Abstract
Objectives: Harmonic devices have become a world-wide standard for dissection and hemostasis in thyroidectomy. Numerous systematic reviews have reported superior operating times, blood loss, post-operative pain, length of stay, and overall safety outcomes. What has not been extensively evaluated in a robust manner is their economic impact. The purpose of this study is to evaluate the hospital costs associated with open thyroidectomy using Harmonic devices compared with conventional techniques for hemostasis. Methods: A systematic review of Medline, Scopus, and CENTRAL was performed from January 1, 2000 to May 23, 2014 without language restrictions for randomized clinical trials comparing Harmonic surgical devices to conventional methods in thyroidectomy. The main outcome measure was total reported costs. Costs were pooled using the ratio of means and a random effects model. Sensitivity analyses assessed whether differences in patient and trial characteristics, healthcare setting, or choice of statistical model affected outcomes. Results: Seven studies met the inclusion criteria. A total of 476 participants had procedures performed with Harmonic devices and 478 with conventional monopolar electrosurgery and clamp, cut and tie techniques. Compared with conventional techniques, Harmonic devices reduced total reported costs by 10% (p = 0.007), resulting in a $229 US dollars (USD) absolute reduction from mean baseline costs. Results remained relatively robust to additional sensitivity analyses. Conclusions: This systematic review and meta-analysis demonstrates that the Harmonic family of surgical devices is associated with a reduction in total reported costs in thyroidectomy compared with conventional techniques. A large portion of the overall savings derives from a reduction in operative costs.
Introduction
Thyroidectomy is one of the most commonly performed procedures in head and neck surgery in the world. In the US alone, more than 90 000 cases are performed each yearCitation1. Due to the high vascularization of the thyroid gland, effective hemostasis during surgery is crucial. In addition, meticulous dissection and minimal thermal injury are critical in avoiding injury to vital nerves for speech and the parathyroid glands. Conventional methods that may be used for hemostasis in thyroidectomy include classic clamp and tie techniques using sutures, metal clips, or staples, or electrosurgery including monopolar- and bipolar-electrosurgical devicesCitation2. Alternatively, Harmonic devices (Harmonic, Ethicon Endo-Surgery, Cincinnati, OH), developed in the early 1990s, have steadily increased in use. These instruments perform simultaneous ultrasonic cutting and coagulation through the use of mechanical vibration, producing hemostasis at a lower temperature than electrosurgical devices while providing excellent dissecting capabilityCitation3,Citation4. Numerous systematic reviews and meta-analyses have reported that harmonic devices are associated with reductions in operating timeCitation5–11, blood lossCitation5–8,Citation10,Citation11, post-operative painCitation8,Citation11, and length of hospital stayCitation8,Citation11 compared with conventional techniques. In addition, these meta-analyses substantiate that Harmonic devices are safe compared with conventional methods in thyroidectomy, are associated with reduced rates of hypocalcemia, and do not have a negative impact on nerve functionCitation5–11.
Given their common occurrence, thyroidectomy procedures are associated with substantial healthcare costs (hospital charges exceeded 2.5 billion US dollars in 2006)Citation1. Although Harmonic devices incur greater instrument costs than conventional techniques, their use is associated with lower hospital resources, such as operating time and length of stay, and so it might be anticipated that overall reported costs would be equivalent or lower. Two meta-analyses assessed costs and reported that ultrasonic coagulation was associated with significantly lower costs, or a trend towards lower costs, as measured by mean differences, compared with conventional methodsCitation5,Citation7. However, these studies failed to provide definitions of costs that were compared, did not include certain studies that reported hospital-related costs with Harmonic devicesCitation12–15, and only reported costs as one of many end-points. Furthermore, resource costs are commonly susceptible to variability depending on the setting both between and within countries, thus limiting the transferability and generalizability of cost estimatesCitation16–18. Mean difference (MD) was the effect measure used in these two meta-analyses and may not be the most appropriate methodology for cost outcomes. The ratio of means (RoM), as well as the ratio of geometric means (RoGM)Citation19, are recently proposed alternative measures suited for meta-analyses of continuous outcomes and that enable the handling of outcomes expressed in different unitsCitation20.
