Abstract
Background:
Since hepatitis C virus therapy is typically prioritized for patients with more advanced disease, predicting which patients will progress could help direct scarce resources to those likely to benefit most. This study aims to identify demographics and clinical characteristics associated with high healthcare resource utilization (HRU) and liver disease progression among CHC patients.
Methods:
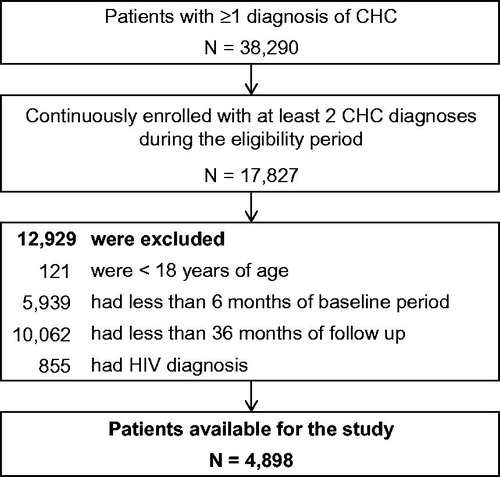
Using health insurance claims (January 2001–March 2013), adult patients with ≥2 CHC claims (ICD-9-CM: 070.44 or 070.54), and ≥6 months of continuous insurance coverage before and ≥36 months after the first CHC diagnosis were included. Patients with human immunodeficiency virus were excluded. Generalized estimating equations were used to identify the demographic and clinical characteristics of being in the 20% of patients with the highest HRU. Factors predicting liver disease progression were also identified.
Results:
In the study population (n = 4898), liver disease severity and both CHC- and non–CHC-related comorbidities and conditions were strong predictors of high healthcare costs, with odds ratios (ORs; 95% confidence interval [CI]) for ≥2 CHC-related and ≥2 non-CHC-related comorbidities/conditions of 2.78 (2.48–3.12) and 2.19 (1.76–2.72), respectively. CHC- and non-CHC-related comorbidities and conditions were also strong predictors of liver disease progression with ORs (95% CI) for ≥2 CHC-related and ≥2 non-CHC-related comorbidities and conditions of 2.18 (1.83–2.60) and 1.50 (1.14–1.97), respectively.
Limitations:
Potential inaccuracies in claims data, information or classification bias, and findings based on a privately insured population.
Conclusion:
This study suggests that CHC patients with high healthcare resource utilization have a high level of comorbidity at baseline and also that non-CHC comorbidities and conditions are strong predictors of high HRU. Non-cirrhotic CHC patients with one or more comorbidities are at high risk of progressing to cirrhosis or end-stage liver disease.
Introduction
The hepatitis C virus (HCV) is the most common chronic blood-borne pathogen in the US, and is associated with a significant economic burdenCitation1–8. Healthcare costs related to HCV in the US were estimated at $6.5 billion in 2013 and are expected to rise to $9.1 billion by 2024Citation5. The National Health and Nutrition Examination Survey (NHANES) recently estimated that 2.7 million US residents are infected with chronic hepatitis C (CHC)Citation9. This estimate was ∼500,000 fewer than the previous NHANES analysis, with high mortality in CHC patients offered as one possible explanation by the authorsCitation10. Morbidity and mortality due to CHC is rising and projected to peak in the next 10–15 years. Progression to cirrhosis and complications of cirrhosis, including liver transplant and death, may continue to riseCitation11–13.
