Abstract
Introduction Mitral regurgitation is a heart condition resulting from blood flowing from the left ventricle towards the left atrium, increasing the risk of heart failure and mortality. While surgery can greatly reduce these risks, some patients are not eligible, resulting in medication being their only therapeutic alternative. The MitraClip (Abbot Vascular) is a medical device that is percutaneously implanted and designed to eliminate leaking of the mitral valve.
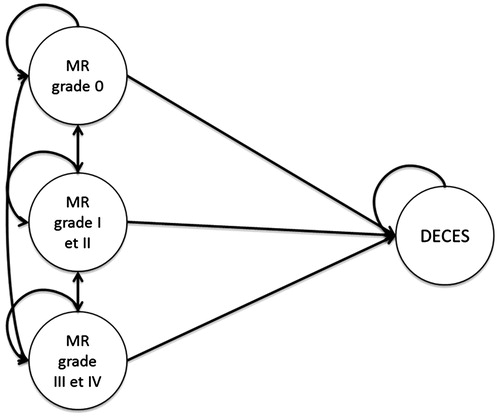
Methods The efficacy of the MitraClip strategy vs medical management was assessed using a 4-state Markov model based on the mitral regurgitation grade (mitral regurgitation grade 0, I/II, and III/IV, and death). At each 1-month cycle, patients were or were not hospitalized. The model analyzed a fictional population of 1000 patients over a 5-year period from a national Health Insurance perspective. The primary end-point was the number of deaths avoided. Data from the EVEREST II High Risk Study patients were used along with a literature review.
Results At 5 years, among the 1000 patients, 276 deaths were found to be avoidable with the MitraClip strategy. The incremental cost-effectiveness ratio (ICER) was €93,363 per death avoided. The annual ICER was calculated to take into consideration excess costs resulting from the MitraClip over the first year (€29,984 vs €8557 for the reference strategy) and the reduction of costs in following years (€3122 for MitraClip vs €8557 for reference strategy). Thus, the mean ICER was calculated to be €20,720 per death avoided.
Conclusion The MitraClip is a novel alternative therapy for mitral insufficiency in patients ineligible for surgery that may offer a medico-economic advantage.
Introduction
Mitral insufficiency is the second most common form of vascular heart diseaseCitation1. Prevalence is estimated to be 1.7% of the global population, increasing to 9.3% in people over the age of 75 yearsCitation2. Mitral insufficiency is caused by leaking of the mitral valve during ventricular systole, resulting in blood flow from the left ventricle to the left atrium. The more severe the insufficiency, the greater the quantity of leaking blood. Gold standard therapeutic management of severe mitral insufficiency is surgery to replace or repair the mitral valve; however, patients considered to be at high risk due to their age or the presence of comorbidities are not eligible for surgery, accounting for 50% of all patientsCitation3.
For these patients, the only therapeutic alternative is medication, based on diuretics, β-blockers, and in some cases anticoagulants and ACE inhibitors in the event of heart failureCitation4; however, this treatment approach is not curative and the condition evolves with a continued worsening of mitral insufficiency. Mitral regurgitation (MR) is graded according to five levels. Grade 0 represents the absence of MR. Grade 1 corresponds to the presence of mild regurgitation, grade 2 to moderate regurgitation. Grades 3 and 4 indicate the existence of moderate-to-severe and severe regurgitation. Mitral insufficiency is a life-threatening pathology: 1-year mortality rates in patients with severe disease have been estimated to be between 7.3–54% while, at 5 years, mortality in asymptomatic patients ranges from 22–42%Citation5. This latter study also highlighted a higher rate of mortality in patients with grade 3 or 4 MR compared to those with grade 1 or 2.
