between the sample means for TAVI when compared with AVR and the two high-risk AVR sub-groups.
Results
Patient demographics and sample characteristics
A total of 188 patients undergoing AVR and 51 patients undergoing TAVI were included in the evaluation, with procedure dates from January 4, 2011 to May 22, 2012. The numbers of patients within the two ‘high risk’ sub-groups were: 48 in the AVR age ≥80 group (mean age = 84 years, mean EuroSCORE = 12.0), and 47 in the AVR ES ≥10 group (mean age = 79 years, mean EuroSCORE = 16.5). Of the 188 patients undergoing AVR, 72 (38%) were known to have undergone AVR with CABG, the remainder being AVR alone. Demographic characteristics for the AVR and TAVI groups are presented separately, for both ‘high risk’ AVR sub-groups and for patients undergoing AVR with and without CABG ().
Table 1. Summary demographic characteristics.
TAVI was predominantly performed via the transfemoral route (25, 49%) but there were also transapical (19, 37%) and transaortic (6, 12%) procedures, with the route unknown in one case (2%). Due to the relatively small sample size overall the resource usage of these were not analyzed separately.
The majority of patients had at least one co-morbidity or cardiovascular risk factor recorded (99% (187/188) in the AVR group and all patients in the TAVI group). In the AVR group, the most commonly recorded were dyslipidaemia (75%; 141/188) and coronary artery disease (58%; 109/188). In the TAVI group, coronary artery disease (55%; 28/51) and being a past smoker (53%; 27/51) were the most commonly recorded.
The presence of a number of co-morbidities was higher in the TAVI group, for example, respiratory disease (37% TAVI, 15% AVR), previous stroke or TIA (18% TAVI, 6% AVR), impaired renal function (20% TAVI, 7% AVR), and previous cardiac surgery (43% TAVI, 18% AVR). These are all component factors contributing to a higher EuroSCORE.
Resource use associated with original inpatient hospitalization
The mean post-operative length of stay, until patient death or discharge, is shown (). Where ITU and HDU data were available, the mean total post-operative length of stay in ITU and/or HDU is also shown in . There were no significant differences between TAVI and the three AVR groups.
Patient pathway
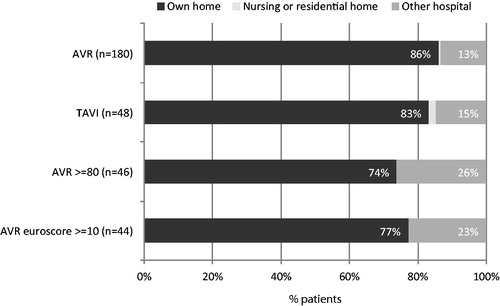
Eight patients (4%) in the AVR group, three (6%) in the TAVI group, two (4%) in the AVR age ≥80 sub-group, and three (6%) in the AVR ES ≥10 sub-group died in hospital following their procedure. Discharge destinations for the four groups are shown in . For patients discharged to another hospital, the length of stay in the receiving hospital was unknown in the majority of cases.
Survival and unplanned re-admissions
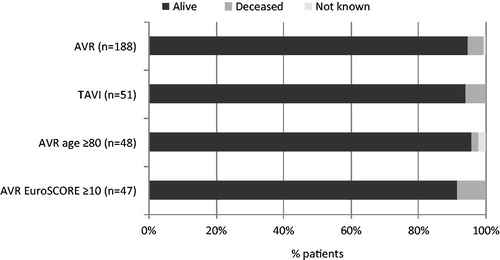
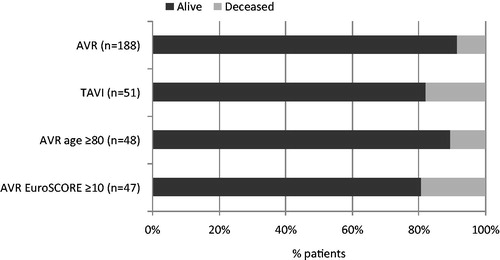
The number and proportion of patients who were known to be alive at 30 days post-procedure is shown in , and at 6 months post-procedure in . One patient was recorded on the data collection form as deceased, but the date of death was unknown. The patient was recorded as deceased at 6 months post-procedure, but vital status at 30 days post-procedure was unknown.
