Abstract
Anxiety disorders are common and costly psychiatric illnesses. Pharmacological treatment was enhanced with the introduction of benzodiazepines, which proved safer and more effective than older drugs. The risk of dependence, however, has made clinicians reluctant to use these medications. In fact, few patients appear to develop significant difficulties with these drugs, given how widely they are used. Careful planning for discontinuation of therapy is important. In addition, for some individuals, there appears to be a complex and as yet unelucidaied relationship between dependence on drugs or alcohol and anxiety. The newer antidepressants offer efficacy without abuse or dependence liability, but are expensive and have side effects that are intolerable for some patients. Pharmacological therapy for anxiety should be prescribed and managed so as to minimize any existing risk, while aiming to restore the patient to wellness in terms of symptoms and function.
Los trastornos de ansiedad son enfermedades psiquiátricas comunes y de alto costo económico. El tratamiento farmacológico mejoró con la introducción de las benzodiazepinas, lo que resultó ser más seguro y efectivo que con los fármacos más antiguos. Sin embargo, el riesgo de dependencia ha determinado que los clínicos sean reticentes con el uso de estos medicamentos. Sin embargo, teniendo en cuenta el amplio uso de este típo de fármacos, los problemas reaies detectados a nivel de paciente, no son significativos. Es importante un plan cuidadoso para discontinuar el tratamiento. Además, en algunos sujetos parece existir una compleja relación aun no aclarada entre la dependencia a drogas o alcohol y la ansiedad. Los antidepresivos más modernos ofrecen gran eficacia sin riesgo de abuso o dependencia, pero son caros y tienen efectos secundarios que resultan díficiles de soportar para algunos pacientes. La terapia farmacológica para la ansiedad debe ser prescrita y manejada con dos objetivos: minimizar cualquier riesgo existente y orientarse hacia la recuperación del bienestar del paciente en términos somáticos y funcíonales.
Les troubles anxieux sont des maladies psychiatriques fréquentes et onéreuses. Le traitement pharmacologique a été amélioré par l'introduction des benzodiazépines, qui se sont révélées plus sûres et plus efficaces que les médicaments plus anciens. Cependant, le risque de dépendance a rendu les praticiens réticents à les utiliser. En pratique, peu de patients semblent rencontrer de réels problèmes avec ces médicaments, eu égard à leur très large utilisation. Une planification soigneuse du sevrage thérapeutique est importante. De plus, une relation complexe et encore non élucidée entre la dépendance médicamenteuse ou alcoolique et l'anxiété semble exister chez certains sujets. Les antidépresseurs plus récents se caractérisent quant à eux par une efficacité sans risque d'emploi abusif ou de dépendance. En revanche, ils sont coûteux et provoquent des effets indésirables insupportables chez certains patients. La prescription et le suivi du traitement pharmacologique de l'anxiété ont comme double objectif de restaurer la bonne santé du patient tant sur le plan des symptômes que de son fonctionnement, tout en réduisant au minimum les risques existants.
Anxiety disorders
Anxiety is a universal response to threatening or frightening situations. Those individuals who present with more pronounced or persistent symptomatology, or without any reasonable context, may in fact, meet, the diagnostic criteria for an anxiety disorder. Such disorders include generalized anxiety disorder (GAD) and panic disorder (PD), as well as obsessive compulsive disorder (OCD), social anxiety disorder, posttraumatic stress disorder, phobias, and a number of other diagnoses.Citation1 Universal estimates of prevalence are difficult, to obtain, but, among US residents age 18 to 54, the National Institute of Mental Health reports that 19 million Americans (approximately 13%) have anxiety disorders.Citation2 In the case of GAD, for which diagnostic criteria were first introduced in the Diagnostic and Statistical Manual, of Mental Disorders, Third Edition Citation3 (DSM-III) and later also added to the International Classification of Mental and Behavioral Disorder Citation4 (ICD10), there has been some question as to whether this is indeed a separate disorder or part of a continuum of another disorder, such as depression.Citation5 Investiga-tions suggest that GAD is a distinct and common disorder,Citation5,Citation6 with lifetime prevalences reported up to 7%.Citation7-Citation11 PD and the other diagnoses appear less common.Citation8 Some data indicate that anxiety disorders result in more occupational disability and cost, society more than affective disorders or schizophrenia, and yet are vastly undertreated.Citation12 Estimates suggest that both psychiatrists and primary care physicians encounter GAD and other anxiety disorders frequently.Citation13-Citation15 Making an accurate diagnosis can be difficult - particularly in primary care settings - because of time constraints on patient contact and the fact that patients often present, with physical rather than psychological or emotional complaints.