Once patients develop end-stage liver disease (ESLD), they will incur high healthcare costs, since their only option to survive is limited to a liver transplant if they qualify according to the MELD (Model for End-stage Liver Disease) scoring systemCitation14 and if a matching donor can be identified in time. Significantly higher healthcare costs have been found in CHC patients with cirrhosis or ESLD compared to non-cirrhotic patients, ∼1.5-times higher for cirrhotic patients and 3-times higher for ESLD patientsCitation8,Citation15. Describing the characteristics of high healthcare consumption and identifying non-cirrhotic CHC patients who are at high risk of progression to ESLD may help prioritize patients for intervention, including antiviral therapy. This information could be used to target sub-groups of non-cirrhotic patients who are at greatest risk of succumbing to their hepatitis liver disease and incurring significant healthcare costs. Therefore, the current study aims at identifying demographics and clinical characteristics associated with high healthcare resource utilization and costs among CHC patients and, furthermore, at investigating which of these characteristics are associated with progression from non-cirrhosis to cirrhosis and ESLD.
Methods
Data source
Claims dated from January 2001 through March 2013 were analyzed from the OptumHealth Reporting and Insights Database. The database includes medical and pharmacy claims of more than 18 million privately insured individuals covered by 82 self-insured Fortune 500 companies with locations in all census areas in the US. To preserve the anonymity and confidentiality of the patients, the database has been de-identified and is in compliance with the Health Insurance Portability and Accountability Act of 1996. Data elements used in the present analysis included information on patient demographics (e.g., age, gender, insurance type), monthly enrollment history, and medical and pharmacy claims including actual payment amounts.
Study design
Using a retrospective cohort design, patients with at least two CHC diagnoses on two different dates (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM]: 070.44, 070.54), who were 18 years of age or older, and who had never been diagnosed with HIV (ICD-9-CM: 042.xx, 043.xx, 044.xx, 079.53, and V08.xx) were selected to form the study population. The date of their first diagnosis of CHC was identified as the index date. Patients were also required to have at least 6 months of continuous health insurance eligibility before the index date and 36 months after.
The observation period spanned from the first diagnosis of CHC (index date) to 36 months following it. The follow-up of 36 months was separated into 6-month intervals for analyses over time. Information that was recorded up to 6 months before this first diagnosis was used to evaluate the patients’ baseline characteristics.
CHC patients in the top 20% of healthcare resource utilization were classified as high healthcare resource utilizers based on their cumulative total healthcare costs during the 36-month follow-up ($63,588 and up/patient; mean [median] of top 20% CHC patients: $162,526 [$102,375]) and compared with the remaining 80% of CHC patients who were classified as low healthcare utilizers (mean [median] of lower 80% CHC patients: $22,203 [$17,436]). CHC patients were also classified similarly as low vs high healthcare resource utilizers based on inpatient and outpatient/emergency room (ER) costs (i.e., total costs excluding pharmacy costs). The 80th percentile threshold was determined based on the literature. It has been shown that the distribution of healthcare spending is very skewed and that ∼20% of the population is responsible for more than 80% of the total healthcare spendingCitation16,Citation17.
Patients with CHC were also classified as non-cirrhotic, compensated cirrhotic, hepatocellular carcinoma (HCC) ESLD, or non-HCC ESLD at baseline (see Appendix 1). The subset without compensated cirrhosis or ESLD at baseline was used as the reference group in the analysis of the predictors of liver disease severity progression.
Study end-points
Patients’ characteristics were analyzed to identify the strongest predictors of being among the 20% of patients with the highest total healthcare costs. The factors that predicted the 20% of patients with the highest inpatient and outpatient/ER costs (excluding pharmacy costs) were also identified. Moreover, the progression of liver disease severity (i.e., to compensated cirrhosis, HCC ESLD, and non-HCC ESLD) was characterized over time, and the factors that predicted a diagnosis of compensated cirrhosis or ESLD were identified.
Statistical analysis
Descriptive statistics were generated to summarize the patient baseline characteristics of the study population. Means and standard deviations were used for continuous variables, and frequencies and percentages were reported for categorical variables.
