Abstract
Objective:
Results of randomized clinical trials (RCT) demonstrate that novel oral anticoagulants (NOAC) are effective therapies for reducing the risk of stroke in non-valvular atrial fibrillation (NVAF). Prior medical cost avoidance studies have used warfarin event rates from RCTs, which may differ from patients receiving treatment in a real-world (RW) setting, where the quality of care may not be the same as in a RCT. The purpose of this study was to estimate the change in medical costs related to stroke and major bleeding for each NOAC (apixaban, dabigatran, and rivoraxaban) relative to warfarin in a RW NVAF population.
Methods:
Patients (n = 23,525) with a diagnosis of NVAF during 2007–2010 were selected from a Medco population of US health plans. Stroke and major bleeding excluding intracranial hemorrhage (MBEIH) events were identified using diagnosis codes on medical claims. RW reference event rates were calculated during periods of warfarin exposure. RW event rates for NOACs were estimated by multiplying the corresponding relative risk (RR) from the RCTs by each reference rate. Absolute risk reductions (ARR) or number of events avoided per patient year were then estimated. Changes in medical costs associated with each NOAC were calculated by applying the ARR to the 1-year cost for each event. Costs for stroke and MBEIH were obtained from the literature. Drug and international normalized ratio monitoring costs were not considered in this analysis.
Results:
Compared to RW warfarin, use of apixaban and dabigatran resulted in total (stroke plus MBEIH) medical cost reductions of $1245 and $555, respectively, during a patient year. Rivaroxaban resulted in a medical cost increase of $144.
Conclusions:
If relative risk reductions demonstrated in RCTs persist in a RW setting, apixaban would confer the greatest medical cost savings vs warfarin, resulting from significantly lower rates of both stroke and MBEIH.
Introduction
It is estimated that more than 5 million Americans may be living with atrial fibrillation (AF)Citation1. AF is a serious condition and a significant risk factor for stroke; individuals with AF have a 5-fold increased risk of ischemic strokeCitation2–4. Around 20% of the stroke cases caused by AF are fatal, while 60% result in serious disabilityCitation5. AF is primarily a disease of the elderly and is prevalent in 9% of the population 80 years or olderCitation2,Citation6. Up to 70% of AF cases are of the non-valvular atrial fibrillation (NVAF) typeCitation7. The rates of stroke and NVAF in the US are projected to increase with the growing elderly populationCitation8. The economic burden associated with NVAF and its resulting complications are significant. In the US, annual costs of managing NVAF are estimated at $6.65 billion, including $4.88 billion in hospitalization expenses and $1.53 billion in outpatient costs (in 2005 dollars)Citation9.
Warfarin has long been the principal anticoagulant used to reduce stroke risk among NVAF patients with a moderate-to-high risk of stroke. Although several clinical trials have demonstrated the benefits of warfarin in preventing strokeCitation10–14, there are several limitations associated with its use. These include a narrow therapeutic range, as measured by the international normalized ratio (INR), the need for frequent INR monitoring, and various clinically important interactions with drugs and food.
To date, three novel oral anticoagulants (NOAC) have been developed and approved by the US Food and Drug Administration as treatment options for patients with NVAF. These new therapies include dabigatran, a direct thrombin inhibitor, as well as rivaroxaban and apixaban, both of which are direct factor Xa inhibitors. All three NOACs have certain advantages over warfarin that were demonstrated in the head-to-head trials: RE-LY, ROCKET-AF, and ARISTOTLECitation15–17. The RE-LY trial demonstrated that dabigatran (150 mg twice a day [bid]) was associated with lower rates of stroke and systemic embolism and comparable rates of major bleeding vs warfarinCitation15. In the ROCKET-AF trial, rivaroxaban was similar in efficacy to warfarin for preventing stroke and systemic embolism with a comparable risk of major bleeding eventsCitation17. Findings from the ARISTOTLE trial showed that apixaban compared to warfarin was more effective in reducing the risk of stroke or systemic embolism, while at the same time significantly reducing the risk of major bleedingCitation16.
There is limited evidence regarding how reductions in stroke and major bleeding events associated with NOACs may impact the medical costs of NVAF patients receiving treatment in real-world (RW) clinical practice. In a recent study, Deitelzweig et al.Citation18 estimated total medical cost reductions related to the use of each NOAC vs warfarin of −$179, −$89, and −$485 during a patient year for dabigatran, rivaroxaban, and apixaban, respectively. The medical cost reductions in that study were calculated by using relative risk reductions (RRR) from the three NOAC clinical trials and a weighted average of the warfarin event rates, also obtained directly from the trials and used as reference rates. It is widely regarded that the reference rates of events obtained from trials may not be generalizable to actual practice as trial investigators often select individuals who are more likely to tolerate the study medicationsCitation19,Citation20. As a result, elderly patients and those at a higher risk of adverse events are often excluded from trials. In addition, the quality of patient care, including INR control, in the real world may not be the same as in a trial setting.