The purpose of this systematic review and meta-analysis is to apply novel methods, using all the latest evidence available, to comprehensively evaluate the total reported costs associated with open thyroidectomy surgery using Harmonic devices compared with conventional techniques for hemostasis.
Methods
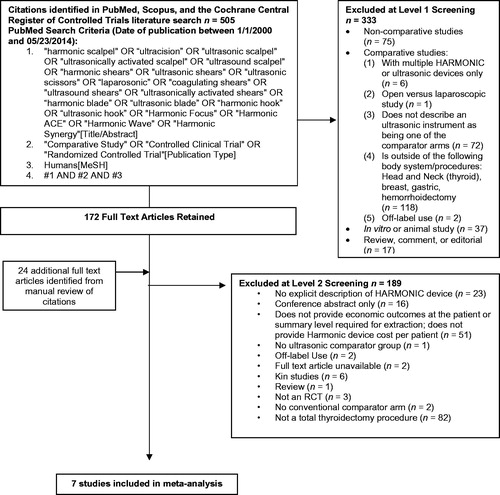
A systematic search of Medline via PubMed, Scopus and the Cochrane Central Register of Controlled Trials (CENTRAL) was performed on all indexed articles published between January 1, 2000 and May 23, 2014. The search strategy combined different terms used for Harmonic devices [Title or Abstract] with comparative study, controlled clinical trial or randomized trial [Publication Type] and Humans [MeSH] (Supplementary Appendix 1). A similar search ranging from November 23, 2013 through May 23, 2014 was conducted in PubMed without the human or publication type limits to capture publisher-supplied citations not yet indexed in MEDLINE. Additionally, a manual search of reference lists from accepted studies and recent reviews was performed to supplement the electronic search. Meeting abstracts were not searched. No language restrictions were applied in this systematic review.
Study inclusion criteria were defined according to PICOS categories (i.e. population, intervention, comparator, outcomes, and study design). All published randomized controlled trials (RCTs) comparing the use of Harmonic surgical devices to conventional methods, such as monopolar or bipolar electrosurgery and suture, clips, or knot tying in human subjects, in total thyroidectomy, were considered for inclusion (). Full text articles were then excluded if they were not a RCT, cost data were not provided for both groups, or the cost of the Harmonic device was not included. Multiple publications of the same or overlapping series of patients were identified and grouped together; the parent study was either the most recent publication or the publication providing the most comprehensive source of data. Data was only extracted from the parent study. The eligibility of each publication was evaluated by two independent reviewers (IS, NCF) and a third reviewer (HC) was consulted in the case of disagreements regarding study inclusion.
Table 1. Study and baseline characteristics for studies meeting inclusion criteria.
For included studies, details (i.e. baseline characteristics and outcomes) were extracted using a data extraction form developed in Excel. Data were extracted by a single reviewer and reviewed for accuracy, completeness, and consistency by a second reviewer. Discrepancies were resolved through consensus. The following data elements were extracted onto a standardized data collection sheet: type of surgical procedure, key patient characteristics, region, study design, devices and/or techniques utilized, number of patients, and detailed cost data.
The outcome measure of interest was total reported costs for thyroidectomy using a Harmonic device or conventional technique. Cost components comprising the definition of total reported costs included one or more of the following: operating room (OR) time, OR personnel, pre-operative exams, anesthesia time, drugs, length of stay, intra-operative resources, admission/discharge fees, and Harmonic scalpel device costs (see ). Mean total reported costs (original cost units) and standard deviations (SD) were extracted from the studies. In two studies, the SD was not reportedCitation12,Citation13. For one studyCitation12, the missing SD was imputed according to methods outlined by Hozo et al.Citation21, assuming a log-normal distribution. For the other studyCitation13, SD values reported by an alternative study with similar baseline costs, country of origin, and yearCitation22 were applied. One study provided the median and range for the total reported costsCitation13; therefore, assuming a log-normal distribution, the mean was imputed using methods outlined by Hozo et al.Citation21. Methods detailed by Altman and BlandCitation23 were applied to detect potential skewness in cost data, and subsequent sensitivity analyses were performed using the ratio of geometric means (RoGM)Citation19 if skewness was present. In all included studies, reported costs were converted to 2015 United States dollars (USDs) using the Campbell and Cochrane Economics Methods Group (CCEMG) and the Evidence for Policy and Practice Information and Coordinating Centre (EEPI-Centre) cost converter (Version 1.4)Citation24.
