Abstract
Objective:
Publications containing recent, real-world data on the economic impact of hip fractures in the UK are lacking. This retrospective electronic medical records database analysis assessed medication and healthcare resource use, direct healthcare costs, and factors predicting increased resource use and costs in adult UK hip fracture patients.
Methods:
Data were obtained from the Clinical Practice Research Datalink linked to the Hospital Episode Statistics for adult patients hospitalized for their first hip fracture between January 1, 2006 and March 31, 2011 (index event); healthcare costs were calculated from the National Health Service perspective using 2011–2012 cost data.
Results:
Data from 8028 patients were analyzed. Resource use and costs were statistically significantly higher in the year following fracture (mean total [standard deviation (SD)] cost £7359 [£14,937]) compared with the year before fracture (mean total [SD] cost £3122 [£9435]; p < 0.001), and were similar to the total amount of the index hospitalization (mean total [SD] cost £8330 [£2627]). Multivariate regression analysis (using an estimated generalized linear model) showed that older age, male gender, higher comorbidity, osteoporosis, discharge to another institution compared with home, and pre-index hospitalization and outpatient visits were associated with increased post-index hospitalization healthcare costs (all p < 0.05).
Conclusions:
Although we did not capture all pre- and post-index costs and healthcare utilization, this study provides important insights regarding the characteristics of patients with hip fracture, and information that will be useful in burden-of-illness and economic analyses.
Introduction
Hip fracture rates vary considerably worldwide, but are very high in northwestern Europe. One estimate for 2010 of the age-adjusted annual incidence of hip fractures in women in the UK was more than 300/100,000 population, with rates in men being approximately half that in womenCitation1. Another estimate of age-standardized hip fracture rates in England was 418.2 per 100,000 women and 143.6 per 100,000 menCitation2. Geographical region, age, and menopausal status affect the risk of hip fracture among womenCitation1–3. The risk of hip fracture increases once women reach the menopause and, in post-menopausal women, the incidence of hip fracture was found to increase steeply with ageCitation3. The incidence of hip fractures is therefore expected to increase as the population agesCitation4.
Hip fractures are not only common, but are also serious consequences of falls in the elderlyCitation5, resulting in substantial mortality, morbidity, reduced ability to perform activities of daily living, mobility limitations that result in muscle atrophy or weakness (MAW), and reduced quality-of-lifeCitation6–11. Many hip fracture patients are already frail; for these patients, a hip fracture may mean the loss of their independence and possibly placement in a nursing homeCitation4,Citation8.
The cost of caring for hip fracture patients is high. When both acute care for the fracture and care during subsequent dependency were taken into account, estimated costs were more than £2 billion a year in the UKCitation4,Citation12. The economic impact of hip fractures is likely to increase as the global population agesCitation4,Citation13,Citation14.
Currently available data on the economic impact of hip fractures in the UK are mostly derived from clinical trials or are outdated. Recent estimates from the ‘real-world’ clinical setting are therefore limited. For example, using data from clinical trials and a database, Bouee et al.Citation15 estimated that, in the UK, the cost of initial treatment of hip fracture plus rehabilitation was £6224. This estimate was based on 2002 costs. Using 2003 costs and analyzing data from a small sample of 100 hip fracture patients, Lawrence et al.Citation16 reported the mean cost of the index hospitalization to be £12,163. Older data (1999/2000 costs) were used by the National Health Service (NHS) Health and Technology Assessment in their cost–utility analysis of osteoporosis treatment. This organization estimated that uncomplicated osteoporotic hip fractures in the UK cost £7398 for the year following fractureCitation17. More recently, in a study that considered only elderly care home residents (mean [standard deviation (SD)] age 85 [9] years), the median cost of the index hospitalization for hip fracture in the UKCitation18 was £9429 (2006 costs). The UK National Hip Fracture Database (NHFD) does not report costsCitation4. Thus, gaps exist in our understanding of the current economic impact of hip fractures in the UK.
The objectives of this study were to explore medication and healthcare resource use and direct healthcare costs among UK hip fracture patients, and to investigate the factors that might predict an increase in resource use and costs. All patients with hip fracture were included, regardless of the reason for the fracture.