The objective of this study was to estimate the impact associated with the use of each NOAC as an alternative to warfarin on medical costs related to stroke and major bleeding among NVAF patients in a RW clinical practice. This analysis was limited to NOACs currently approved for use in the US market. In order to obtain results which are more reflective of patients in actual clinical practice, reference event rates of stroke and major bleeding excluding intracranial hemorrhage (MBEIH) were estimated for RW NVAF patients using the Medco research database. The rates of clinical events in the real world are often higher compared to rates estimated in clinical trials. If RW warfarin event rates are used as reference rates rather than those derived from trials, and if the RRRs for each NOAC vs warfarin demonstrated in the trials persist in actual clinical practice, then the associated medical cost estimates will more closely approximate RW cost reductions or increases for each NOAC compared with warfarin.
Methods
Data source
The Medco research database was used to collect data for NVAF patients receiving warfarin in a RW clinical practice. The data were administered by Medco Health Solutions, formerly a pharmacy benefits management company in the US. As of 2011, the data were available for ∼12.7 million covered lives. Along with an eligibility file, the Medco database contains fully integrated pharmacy and medical claims. The eligibility file contains demographic information and dates of health plan eligibility. The medical claims include service dates, primary and secondary International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes, and Healthcare Common Procedure Coding System (HCPCS) procedure codes for medical services. Information pertaining to the use of prescription drugs including dispense dates, National Drug Codes, quantity, and days supplied were obtained from the pharmacy claims.
Cohort identification
Patients ≥ 18 years old were selected for entry into the study if they had at least two medical claims with a primary or secondary ICD-9-CM diagnosis code indicating AF (427.31) separated by at least 30 days between January 1, 2007 and June 30, 2010. The study index date was set to the date of the first qualifying medical claim for AF. Patients with at least one prescription claim for warfarin following the study index date were further selected. Both newly diagnosed and prevalent AF cases were included in the analysis. Patients without at least 1 year of continuous enrollment in pharmacy and health benefits prior to the study index date were excluded. Patient characteristics including demographics, stroke risk measured by congestive heart failure, hypertension, age ≥ 75, diabetes, stroke (CHADS2) risk score, and comorbidities were evaluated during the baseline period, defined as 1 year prior to the index date. To match the inclusion criteria for baseline stroke risk used in the NOAC trials, patients with a CHADS2 score ≥ 1 were selected. Finally, in an attempt to match the clinical trial populations that generally excluded patients with moderate-to-severe mitral stenosis or prosthetic valves, we excluded patients with medical claims during the study period (baseline or follow-up) indicating treatment for cardiac valvular disease in order to select NVAF patients only. A total of 23,525 patients satisfied the criteria for inclusion in this analysis.
The study period started on the index date and continued until the date of disenrollment from the pharmacy or medical benefits or the end of available follow-up in the database (June 30, 2011), whichever occurred earlier. The reason for health plan disenrollment was not available in the database and may have included death.
Identifying periods of warfarin exposure
Periods of warfarin exposure were identified using previously publishedCitation21–23 methods based on prescription claims for warfarin following the study index date. A warfarin exposure period began on the date that the prescription was filled and continued until there was a gap of at least 60 days between the end of one warfarin prescription and the fill date of the next prescription. Some patients receiving warfarin before the study index date had remaining warfarin supply after the study start. For these patients, warfarin exposure was measured from the index date based on the estimated number of days supply remaining from their last prescription prior to study index.
Identification of stroke and MBEIH in real-world Medco patients
Stroke was identified in the Medco database using primary or secondary ICD-9-CM diagnosis codes appearing on inpatient hospital or emergency room (ER) claims (Appendix Table I). Due to ICD-9-CM diagnosis coding limitations, it was not possible to distinguish intracranial hemorrhages (IH) from hemorrhagic strokes as in the NOAC trials. All encounters for IH were categorized as hemorrhagic stroke. MBEIH was identified using primary or secondary diagnosis and procedure codes. Intracranial hemorrhage was excluded from major bleeding in order to avoid the double-counting of these events as both efficacy outcomes (stroke) and as safety outcomes (bleeding). All bleeding events associated with inpatient care, blood transfusion, decreased hemoglobin or hematocrit, or physician-guided medical or surgical treatment were considered major (Appendix).