The Cochrane Collaboration toolCitation18 for assessing risk of bias was used to evaluate the quality of the included studies. For each RCT, the risk of bias for each domain (sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting, and other sources of bias) and across all domains was assigned as low, unclear, or high risk of bias. Two authors independently assessed the study quality. Differences were resolved through discussion with a third author.
The primary meta-analysis was performed with the ratio of means (RoM) (i.e. the ratio of the mean value in the experimental group and control group) as the effect measure for analyzing the cost outcome using methods outlined by Friedrich et al.Citation20. To conduct this analysis, the natural logarithm and standard error of each trial’s RoM, was calculated (see Supplementary Appendix 2 for equations). To pool results, the natural logarithm transformed ratios were aggregated across studies using the inverse-variance method in Review Manager (Version 5.3, The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark, 2014). The meta-analysis used a random effects model. Study heterogeneity was evaluated through the χ2 test and I2 measure.
The primary analysis compared the total reported costs (2015 USD) for Harmonic scalpel with conventional techniques. A sensitivity analysis was performed using the RoGM, instead of the RoM, to account for the inherent skewness in cost dataCitation19. Additional sensitivity analyses were also completed for a sub-set of the total reported costs, where only operative-specific costs were included in the analysis. In two studiesCitation15,Citation25, operative-specific costs were determined through the calculated addition of reported broken down cost components (i.e. OR utilization, OR personnel, disposables, and drug costs), excluding length of stay costs. Variance measures were imputed by the pooling of SD values reported for each cost component. One studyCitation26 did not report operative-specific costs and was, therefore, excluded from this sensitivity analysis. Country-specific sensitivity analyses were performed, excluding countries with developing economiesCitation15 based on classifications set by the United Nations Secretariat (UN/DESA)Citation27. Further sensitivity analyses were completed for the imputation of missing variance measures, where alternative methods of imputationCitation21 were used to determine the mean in one studyCitation13, or studies requiring imputation were excludedCitation12,Citation13. Additional sensitivity analyses included the conversion of all costs to 2015 Euros, the inclusion of one studyCitation28 differing in Harmonic scalpel device cost inclusion, and the exclusion of one studyCitation12 that did not have overlapping confidence intervals with the other studies. A sensitivity analysis was also conducted on total costs using a fixed effects model.
The overall percentage reduction in cost for all analyses was calculated using the RoM and was translated to an absolute reduction in cost by applying the percentage reduction in cost to the mean and range of baseline costs of conventional techniques.
Results
A total of 505 citations were identified from database searching, and 24 additional studies were identified through manual searches of accepted studies and published systematic reviews. Of the 505 citations identified in the search, 333 were excluded following abstract screening (). Of the 196 full text articles retrieved and reviewed, 189 were further excluded. Major reasons for exclusion included: studies were non-RCTs, the surgical procedure was not total thyroidectomy, there was no explicit description of a Harmonic branded device, inadequate data for economic outcomes, conference abstract only, and conventional methods were not included as a comparator. Overall, seven studies consisting of 954 patients in total reporting on the costs associated with Harmonic scalpel device or conventional method use in total thyroidectomy were included in the meta-analysisCitation12–15,Citation22,Citation25,Citation26. Although a systematic search using all the noted databases was not conducted to today’s date using our search criteria, a current PubMed search did not reveal any new relevant findings.
Study characteristics are presented in . Sample sizes of the included studies ranged from 40–261 patients, and in all studies Harmonic surgical devices were compared to conventional techniques in thyroidectomy. Different Harmonic devices were used in these analyses. The FOCUS device was used in two RCTsCitation14,Citation22; the Ultrasonic Harmonic scalpel and ACE in one RCT (Kowalski et al.Citation15; personal communication) and the HARMONIC CS-14C in one studyCitation25. Ultracision was used in three studiesCitation12,Citation13,Citation26. In total, three studiesCitation13,Citation14,Citation22 compared the Harmonic device to monopolar or bipolar electrocautery with one or more of sutures, clips, or clamp and tie. One studyCitation26 compared the Harmonic device to conventional clamp and tie, and oneCitation25 compared to knot tying. Ligature and cauterization was compared in one studyCitation12, and oneCitation15 compared to cut and ligature. One three-armed study included the Ligasure vessel sealing system as a comparator; however, cost data from this arm was excluded from the analysis. Of the seven included studies, the majority were EuropeanCitation12–14,Citation22,Citation25,Citation26, with one study from BrazilCitation15.