After the diagnosis of any anxiety disorder has been established, treatment of patients with either acute or chronic anxiety can be complicated by the concern that one useful class of drugs that had shown efficacy and medical safety in treatment settings, namely the benzodiazepines,Citation16-Citation19 also has the liability of potentially producing dependence with chronic use.Citation20-Citation25 Reclassification attempts, regulatory actions, and dramatic anecdotal presentations of the possible problems of these medications, often in the general media, are part, of what, has led to an overall decrease in benzodiazepine use, sometimes with the substitution of older, less safe, and less efficacious medications.Citation26,Citation27 Such prescribing decisions affect, large numbers of patients of both psychiatrists and primary care physicians, undoubtedly including some patients with anxiety disorders. More recently, newer antidepressants, the selective serotonin reuptake inhibitors (SSRIs),havc shown efficacy in anxiety disorders without raising the same concerns about dependence.Citation28-Citation31 These medications do have their own side effects and liabilities, which can influence the ability of patients to adhere to therapy, however.Citation32 In addition, many of these medications remain some of the most expensive drugs on the market. The benzodiazepines, by contrast, are largely available as generic medications and have become very inexpensive.
Other medications have shown efficacy in anxiety disorders, but these drugs also have their own drawbacks.Citation29 Buspirone is one of a number of compounds of the azapirone group.Citation33,Citation34 It is structurally unrelated to the benzodiazepines, and although its mechanism of action is not entirely known, it appears to be at least, partially dependent on decreasing serotonergic nerve fiber activity.Citation29 Buspirone shows anxiolytic activity after a number of weeks and does not appear to have any dependence liability. Its efficacy, however, does not appear to match that of the benzodiazepines in some studies, and it is not helpful in controlling acute anxiety. Older antidepressants have been shown to have anxiolytic properties and are sometimes used in the treatment of anxiety.Citation22 The tricyclic antidepressants, such as imipramine, relieve some symptoms in patients with generalized anxiety. The adverse effects of these drugs are numerous, however, and their narrow margin of safety in overdose situations diminishes their usefulness.
In an effort, to expand treatment options to include remedies that seem to some to be more “natural,” and therefore implying lower risk, herbal or other alternative medicine-based therapies, such as kava, are also being used.Citation35-Citation37 Knowledge on the safety and efficacy of these often unregulated products is continuing to accumulate.Citation38,Citation39 Kava, for example, has been reported to show efficacy, and little physiologic or learned tolerance was apparent in animal models at low doses. Higher doses, however, reportedly do result, in some physiologic tolerance. In addition, kavakava was the focus of a consumer advisory alert from the USA Food and Drug Administration (FDA) in 2002 because of reports from Europe and the USA of serious hepatotoxicity:Citation10 It is not yet clear whether such toxicity is a result, of the chemical constituents of the herb itself or to the presence of unexpected or unknown compounds, which could be introduced during manufacturing or formulation. It is also possible that interactions with other substances, such as ethanol, may potentiate the toxic potential of a compound present in the preparation.
Because of the expense of newer medications as well as safety and efficacy concerns about some older or alternative medications, the possibility still remains that for many patients with anxiety disorders, the best, available treatment will be a benzodiazepine. Understanding what has been learned about benzodiazepine use and the development, of dependence may be helpful in ensuring that, these patients are not denied effective treatment.Citation41
Dependence
The reported potential of a class of prescription drugs to result, in dependence in some patients needs to be viewed as part, of an overall risk-benefit analysis in the same way as that process is applied to nonpsychiatric medical illness. Many other authors have commented on the historical biases that, have been present in shaping social views on the acceptability of treating illnesses such as anxiety and depression with pharmacological intervention. The presence of what, has eloquently been called “pharmacological Calvinism” is still a factor in the acceptability of the appropriateness of biologically based treatments for these disorders.Citation26 The context in which medications are used includes the suffering and disability caused by the condition being treated as well as the overall risks of a proposed therapy for a given patient.