Estimation of stroke and major bleeding reference rates
Unadjusted rates of stroke and MBEIH were calculated for the Medco population as follows:
Event rates from the Medco database are expressed per 100 person years (PY) of warfarin exposure.
Estimation of changes in clinical event rates and medical costs with NOACs in the real world
The absolute risk reductions (ARR) for stroke and MBEIH per 100 patient years were calculated separately for each NOAC (apixaban, dabigatran, and rivaroxaban) compared to warfarin. ARRs were estimated by multiplying the NOAC RRRs from the trials by the reference event rates. The RRRs were obtained from the ARISTOTLE, RE-LY, and ROCKET-AF trials (), while the reference event rates were observed in the RW Medco population during periods of warfarin exposure:
Table 1. Relative risk and cost inputs for stroke and major bleeding outcomes.
The calculated ARRs represent the absolute number of stroke and MBEIH events that might be avoided with each NOAC per 100 patient years. The medical costs avoided or gained with each NOAC vs warfarin were then calculated by multiplying the ARR for each event by the incremental medical costs associated with the event. Incremental medical costs were defined as the incremental costs to a US payer that would be incurred as a result of an NVAF patient experiencing a stroke or major bleeding event during 1 year following the event. The incremental medical costs for stroke and MBEIH were obtained from a study by Mercaldi et al.Citation24 as cost data were not available in the Medco database (). Since the costs of ischemic and hemorrhagic stroke were reported separately in Mercaldi et al., we calculated a combined cost of stroke by applying a weighted average to the separate cost estimates based on an assumption that strokes would occur in a ratio of 31 hemorrhagic to 69 ischemic, similar to the ratio of events observed in the warfarin arm of the ARISTOTLE trial. Medical costs were adjusted to 2011 dollars using the medical care component of the consumer price index. The medical costs avoided with each NOAC (apixaban, dabigatran, and rivaroxaban) relative to warfarin were calculated separately for stroke, MBEIH, and the net outcome of stroke and MBEIH combined. Since the objective of this study focused on the medical cost impact associated with the clinical outcomes of stroke and MBEIH, we did not take into account drug costs or INR monitoring-related expenses.
Data analyses
Numbers of events avoided and their associated medical costs were calculated for the overall population and for various sub-groups. Patient sub-groups of interest were created based on baseline CHADS2 scores (1, 2, and ≥3) and age ( < 65 years and ≥ 65 years old). Another sub-group of interest included patients with specific conditions that would have excluded them from a NOAC trial, which were referred to in this study as ‘long-term trial exclusion criteria (TEC)’. The conditions considered TEC and their administrative coding definitions are shown in the Appendix.
Univariate sensitivity analyses were also conducted to determine whether the effect of varying the RRR for an event, the corresponding incremental medical cost, or the reference event rates would significantly affect the total medical costs avoided with the use of each NOAC. The RRRs for events were varied across the ranges of their respective 95% confidence intervals. Incremental cost estimates and reference event rates were varied by ± 30% and ± 50%, respectively.
Results
Baseline characteristics
Descriptive comparisons of the baseline characteristics of NVAF patients receiving warfarin from the Medco database with patients randomized to the warfarin arms of each NOAC clinical trial are presented in . The Medco population was older compared to NOAC trial participants. The median age of patients in the Medco population was 78.0 years compared with a median age of 70.0 years and 73.0 years for patients enrolled in the ARISTOTLE and ROCKET-AF trials, respectively. The mean age of patients in RE-LY was 71.6 years (median not reported). Approximately 13% of the Medco population were <65 years old (n = 3096) and 87% were ≥ 65 years old (n = 20,429). There was a higher proportion of female patients in the Medco population (44.6%) compared with the proportions in ARISTOTLE (35.0%), RE-LY (36.7%), and ROCKET-AF (39.7%). Although the baseline risk of stroke for Medco patients based on CHADS2 scores was lower compared to any trial, the stroke risk of patients enrolled in ARISTOTLE and RE-LY more closely resembled the RW Medco population compared with ROCKET-AF. Nearly 87% of patients in ROCKET-AF had CHADS2 scores ≥3 compared with only 32.1%, 30.2%, and 21.6% of patients with CHADS2 scores ≥3 in RE-LY, ARISTOTLE, and the RW Medco population, respectively. This result was mostly a function of trial design, as ROCKET-AF included only patients with at least two risk factors for stroke (e.g., CHADS2 ≥2). 11% of Medco patients were identified as having TEC (n = 2513) that would have prevented them from being enrolled in the clinical trials.