The number of discharged patients with unplanned cardiac-related re-admissions in the 30 days and 6 months following discharge is shown in . The mean (SD) time to first unplanned cardiac-related re-admission was significantly longer for the TAVI group at 74.6 (34.0) days, than for the AVR group at 35.0 (34.2) days (p = 0.02 vs TAVI), the AVR sub-group aged ≥80 at 20.8 (9.7) days (p = 0.003 vs TAVI), and the AVR ES ≥10 at 22.6 (14.3) days (p = 0.004 vs TAVI).
Table 2. Proportion of patients re-admitted within 30 days post-discharge or during the 6 months post-procedure (unplanned cardiac-related re-admissions only).
NHS resource use associated with post-discharge care in the 6 months following procedure
For patients discharged following the index procedure (n = 180, 48, 46, and 44, respectively, for AVR, TAVI, AVR age ≥80, and AVR ES ≥10), post-discharge resource use data were provided from the patient’s general practitioner for 134 (74%) AVR, 33 (69%) TAVI, 38 (83%) AVR age ≥80, and 33 (75%) AVR ES ≥10. Demographic and risk scoring data in this sub-group were similar to the entire cohort; the mean (SD) age at the date of the procedure was 71.8 (13.4) for AVR and 82.3 (9.4) for TAVI; 74 (55%) of AVR and 21 (64%) of TAVI were male, and mean EuroSCORE was 8.2 (6.7) and 24.2 (11.8) for AVR and TAVI, respectively. Fifty-three (40%) underwent AVR with CABG.
The mean number of inpatient hospital admissions per patient is shown in . There were no significant differences in the number of inpatient admissions between TAVI and the three AVR groups. Where inpatient admissions occurred, the mean (SD) length of stay was 7.9 (11.8) days for AVR, 11.2 (11.8) days for TAVI, 9.3 (7.6) days for AVR aged ≥80, and 13.9 (18.0) days for AVR ES ≥10. For the AVR and TAVI groups, and both AVR sub-groups, the most common reasons for admission were cardiac and respiratory.
Figure 5. Resource use associated with post-discharge care. ‘Primary care contacts’ includes any recorded primary care visit or contact (at the GP surgery, patient’s home or via telephone) with any health professional (GP, nurse, physiotherapist, other).
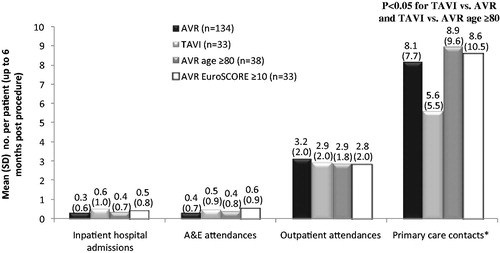
The number of primary care contacts in the period following discharge up to 6 months post-procedure was significantly lower for TAVI (5.6) than for the AVR (8.2, p = 0.016 vs TAVI) or AVR aged ≥80 (9.0, p = 0.035 vs TAVI) sub-groups. For all groups, most primary care contacts were with a GP (67% for AVR, 72% for TAVI, 64% for AVR aged ≥80 and 66% for AVR ES ≥10). Of all recorded visits/contacts with a GP, the proportion of visits which were made at the patient’s home was 9%, 22%, 14%, and 19%, respectively.
Of the patients with primary care data available, where information on residential status was available for both pre- and post-procedure (n = 131, 33, 35, and 32, respectively, for AVR, TAVI, AVR aged ≥80, and AVR ES ≥10), only one patient (in the AVR group) was known to have been newly admitted to a residential or nursing care home following the procedure. This patient was admitted to a nursing home for a few weeks post-operatively.