Definitions of substance dependence often lack consistency, but, they usually include a number of criteria composed of issues relating to psychological dependence and/or physical dependence.Citation1 In many characterizations, there are overlaps with abuse and addiction. Table I summarizes the Diagnostic: and Statistical Manual of Mental Disorders, Fourth Edition Citation1 (DSM-LV) criteria for dependence. A central concept is the exhibition of a maladaptive pattern of substance use leading to clinically significant impairment or distress. Accompanying features may include tolerance, which can result in an escalation in dose, and patients may spend inordinate amounts of time obtaining, using, and recovering from the drug. Drug seeking and drug use may become more important, than customary social, recreational, and occupational obligations and activities, and the patient, often knows that, the use of the drug may be causing physical and/or psychological problems. Attempts to control or reduce substance use are unsuccessful, and a withdrawal syndrome characteristic for the given substance may occur. Although much of the focus on dependence emphasizes what happens when the drug is discontinued, concerns about reinforcing effects with acute administration are also important. Euphorogenic effects, which have been described as enhancing abuse liability, are also a component of the discussion of psychological dependency.
Table I. Characteristics of the substance dependence syndrome. “Physiological dependence” is present if either Item 1 or Item 2 is applicable. Adapted in part from reference 1.
Benzodiazepines
First introduced in the 1960s with the appearance of chlordiazepoxidc and diazepam, the benzodiazepines quickly supplanted the barbiturates as the preferred treatment of most, anxiety disorders.Citation18,Citation19,Citation42 They have shown efficacy in both acute and chronic anxiety states, and they have a wide margin of medical safety. As a class, they also have utility as anticonvulsants, muscle relaxants, hypnotics, and adjuncts to anesthesia and conscious sedation. Some effects, such as sedation and anterograde amnesia, are a desirable effect in certain settings, such as in the treatment of insomnia or in the endoscopy suite, but are considered undesirable side effects under circumstances such as the treatment, of anxiety. Tolerance appears to develop over time to some of the sedating properties of the benzodiazepines. Tolerance to other effects also seems to occur, but along distinctly different time courses, suggesting mechanistic differences. Abrupt, discontinuation can lead to insomnia and anxiety after more than a couple of weeks of using short-acting benzodiazepines to treat, sleep disorders. Patients who have been receiving daily therapy with longer-acting agents for anxiety and other diagnoses, and whose therapy has been suddenly halted or reduced, can experience a range of withdrawal symptoms.Citation18 These are usually mild and transient, and may include both psychological and physical symptoms. Heightened anxiety, tremor, tachycardia, and photophobia are some of the symptoms that, are often reported. In extreme cases following prolonged therapy with high doses, seizures and delirium can occur. The duration of therapy, dose of medication, and manner in which therapy is discontinued are all important determinants of whether a withdrawal syndrome will occur and how severe it will be. It is important to keep in mind that other medications that are not, thought of as having dependence liability also cause a physiologic “rebound” or other pronounced adverse effects if stopped abruptly. βP- Adrenergic blockers are one example of such a medication. These drugs are therapeutically important, in patients with hypertension and coronary artery disease, with proven efficacy in reducing actual mortality in some cohorts, but they can result in a withdrawal syndrome if therapy is suddenly stopped. Signs and symptoms can include a return of hypertension as well as tremor, palpitations, and sweating, and can be as severe as the precipitation of arrhythmias and unstable angina, in patients with severe underlying coronary disease. Hence, benzodiazepines are not unique in their ability to cause clinical difficulties after sudden, unstructured discontinuation.