The MitraClip is a novel treatment option for mitral insufficiency allowing the mitral valve to be repaired percutaneously using the Alfieri stitch. The MitraClip was evaluated in a randomized, controlled, prospective, multi-center study, EVEREST II (Endovascular Valve Edge-to-Edge Repair)Citation6. The High Risk Study (HRS) arm evaluated the efficacy and safety of the MitraClip in patients at high surgical mortality risk with MR grade 3 or higher. Survival at 1 year in high risk patients with a MitraClip implant was 75.4%, compared to 55.3% for patients receiving medicationCitation7. Likewise, at 2 years, survival in MitraClip patients was higher than in the reference armCitation8.
To date, no studies evaluating costs specific to mitral insufficiency have been published, with the only studies available being those evaluating the general economic cost of heart failure. Heart failure was estimated to account for 2% of healthcare costs in the US in 2010Citation9, while in France, according to a publication by the National Health Insurance Fund for Employees (CNAMTS), the annual cost is 1.6 billion euros, equivalent to a mean annual cost of €10,842 per patientCitation10. The MitraClip has raised medico-economic interest in both the UK and Canada in terms of efficacy outcomes and economic costs for MRCitation11–13. In France a model was developed and submitted to the Economic Evaluation and Public Health Committee of the National Health Authorities for product reimbursement by the National Health Insurance.
This medico-economic evaluation of the MitraClip as an innovative therapeutic approach for high-risk patients ineligible for surgery was designed to analyze the efficacy of this device compared to standard medical treatment, considered to be the current reference strategy.
Methods
A multi-state Markov model was developed using four states corresponding to the severity of mitral insufficiency after treatment and a death state, in a fictional population of 1000 patients (). The analysis was performed from a payer perspective, integrating direct medical costs covered 100% due to the classification of mitral insufficiency as a chronic illness, over a 5-year period, with 1-month analysis cycles. Efficacy data were from the EVEREST II HRS and REALISM studies, and cost data extracted from a French hospital database (PMSI, the Program for Medicalization of Information Systems)Citation14. Results are expressed as life-years gained in the absence of useful data for calculating QALYs (Quality Adjusted Life Years). The number of life years gained is a relevant criterion in the context of this disease and the results of the EVEREST II studies. The Incremental Cost Effectiveness Ratio (ICER) was calculated per life-year gained.
The model was developed using Microsoft Excel 2007 MSO 32 bits and Microsoft Visual Basic for Applications, defined by the ‘.xlsm’ extension. The methodological recommendations of the French Health AuthoritiesCitation15 were implemented with the costs and results updated at a rate of 4% annually, and the costs of transporting patients were integrated into the analysis. The choice of the model structure was based on the MR grade, which characterizes a state of health.
At each cycle, a given patient in a particular state of health was or was not hospitalized for cardiovascular causes. The patient may or may not die, irrespective of hospitalization, and surviving patients are maintained as having an MR state. The death rate of the patients in each MR grade is the combination of the two probabilities ():
The death probability from hospitalization, which is the monthly rate issued from Logeart et al.Citation16.
The death probabilities linked to the MR grade, which is the monthly rate issued from Cioffi et al.Citation5.
Table 1. Number of life years gained over 5 years in a model based on 1000 patients.
The state transition probabilities are issued from the Everest II HRR trial. During the 1st cycle, which is the post-operative cycle, there is no MR grade transition. The probability of staying in a state directly depends on the death probability; however, from the 2nd cycle, the state–transition probability is time-dependent, which allows a more consistent modelling of the disease ().
Table 2. Summary of costs used in the model.
A separate arm for patients having failed MitraClip placement was not included, given that a published study reported a 99% placement success rate, with the 1% corresponding to incorrect randomizationCitation17. In the absence of randomized controlled data, our model assumed two conservative hypotheses: a patient receiving medical management for mitral insufficiency does not experience MR grade improvement as the patient’s status is considered to be sufficiently serious that no improvement will occur with this treatment. The second hypothesis relates to reproducibility of 1-year mortality in terms of MR grade in the absence of other dataCitation5.
Finally, a non-conservative hypothesis was made, that all non-cardiovascular events had a similar rate in the two populations and, thus, were not considered in the model.