Table 2. Baseline characteristics of NVAF patients receiving warfarin from Medco population compared with patients randomized to warfarin arm of NOAC clinical trials.
Rates of stroke and MBEIH events
The rates of stroke and MBEIH following a diagnosis of NVAF during periods of warfarin exposure were higher among Medco patients compared to those randomized to the warfarin arms of the NOAC clinical trials. Stroke rates for the Medco population were more than 3-times higher compared with the warfarin group of ARISTOTLE and RE-LY (Medco 5.3 per 100 PY, ARISTOTLE 1.5 per 100 PY, and RE-LY 1.6 per 100 PY) and more than 2-times higher compared with ROCKET-AF (Medco 5.3 per 100 PY and ROCKET-AF 2.0 per 100 PY). For MBEIH, rates of events were more than 3-times higher for Medco patients (10.0 per 100 PY) compared to warfarin arms of each clinical trial (ARISTOTLE 2.3 per 100 PY, RE-LY 2.6 per 100 PY, and ROCKET-AF 2.9 per 100 PY). Event rates among the sub-set of Medco patients with TEC (stroke 7.9 per 100 PYs, MBEIH 12.8 per 100 PYs) were even higher compared with the overall Medco population (stroke 5.3 per 100 PYs, MBEIH 10.0 per 100 PYs).
Estimated changes in clinical event rates with each NOAC in the real world
presents the absolute number of stroke and MBEIH events estimated to be avoided with the use of each NOAC compared to warfarin in the real world. We estimate that 1.1 (95% confidence interval [CI] = 0.3–1.8) stroke events per 100 PYs would be avoided with apixaban, while 1.9 (95% CI = 1.0–2.6) and 0.8 (95% CI = −0.2–1.6) stroke events per 100 PYs would be avoided with dabigatran and rivaroxaban, respectively. Treatment with apixaban instead of warfarin would result in 2.1 (95% CI = 0.7–3.2) MBEIH events avoided per 100 PYs, but a higher absolute number of MBEIH events with dabigatran (0.7 additional events per 100 PYs) and with rivaroxaban (1.4 additional events per 100 PYs).
Table 3. Estimated number of stroke and major bleeding events avoided per 100 person years of follow-up in the real world with each NOAC vs warfarin.
The number of stroke events avoided with each NOAC is greater for certain high risk sub-groups (CHADS2 ≥3, age ≥65 years, TEC) compared to the overall patient population. In contrast, while more MBEIH events are estimated to be avoided with apixaban, more MBEIH events are estimated to be incurred with rivaroxaban and dabigatran in each of these higher risk sub-groups.
The use of apixaban may provide patients with the greatest clinical benefit as it had the highest number of net clinical events (stroke plus MBEIH) avoided of all of the NOACs. Compared with warfarin per 100 PYs, we estimate that 3.2 clinical events would be avoided using apixaban, 1.2 clinical events averted with dabigatran, and 0.6 more clinical events incurred with rivaroxaban.
Estimated changes in medical costs with each NOAC in the real world
Estimation of the number of clinical events avoided or gained enables estimation of the cost impact per PY associated with use of each NOAC. The medical costs avoided with the use of apixaban instead of warfarin were $493 for stroke and $752 for MBEIH (). For dabigatran, there was $806 of medical cost savings for stroke, but $251 of additional medical costs incurred as a result of higher number of MBEIH events. For rivaroxaban, there was $358 of medical cost savings for stroke, but this was offset by $502 of additional medical costs related to MBEIH. For the combined outcomes of stroke and MBEIH, the medical costs avoided were $1245 and $555 for apixaban and dabigatran, respectively. Treatment with rivaroxaban increased combined stroke and MBEIH medical costs by $144.
Table 4. Estimated medical costs averted per patient year with use of each NOAC compared to warfarin.
For each NOAC, the medical cost savings related to stroke was greater for patients with high baseline stroke risk (CHADS2 ≥3), for the elderly (e.g., ≥65 years old), and for patients with long-term TEC compared to the overall patient population (). While the cost savings related to avoiding MBEIH events are expected to be greater for apixaban, higher MBEIH-related medical costs are estimated to be incurred with rivaroxaban and dabigatran in each of these higher risk sub-groups. For each sub-group, apixaban use had the highest combined stroke and MBEIH medical cost savings of all the NOACs examined and approximately twice the total savings achieved with dabigatran relative to warfarin. Rivaroxaban was associated with increased combined stroke and MBEIH medical costs compared to warfarin in all sub-groups. These results were consistent with results observed for the overall population.