Discussion
Overall this study observed notable differences (some significant) in patient profiles and resource usage between TAVI and AVR groups with TAVI patients using somewhat fewer resources, despite being older and at a higher pre-operative risk as judged by their EuroScore.
Patient demographics and sample characteristics
At present, TAVI is funded for patients who are judged by a specialist team, in agreed cardiac centers, to be at too high a risk for open heart surgery, primarily as a result of other conditions (co-morbidities)Citation12. In this cohort, patients undergoing TAVI had significantly higher logistic EuroSCOREs than patients undergoing AVR and mean age at the date of the procedure was also significantly higher for patients undergoing TAVI (83 vs 71 years). Although this local service evaluation was not powered to determine statistical significance across all parameters, it was observed that the presence of co-morbidities was higher in patients undergoing TAVI. As expected, and in accordance with previously published dataCitation13, patients undergoing combined AVR and CABG were older (mean age = 75 years) than those undergoing isolated AVR procedures (mean age = 69 years).
Inpatient resource use
Although patients undergoing TAVI were older and at higher risk than the overall AVR group, the total post-operative length of stay and the length of stay on the ITU/HDU were similar for the TAVI and AVR groups. When examining the results by sub-groups (AVR aged ≥80 and AVR ES ≥10), the length of stay for TAVI compared favorably to AVR. However, although there was a trend towards a shorter length of stay in ITU/HDU for TAVI, the differences were not statistically significant. This may be because this sample was under-powered or it could be the consequence of local management practices and development of the clinical approach taken for TAVI. There have been recent discussions on an approach pioneered in Canada advocating a very rapid (next day) discharge protocol for TAVICitation14. This required a specific program for patient selection and appraisal, but has shown the potential for enormous cost savings and efficiencies in hospital economics. When one considers the published NHS mean daily cost estimate for an ICU stay is between £631–£1796Citation15 it is immediately apparent that there are potential cost savings achievable with procedures that enable rapid recovery and discharge. There are also important considerations regarding operational efficiencies and increased capacities, reduced cancelled elective procedures, etc., due to lower bed occupancy and/or predictable use. However, these are complex considerations outside the scope of this analysis and all of these also fail to account for the benefit to the patient, i.e., faster recovery and return to normal activities and potentially improved quality-of-life. Therefore, further, prospective, adequately powered research is warranted to investigate this.
The trends observed in this evaluation are similar to those of a previous study undertaken in Germany, which matched a group of consecutive patients undergoing TAVI with AVR patients in terms of baseline characteristics and risk factorsCitation16. Patients in the TAVI group were found to have a significantly shorter ITU stay, although there was no difference in overall duration of hospital stay. Additionally, a recent UK-specific economic analysis showed that TAVI appears likely to be cost-effective in a high-risk elderly population, when compared with AVRCitation8. It was found that TAVI was between £1350–£1600 cheaper than surgical AVR per patient per year. Importantly, however, this model was based on a number of assumptions and local evidence in addition to real life data.
Unplanned cardiac-related re-admissions
Of great significance to healthcare providers, under NHS PbR guidance there is non-payment by the commissioner for a proportion of emergency re-admissions that occur within 30 days of dischargeCitation17. Importantly, in the TAVI group, there were no cardiac-related re-admissions within 30 days of discharge, and the time to first re-admission was significantly longer. Although this finding is based on small numbers of patients, it has potentially important economic implications for cardiothoracic centers.
Post-discharge resource use
There was a good response rate to the request for details of resource use in the period following discharge, with 73% (167/228) providing data. Patient characteristics were similar to those of the overall TAVI and AVR groups. In the 6-month period following discharge, the mean number of inpatient admissions, A&E attendances, and outpatient appointments per patient were similar for all groups.
In contrast, primary care resource use following discharge was significantly lower for TAVI than for AVR or AVR age ≥80. This is perhaps surprising given the higher prevalence of co-morbidities seen in the TAVI group.