The overall results of the risk of bias assessments and individual study quality assessments are summarized in Supplementary Appendix 3. The randomization method was known in four studiesCitation13–15,Citation22. Two studies described randomization through the use of envelopesCitation13,Citation15, one used a random permuted block designCitation14, and one described the use of a drawing techniqueCitation22. Three studiesCitation13–15 described concealment of the randomization sequence. Blinding of patients to the surgical technique was reported in four studiesCitation14,Citation15,Citation22,Citation25, and two studiesCitation14,Citation15 reported blinding of the outcome assessors. Risk of performance bias was deemed low in non-blinded studies, as the cost outcome was considered objective and unlikely affected by a lack of blinding. There were minimal-to-no missing data or patient withdrawals in all of the included studies. Selective reporting remained unclear in six studiesCitation12–15,Citation25,Citation26, while one study was deemed to have a high risk of bias as a certain outcome noted in the protocol was not included in the resultsCitation22.
Primary analysis
The economic outcome of interest, total reported costs, was provided by all included studiesCitation12–15,Citation22,Citation25,Citation26. Mean total reported costs (2015 USD) for the procedure using the Harmonic scalpel ranged from $831.72–$2875.80, while mean total reported costs ranged from $896.65–$3042.84 with conventional techniques (). Of the included studies, 43% reported statistically significant reductions in total reported costs, while 29% reported numerical reductions in costs but were not statistically significant (). Reported Harmonic scalpel device costs ranged from $274.36–$408.48 2015 USD in included studies. The primary meta-analysis results showed that mean total reported costs were statistically significantly reduced by 10% (RoM =0.90; 95% CI =0.83–0.97; p = 0.007; seven studies; I2 = 96%) with the Harmonic scalpel device compared to conventional methods in total thyroidectomy (). This translates to a $229.27 (range = $89.67–$304.28) absolute reduction from mean (conventional) baseline costs with the Harmonic scalpel device ().
Figure 2. Proportion of included studies reporting statistically significant or non-significant reductions or increases in total reported costs using the Harmonic scalpel compared to conventional methods.
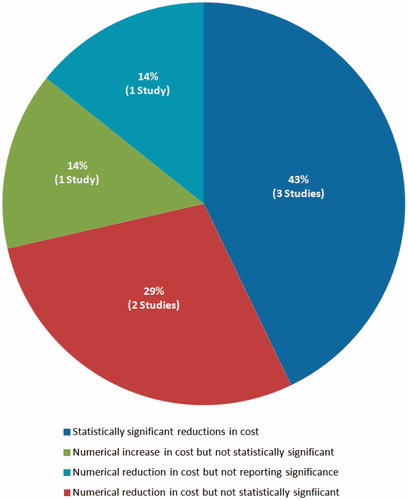
Figure 3. Forest plot of primary meta-analysis results for total reported costs (USD) expressed as ratio of means.
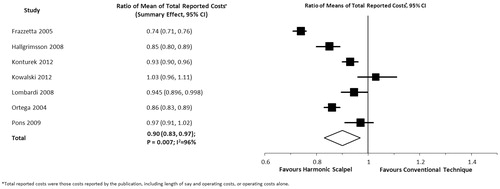
Table 2. Cost inputs and assumptions for primary analysis on total reported costs.
Table 3. Percentage and absolute reduction in total reported costs with Harmonic scalpel compared with conventional care.