Sensitivity analyses
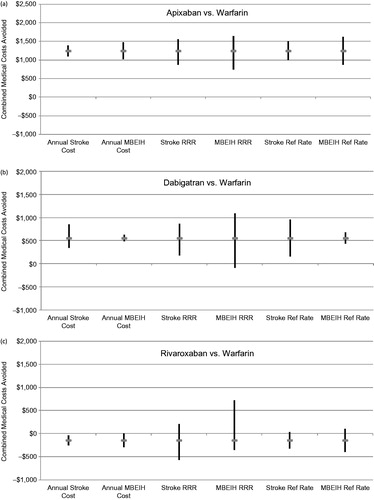
Results of univariate sensitivity analyses demonstrate consistent combined (stroke + MBEIH) medical cost savings associated with apixaban and dabigatran following variations in key study parameters (, respectively). Apixaban provided the greatest combined medical cost savings of all the NOACs for all scenarios examined and was the only NOAC for which the range of medical cost changes did not reach zero or result in increased costs relative to warfarin. Varying the RRR for stroke (range = $870–$1557), RRR for MBEIH (range = $744-$1641), and the MBEIH reference event rate (range = $870–$1624) had the greatest impact on combined stroke and MBEIH medical cost savings for apixaban. Similarly for dabigatran, varying the RRR for stroke (range = $175–$862) and RRR for MBEIH (range = −$91–$1093) had the greatest impact on combined medical cost savings. For nearly all of the scenarios examined, rivaroxaban was either associated with increased combined medical costs or only modest cost savings (). Significant combined stroke and MBEIH cost savings with rivaroxaban were only achieved at the high end of the MBEIH RRR range ($717).
Figure 1. Univariate sensitivity analyses examining the influence of variations in the relative risk reduction, annual event costs, and reference event rates on combined medical costs aoided for stroke and MBEIH; (a) Apixaban vs Warfarin, (b) Dabigatran vs Warfarin, and (c) Rivaroxaban vs Warfarin. MBEIH, major bleeding excluding intracranial hemorrhage; Ref, reference; RRR, relative risk reduction.
Net clinical events avoided were also estimated by applying a bleeding ratio of 2:1 to the calculation as a sensitivity analysis. A higher bleeding ratio indicates that patients place a higher priority on efficacy due to the higher negative impacts to quality-of-life and overall health associated with strokeCitation25. While the adjusted net clinical events avoided were higher for dabigatran (1.6) and rivaroxaban (0.1), apixaban still had the highest net clinical benefit of all of the NOACs examined (2.2 adjusted net clinical events avoided).
Discussion
This economic analysis shows that, if the RRRs demonstrated in the three NOAC trials persist in the real world, 1-year medical costs can be expected to be lower for NVAF patients using apixaban and dabigatran instead of warfarin, while medical costs for patients receiving rivaroxaban instead of warfarin can be expected to be higher. The estimated medical cost savings in a PY for the combined end-point of stroke and MBEIH was $1245 and $555 for apixaban and dabigatran, respectively, while treatment with rivaroxaban was estimated to result in $144 of additional medical costs. Medical costs avoided were calculated using reference event rates for stroke and MBEIH from 23,525 RW patients in the Medco research database receiving warfarin. The estimated impact of each NOAC relative to warfarin, as measured by changes in medical costs, may be a helpful approach in determining the value of NOACs in managing NVAF patients.
The economic analyses in this study serve to estimate the RW cost impact associated with NOAC use for NVAF based primarily on net clinical outcomes, defined as the combined outcomes of stroke and MBEIH, in terms of the combined medical costs (stroke plus MBEIH) either saved or incurred with each NOAC. Apixaban was the only NOAC examined to result in a reduction of both stroke and MBEIH events compared with warfarin. Hence, the combined medical cost savings for apixaban ($1245 per PY) was the highest of all of the NOACs evaluated. While our analysis indicates that use of dabigatran may result in the highest number of stroke events avoided compared to warfarin of all NOACs, this key advantage was largely offset by an increase in MBEIH events and associated costs for combined medical cost savings of $555 per PY. For rivaroxaban, the medical cost savings related to avoiding stroke events were offset by the additional costs associated with having higher incremental MBEIH events compared to warfarin. As a result, rivaroxaban was the only NOAC estimated to result in additional medical costs ($144 per PY).