Generalized estimating equations (GEE) with logit link for binary outcomes controlling for patient identifiers (IDs) and using characteristics prior to each 6-month interval (i.e., characteristics of the 0–6-month period were used as predictors of the 6–12-month period of follow-up; characteristics of the 6–12-month period were used as predictors of the 12–18-month period of follow-up, etc.) were conducted to obtain odds ratios (ORs) and 95% confidence intervals (CIs). The dependent variable (e.g., 20% of patients with the highest total costs) was also updated for each 6-month interval. Patient characteristics that were used as predictors included: age, gender, type of beneficiary, geographic region, type of insurance, year of index date, specialist visit, liver disease severity (i.e., non-cirrhotic disease, compensated cirrhosis, or HCC ESLD and non-HCC ESLD), comorbidities and conditions (i.e., 0, 1, and ≥2 CHC-related and non-CHC-related) and CHC treatment (interferon-based therapies). A second model, where the dependent variable was the 20% of patients with the highest inpatient and outpatient/ER costs (excluding pharmacy costs), was also estimated.
Comorbidities that may be clinically (or behaviorally) related to CHC infection or HCV therapy have been identified by the authors and the literature reviewedCitation8,Citation18–22. CHC-related comorbidities included: anemia, diabetes, depression, schizophrenia, bipolar disorder, psychiatric disease, substance abuse, renal failure (and dialysis as a proxy), lichen planus, porphyria cutanea tarda, vasculitis, psoriasis, and non-Hodgkin’s lymphoma. Non-CHC-related specific conditions and comorbidities included: pregnancy, epilepsy, rheumatoid arthritis, cardiac arrest, heart failure, coronary arterial disease, lung/heart transplant, kidney transplant, autoimmune deficiency, chronic obstructive pulmonary disease (COPD), and Crohn’s disease.
The evolution of liver disease was also characterized using descriptive statistics. The proportion of patients with a diagnosis of compensated cirrhosis, HCC ESLD, and non-HCC ESLD in each group (i.e., the 20% of patients with the highest total healthcare costs and the remaining 80%) was reported for the baseline period and each of the 6-month intervals of the observation period. A patient was considered non-cirrhotic until he/she received a diagnosis of compensated cirrhosis or ESLD; similarly, a patient was considered compensated cirrhotic until he/she received a diagnosis of ESLD. The predictors of liver disease progression (i.e., to compensated cirrhosis or ESLD) were also evaluated with GEE as described for the evaluation of characteristics associated with high healthcare utilizers.
Since the OptumHealth Reporting and Insights Database includes only commercial insurance claims, cost information covered by Medicare was not available. Therefore, a sensitivity analysis for the predictors of high healthcare costs was conducted on the subset of patients aged <65 years.
Results
Patient characteristics
A total of 4898 patients with CHC were selected and formed the study population (). Baseline characteristics of the study population are presented in . The mean age of the overall study population was 52 years, and 39% of patients were female. Overall, the most common CHC-related comorbidities were diabetes (12.1%), psychiatric disease (8.7%), depression (7.5%), and anemia (6.6%), while the most frequent non-CHC-related comorbidities were coronary artery disease (5.3%) and COPD (4.5%). Patients with the highest healthcare costs during follow-up (top 20% percentile) had a qualitatively higher proportion of comorbidities and conditions at baseline compared to the remaining patients with the lowest healthcare costs (CHC-related: 47.2% vs 29.3%; non-CHC-related: 21.5% vs 11.6%).
Table 1. Demographic and clinical characteristics.
Liver disease progression
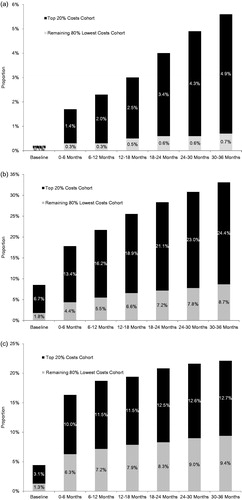
present the evolution over time of the proportion of patients that received a diagnosis of HCC ESLD and non-HCC ESLD during the baseline period and each follow-up interval. During the study period in CHC patients with the highest costs, the proportion of patients with HCC ESLD and non-HCC ESLD increased from 0.1% to 4.9% and from 6.7% to 24.4%, respectively. The corresponding proportion of patients with HCC ESLD and non-HCC ESLD increased from 0.1% to 0.7% and from 1.8% to 8.7% in CHC patients with the lowest costs. The proportion of patients with compensated cirrhosis increased from 3.1% to 12.7% in CHC patients with the highest costs and from 1.3% to 9.4% in CHC patients with the lowest costs ().