Results
The results for life-years gained obtained with this model using the results of the EVEREST II HRS study are presented in .
Table 3. Results of the medico-economic evaluation.
For each of the two strategies, the following costs were taken into consideration for each patient:
initial hospitalization cost for clip placement (MitraClip approach only);
cost of the MitraClip system (MitraClip approach only);
mean annual cost of re-hospitalization;
care and rehabilitation costs;
transport costs; and
mean annual cost of outpatient follow-up.
Data for hospital costs for the MitraClip strategy were obtained retrospectively via the local Department of Medical Information (DIM) from the list of 17 patients who underwent the MitraClip placement at the Louis Pradel Hospital in Lyon (Study MITRA-FR, referenced on clinicaltrials.gov)Citation13.
To estimate the mean cost of the procedure for the National Health Insurance, hospital stays were considered to correspond to the Diagnosis-Related Groups (DRG) costs applicable in 2011 (note that DRG costs specific to the MitraClip procedure are not reported and that patients were categorized in existing DRGs), with adjustment for the length of the stay, and additional expenses linked to intensive care as observed in the Lyon cohort. Transport costs were obtained from an information report done by the National Assembly. In the absence of long-term follow-up for the MitraClip strategy or for mitral insufficiency patients treated with medication, these costs are based on hypotheses extrapolated in part from the 1–3 year results of the EVEREST II HRS study and also from data obtained from the literature () for unitary costs used in the model.
The cost of the MitraClip strategy is impacted by the initial hospital stay for the surgery for placement of the device. The annual cost of each strategy was calculated for the first year and then for the following years. The first year, the cost of the MitraClip strategy was €29,984 ves €8557 for medical management, this difference in cost is largely due to the placement of the MitraClip system. In subsequent years the annual MitraClip strategy costs were €3122, while those associated with medical management remained at €8557, given that no aspects of follow-up with this approach are altered: the cost of treatments remains similar and the number of re-hospitalizations is presumed to be stable in the model.
It is apparent that the costs over subsequent years are less for the MitraClip approach. For these patients, the MR grade and survival improve, and there are fewer re-hospitalizations than for patients under the reference strategy. Figures are derived from the EVEREST II HRS where the reduction in the number of re-hospitalizations is 77% in favor of the MitraClip strategy.
The ICER is €15,741.10 per life year gained after 5 years, which means that, for each life year gained, the payer will have to pay €15,741.10.
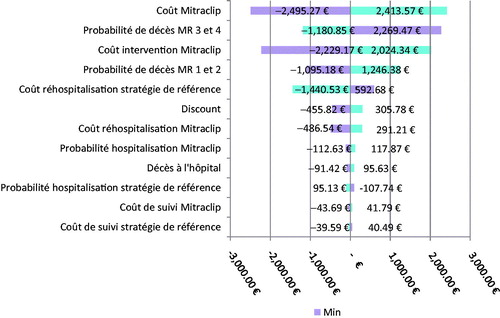
For the secondary efficacy end-point, the result is €79,792.73 per death avoided. Sensitivity analyses have been performed in order to show the robustness of the model. If no confidence interval were derived from the literature, a deviation of 20% from the mean value was chosen.
indicates that ICER is sensitive to the initial costs of the device placement. The number of patients with grades I and II is a determining parameter as the difference in efficacy lies in the fact that the MR grade of patients undergoing the MitraClip strategy decreases (grade III and IV vs grades I and II) and this improvement is maintained with timeCitation8. Univariate sensitivity analyses on the primary end-points complete the deterministic sensitivity analyses. This relative stability can also be observed through the Monte Carlo simulation that has been performed.
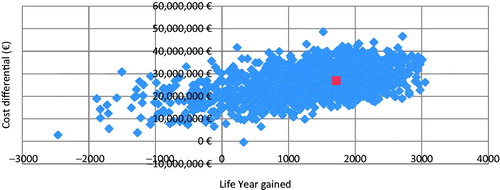
For asymmetrical data, such as costs, the authors advise the use of the gamma function. A beta function was used for the death probabilities.