Results of this study may be extrapolated to a hypothetical cardiology practice to gain additional insight into the total potential numbers of events avoided and resulting effect on combined costs of stroke and MBEIH. For a cardiology practice with 1000 patients, 200 of which have NVAF, it is expected that there would be 2.2 fewer strokes and 4.2 fewer MBEIH events for a total of 6.4 fewer net clinical events (stroke plus MBEIH) avoided per year with apixaban relative to warfarin. The combined medical cost savings related to stroke and MBEIH achieved with use of apixaban instead of warfarin is estimated at $249,000 per year for this practice. In the same cardiology practice, the use of dabigatran instead of warfarin is expected to result in 2.4 fewer net clinical events (3.8 fewer strokes and 1.4 additional MBEIH events) per year for cost savings of $111,000 related to stroke and MBEIH. Finally, it is estimated that use of rivaroxaban would result in an additional 1.2 net clinical events (1.6 fewer strokes but 2.8 additional MBEIH events) per year and increase medical costs related to stroke and MBEIH by $28,800 relative to warfarin.
Medical cost reductions associated with using different NOACs in place of warfarin have been estimated previouslyCitation18. However, the analyses performed by Deitelzweig et al.Citation18 were based on data obtained primarily from clinical trials and may be less generalizable to RW patients. This study adds to those analyses by estimating changes in medical costs by using reference event rates from a RW population of NVAF patients treated with warfarin. The reference risks of clinical events in the real world are often higher compared to rates estimated from clinical trials. The incorporation of RW data allowed us to estimate changes in medical costs in a RW clinical practice setting where there may be more variability in patients’ clinical characteristics and the quality of care than in a clinical trial. Deitelzweig et al.Citation18 reported combined medical cost reductions for stroke and major bleeding of −$254, −$14, and −$431 per PY for dabigatran, rivaroxaban, and apixaban, respectively (negative values indicate cost savings). Indeed, the medical cost savings estimated in our study were much higher for apixaban and dabigatran. Additionally, we report an increase in medical costs incurred with the use of rivaroxaban, where Deitelzeweig et al.Citation18 showed some modest savings. Much of these differences may be explained by the lower trial-based reference event rates used in Deitelzweig et al.Citation18.
Several recent analyses have been published examining the cost-effectiveness of apixaban 5 mg, dabigatran 150 mg, and rivaroxaban 20 mg relative to warfarinCitation26,Citation27. In Harrington et al.Citation27, all of the NOACs met the $50,000 per quality adjusted life-year (QALY) threshold for treating NVAF patients ≥ 70 years old and CHADS2 scores ≥ 1. However, the authors concluded that apixaban was preferred after results of probabilistic sensitivity analyses indicated it was most likely to be cost-effective at the $50,000 per QALY and $100,000 per QALY thresholds. The study conducted by Canestaro et al.Citation26 also found that apixaban was the optimal strategy at a cost-effectiveness threshold of $100,000 per QALY. Similarly, results of this study indicate that apixaban may be the preferred choice for anticoagulation in NVAF from an economic standpoint.
An important assumption used in this analysis of changes in medical costs associated with each NOAC was that the RRRs observed in each of the RCTs would persist in a RW setting. This assumption is widely accepted and is the basis for many policy decisions regarding whether a drug should be added to a formulary. The reference (or baseline) rates of events on the other hand may not be broadly generalizable to RW practice settingsCitation20. In fact, the risks of major bleeding and stroke are consistently reported to be higher in RW settings. This is likely explained by several factors. For example, it is common for clinical trials to enroll ‘healthier’ patients by excluding those with advanced disease or who have higher risks of adverse events. Indeed, sub-group analyses conducted as a part of this study revealed that event rates among patients with long-term TEC were 50% and 28% higher for stroke and MBEIH, respectively, compared to the overall Medco population. Clinical trial patients must also follow strict treatment protocols and, as a result, are evaluated more frequently by healthcare providers. Another relevant difference between clinical trials and RW experience is the quality of warfarin management, reflected by the TTR calculation. In the ARISTOTLE and RE-LY trials, warfarin management was generally better than the average US practice (median time in therapeutic range [TTR]: 66% in ARISTOTLE, 67% in RE-LY, and mean TTR: 57% in general US practiceCitation28, whereas in the ROCKET-AF trial the quality of warfarin control (median TTR: 58%) was similar to levels observed in RW practices.