Predictors of high healthcare costs
Liver disease severity and both CHC- and non-CHC-related comorbidities and conditions were strong predictors of high healthcare costs (). The ORs (95% CI) of being in the top 20% of high healthcare utilizers for CHC patients diagnosed with compensated cirrhosis, HCC, and non-HCC ESLD were 1.39 (1.21–1.60), 8.16 (4.75–14.00), and 3.07 (2.60–3.63), respectively. The corresponding ORs (95% CI) of CHC patients diagnosed with 1 or ≥2 CHC-related comorbidities were 1.61 (1.48–1.74) and 2.78 (2.48–3.12), respectively, while those of patients diagnosed with 1 or ≥2 non-CHC-related comorbidities/conditions were 1.78 (1.60–1.98) and 2.19 (1.76–2.72), respectively. Similar results were found in the analysis using only inpatient and ER/outpatient healthcare costs.
Table 2. Predictors of high healthcare costs in patients with CHC.
Patients aged 45–64 years had a higher likelihood of being in the top 20% of high healthcare utilizers compared to patients younger than 45 years (OR [95% CIs]: 1.15 [1.02–1.29]). Patients 65 years and over were found to have a lower likelihood of being in the top 20% of higher healthcare costs patients; this can be explained by the use of a commercial insurance claim database for this study. Results of the sensitivity analysis on patients aged ≤65 years (n = 4397) showed similar trends for the other predictors of high healthcare costs as those reported in the main analysis (Appendix 2).
The use of interferon-based therapy was the highest significant predictor of higher total healthcare costs (OR [95% CI] = 4.21 [3.85–4.62]); however, this was also associated with a significantly lower likelihood of being in the higher cost cohort when only inpatient and ER/outpatient healthcare costs were considered (OR [95% CI] = 0.86 [0.76–0.96]).
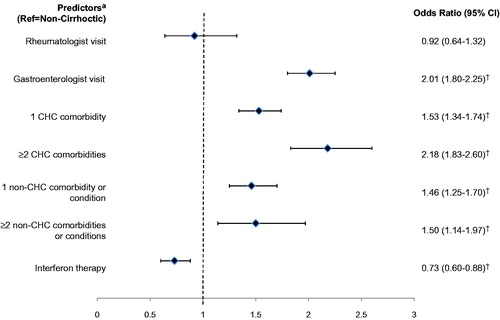
Predictors of liver disease progression
Gastroenterologist visit and both CHC-related and non-CHC-related comorbidities and conditions were all strong predictors of progression to compensated cirrhosis or ESLD (). The OR (95% CI) of progression for CHC patients seen by a gastroenterologist was 2.01 (1.80–2.25), while those of CHC patients diagnosed with 1 or ≥2 CHC-related comorbidities were 1.53 (1.34–1.74) and 2.18 (1.83–2.60), respectively, and those of patients diagnosed with 1 or ≥2 non-CHC-related comorbidities or conditions were 1.46 (1.25–1.70) and 1.50 (1.14–1.97), respectively. Moreover, CHC patients treated with interferon-based therapies were significantly less likely to be diagnosed with cirrhosis or ESLD (OR [95% CI] = 0.73 [0.60–0.88]).
Figure 3. Predictors of patients with CHC being diagnosed with compensated cirrhosis or ESLD (n = 4676). CHC, chronic hepatitis C; ESLD, end-stage liver disease; CI, confidence interval. †Denotes statistical significance. *Additional predictors not reported include the following: age group (i.e., ≤45, 45–65, >65 years), female, type of beneficiary, type of insurance (i.e., health maintenance organization, point of service, preferred provider organization, indemnity), region (i.e., Northeast, Midwest, South, and West), and the index year (i.e., 2001–2013).