A Dirichlet distribution was chosen for every transition probability, which is a multivariate generalization of the Beta distribution. It is used to represent the transition probabilities toward several states of the model, according to BriggsCitation18.
The simulation was performed on 2000 iterations, which is sufficient to observe a tendency on the cost-effectiveness plane. The scatter-plot analysis () indicates that the uncertainty of the result, in Euro per life-year gained, is mainly located in the north-east quarter of the plane. This shows the consistency of the results. Only a minority of dots are located in the North-West quarter.
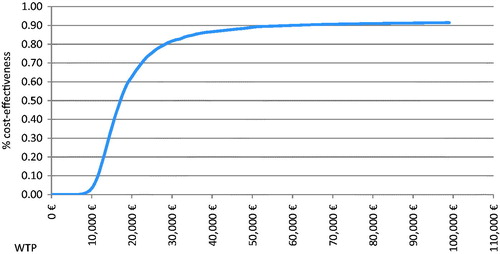
The acceptability curve () gives a chance to conclude on the efficiency of the MitraClip strategy depending on the willingness to pay of the payer.
However, in the absence of an established threshold, shows that the MitraClip strategy has a 90% chance of being cost-effective at a threshold of €60,000 per life-year gained.
In regards of the threshold commonly applied in Europe, the probability of the MitraClip strategy of being efficient is greater than 80% at a threshold of €30,000 per life-year gained.
Discussion
It appears that the model has several strengths and, thus, can be a reliable decision-making tool. First, it is one of the first health-economics analyses of MR on high-risk patients. The model is directly based on data obtained during a clinical trial, the Everest II HRS study. The latter includes more than 350 patients coupling to previous studies: Everest II High Risk Registry and REALISM High Risk. The large number of patients and their diversity gives the model the opportunity to be updated on a regular basis.
Moreover, this model is the first one operated in the French context. The France health economics field has become more and more important in the last few years, in a choice to rationalize decision-making in healthcare. This model has been developed in accordance with French authorities and is part of the regulatory market-access process. Being the first model published on mitral regurgitation, this study highlights the health-economic aspect of the MitraClip system.
Third, the considered costs of the initial hospitalization and of re-hospitalization linked with mitral regurgitation come from a study by Trochu et al.Citation14. The 12-month retrospective population-based analysis of resource utilizations extracted from the 2009 French Medical Information System show the heterogeneity of the costs of care associated with MR. Finally, the model structure has been validated by clinicians and has been described as consistent with the disease’s progression by the French health authorities.
As seen, the medico-economic evaluation is mainly based on the data from the Everest II studies. The limits of the model are, therefore, linked to this dependence, but also to the poor literature surrounding mitral insufficiency. First, the model considers that patients suffering from mitral insufficiency could be defined only by their MR grade level. This point is supported in many publications that use the MR grade or the NYHA score as health state indicators. Considering that mitral insufficiency is one of the many causes of heart failure, the MR grade criteria are relevant to measure the evolution of the disease.
Second, as mitral insufficiency can be degenerative or functional, a sub-group analysis could have shown more thin results; however, the Everest II studies did not consider the variety of etiology and the results are, thus, obtained for a pooled population. As the main form of mitral insufficiency in Everest II is degenerative (73%), the results can be biased. A functional form is considered as a bad prognosis, by the sur-representation of the degenerative form is a non-conservative hypothesisCitation19; however, this repartition is in accordance with a real life oneCitation1.
Finally, mitral insufficiency causes an important decrement in quality-of-life. Consequently, a cost-utility analysis could have introduced this notion in the efficacy criteria. The Everest II studies planned a collection of quality-of-life data, based on the SF-36 questionnaire, but the choice was made to not use those data as it was irrelevant to use non-French quality-of-life data; rescoring in utility (via the SF-6D form) is not validated by the methodological guidelines of the HAS.