Methods
Study design and data sources
This was a retrospective database analysis. Data for patients with hip fracture in the UK were extracted from electronic medical records held on the Clinical Practice Research Datalink (CPRD)Citation19 that were linked to the Hospital Episode Statistics (HES)Citation20. The CPRD contains longitudinal data from 630 general practitioner (GP) practices and covers ∼8% of the UK population. CPRD diagnoses are recorded using the Read coding system that includes terms relating to observations (signs and symptoms), diagnoses, procedures, and laboratory and radiology testsCitation21. The HES contains details of all admissions to NHS hospitals in England, using the International Classification of Diseases, Tenth Edition (ICD-10), coding system for diagnosisCitation22, and includes information on inpatient hospitalizations and day cases delivered to all patients by treatment centers funded by the NHS plus healthcare utilization by NHS patients treated in the independent sector but commissioned by the NHS. The CPRD is linked with the HES for English practices only; of the 465 practices represented in the CRPD, 244 (52%) are linked to HES.
This study was conducted from the perspective of the English NHS using 2011 costs. Unit costs from available English resources were applied to estimate direct healthcare costs; these resource costs included NHS reference costs for 2011–2012Citation23, medication costs from the British National FormularyCitation24 and NHS Drugs TariffsCitation25, and unit costs for 2011Citation26.
No ethical committee approval was required; Independent Scientific Advisory Committee approval was obtained for research involving CPRD data.
Study population
Adult patients, regardless of age and underlying disease, being hospitalized for the first time between January 1, 2006 and March 31, 2011 for hip fracture (ICD-10: S72 or M84.4) (the index event) with no previous hip fracture 7 days to 1 year pre-index and with computerized HES data available for 1-year pre-index hospital admission and 1-year post-index hospital discharge were eligible for entry to the study.
Study variables
Data for the following study variables were extracted from the linked CPRD and HES.
Information relating to the index hospitalization included patient demographics and characteristics (e.g., age, gender, and body mass index [BMI]) identified using diagnostic records dated 1 year prior to the index stay. The extent of overall comorbidity was measured using the original Charlson Comorbidity Index (CCI)Citation27 (to enable comparison with published data) and with an updated version that complies with UK guidelines. Unlike the original CCI, the updated version uses new weightings that are based on ICD-10 codesCitation28. The CCI can be used for patients of all ages and is the most commonly used measure of the extent of overall comorbidity in health outcomes studiesCitation29; a score is assigned according to disease severity, with a higher score indicating greater severityCitation27. An aggregate score can be used to predict 1-year mortalityCitation27. The original CCI is scored from 1–6 and the updated CCI is scored from 0–5+. In addition, musculoskeletal-related comorbidities that have an impact on the care of patients with hip fracture (e.g., MAW, osteoarthritis, rheumatoid arthritis, and osteoporosis) were investigated to assess their impact on patient health, healthcare utilization, and costs. Healthcare resource use data included length of stay, healthcare provider specialty, specific procedures performed, and discharge information.
Healthcare resource use data were extracted for the 1-year pre-index hospitalization and 1-year post-index hospitalization periods. The healthcare resource use data included osteoarthritis-related and osteoporosis-related prescription drug use, GP/nurse/specialist consultations, inpatient stays, emergency department visits, laboratory and imaging tests, and (for the post-index period) subsequent fractures and surgeries.
During all the relevant assessment periods, healthcare costs for inpatient, outpatient/GP practice, and pharmacy costs were obtained by multiplying the mean usage of hip-fracture-related resources by their corresponding unit costs; these healthcare costs included those identified as hip-fracture-related rather than all-cause healthcare costs. Data on prescription costs during inpatient stays (for both the index and other hospitalizations) were not available, so were not included.
Statistical analysis
Descriptive statistics were used to summarize study variables; means and SDs for continuous variables, and numbers (%) for categorical variables are presented. Pre-index period costs were compared with post-index period costs using two-sided t-tests. A generalized linear model (GLM) with a gamma distribution and log link function was used to identify factors associated with hospitalization healthcare costs incurred during the post-index year. Given the highly skewed distribution of healthcare cost data, in which a small percentage of patients may incur high costs, the GLM is highly recommended as a modeling approachCitation30–33. Regression coefficients from the GLM quantify the relationship between 12-month post-index costs and selected patient characteristics. These are presented in the exponentiated form using a base of e, and coefficients represent the percentage increase/decrease in costs compared with patients without that characteristic. Exponentiated coefficients (95% confidence intervals) and p-values from the GLM analysis are presented.