Sensitivity analyses
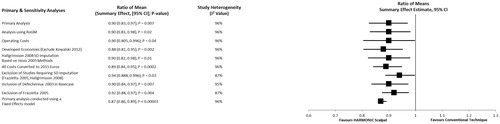
Results of sensitivity analyses were relatively similar to the primary analysis and remained statistically significantly in favor of the Harmonic scalpel device in total thyroidectomy (). Sensitivity analysis results using the RoGM method demonstrated a statistically significant reduction in mean total reported costs by 10% (RoGM =0.90; 95% CI =0.83–0.98; p = 0.02; seven studies; I2 = 96%) with the Harmonic scalpel device compared to conventional methods in total thyroidectomy (). This translates to an identical absolute reduction from mean baseline costs with the Harmonic scalpel device as compared with the primary analysis (). Operative-specific costs were reported by six of the seven included studiesCitation12–15,Citation22,Citation25, and comprised the majority of the total reported costs. When only operative-specific costs were included in the analysis, a statistically significant reduction by 10% (RoM =0.90; 95% CI =0.805–0.996; p = 0.04; six studies; I2 = 96%) was reported with the Harmonic scalpel device compared to conventional methods in total thyroidectomy (, ). Thus, the Harmonic scalpel device resulted in an absolute reduction in mean (conventional) baseline costs of $236.27 (range = $89.67–$304.28) (). When the primary meta-analysis of total reported costs was conducted using a fixed effects model, a 13% reduction in costs (absolute reduction in mean baseline costs: $298.05) was reported with the Harmonic scalpel (RoM =0.87; 95% CI =0.86–0.89; p < 0.000 01) (, ). The exclusion of developing economiesCitation15, and conversion of all costs to 2015 Euros resulted in a large reduction in total reported costs with the Harmonic scalpel device, with cost reductions of $266.44 (RoM =0.88; 95% CI =0.806–0.951; p = 0.002) and $252.20 (RoM =0.89; 95% CI =0.842–0.948; p = 0.0002), respectively (, ).
Discussion
Thyroidectomy is a very common procedure with a high associated economic burdenCitation1. Consequently, it is important to assess methods by which such costs may be reduced. Our study is the most comprehensive meta-analysis that focused on the assessment of total reported costs in thyroidectomy procedures using Harmonic devices compared with conventional methods in thyroidectomy. Using the most appropriate methods possible for pooling and interpreting cost data, our findings demonstrate that Harmonic devices are associated with lower total reported thyroidectomy costs compared with conventional methods. In absolute terms, the cost savings associated with Harmonic device use is estimated to be over $200 USD per procedure.
The results of our primary analysis remained reasonably consistent when sensitivity analyses were conducted that limited studies based on type of cost, country of origin, data imputation of results, base currency, differences in assumptions about Harmonic device costs, and when using the ratio of geometric means as an alternative analysis method. The overall quality of the included studies was evaluated by methods outlined by CochraneCitation18. Findings demonstrated that the included studies were of acceptable quality, with fairly low risk of bias.
Two previously published meta-analyses have included costs as one of many outcomes comparing ultrasonic coagulators (including Harmonic surgical devices), or advanced bipolar technology to conventional techniques in thyroidectomyCitation5,Citation7. In a recent network meta-analysis (NMA) by Garas et al.Citation7, Harmonic surgical devices were compared to both advanced bipolar technology (Ligasure) and conventional techniques. This NMA demonstrated that both ultrasonic coagulation and advanced bipolar techniques maintained a key advantage over conventional clamp-and-tie techniques, reporting significant reductions in OR timeCitation7. When comparing ultrasonic coagulation with clamp-and-tie methods, significant differences were reported in costs, in favor of ultrasonic coagulation (standardized mean difference (SMD) = −0.57; 95% CI = −1.07 to −0.07; p = 0.03; four studies)Citation7. Although Harmonic surgical device costs are significantly greater than those of conventional techniques (Harmonic $255Citation7,Citation29, plus generator costs), Garas et al.Citation7 reported that ultrasonic coagulation may represent a cost-effective hemostatic method for thyroidectomy, as reductions in operative time and length of stay (LOS) outweigh these increased device costs. An important limitation to the Garas et al. study is the use of the SMD in the reporting of cost results, given difficulties with interpretation of such effect sizes. In contrast, our study used the RoM (and RoGM), which also facilitates combining costing data across healthcare settings, but enhances interpretation compared to SMD. RoM reports a percentage reduction in costs as opposed to a SMD. The SMD is not very useful to clinicians and decision-makers because it requires knowledge of the pooled SD, a quantity generally unknown. In a second meta-analysis conducted by Zhang et al.Citation5, it was found that the ultrasonic coagulator similarly demonstrated reductions in OR time and total hospital costs trended in favor of the Harmonic scalpel compared to conventional techniques (MD = −107.92; 95% CI = −229.25 to 13.41; p = 0.08; two studies). Zhang et al. only included two studies in the cost meta-analysis and also only reported mean differences as the effect measure.