All benzodiazepines interact with the γ-aminobutyric acid receptor (GABAA) and produce similar physiological and clinical effects.Citation43,Citation44 The anxiolytic effect, appears to be mediated by the alpha-2 subunit, of the receptor complex. Preferred terminology refers to these drugs as positive modulators since they do not have any effect in the absence of GABA. With chronic exposure, a number of molecular effects have been reported.Citation43-Citation45 Downregulation of binding sites with a reduction in the number of the GABAA receptors is one molecular phenomenon that has been proposed as a mechanism for tolerance. Other changes that have been reported include changes in mRNA, a disturbance in the linking relationship between the benzodiazepine site and GABA, and perturbations in the rate of turnover of subunits of the benzodiazepine receptor. Determinations of whether these findings can be directly and causally linked to tolerance and discontinuation syndromes have been difficult, because of the differences in timing of the molecular and clinical phenomena.Citation46,Citation47 Molecular changes seem to occur more quickly than the development, of clinical tolerance.
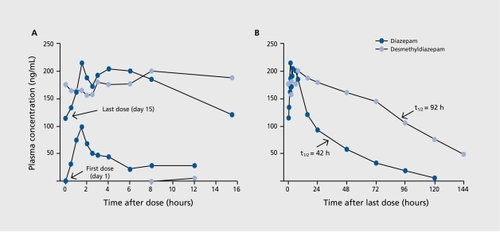
Although the benzodiazepines work via a common mechanism of action, there are definite pharmacokinetic and metabolic differences that affect, the presence and concentration of an active entity at the molecular site of action.Citation48 These differences determine the clinical indications for which a given benzodiazepine is used, and they also result, in differences in clinical course once an administered medication is discontinued.Citation49-Citation51 The most important factors in this realm arc the speed at which the parent drug is cleared and the presence or absence of pharmacologically active metabolites (Table II). As an example, for a drug such as diazepam, the parent, drug is cleared slowly, and at least, three metabolically active compounds are generated during the course of its clearance. Some of these compounds are actually separate benzodiazepine entities available for prescription is their own right. After one 10 mg dose of diazepam, pharmacologically active metabolites are detectable for at least 2 weeks. Hence, even with abrupt, discontinuation of diazepam, an intrinsic tapering process results (). The potency of a given benzodiazepine parent drug at the site of activity is not a major determinant of clinical differences, since dosages are adjusted to produce a clinical effect, through the same molecular mechanism.
Table II. Representative benzodiazepine derivatives in clinical use as antianxiety agents. The usual range of elimination half-life is shown in parentheses. * Prodrug, converted to desmethyldiazepam.
Interestingly, other physical differences between diazepam and some other benzodiazepines may affect, its abuse potential among some patients. Diazepam is exceedingly lipophilic, with nearly immediate central nervous system (CNS) penetration upon administration.Citation52,Citation53 The speed of onset of sensation has been linked to abusability for other medications, such as opiates, and may be a factor for some patients treated with diazepam. For those involved with use of illicit drugs, including the illegal use of benzodiazepines, investigators have not been able to designate any particular benzodiazepine as preferentially abused. Instead, many factors in a local drug use culture seem to be important in determining the individual user's benzodiazepine of choice.Citation26
Most, information indicates that treatment with benzodiazepines for at least, a few weeks is needed before withdrawal is generally a serious concern, and that, withdrawal is most, likely to occur when shorter-acting agents are stopped abruptly. Taper regimens have been described to lessen the difficulty in discontinuing benzodiazepine therapy.Citation51,Citation54 Most, emphasize that the initial decrement, in dosage can be fairly rapid, with some authors aiming for getting to one-fourth to one-half of the initial dosage over the course of the first, month. Others aim for a dosage equivalent, to approximately 10 mg diazepam. Tapering from that point is slow, especially in patients with panic disorders, and patients may remain at steady, low doses of benzodiazepines for many months.