This study was also subject to limitations concerning the estimation of stroke and major bleeding rates. Administrative ICD-9-CM diagnosis and Common Procedural Terminology (CPT)-4 procedure codes on medical claims were used to identify stroke and major bleeding events instead of confirmatory clinical data. Administrative codes are primarily used for rendering payments to physicians and other healthcare providers rather than research purposes. Therefore, diagnostic and procedure coding errors are possible and even correct codes in certain cases could have represented ‘rule-out’ diagnoses. In creating the coding definitions for defining outcome events in the Medco data, we sought to define events so that they would provide as close a match as possible to the definitions used in the RCTs. However, due to our reliance on the diagnostic and procedural codes appearing on the claims, it is possible that some events identifiable in the trials would not be picked up in a healthcare claims database. Outcomes created using the Medco data were defined using codes appearing on hospital admission or ER visit claims for stroke and codes appearing on either hospital admission, outpatient hospital visit, or ER claims for MBEIH. Some stroke events may not have been counted in the Medco data if they did not result in an ER visit or hospital stay. Therefore, there is the possibility of under-estimating the occurrence of events in some instances. Alternatively, there may have been some claims for follow-up care for events occurring prior to the study index date that could have been misclassified as a new stroke or bleeding event. However, we expect this bias to be limited as most follow-up care was likely to occur during a physician office visit and these claims were not included in study event definitions.
In estimating the changes in medical costs associated with each NOAC, this analysis focused on 1-year medical costs of stroke and MBEIH. INR monitoring and drug costs were not included in this study. Further research is needed to more fully evaluate the total cost differences between NOACs relative to warfarin and include drug costs, INR monitoring, office visit, laboratory testing, indirect costs, and long-term costs. Results of several cost effectiveness analyses examining NOACs have established that, despite having higher costs, they are cost-effective relative to warfarin for NVAFCitation22–26.
This study was subject to additional limitations common to many retrospective database analyses. Periods of warfarin use were inferred from the fill dates appearing on prescription claims. It was also assumed that patients were compliant with their prescriptions in assessing periods of warfarin use. In addition, the complexity of warfarin dose adjustments may have affected our ability to accurately assess periods of warfarin exposure. As a result, some major bleeding and stroke events may have been misclassified as occurring during warfarin use. It was not possible to distinguish between IH and hemorrhagic stroke due to ICD-9-CM diagnosis coding limitations. We assumed that healthcare encounters for IH would have occurred because a patient received treatment due to a neurological deficit and, thus, classified these encounters as hemorrhagic stroke. Finally, the Medco database did not include information regarding laboratory results. Therefore, the level of anticoagulation (target INR and time in therapeutic range) could not be determined for the Medco population. However, since the rates of stroke and major bleeding were much higher in the Medco population compared to RCTs, one could probably speculate that the level of control was inferior to trial participants.
Conclusion
This analysis suggests that, if the relative risk reductions from the NOAC clinical trials persist in the real world, the use of apixaban and dabigatran may be associated with a reduction in medical costs (not including INR or drug costs), while rivaroxaban may be associated with an increase in medical costs when used in place of warfarin in a RW, NVAF, managed-care patient population. The use of apixaban may be associated with the highest medical cost reduction, driven by the reduction of both stroke and MBEIH relative to warfarin.
Transparency
Declaration of funding
This research was supported by Bristol-Myers Squibb and Pfizer.
Declaration of financial/other relationships
D.M. and J.L. are full-time employees of Bristol-Myers Squibb and own stock in the company. D.W. is a full-time employee of Pfizer Inc. and owns stock in the company. M.S. and N.W. are full-time employees of Evidera, which received funding from Bristol-Myers Squibb and Pfizer for services performed in connection with the development of this study and manuscript. In this salaried position, they work with a variety of companies and organizations. They receive no payment or honoraria directly from these organizations for services rendered. A.A. is a consultant for Evidera in connection with this research. JME peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Supplementary Appendix Table 1. Administrative Codes used to identify Stroke, Major Bleeding, and Long-term Trial Exclusion Criteria in the Medco Database
Download PDF (22.5 KB)Acknowledgments
The authors wish to acknowledge Luke Boulanger for his leadership contributions to study design and execution. We would also like to acknowledge Nancy Brady for editorial support and review of this manuscript. Finally, the authors wish to thank Elyse Gatt for her contributions to this study. Luke Boulanger and Nancy Brady are full-time employees of Evidera, which received funding from Bristol-Myers Squibb and Pfizer for services performed in connection with the development of this manuscript. Elyse Gatt is a former Evidera employee.