Both the aforementioned NMA and meta-analysisCitation5,Citation7 failed to provide definitions of the costs that were compared, while the current analysis is the first of its kind to provide a detailed cost component breakdown and specifically meta-analyze total reported costs. Furthermore, in contrast to these previous publications, the current study was limited to Harmonic surgical devices and conventional techniques, and included only RCTs. The present analysis used emerging meta-analytic methods for continuous outcomes to pool cost data. Pooling across regions is challenging as resource use and associated costs are sensitive to between and within country variability due to heterogeneity in health systems and variation in treatment practices. Consequently, generalizability and transferability of one region’s cost estimates to another region is limitedCitation16–18. As such, our analysis has adhered to best practices and demonstrated methodological rigor in order to help address this limitation. Careful assessment and reporting of the cost components included in each identified study, for the analysis of total reported costs, was conducted to optimize interpretability and to partition analyses. Baseline costs were all converted to a common currency, taking into consideration inflation of costs. Additionally, the RoM effect measure was selected as it allows for the handling of outcomes expressed in different units and does not require knowledge of the pooled SDCitation20. In contrast to SMDs, this approach also facilitates ease of interpretation of effect importanceCitation20. Furthermore, in reviewing the potential concern of skewness in cost data, a sensitivity analysis was conducted using the RoGM method, an alternative effect measure for analyzing skewed continuous dataCitation19. This alternative analysis produced findings that were consistent with those from our primary analysis for total costs, providing further confidence in the results.
Typically, newer interventions are costlier and more effective than existing interventions, necessitating the calculation of an incremental cost-effectiveness ratio to determine relative value. However, published meta-analysesCitation5,Citation7 suggest that ultrasonic coagulators (including Harmonic surgical devices) are associated with lower costs and are more effective than conventional methods, although Zhang et al.Citation5 did not report a statistically significant difference. In that regard, it is noteworthy that traditional rules of inference are not often applied when considering costs and cost-effectivenessCitation30. Rather, decisions should be based only on the mean net benefits, irrespective of whether differences are statistically significantCitation30. In this light, it appears that ultrasonic coagulators (including Harmonic surgical devices) would be considered to represent good value for healthcare systems, as assessed by traditional health economic benchmarks, and not withstanding significant benefits to patients.
For hospital cost analyses, there is variability in the literature in terms of whether all types of hospital costs are considered or only certain cost domains. The relevance of assessing different cost categories varies, likely by hospital decision-maker and by hospital, as there is no set process common to all hospitals. As the US healthcare reform rules change, we know that it is more relevant to consider more comprehensive costs (e.g. evaluate the entire episode of care rather than just the initial procedure) in US hospital economic analyses. Our analysis tries to take into account the range of costs that are included across studies to produce a more holistic view of how adopting Harmonic technology can affect total hospital costs rather than one domain only. At a minimum, the studies included in this meta-analysis included possible resources, such as operative time, that could offset the initial device costs. Some, but only a few studies, went beyond the operative budget and included the length of hospital stay differences. This was possible because the clinical trials collected data on hospital length of stay. As such, costing studies are dependent on the resource use data collected from clinical trials. In summary, the more resource use data that can be collected from clinical trials, the more comprehensive a cost analysis can be, and, thus, the more relevant to multiple decision-makers.