A few studies have been performed on the cost-effectiveness profile of the MitraClip device. One such study from Mealing et al.Citation11 relates to high-risk surgery and inoperable patients. The modelling was performed using data from the Everest II HRS study. The utility data are issued from the Health Technology Assessment on cardiac Resynchronization Therapy and costs from national databases. The results showed that the MitraClip device is cost-effective with an ICER standing at £14,800 per QALY with a time horizon of 10 years.
Cameron et al.Citation12 conducted a study about high-risk patients in the Canadian payer’s perspective. The utility data were issued from the Göhler et al.Citation20 study, which were based on chronic heart failure patients using the German preferences. The results show an ICER of $23,433 per QALY and $22,109 per life-year gained.
Considering the heterogeneity between French, Canadian, and UK healthcare systems, and the differences in the evaluation methodology, it is difficult to compare the results of each study; however, it is noticeable that the authors choose three different model structures. Mealing et al.Citation11 modeled the disease pathway with the significant events (hospital care, rehabilitation, MV surgery, etc.) and Cameron focused on the health states of each patient using the NYHA classification. The study presented in the present paper also focused on health states, but the MR grades were used as indicators.
Another difference comes from the time horizon chosen. Mealing et al.Citation11 chose a 5-year perspective, whereas Cameron et al.Citation12 evaluated the device with a lifetime horizon. The two studies show that the choice of the time horizon has a significant impact on the final results.
Beyond the population chosen, which are very similar from one study to another, the cost-effectiveness evaluations have a major common point. All modeling processes were performed using Everest II HSR study data, which are the most complete clinical data available.
Conclusion
From a clinical perspective, the MitraClip strategy presents an advantage in terms of improved survival, but also in qualitative terms for the patient and economically for the Payer, given that the improved MR grade for patients with the MitraClip strategy is maintained over time, avoiding re-hospitalizationsCitation8,Citation21.
From an economic perspective, this improvement is accompanied by costs linked to the initial surgery and the placement of an implantable device. In terms of efficacy, measured in life-years gained, all analyses position the ICER at ∼ €16 000 per life-year gained, taking into consideration total cumulative costs. The uncertainty level surrounding these results is low considering the probabilistic analysis. The probability of being cost-effective for a threshold of €30,000 per life year gained is 80%.
In the absence of a decision threshold and considering the MitraClip strategy as the only therapeutic alternative to the reference strategy of medical management, the MitraClip strategy constitutes an attractive therapeutic alternative, for both the patient and the payer.
Transparency
Declaration of funding
This manuscript was funded by Abbott Vascular.
Declaration of financial/other relationships
PG is a consultant for Abbott. SB and NJ have received sponsorship from Abbott Vascular and are consultants/advisors for Stratégique Santé. NJ also owns stock and/or shares in Sanofi. SM is the manager of Capionis, who have been funded by Abbott to perform this analysis. JME peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
References
- Iung B, Baron G, Butchart EG, Delahaye F, Gohlke-Bärwolf C, Levang OW, et al. A prospective survey of patients with valvular heart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. Eur Heart J. 2003;24:1231–43
- Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart diseases: a population-based study. The Lancet. 2006;368:1005–11