Discussion
Using real-world data, this large retrospective study was conducted to find the patient characteristics most predictive of being among the 20% of CHC patients that incurred the highest healthcare resource utilization and costs. During the period from January 2001 to March 2013, a total of 4898 CHC patients were studied and, not only liver disease severity, but also the presence of CHC-related and non-CHC-related comorbidities and conditions were significantly associated with a higher likelihood of being among the highest healthcare utilizers. At baseline, around one-third of patients with CHC had at least one CHC-related comorbidity and around 15% had at least one non-CHC-related condition, which suggests that an important proportion of the population is at risk of being high healthcare utilizers.
Recent studies have shown that the economic burden of HCV increases with liver disease severityCitation8,Citation15. Gordon et al.Citation15 demonstrated that patients with compensated cirrhosis and ESLD had 32% and 247% higher healthcare costs than non-cirrhotic patients. In the current study, we also found that patients with compensated cirrhosis (OR = 1.39) and ESLD (ORs >3) were associated with significantly higher healthcare resource utilization and costs compared to non-cirrhotic patients. Recent studies also suggested that comorbidities not related to CHC such as coronary artery disease, COPD, and rheumatoid arthritis have an important influence on total healthcare costs of patients infected with CHCCitation8,Citation15. A retrospective matched cohort study comparing HCV patients to patients without HCV reported that non-HCV-related conditions accounted for 54% of the total healthcare cost difference found between the two cohortsCitation8. Our study concurs with the literature and suggests that appropriate care for HCV patients with non-CHC-related comorbidities/conditions could decrease overall cost of care for these patients.
A recent study identified new-onset diabetes among patients with CHC infection as a predictor for the subsequent development of cirrhosis and hepatic decompensationCitation23. Our analysis supports that finding since diabetes was the most common CHC-related comorbidity in the population analyzed in this study. Further, a patient with any other CHC-related condition who develops new-onset diabetes would then have two CHC-related comorbidities and, according to our analysis, would have ∼2-fold increased risk for the development of cirrhosis and/or ESLD. Taken together, the two studies suggest that CHC patients with diabetes (either newly diagnosed or with an existing diagnosis) could be targeted for antiviral therapy prior to the development of cirrhosis or decompensation and the corresponding life-long increased risk for HCC and death. Prioritizing HCV therapy for patients without cirrhosis based on the presence of comorbidities, including diabetes, is consistent with the current AASLD/IDSA/IAS-USA recommendations for testing, managing, and treating hepatitis CCitation24. Studies have documented that sustained virologic response is linked to lower risk of compensated cirrhosis and ESLDCitation25,Citation26. In the current study we found that patients treated with interferon-based therapies had significantly higher odds (OR = 4.21) of being among the 20% highest utilizers; however, they were significantly less likely to be among the 20% of patients with the highest inpatient and outpatient/ER costs (OR = 0.86). Most importantly, patients treated with interferon-based therapies had significantly lower odds of progressing to an advanced stage of liver severity. Previous analyses of the impact of drug therapy on healthcare costs in patients with hepatitis C have been conductedCitation8,Citation27,Citation28. McCombs et al.Citation28 reported that CHC patients’ persistence to 48 weeks or more of therapy led to a reduction of hospital admission and to a cost reduction relative to treated patients who were persistent for less than 24 weeks. A recent retrospective study concluded that completion of 36 weeks of interferon-based therapy was significantly associated with lower levels of healthcare resource utilization post-therapy among CHC patientsCitation29. The current study concurs with the literature that interferon-based HCV therapy is an important factor to control both healthcare costs and liver disease progression of patients infected with CHC. This analysis should be repeated once sufficient follow-up data is available for patients treated with all oral regimens to confirm whether similar results are found.