Factors that were investigated included age, gender, CCI, presence of MAW, total joint arthroplasty/hip-fracture-related comorbidities, discharge status from index hospitalization, and hospitalizations, emergency department visits, and outpatient visits in the pre-index period.
Analysis of the descriptive statistics was conducted using SAS version 9.2 (SAS Institute Inc., Cary, NC), and the GLM analysis was conducted using STATA version 11 (StataCorp, College Station, TX).
Results
Patients
A total of 25,428 patients were identified in the CRPD/HES database as hospitalized for hip fracture in the study period; of these, 8028 patients met all inclusion criteria and were included in the analyses (). The baseline demographics, clinical characteristics and comorbidities of the eligible hip fracture patients are summarized in . Most patients (73.7%) were aged 75 years or older; only 11.5% of patients were aged 18–65 years. Overall, 75.8% of the study population was female, and most patients were not overweight or obese (83.3% had BMI < 25 kg/m2). The most common comorbidities recorded during the year before hip fracture were osteoarthritis, pulmonary disease, renal disease, osteoporosis, and cancer.
Figure 1. Selection of the study sample of UK patients with hip fracture from the Clinical Practice Research Datalink (CPRD) linked to the Hospital Episode Statistics (HES).
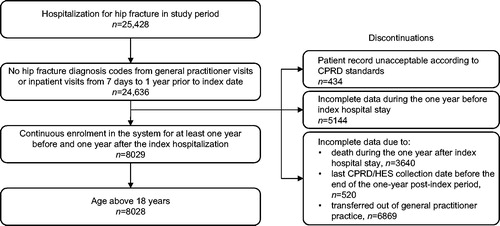
Table 1. UK hip fracture patients: demographics and clinical characteristics at the index hospitalization, and comorbidities recorded during the year before index hospitalization.
Resource use
Resource use in the year prior to hip fracture is summarized in . The use of pain relief medications was common, with opioids and paracetamol being the most commonly prescribed medications. Bisphosphonate use was low (used in 13.4% of patients). During the year prior to hip fracture, most patients made frequent GP surgery visits; 90.7% of patients had made at least one GP surgery visit, with a mean (SD) of 7.37 (8.22) visits per patient. A total of 35.3% of patients had had at least one inpatient stay and the mean (SD) number of inpatient days per patient was 5.67 (20.41).
Table 2. Pre-index hospitalization resource use among UK hip fracture patients.
Index hospitalization characteristics and resource use are summarized in . The mean length of stay was 19.53 (18.84) days; the median length of stay was 14.00 (interquartile range: 9.00–23.00) days. Most patients (97.5%) were treated by trauma and orthopedics specialists, and only a small percentage of patients (10.2%) were treated by rehabilitation specialists; the total percentage is greater than 100% because patients could be treated in multiple specialties. Non-arthroplasty procedures were performed in 33.7% of patients, partial hip arthroplasty was performed in 38.5% and total hip arthroplasty was performed in only 5.1% of patients. After this index hospitalization for hip fracture, most patients (73.1%) were discharged to their place of residence.
Table 3. Index hospitalization characteristics and resource use among UK hip fracture patients.
Medication and resource use, and subsequent fractures and surgeries in the year following hospitalization for hip fracture, are summarized in . Pain relief continued to be commonly used in the post-index period. Paracetamol, opioid and bisphosphonate use was high, with these agents being used by 56.3%, 46.2%, and 45.9% of patients, respectively. GP visits continued to be common: 92.0% of patients had at least one GP surgery visit, with a mean of 7.34 (7.29) visits per patient, and 31.7% of patients had a home visit by a GP. A total of 50.5% of patients had at least one inpatient stay, with a mean of 13.30 (30.43) days per stay. The incidence of subsequent fractures in the following year and subsequent surgery was low: the most common subsequent fracture was hip fracture (in 5.7% of patients) and the most common subsequent surgery was partial hip arthroplasty (in 3.4% of patients).