Difficulty in tapering, with more pronounced withdrawal symptoms, does not seem to predict inability to successfully complete the taper. Psychological support, appears to be a critical factor in this process.Citation55 A number of pharmacological agents have been proposed as useful adjuncts during the withdrawal process.Citation54,Citation56 These include P-adrenergic blockers, antidepressants, and buspirone. The majority of patients treated with chronic benzodiazepines arc able to successfully taper off their therapy. In a study that looked at, those completing the taper, most, were still not, requiring benzodiazepines 3 years later.Citation54 The issue of whether differences among treatment regimens (as needed versus scheduled dosing) can result in differing propensities for leading to discontinuation syndromes or dependence has also been raised and continues to be investigated.Citation57
Research into the relationship between the benzodiazepines and dependence in patients with anxiety disorders has failed to produce a consensus opinion regarding causality. There seems to be wide agreement, among investigators of this topic that, most, patients who use benzodiazepines do not generally misuse these medications or become chronically dependent, on them.Citation17,Citation26 Hence, in discussing those who abuse benzodiazepines or cannot, discontinue therapy, it is important, to keep in mind that, this constitutes a minority of patients who are treated with these drugs. Investigating whether certain subgroups of patients might, be at increased risk of developing significant dependence from treatment is an extremely important, issue in the treatment of anxiety, since many of these patients require relatively long periods of treatment. The risk of dependence in general is felt to increase also with the presence of some patient factors. These include - but are not limited to - the nature of the diagnosis at the time of treatment initiation, the level of anxiety prior to treatment, the presence of personality disorders, and a current or past history of substance abuse or dependence.Citation54,Citation55,Citation58 For some chronically treated patients, it, appears that, the development, of a “withdrawal syndrome,” which would suggest physical and psychological dependence and results in difficulty in stopping drug treatment, may in fact be at least in part a reemergence of the original pathology that initially required treatment. Similar phenomena occur following the discontinuation of antidepressants and antipsychotics in some patients, with the ensuing reemergence of depression and psychosis, respectively.
In addition, for some individuals, there appears to be a reciprocating and complex relationship between anxiety and dependence on other substances.Citation59-Citation68 Individuals dependent on other nonbenzodiazepine medications, such as analgesics, as well as alcohol, nicotine, and illicit, drugs, are often reported to have concomitant anxiety disorders. The extent to which independent anxiety disorders and substance abuse are related has not been resolved. Study of this issue has been complicated by many factors, including the fact that drug use and withdrawal can precipitate anxiety symptoms. It, has been postulated that some individuals may have become dependent, on substances while trying to self-medicate anxiety or other psychiatric disorders. Alternatively, another variable, such as a genetic factor, may promote both conditions. Because of this possible link between dependence as a phenotype and dependence difficulties with multiple substances, the traditional recommendation has been to avoid the use of benzodiazepines in individuals with any history of substance abuse or dependence. Such patients were felt, to be at increased risk for developing dependence on benzodiazepines. In addition, benzodiazepines were felt to be capable of inducing a relapse of the original substance abuse problem. Some authors have pointed out that empirical evidence does not fully support, these generalizations,Citation69 and further study is needed.
Selective serotonin reuptake inhibitors
Beginning with the introduction of fluoxetine and fluvoxamine in the 1980s for depression, this class of medications now includes some of the most, widely and frequently prescribed drugs in the world. They have proven to be efficacious and safe.Citation29-Citation32,Citation70 Agents also include sertraline, citalopram, paroxetine, and the mixed serotonin and norepinephrine reuptake inhibitor venlafaxine. They have been generally referred to as the SSRIs. These drugs are now used in both pediatric and adult populations across a wide and growing range of indications, which include a number of anxiety disorders. The SSRIs are listed by some as their preferred first-line treatment for many anxiety disorders. These drugs have not to date been reported to have a propensity to cause dependence or abuse, though a “discontinuation syndrome” has been described.Citation71-Citation76 A panel of recognized authorities on the pharmacotherapy of anxiety and depression was near unanimous in its rating of members of the SSRI class of drugs as offering less relative risk of dependence when compared with the benzodiazepines.Citation77 One major drawback to their use, however, has been the lag between treatment initiation and the onset, of antianxiety activity. Hence, they are not, useful for treatment, of acute anxiety. Because their use is not accompanied by the worry of dependence, they may allow more clinicians to confidently begin pharmacological treatment for patients who suffer from chronic anxiety disorders. Some clinicians have described a treatment paradigm that utilizes concomitant benzodiazepine treatment during the time that it is anticipated to be required for SSRIs to exert an anxiolytic effect.