Differences in devices and access routes
In addition to the expected variability in patients, the outcomes for TAVI in our evaluation could be impacted by several factors, most notably the specific device used and the access route. Concerning the device, the data on TAVI in this study were exclusively collected from patients receiving a Sapien XT (Edwards Lifesciences, Irvine, CA). Other devices are available and, although data is minimal for all except CoreValve (Medtronic, Minneapolis, MN) there are acknowledged differences in performance which are likely to lead to differences in resource usage. For example, CoreValve is associated with increased requirement for post-operative implantation of a permanent pacemaker. In addition, some registries have found an increased incidence of significant paravalvular leak and of repeat procedures following Corevalve implantation, and an increased incidence of surgical conversion following Sapien implantationCitation18–20, but no differences in mortality have been demonstrated at 30 days or 1 year. TAVI is also performed via different access routes (femoral, apical, aortic, and subclavian). In this evaluation the access route was predominantly transfemoral, but there were also several transapical and transaortic procedures. These are more invasive surgical procedures and would be expected to increase recovery time, affecting the overall results and any comparison with AVR.
Limitations
Ours was a retrospective evaluation and not specifically powered to determine if differences in resource use were significant between TAVI and AVR. It, therefore, suffers from the limitations inherent to any retrospective study including sub-optimal completeness of data and the inherent variability and potential bias in patient populations. Nonetheless, it was possible to determine significant differences between patient groups, and this has important implications to local practice and the Trust. It should be noted in particular that other centers may find substantial differences in post-operative resource use (predominantly length of stay) and patient destination after discharge due to local conditions and guidelines. However, it should be possible to test this locally and could be the subject of a multi-center investigation.
Conclusion
In this single-center evaluation, despite TAVI being performed in an older, higher risk population, the length of post-operative and ITU/HDU stay were similar to those following AVR, and compared favorably to those following AVR in high-risk groups. Importantly, in the TAVI group, in contrast to AVR, there were no recorded cardiac-related re-admissions within 30 days of discharge, and time to first re-admission was significantly longer. Overall post-discharge resource use and 6-month cardiac-related re-admission rates were similar. This evaluation suggests that TAVI conducted in Barts Health NHS Trust is clinically appropriate and is likely to provide economic advantages for the Trust. The findings also suggest long-term benefits for the local health economy, extending beyond patient discharge, which may offset the additional cost of the procedure. To confirm the encouraging results from our investigation, a larger, prospective, observational research study collecting more detailed data is required.
Transparency
Declaration of funding
This evaluation was facilitated by pH Associates, an independent research consultancy specializing in the evaluation of NHS services, and funded by Edwards Lifesciences.
Declaration of financial/other relationships
Mr Wael Awad, Professor Anthony Mathur, and Dr Simon Kennon have received sponsorship to support attendance at conferences from both Edwards Lifesciences and Medtronic. Laura Baldock and Sam Oliver are employees of pH Associates Ltd, an independent research consultancy who received funding from Edwards Lifesciences to facilitate the evaluation. JME peer reviewers on this manuscript have received grants from Medtronic in the past.
Acknowledgments
This evaluation has been previously presented as a poster presentation at the ISPOR 16th Annual European Congress, Dublin, November 2–6, 2013 (abstract presentation code PCV115) and as abstract presentations at the PCR London Valves Conference, London, September 15–17, 2013.