References
- Miyasaka Y, Barnes ME, Gersh BJ, et al. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation 2006;114:119-25
- Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation: a major contributor to stroke in the elderly. The Framingham Study. Arch Intern Med 1987;147:1561-4
- Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke 1991;22:983-8
- American Heart Association (AHA). What is Atrial Fibrillation (AFib or AF)? 2014. http://www.heart.org/HEARTORG/Conditions/Arrhythmia/AboutArrhythmia/What-is-Atrial-Fibrillation-AFib-or-AF_UCM_423748_Article.jsp. Accessed April 25, 2013
- Gladstone DJ, Bui E, Fang J, et al. Potentially preventable strokes in high-risk patients with atrial fibrillation who are not adequately anticoagulated. Stroke 2009;40:235-40
- Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA 2001;285:2370-5
- Stettin GD. Treatment of nonvalvular atrial fibrillation. West J Med 1995;162:331-9
- Ali A, Bailey C, Abdelhafiz AH. Stroke prevention with oral anticoagulation in older people with atrial fibrillation - a pragmatic approach. Aging Dis 2012;3:339-51
- Coyne KS, Paramore C, Grandy S, et al. Assessing the direct costs of treating nonvalvular atrial fibrillation in the United States. Value Health 2006;9:348-56
- The effect of low-dose warfarin on the risk of stroke in patients with nonrheumatic atrial fibrillation. The Boston Area Anticoagulation Trial for Atrial Fibrillation Investigators. N Engl J Med 1990;323:1505-11
- Secondary prevention in non-rheumatic atrial fibrillation after transient ischaemic attack or minor stroke. EAFT (European Atrial Fibrillation Trial) Study Group. Lancet 1993;342:1255-62
- Adjusted-dose warfarin versus low-intensity, fixed-dose warfarin plus aspirin for high-risk patients with atrial fibrillation: Stroke Prevention in Atrial Fibrillation III randomised clinical trial. Lancet 1996;348:633-8
- Connolly SJ, Laupacis A, Gent M, et al. Canadian Atrial Fibrillation Anticoagulation (CAFA) Study. J Am Coll Cardiol 1991;18:349-55
- Ezekowitz MD, Bridgers SL, James KE, et al. Warfarin in the prevention of stroke associated with nonrheumatic atrial fibrillation. Veterans Affairs Stroke Prevention in Nonrheumatic Atrial Fibrillation Investigators. N Engl J Med 1992;327:1406-12
- Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 2009;361:1139-51
- Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med 2011;365:981-92
- Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med 2011;365:883-91
- Deitelzweig S, Amin A, Jing Y, et al. Medical cost reductions associated with the usage of novel oral anticoagulants vs warfarin among atrial fibrillation patients, based on the RE-LY, ROCKET-AF, and ARISTOTLE trials. J Med Econ 2012;15:776-85
- Britton A, McKee M, Black N, et al. Threats to applicability of randomised trials: exclusions and selective participation. J Health Serv Res Policy 1999;4:112-21
- Caro JJ, Migliaccio-Walle K. Generalizing the results of clinical trials to actual practice: the example of clopidogrel therapy for the prevention of vascular events. CAPRA (CAPRIE Actual Practice Rates Analysis) Study Group. Clopidogrel versus Aspirin in Patients at Risk of Ischaemic Events. Am J Med 1999;107:568-72
- Amin A, Stokes M, Wu N, et al. Application of randomized clinical trial data to actual practice: apixaban therapy for reduction of stroke risk in non-valvular atrial fibrillation patients. Curr Med Res Opin 2013;29:1253-61
- Amin A, Stokes M, Wu N, et al. Estimated medical cost reductions associated with apixaban in real-world patients with non-valvular atrial fibrillation. J Med Econ 2013;16:1193-202
- Boulanger L, Hauch O, Friedman M, et al. Warfarin exposure and the risk of thromboembolic and major bleeding events among medicaid patients with atrial fibrillation. Ann Pharmacother 2006;40:1024-9
- Mercaldi CJ, Ciarametaro M, Hahn B, et al. Cost efficiency of anticoagulation with warfarin to prevent stroke in medicare beneficiaries with nonvalvular atrial fibrillation. Stroke 2011;42:112-18
- LaHaye SA, Gibbens SL, Ball DG, et al. A clinical decision aid for the selection of antithrombotic therapy for the prevention of stroke due to atrial fibrillation. Eur Heart J 2012;33:2163-71
- Canestaro WJ, Patrick AR, Avorn J, et al. Cost-effectiveness of oral anticoagulants for treatment of atrial fibrillation. Circ Cardiovasc Qual Outcomes 2013;6:724-31
- Harrington AR, Armstrong EP, Nolan PE Jr, et al. Cost-effectiveness of apixaban, dabigatran, rivaroxaban, and warfarin for stroke prevention in atrial fibrillation. Stroke 2013;44:1676-81
- Ansell J, Hollowell J, Pengo V, et al. Descriptive analysis of the process and quality of oral anticoagulation management in real-life practice in patients with chronic non-valvular atrial fibrillation: the International Study of Anticoagulation Management (ISAM). J Thromb Thrombolysis 2007;23:83-91