Tolerability of side effects has also been a concern with these medications.Citation32 Sexual dysfunction and weight gain are frequently problems for patients taking these drugs over the spectrum of indications. In addition, some patients experience initial insomnia, restlessness, and agitation. Precipitation of overt panic attacks have also been reported.Citation78,Citation79 For patients who take numerous medications, such as many elderly patients, some of the SSRIs can be difficult, to blend into a medication regimen because of their ability to cause clinically important drug interactions.Citation80 Although regarded as nonsedating and thus less likely to be a hazard for accidents and falls, it should be noted that the SSRIs have also been linked to increased falls in the elderly.Citation81-Citation84
The discontinuation syndrome that has been noted by many authorsCitation71-Citation76 and investigators includes both physical and psychological symptoms, including lethargy, headache, and dizziness. The course is usually mild, with spontaneous resolution within a month. The cause may be transient serotonin dysregulation following abrupt withdrawal of an SSRI. As with the benzodiazepines, differences between SSRIs are seen with regard to their propensity to cause this syndrome following cessation. Drugs with slower clearance and pharmacologically active metabolites, such as fluoxetine, are reported to be less likely to cause this condition when stopped as compared with a drug such as paroxetine, which is not, known to have active metabolites.Citation76 Norfluoxetine, the active metabolite of fluoxetine, is detectable for weeks following cessation of chronic fluoxetine therapy. Tapering medication prior to stopping is suggested to minimize the discontinuation syndrome.
Conclusion
Anxiety is an important cause of disability in the community and has been underrecognized and undertreated. Treatment should aim for a remission of all major and debilitating symptoms. Therapy with the benzodiazepines has always been complicated by the worry of medication dependence, though only a minority of those on treatment appear to develop significant difficulties with dependence or the overlapping syndromes of abuse and addiction. Careful tapering of medication prior to stopping appears to ease withdrawal or other difficulty experienced in discontinuing therapy, especially when this is combined with psychological support. Additionally, the phenomena of a physiological rebound and/or a return of underlying psychopathology affect, patients treated with medications for other conditions, without causing the trepidation and stigma that, are attached to benzodiazepine use for treatment of anxiety. More study is needed to identify the patient factors that might, be predictive of difficulty with this class of drugs.
Newer medications offer the possibility of a wider spectrum of efficacy without the same concerns of dependence. It is hoped that the SSRIs will allow many more clinicians to confidently treat patients with anxiety disorders, without the fear of having to use drugs regarded as having abuse potential. Expense or side effects, however, could preclude some patients from being able to use these medications. Because the suffering with these disorders is substantial, anxiety disorders should not go untreated. Clinicians arc urged to consider the issue of the possibility of dependence in the context of overall medical safety and efficacy.
Supported by Grants MH-58435, DA-05258, DA-13209, DA-13834, DK58496, AG-17880, AT-01381, and RR-00054 from the Department of Health and Human Services.
REFERENCES
- American Psychiatrie Association.Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition. Washington, DC: American Psychiatric Association;1994
- National Institute of Mental Health Anxiety Disorders Research at the National Institute of Mental Health, December 7, 2002 Available at: http://www.nimh. nih.gov/publicat/anxresfact.cfm. Accessed June 12, 2003.