Table 4. Post-index hospitalization resource use among UK hip fracture patients.
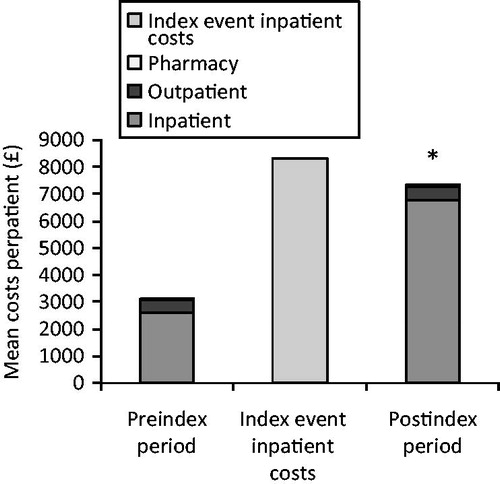
Costs for the three periods are summarized in . Mean (SD) total healthcare costs per patient for the year prior to fracture were £3122 (£9435), comprising inpatient costs of £2603 (£9349) (representing 83% of the total cost), outpatient costs of £461 (£467) (15% of the total cost) and pharmacy costs of £57 (£170) (2% of the total cost). Mean (SD) total healthcare costs per patient for the index hospitalization were £8330 (£2627). Mean (SD) total healthcare costs per patient for the year following fracture were £7359 (£14,937), comprising inpatient costs of £6746 (£14,864) (representing 92% of the total cost), outpatient costs of £532 (£466) (7% of the total cost), and pharmacy costs of £81 (£244) (1% of the total cost). Mean inpatient, outpatient, pharmacy, and total costs in the post-index period all were statistically significantly higher vs the corresponding pre-index costs (p < 0.001).
Figure 2. Pre-index, index, and post-index hospitalization resource costs among UK hip fracture patients (n = 8028). *p Value < 0.001 for all post-index costs vs pre-index costs.
The GLM analysis results for post-index hospitalization healthcare costs are summarized in . Variables associated with significantly higher post-index hospitalization healthcare costs included older age (>65 years vs 18–64 years: 30% increase in costs), higher updated CCI score (5+ vs 0: 31% increase), comorbid osteoporosis (vs no osteoporosis: 20% increase), being discharged to another institution rather than home (e.g., discharged to hospital, nursing home, residential care, or group home: 68–308% increase), pre-index hospitalization (vs no pre-index hospitalization: 4% increase), and pre-index outpatient visits (vs no pre-index outpatient visits: 3% increase) (an overall measure of the number of visits) (all p < 0.05). Compared with males, female gender was associated with a significant 11% decrease in total post-index hospitalization costs.
Table 5. Regression results for factors associated with increased or decreased post-index hospitalization healthcare costs among UK hip fracture patients.
Discussion
This retrospective database study provides information on patient characteristics and recent estimated costs, and important insights regarding the surgical management and resource use during the hospitalization period associated with the hip fracture and during the 1-year periods prior to and following the index hospitalization among patients experiencing a hip fracture in the UK. Variables associated with an increase in resource use and costs in the year following hip fracture were also identified.
As expected, the patients we identified were predominantly women (75.8%), in line with percentages of 74–77% reported in other studies in UK patients with hip fractureCitation4,Citation16. Our patients were mainly elderly, with 73.7% aged 75 years or older and a mean age of 79.05 years, which is slightly younger than reported in the other UK studies, but is to be expected as the previous studies included only elderly patients in their assessmentsCitation4,Citation16,Citation34. A total of 22.1% of the patients we identified had osteoporosis. Overall comorbidity, as indicated by a mean (SD) CCI original score of 2.13 (2.00), was higher than the original CCI score of 1.2 (SD = 1.3) among patients in the study by Gutiérrez et al.Citation34, indicating that patients had greater comorbidity in the present study.