This study is subject to certain limitations. As is the case with claims databases, the OptumHealth Reporting and Insights database may have contained inaccuracies or omissions in procedures, diagnoses, or costs. Moreover, the observational design was susceptible to various biases such as information or classification bias (e.g., identification of false-positive CHC events). Also, since our study population consisted of privately insured individuals, our results might not be generalizable to the entire CHC population, of which an important proportion is uninsured or publicly insuredCitation30. Of note, the evaluation of predictors of liver disease progression and highest healthcare resource utilization and costs in the current study was for the most part prior to the availability of triple therapy (peginterferon, ribavirin, and the direct antiviral agents boceprevir, telaprevir, sofosbuvir, or simeprevir) usage since boceprevir and telaprevir were approved by the FDA in 2011, and sofosbuvir and simeprevir were approved in 2013. More recently, the single-pill combination of sofosbuvir plus ledipasvir was also approved by the FDA (October 2014). Finally, including only patients with at least 36 months of follow-up induced a survival bias in the study. Despite having limitations, well designed observational studies provide valuable information on real-life scenarios.
Conclusion
This real-world study suggests that CHC patients with the highest healthcare resource utilization and costs had a high level of comorbidity, and that non-CHC comorbidities and conditions are strong predictors of high healthcare costs. Since the majority of patients were non-cirrhotic, liver disease severity alone did not fully predict high resource utilization, although, when present, it was a predictor of high resource utilization. CHC and non-CHC-related comorbidities were both strong predictors of liver disease progression among CHC patients without cirrhosis at baseline.
Transparency
Declaration of funding
The research was funded by Janssen Scientific Affairs, LLC, in Titusville, NJ.
Declaration of financial/other relationship
FL, GG, DP, and PL are employees of Analysis Group, Inc., a consulting company that has received research grants from Janssen Scientific Affairs. JL, NT, and AP are employees of Janssen Scientific Affairs. JME peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Acknowledgment
Technical editorial assistance was provided by Shannon O’Sullivan, ELS, of MedErgy, and was funded by Janssen Scientific Affairs, LLC.
References
- Davis KL, Mitra D, Medjedovic J, et al. Direct economic burden of chronic hepatitis C virus in a United States managed care population. J Clin Gastroenterol 2011;45:e17-24
- McAdam-Marx C, McGarry LJ, Hane C a, et al. All-cause and incremental per patient per year cost associated with chronic hepatitis C virus and associated liver complications in the United States: a managed care perspective. JMCP 2011;17:531-46
- McCombs JS, Yuan Y, Shin J, et al. Economic burden associated with patients diagnosed with hepatitis C. Clin Therapeut 2011;33:1268-80
- Poret AW, Ozminkowski RJ, Goetzel R, et al. Cost burden of illness for Hepatitis C patients with employer-sponsored health insurance. Dis Manag 2002;5:95-107
- Razavi H, Elkhoury AC, Elbasha E, et al. Chronic hepatitis C virus (HCV) disease burden and cost in the United States. Hepatology (Baltimore, MD) 2013;57:2164-70
- Rosenberg DM, Cook SF, Lanza LL. Health care, treatment patterns and cost of services for patients infected with chronic hepatitis C virus in a large insured New England population. J Viral Hepatitis 2000;7:361-7
- Su J, Brook R a, Kleinman NL, et al. The impact of hepatitis C virus infection on work absence, productivity, and healthcare benefit costs. Hepatology (Baltimore, MD) 2010;52:436-42
- Tandon N, Reddy KR, Lefebvre P, et al. Direct and indirect cost burden of chronic Hepatitis C infection in privately-insured patients, stratified by liver disease severity. Am J Pharm Benefits 2015;7:e90-e100