- Mirabel M, Iung B, Baron G, Messika-Zeitoun D, Détaint D, Vanoverschelde J-L, et al. What are the characteristics of patients with severe, symptomatic, mitral regurgitation who are denied surgery? Eur Heart J. 2007;28:1358–65
- Vahanian A, Alfieri O, Andreotti F, Antunes MJ, Barón-Esquivias G, Baumgartner H, et al. Guidelines on the management of valvular heart disease (version 2012) The Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2012;33:2451–96
- Cioffi G, Tarantini L, De Feo S, Pulignano G, Del Sindaco D, Stefenelli C, et al. Functional mitral regurgitation predicts 1-year mortality in elderly patients with systolic chronic heart failure. Eur J Heart Fail. 2005;7:1112–17
- Feldman T, Foster E, Glower DD, Kar S, Rinaldi MJ, Fail PS, et al. Percutaneous repair or surgery for mitral regurgitation. N Engl J Med. 2011;364:1395–406
- Whitlow PL, Feldman T, Pedersen WR, Lim DS, Kipperman R, Smalling R, et al. Acute and 12-month results with catheter-based mitral valve leaflet repair: the EVEREST II (Endovascular Valve Edge-to-Edge Repair) High Risk Study. J Am Coll Cardiol. 2012;59:130–9
- Kar S, E. a. Analysis of the Everest II- High Risk Two Year Outcomes. New Orleans, LA: American College of Cardiology Annual Conference, 2011
- Braunschweig F, Cowie MR, Auricchio A. What are the costs of heart failure? Eur Eur Pacing Arrhythm Card Electrophysiol J Work Groups Card Pacing Arrhythm Card Cell Electrophysiol Eur Soc Cardiol. 2011;13 Suppl 2:ii13–7
- Merlière J, Couvreux C, Smadja L, Jolivet A. Caractéristiques et trajet de soins des insuffisants cardiaques du Régime général. Caisse Nationale d’Assurance Maladie des Travailleurs Salariés; 2012 août. (Point de répère). Report No.: 38.
- Mealing S, Feldman T, Eaton J, Singh M, Scott DA. EVEREST II high risk study based UK cost-effectiveness analysis of MitraClip® in patients with severe mitral regurgitation ineligible for conventional repair/replacement surgery. J Med Econ. 2013;16:1317–26
- Cameron HL, Bernard LM, Garmo VS, Hernandez JB, Asgar AW. A Canadian cost-effectiveness analysis of transcatheter mitral valve repair with the MitraClip system in high surgical risk patients with significant mitral regurgitation. J Med Econ. 2014;17:599–615
- Charroin C, Lamure M, Aulagner G, Constant H, Obadia J, Armoiry X. Cost-effectiveness of percutaneous edge-to-edge mitral valve repair in patients with high surgical risk. 2014; ESC Congress.
- Trochu J-N, Le Tourneau T, Obadia J-F, Caranhac G, Beresniak A. Economic burden of functional and organic mitral valve regurgitation. Arch Cardiovasc Dis. 2015;108:88–96
- HAS. Guide méthodologique pour l'évaluation méidco-économique à la Haute Autorité de Santé. Paris: Haute Autorité de Santé, 2011
- Logeart D, Isnard R, Resche-Rigon M, et al. Current aspects of the spectrum of acute heart failure syndromes in a real-life setting: the OFICA study. Eur J Heart Fail 2013;15:465–76
- Taramasso M, Maisano F, Latib A, Denti P, Buzzatti N, Cioni M, et al. Clinical outcomes of MitraClip for the treatment of functional mitral regurgitation. EuroIntervention J Eur Collab Work Group Interv Cardiol Eur Soc Cardiol. 2014;
- Briggs A, Sculpher M, Claxton K. Decision Modelling for Health Economic Evaluation. 1 edition. Oxford: OUP Oxford; 2006. 256 p.
- Martins R-P, Baruteau A-E, Donal E, et al. Insuffisance mitrale ischemique: apport de l'echocardiographie d'effort et nouvelles perspectives therapeutiques. Ann Cardiol Angeiolog 2007;56:289–96
- Göhler A, Conrads-Frank A, Worrell SS, et al. Decision-analytic evaluation of the clinical effectiveness and cost-effectiveness of management programmes in chronic heart failure. Eur J Heart Fail 2008;10:1026–32
- Mauri L, Foster E, Glower DD, Apruzzese P, Massaro JM, Herrmann HC, et al. 4-year results of a randomized controlled trial of percutaneous repair versus surgery for mitral regurgitation. J Am Coll Cardiol. 2013;62:317–28