References
- Carabello BA, Paulus WJ. Aortic stenosis. Lancet 2009;373:956-66
- National Institute for Health and Care Excellence (NICE). Transcatheter aortic valve implantation for aortic stenosis. Manchester: NICE Interventional Procedure Guidance 421, 2012. Available at: http://publications.nice.org.uk/transcatheter-aortic-valve-implantation-for-aortic-stenosis-ipg421 [Last accessed 27 June 2013]
- Svensson LG, Tuzcu M, Kapadia S, et al. A comprehensive review of the PARTNER trial. J Thorac Cardiovasc Surg 2013;145:S11-16
- Lord Darzi. High quality care for all: NHS Next Stage Review final report. London: Department of Health, 2008. Available at: http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_085825 [Last accessed 27 June 2013]
- Conradi L, Seiffert M, Treede H, et al. Transcatheter aortic valve implantation versus surgical aortic valve replacement: a propensity score analysis in patients at high surgical risk. J Thorac Cardiovasc Surg 2012;143:64-71
- Watt M, Mealing S, Eaton J, et al. Cost-effectiveness of transcatheter aortic valve replacement in patients ineligible for conventional aortic valve replacement. Heart 2012;98:370-6
- Murphy A, Fenwick E, Briggs A, et al. How best to handle the evidence in a cost-effectiveness analysis of TAVI in the UK. Trials 2011;12(1 Suppl):A46
- Fairbairn TA, Meads DM, Hulme C, et al. The cost-effectiveness of transcatheter aortic valve implantation versus surgical aortic valve replacement in patients with severe aortic stenosis at high operative risk. Heart 2013;99:914-20
- Orlando R, Pennant M, Rooney S, et al. Cost-effectiveness of transcatheter aortic valve implantation (TAVI) for aortic stenosis in patients who are high risk or contraindicated for surgery: a model-based economic evaluation. Health Technol Assess 2013;17:1-86
- Ryan WH, Brinkman WT, Dewey TM, et al. Mitral Valve Surgery: comparison of outcomes in matched Sternotomy and Port Access Groups. J Heart Valve Dis 2010;19:51-9
- Miceli A, Murzi M, Gilmanov D, et al. Minimally invasive aortic valve replacement using right minithoracotomy is associated with better outcomes than ministernotomy. J Thorac Cardiovasc Surg 2013; doi:pii: S0022-5223(13)00893-3. 10.1016/j.jtcvs.2013.07.060. [Epub ahead of print].
- NHS Commissioning Board Clinical Reference Group for Specialised Cardiology. Clinical Commissioning Policy: Transcatheter Aortic Valve Implantation (TAVI) for Aortic Stenosis. 2013, Reference: NHSCB/A09/P/a. Available at: http://www.england.nhs.uk/wp-content/uploads/2013/04/a09-p-a.pdf [Last accessed 17 October 2013]
- deWaard GA, Jansen EK, de Mulder M, et al. Long-term outcomes of isolated aortic valve replacement and concomitant AVR and coronary artery bypass grafting. Neth Heart J 2012;20:110-17
- Wood DA, Poulter RS, Cook R, et al. A multidisciplinary, multimodality, but minimalist (3M) approach to transfemoral transcatheter aortic valve replacement facilitates safe next day discharge in high risk patients. J Am Coll Cardiol 2013;62:B38-9
- Department of Health. National Schedule of Reference Costs 2011-2012 for NHS Trusts and NHS Foundation Trusts. Leeds: Department of Health Payment by Results Team, 2012. Available at: https://www.gov.uk/government/publications/nhs-reference-costs-financial-year-2011-to-2012 [Last accessed 24 October 2013]
- Conradi L, Seiffert M, Treede H, et al. Transcatheter aortic valve implantation versus surgical aortic valve replacement: a propensity score analysis in patients at high surgical risk. J Thorac Cardiovasc Surg 2012;143:64-71
- Department of Health, Payment by Results team. Payment by Results Guidance for 2013-14. Leeds: Department of Health, 2013. Available at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/214902/PbR-Guidance-2013-14.pdf [Last accessed 10 September 2013]
- Abdel-Wahab M, Zahn R, Horack M, et al. Aortic regurgitation after transcatheter aortic valve implantation: incidence and early outcome. Results from the German transcatheter aortic valve interventions registry. Heart 2011;97:899–906
- Athappan G, Patvardhan E, Tuzcu M, et al. Incidence, predictors and outcomes of aortic regurgitation after transcatheter aortic valve replacement: meta-analysis and systematic review of literature. J Am Coll Cardiol 2013;61:1585-95
- Moat NE, Ludman P, deBelder MA, et al. Long-term outcomes after transcatheter aortic valve implantation in high-risk patients with severe aortic stenosis: The UK TAVI Registry. J Am Coll Cardiol 2011;58:2130-8