Although this study addressed important limitations from previous cost meta-analyses, some limitations remain. First, as noted, there was variability in the components included within the definitions of costs across studies. However, for the majority of studies, total reported costs were mainly composed of operating costs. Specifically, in four of the included studiesCitation12–14,Citation22, total reported costs were comprised of operating-specific costs only, and in two studiesCitation15,Citation25 the majority of the total reported costs were operating-specific. As such, sensitivity analyses showed that cost savings were similar in magnitude when focusing on operative costs compared with the primary analysis. Therefore, a large proportion of the total cost savings observed in this analysis are likely attributed to a decrease in operative time and resources with the Harmonic scalpel. Furthermore, unlike other published reports, we ensured that the cost of the Harmonic device was always included in total reported costs for each study. However, the cost of the Harmonic device was based on that reported in the study—decision-makers should ensure that these costs are reflective of their setting. Second, I2 values were high between studies, despite the majority of studies reporting numerical reductions in costs in favor of the Harmonic scalpel, albeit not statistically significant. This is a somewhat expected limitation when pooling costing data across regions, and when there are effect estimates that do not overlap. To address this, a random effects model was used to pool all outcome data. Further, multiple sensitivity analyses were conducted to ensure findings were robust. Findings remained largely unaltered, although I2 values were only minimally changed. Third, an additional limitation included the lack of some data to inform variance inputs for the meta-analysis. In order to overcome this, imputation methods and assumptions outlined by CochraneCitation18 and Hozo were employed. When alternative imputation methods were utilized, or studies requiring imputation were excluded in sensitivity analyses, the results remained relatively similar to the primary analysis. Fourth, our study did not meta-analyze costs for Harmonic scalpel vs Ligasure, given only one studyCitation22 was available to inform this. This single study reported, however, that the total operative time and costs were significantly less with the Harmonic scalpel vs Ligasure. Lastly, the studies included in this analysis were mainly from European countries. Although this is beneficial in terms of limiting diversity for pooling cost data, future study is warranted to determine if similar findings are exhibited across other developed or developing regions.
Conclusions
This systematic review and meta-analysis demonstrates that the known clinical benefits of using the Harmonic scalpel to perform thyroidectomies are further supported by positive health economic benefits. Specifically, our results demonstrate the benefits of Harmonic devices in comparison to conventional techniques in reducing total reported costs for total thyroidectomy procedures. Limitations in the interpretation of cost results due to the variability in cost components amongst studies also highlights the need for additional studies that use standardized cost definitions and that come from a wider geographic area. In conclusion, the Harmonic family of devices improves efficiency, enhances surgical safety, and reduces costs to the hospital and society when they are used to perform thyroidectomy.
Transparency
Declaration of funding
This work was supported by Ethicon, Inc., manufacturer of the Harmonic Focus and Focus+, who provided funding to conduct the analysis and prepare the manuscript.
Declaration of financial/other relationships
HC, JWC, and JFA are employees of Ethicon, Inc., manufacturer of the Harmonic family of devices. NCF, CGC, and IMS are employees of Cornerstone Research Group, who were sponsored to perform this study by Ethicon, Inc. JME peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Supplementary_Appendix.docx
Download MS Word (74.7 KB)References
- Sun GH, DeMonner S, Davis MM. Epidemiological and economic trends in inpatient and outpatient thyroidectomy in the United States, 1996-2006. Thyroid 2013;23:727-33
- Butskiy O, Wiseman SM. Electrothermal bipolar vessel sealing system (LigaSure) for hemostasis during thyroid surgery: a comprehensive review. Expert Rev Med Devices 2013;10:389-410
- Carlander J, Johansson K, Lindstrom S, et al. Comparison of experimental nerve injury caused by ultrasonically activated scalpel and electrosurgery. Br J Surg 2005;92:772-7