- Denniston MM, Jiles RB, Drobeniuc J, et al. Chronic hepatitis C virus infection in the United States, National Health and Nutrition Examination Survey 2003 to 2010. Ann Intern Med 2014;160:293-300
- Armstrong GL. The prevalence of Hepatitis C virus infection in the United States, 1999 through 2002. Ann Intern Med 2006;144:705
- Davis GL, Alter MJ, El-Serag H, et al. Aging of hepatitis C virus (HCV)-infected persons in the United States: a multiple cohort model of HCV prevalence and disease progression. Gastroenterology 2010;138:513-21, 521.e1-6
- Ly KN, Xing J, Monina Klevens R, et al. The increasing burden of mortality from viral hepatitis in the United States between 1999 and 2007. Ann Intern Med 2012;156:271-278
- Rein DB, Wittenborn JS, Weinbaum CM, et al. Forecasting the morbidity and mortality associated with prevalent cases of pre-cirrhotic chronic hepatitis C in the United States. Digest Liver Dis 2011;43:66-72
- Kamath PS, Wiesner RH, Malinchoc M, et al. A model to predict survival in patients with end-stage liver disease. Hepatology (Baltimore, MD) 2001;33:464-70
- Gordon SC, Pockros PJ, Terrault N, et al. Impact of disease severity on healthcare costs in patients with chronic hepatitis C (CHC) virus infection. Hepatology (Baltimore, MD) 2012;56:1651-60
- Smith DH, Malone DC, Lawson K a, et al. A national estimate of the economic costs of asthma. Am J Respir Crit Care Med 1997;156:787-93
- Nihcm Foundation. The Concentration of Health Care Spending. 2012 Washington, DC
- Basseri B, Yamini D, Chee G, et al. Comorbidities associated with the increasing burden of hepatitis C infection. Liver Int Off J Int Assoc Study Liver 2010;30:1012-18
- El-Zayadi A-R. Hepatitis C comorbidities affecting the course and response to therapy. World J Gastroenterol 2009;15:4993
- Jacobson IM, Cacoub P, Dal Maso L, et al. Manifestations of chronic hepatitis C virus infection beyond the liver. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc 2010;8:1017-29
- Khattab MA, Eslam M, Alavian SM. Hepatitis C virus as a multifaceted disease: a simple and updated approach for extrahepatic manifestations of hepatitis C virus infection. Hepatitis Monthly 2010;10:258-69
- Ko HM, Hernandez-Prera JC, Zhu H, et al. Morphologic features of extrahepatic manifestations of hepatitis C virus infection. Clin Dev Immunol 2012;2012:740138
- Huang Y-W, Yang S-S, Fu S-C, et al. Increased risk of cirrhosis and its decompensation in chronic hepatitis C patients with new-onset diabetes: a nationwide cohort study. Hepatology 2014;60:807-14
- AASLD/IDSA HCV Guidance Panel. Hepatitis C Guidance: AASLD-IDSA recommendations for testing, managing, and treating adults infected with Hepatitis C Virus. Hepatology 2015;62:932-54
- Moon C, Jung KS, Kim DY, et al. lower incidence of hepatocellular carcinoma and cirrhosis in Hepatitis C patients with sustained virological response by pegylated interferon and ribavirin. Digest Dis Sci 2014;60:573–81
- Fransen van de Putte DE, Makris M, Fischer K, et al. Long-term follow-up of hepatitis C infection in a large cohort of patients with inherited bleeding disorders. J Hepatol 2014;60:39-45
- Manos MM, Darbinian J, Rubin J, et al. The effect of hepatitis C treatment response on medical costs: a longitudinal analysis in an integrated care setting. JMCP 2013;19:438-47
- McCombs J, Matsuda T, Tonnu-Mihara I, et al. The risk of long-term morbidity and mortality in patients with chronic hepatitis C: results from an analysis of data from a Department of Veterans Affairs Clinical Registry. JAMA Intern Med 2014;174:204-12
- Tandon N, Balart L a, Laliberté F, et al. Impact of completing chronic hepatitis C (CHC) treatment on post-therapy healthcare cost. J Med Econ 2014;17:1-10
- Ong JP, Collantes R, Pitts A, et al. High rates of uninsured among HCV-positive individuals. J Clin Gastroenterol 2005;39:826-30