With regard to resource use, GP visits during the pre- and post-index periods were high, as expected, but home visits by healthcare providers were more common after hip fracture, indicating ongoing health problems following this event (see and ). Inpatient stays were also more common post-index, confirming the ongoing health problems following hip fracture, and highlighting that some of these problems were severe enough to warrant hospital admission and bringing into question whether discharge home for 73.1% of patients was appropriate. While encouraging patients to return home is important on a number of levels, this finding suggests that more could be done to support these patients. However, the occurrence of subsequent fractures was low (5.7% of patients had a subsequent hip fracture), a finding in line with the 5.1% of patients who had at least one subsequent fracture in the study by Gutiérrez et al.Citation34. The occurrence of subsequent surgeries was also low, indicating that arthroplasty revisions were not often required. Bisphosphonate use was higher in the post-index period than in the pre-index period (used by 45.9% vs 13.4% of patients, respectively). The increase in bisphosphonate use in the post-index period suggests that the hip fracture event prompted the prescription of these anti-osteoporotic agents. This low overall prescription of bisphosphonates is in line with the finding that bone protection therapy is under-utilized for the secondary prevention of fragility fractures in the UKCitation35.
That increased healthcare resource use increases costs is clear. Consideration of pre- and post-index costs revealed that total healthcare costs were numerically higher in the year following hip fracture than during the year before hip fracture. In both of these periods, the main driver was inpatient costs, although these appeared substantially higher in the post-index period than in the pre-index period. The post-index costs were similar to those of the index hospitalization costs, and it is possible that the high post-index costs were associated with post-fracture recovery and other complications. Length of stay for the index hospitalization was 19.53 days in the present study, which is similar to that reported in the NHFD report (20 days)Citation4 and in the study by Lawrence et al.Citation16 (23 days). A total of 5.1% of patients received a total hip arthroplasty, which is lower than the 15.6% of patients in the NHFD reportCitation4.
Comparison of findings relating to cost, resource use, and patient characteristics was hampered by limited data suitable for comparison, as the present study differed from many other studies with regard to methods, year of cost data, time periods, databases, and patient populationsCitation4,Citation15,Citation16,Citation18,Citation34. Bearing these differences in mind, comparison of the findings of the present study with published studies revealed some similarities and some differences. Mean total healthcare cost per patient for the index hospitalization in the current study was £8330. This was lower than the mean cost of £12,163 (2003 costs) reported for the index hospitalization for a small sample of 100 hip fracture patients reported by Lawrence et al.Citation16, and closer to, but still lower than, the median cost per patient for the index hospitalization for hip fracture of £9429 (2006 costs) reported by Sahota et al.Citation18 for elderly care home residents. The mean total healthcare cost per patient for the year following fracture was £7359, which is similar to the estimated cost of £7398 for uncomplicated osteoporotic hip fractures used in the cost–utility analysis of osteoporosis treatment in the UK NHS Health and Technology AssessmentCitation17. However, this latter estimate was for 1999/2000 costs and was limited to osteoporotic fractures; more recent costs would be expected to be higher. The choice of the database used for healthcare resource and economic analyses is important as it can influence findings. The present study used directly linked data from the CPRD and the HESCitation21,Citation22, whereas Gutiérrez et al.Citation34 used data from the Health Improvement Network (THIN) research database, in which data linking is indirect and, therefore, likely to be less precise. The direct link between the CPRD and HES is considered a strength of the present study.
The findings of the regression analysis indicated that variables associated with higher costs included older age, higher CCI score, comorbid osteoporosis, being discharged to another institution instead of home, and pre-index hospitalization and outpatient visits. Given that inpatient costs were the main driver of total costs in the present study, our findings are in line with other studies which have demonstrated that factors such as older age, frailty, greater comorbidity, and living in an institution predicted longer inpatient staysCitation36,Citation37.