- Bandi G, Wen CC, Wilkinson EA, et al. Comparison of blade temperature dynamics after activation of Harmonic Ace scalpel and the Ultracision Harmonic Scalpel LCS-K5. J Endourol 2008;22:333-6
- Zhang ZJ, Zhang P, Tian JH, et al. Ultrasonic coagulator for thyroidectomy: a systematic review of randomized controlled trials. Surg Innov 2010;17:41-7
- Contin P, Goossen K, Grummich K, et al. ENERgized vessel sealing systems versus CONventional hemostasis techniques in thyroid surgery–the ENERCON systematic review and network meta-analysis. Langenbecks Arch Surg 2013;398:1039-56
- Garas G, Okabayashi K, Ashrafian H, et al. Which hemostatic device in thyroid surgery? A network meta-analysis of surgical technologies. Thyroid 2013;23:1138-50
- Ecker T, Carvalho AL, Choe JH, et al. Hemostasis in thyroid surgery: harmonic scalpel versus other techniques–a meta-analysis. Otolaryngol Head Neck Surg 2010;143:17-25
- Melck AL, Wiseman SM. Harmonic scalpel compared to conventional hemostasis in thyroid surgery: a meta-analysis of randomized clinical trials. Int J Surg Oncol 2010;2010:396079
- Cirocchi R, D'Ajello F, Trastulli S, et al. Meta-analysis of thyroidectomy with ultrasonic dissector versus conventional clamp and tie. World J Surg Oncol 2010;8:112
- Cheng H, Soleas I, Ferko NC, et al. A systematic review and meta-analysis of Harmonic Focus in thyroidectomy compared to conventional techniques. Thyroid Res 2015;8:15
- Frazzetta M, Furgiuele G, Raimondo D, et al. [Ultrasonic dissector for total thyroidectomy: results of prospective randomized study]. G Chir 2005;26:295-301
- Hallgrimsson P, Loven L, Westerdahl J, et al. Use of the harmonic scalpel versus conventional haemostatic techniques in patients with Grave disease undergoing total thyroidectomy: a prospective randomised controlled trial. Langenbecks Arch Surg 2008;393:675-80
- Konturek A, Barczynski M, Stopa M, et al. Total thyroidectomy for non-toxic multinodular goiter with versus without the use of harmonic FOCUS dissecting shears - a prospective randomized study. Wideochir Inne Tech Maloinwazyjne 2012;7:268-74
- Kowalski LP, Sanabria A, Vartanian JG, et al. Total thyroidectomy with ultrasonic scalpel: a multicenter, randomized controlled trial. Head Neck 2012;34:805-12
- Drummond M, Pang F. Transferability of economic evaluation results. In: Drummond M, McGuire A, eds. Economic evaluation in health care: merging theory with practice. New York, NY: Oxford University Press, 2001
- Sculpher MJ, Pang FS, Manca A, et al. Generalisability in economic evaluation studies in healthcare: a review and case studies. Health Technol Assess 2004;8:iii-iv, 1–192
- Higgins J, Green S. The Cochrane handbook for systematic reviews of interventions. 2011. Wiley & Sons, Ltd. West Sussex, England http://www.cochrane-handbook.org. Accessed July 2015
- Friedrich JO, Adhikari NK, Beyene J. Ratio of geometric means to analyze continuous outcomes in meta-analysis: comparison to mean differences and ratio of arithmetic means using empiric data and simulation. Stat Med 2012;31:1857-86
- Friedrich JO, Adhikari NK, Beyene J. Ratio of means for analyzing continuous outcomes in meta-analysis performed as well as mean difference methods. J Clin Epidemiol 2011;64:556-64
- Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 2005;5:13
- Pons Y, Gauthier J, Ukkola-Pons E, et al. Comparison of LigaSure vessel sealing system, harmonic scalpel, and conventional hemostasis in total thyroidectomy. Otolaryngol Head Neck Surg 2009;141:496-501
- Altman DG, Bland JM. Detecting skewness from summary information. BMJ 1996;313:1200
- CCEMG. E-C. CCEMG - EPPI-Centre Cost Converter. 2014. eppi.ioe.ac.uk/costconversion/Default.aspx. Accessed January 2015.
- Lombardi CP, Raffaelli M, Cicchetti A, et al. The use of “harmonic scalpel” versus “knot tying” for conventional “open” thyroidectomy: results of a prospective randomized study. Langenbecks Arch Surg 2008;393:627-31
- Ortega J, Sala C, Flor B, et al. Efficacy and cost-effectiveness of the UltraCision harmonic scalpel in thyroid surgery: an analysis of 200 cases in a randomized trial. J Laparoendosc Adv Surg Tech A 2004;14:9-12
- Department of Economic and Social Affairs of the United Nations Secretariat. Country classification: data sources, country classifications and aggregation methodology. New York, United Nations, 2014
- Defechereux T, Rinken F, Maweja S, et al. Evaluation of the ultrasonic dissector in thyroid surgery. A prospective randomised study. Acta Chir Belg 2003;103:274-7
- Voutilainen PE, Haglund CH. Ultrasonically activated shears in thyroidectomies: a randomized trial. Ann Surg 2000;231:322-8
- Claxton K. The irrelevance of inference: a decision-making approach to the stochastic evaluation of health care technologies. J Health Econ 1999;18:341-64