Limitations that should be kept in mind when considering the findings of this study are as follows. The low percentage of hip fracture cases that were identified as surgically managed (77%) suggests that some surgical repair procedures were not well captured. ‘Non-arthroplasty procedures’ includes only the following: primary reduction of intra-articular fracture of bone using arthrotomy as approach; primary open reduction of fracture of neck of femur and open fixation using pin and plate (including primary open reduction of fracture of neck of femur and open fixation using dynamic hip screw); closed reduction of fracture of bone and internal fixation; application of internal fixation to bone, not elsewhere classified; and manipulation of fracture of bone and skeletal traction, not elsewhere classified. It has been assumed that data for England HES are representative of the whole UK. Unit costs from available English resources were applied to estimate direct healthcare costs. Under-reporting of some inpatient procedures in the HES is likely; laboratory and imaging procedures, use of rehabilitation services, and specialist outpatient visits, for example, were probably under-reported in HES, resulting in an under-estimation of costs. Social services and indirect costs incurred by patients were not captured in any of the datasets, so have not been included in the analysis. However, whereas pre- and post-index costs do not capture total healthcare utilization in terms of surgeries and medications, they do capture hip-fracture-related utilization. Despite this limitation, this study provides important insights regarding the characteristics of patients experiencing a hip fracture in the UK.
Conclusion
Healthcare resource use and associated costs were higher in the 1-year period post-hip fracture compared with the 1-year period before hip fracture and were similar to those of the index hospitalization. Variables associated with an increase in resource use and costs during the year following hospitalization for hip fracture included older age, female gender, higher CCI score, comorbid osteoporosis, discharge to another institution instead of home, and pre-index hospitalization and outpatient visits. This information will be useful in burden-of-illness and economic analyses and may help to identify patients likely to require increased healthcare resource use.
Transparency
Declaration of funding
This study was funded by Eli Lilly and Company. The study sponsor participated in the data analysis.
Declaration of financial/other relationships
R. B. and M. S. are employees of and shareholders in Eli Lilly and Company. D. L., M. R-C., S. C., and N. W. are employees of Evidera, the company contracted by Eli Lilly and Company to perform this research.
Acknowledgments
The authors would like to acknowledge Sarah Smith and Caroline Spencer (Rx Communications, Mold, UK) for medical writing assistance with the preparation of this article, funded by Eli Lilly and Company. JME peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
References
- Kanis JA, Odén A, McCloskey EV, et al; IOF Working Group on Epidemiology and Quality of Life. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 2012;23:2239-56
- Dhanwal DK, Dennison EM, Harvey NC, et al. Epidemiology of hip fracture: worldwide geographic variation. Indian J Orthop 2011;45:15-22
- Banks E, Reeves GK, Beral V, et al; Million Women Study Collaborators. Hip fracture incidence in relation to age, menopausal status, and age at menopause: prospective analysis. PLoS Med 2009;6:e1000181
- The National Hip Fracture Database. London: Royal College of Physicians, 2012. www.nhfd.co.uk. Accessed January 20, 2014
- Bell AJ, Talbot-Stern JK, Hennessy A. Characteristics and outcomes of older patients presenting to the emergency department after a fall: a retrospective analysis. Med J Aust 2000;173:179-82
- Bass E, French DD, Bradham DD, et al. Risk-adjusted mortality rates of elderly veterans with hip fractures. Ann Epidemiol 2007;17:514-19
- Bliuc D, Nguyen ND, Milch VE, et al. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA 2009;301:513-21
- Braithwaite RS, Col NF, Wong JB. Estimating hip fracture morbidity, mortality and costs. J Am Geriatr Soc 2003;51:364-70
- Hopley C, Stengel D, Ekkernkamp A, et al. Primary total hip arthroplasty versus hemiarthroplasty for displaced intracapsular hip fractures in older patients: systematic review. BMJ 2010;340:c2332
- Wolinsky FD, Fitzgerald JF, Stump TE. The effect of hip fracture on mortality, hospitalization, and functional status: a prospective study. Am J Public Health 1997;87:398-403
- Zhao Y, Chen SY, Lee YC, et al. Clinical and economic characteristics of hip fracture patients with and without muscle atrophy/weakness in the United States. Arch Osteoporos 2013;8:127
- Burge RT, Worley D, Johansen A, et al. The cost of osteoporotic fractures in the UK: projections for 2000–2020. J Med Econ 2001;4:51-62
- Bergström U, Jonsson H, Gustafson Y, et al. The hip fracture incidence curve is shifting to the right. Acta Orthop 2009;80:520-4
- Turkington P, Mcdonald S, Elliott J, et al. Hip fracture in Northern Ireland, 1985–2010. Are age-specific fracture rates still rising? Ulster Med J 2012;81:123-6
- Bouee S, Lafuma A, Fagnani F, et al. Estimation of direct unit costs associated with non-vertebral osteoporotic fractures in five European countries. Rheumatol Int 2006;26:1063-72
- Lawrence TM, White CT, Wenn R, et al. The current hospital costs of treating hip fractures. Injury 2005;36:88-91
- Kanis JA, Brazier JE, Stevenson M, et al. Treatment of established osteoporosis: a systematic review and cost-utility analysis. Health Technol Assess 2002;6:1-146
- Sahota O, Morgan N, Moran CG. The direct cost of acute hip fracture care in care home residents in the UK. Osteoporos Int 2012;23:917-20
- Clinical practice research datalink. London: National Institute for Health Research, http://www.cprd.com/home. Accessed January 20, 2014
- Hospital episode statistics. Leeds, UK: Health & Social Care Information Centre, http://www.hscic.gov.uk/hes. Accessed January 20, 2014
- Read codes. Leeds, UK: Health & Social Care Information Centre, http://systems.hscic.gov.uk/data/uktc/readcodes. Accessed January 20, 2014
- ICD 10 classification. Leeds, UK: Health & Social Care Information Centre, http://systems.hscic.gov.uk/data/clinicalcoding/codingstandards/icd10. Accessed January 20, 2014
- Reference costs 2011-12. London: Department of Health, 2012. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/213060/2011-12-reference-costs-publication.pdf. Accessed January 20, 2014
- British National Formulary. London, UK: BMJ Publishing Group Ltd and the Royal Pharmaceutical Society of Great Britain, http://www.bnf.org/bnf. Accessed January 20, 2014
- Drug tariffs. Surrey, UK: National Health Service Business Services Authority, http://www.ppa.org.uk/ppa/edt_intro.htm. Accessed January 20, 2014
- Curtis L. Unit costs of health and social care 2011. Kent, UK: Personal Social Services Research Unit, 2011. http://www.pssru.ac.uk/pdf/uc/uc2011/uc2011.pdf. Accessed January 20, 2014
- Charlson ME, Charlson RE, Peterson JC, et al. The Charlson comorbidity index is adapted to predict costs of chronic disease in primary care patients. J Clin Epidemiol 2008;61:1234-40
- Indicator specification: summary hospital-level mortality indicator. Leeds, UK: Health & Social Care Information Centre Clinical Indicators Team, 2013. http://www.hscic.gov.uk/CHttpHandler.ashx?id=11151&p=0. Accessed January 20, 2014
- Thygesen SK, Christiansen CF, Christensen S, et al. The predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish National Registry of Patients. BMC Med Res Methodol 2011;11:83
- Blough D, Ramsey SD. Using generalized linear models to assess medical care costs. Health Serv Outcomes Res Methodol 2000;1:185-202
- Buntin MB, Zaslavsky AM. Too much ado about two-part models and transformation? Comparing methods of modeling Medicare expenditures. J Health Econ 2004;23:525-42
- Manning W. Dealing with skewed data on costs and expenditure. In: Jones AM, ed. The Elgar Companion to Health Economics. Cheltenham: Edward Elgar, 2006
- Manning WG, Basu A, Mullahy J. Generalized modeling approaches to risk adjustment of skewed outcomes data. J Health Econ 2005;24:465-88
- Gutiérrez L, Roskell N, Castellsague J, et al. Study of the incremental cost and clinical burden of hip fractures in postmenopausal women in the United Kingdom. J Med Econ 2011;14:99-107
- Brankin E, Mitchell C, Munro R; Lanarkshire Osteoporosis Service. Closing the osteoporosis management gap in primary care: a secondary prevention of fracture programme. Curr Med Res Opin 2005;21:475-82
- Krishnan M, Beck S, Havelock W, et al. Predicting outcome after hip fracture: using a frailty index to integrate comprehensive geriatric assessment results. Age Ageing 2014;43:122-6
- Moppett IK, Wiles MD, Moran CG, et al. The Nottingham Hip Fracture Score as a predictor of early discharge following fractured neck of femur. Age Ageing 2012;41:322-6