- American Psychiatric Association.Diagnostic and Statistical Manual of Mental Disorders. 3rd ed. Washington, DC: American Psychiatric Association;1980
- World Health Organization.The ICD-10 Classification of Mental and Behavioral Disorders. Clinical descriptions and diagnostic guidelines. Geneva, Switzerland: World Health Organization;1992
- KesslerRC.WittchenHU.Patterns and correlates of generalized anxiety disorder in community samples.J Clin Psychiatry.200263(suppl 8)41012044107
- SheltonRC.BrownLL.Mechanisms of action in the treatment of anxiety.J Clin Psychia try.200162(suppl 12)1015
- NuttDJ.BallengerJC.SheehanD.WittchenHU.Generalized anxiety disorder: comorbidity, comparative biology and treatment.Int J Neuropsychopharmacol.2002531532512466031
- ShaderRl.GreenblattDJ.Drug therapy Benzodiazepines.N Engl J Med.1974291101110154153318
- ShaderRl.GreenblattDJ.Drug therapy Benzodiazepines.N Engl J Med.1974291123912434153568
- WittchenHU.KesslerRC.BeesdoK.KrauseP.HoflerM.HoyerJ.Generalized anxiety and depression in primary care: prevalence, recognition, and management.J Clin Psychiatry.200263(suppl 8)243412044105
- JacobiF.WittchenHU.HoltingC.et al.Estimating the prevalence of mental and somatic disorders in the community: aims and methods of the German National Health Interview and Examination Survey,.Int J Methods Psychiatr Res.20021111812459800
- RiceDP.MillerLS.Health economics and cost implications of anxiety and other mental disorders in the United States.Br J Psychiatry Suppl.1998499829010
- HouseA.StarkD.Anxiety in medical patients.BMJ.200232520720912142312
- WittchenHU.KrauseP.HoyerJ.et al.Prevalence and correlates of generalized anxiety disorders in primary care [in German].Fortschr Med Orig.2001119(suppl 1)172511935664
- CulpepperL.Generalized anxiety disorder in primary care: emerging issues in management and treatment.J Clin Psychiatry.200263(suppl 8)354212044106
- HollisterLE.Müller-OerlinghausenB.RickelsK.ShaderRl.Clinical uses of benzodiazepines.J Clin Psychopharrnacol.199313(suppl 1)1S169S
- ShaderRl.GreenblattDJ.Use of benzodiazepines in anxiety disorders.N Engl J Med.1993328139814058292115
- GreenblattDJ.ShaderRl.AbernethyDR.Drug therapy. Current status of benzodiazepines.N Engl J Med.19833093543586135156
- GreenblattDJ.ShaderRl.AbernethyDR.Drug therapy. Current status of benzodiazepines.N Engl J Med.19833094104166135990
- MöllerHJ.Effectiveness and safety of benzodiazepines.J Clin Psychopharrnacol.199919(suppl 2)2S11S
- UhlenhuthEH.BaiterMB.BanTA.YangK.International study of expert judgment on therapeutic use of benzodiazepines and other psychotherapeutic medications. V. Treatment strategies in panic disorder, 1992-1997.J Clin Psychopharrnacol.199818(suppl 2)27S31S
- LaderMH.Limitations on the use of benzodiazepines in anxiety and insomnia: are they justified?.Eur Neuropsychopharmacol.1999(suppl 6)S399S40510622686
- WoodsJH.KatzJL.WingerG.Abuse liability of benzodiazepines.Pharmacol Rev.1987392514132893392
- WoodsJH.KatzJL.WingerG.Use and abuse of benzodiazepines. Issues relevant to prescribing.JAMA.1988260347634803062199
- WoodsJH.KatzJL.WingerG.Benzodiazepines: use, abuse, and consequences.Pharmacol Rev.1992441513471356276
- WoodsJH.Problems and opportunities in regulation of benzodiazepines.J Clin Pharmacol.1998387737829753204
- ShaderRl.GreenblattDJ.BaiterMB.Appropriate use and regulatory control of benzodiazepines.J Clin Pharmacol.1991317817841687147
- NinanPT.New insights into the diagnosis and pharmacologic management of generalized anxiety disorder.Psychopharrnacol Bull.200236105122
- GormanJM.Treatment of generalized anxiety disorder.J Clin Psychiatry.200263(suppl8)172312044104
- KapczinskiF.SchmittR.LimaMS.The use of antidepressants for generalized anxiety disorder.The Cochrane Library. 2002 (Issue 2). Oxford, UK: Update Software.
- KasperS.ResingerE.Panic disorder: the place of benzodiazepines and selective serotonin reuptake inhibitors.Eur Neuropsychopharmacol.20011130732111532386
- MasandPS.GuptaS.Selective serotonin-reuptake inhibitors: an update.Harv Rev Psychiatry.19997698410471245
- MahmoodI.SahajwallaC.Clinical pharmacokinetics and pharmacodynamics of buspirone, an anxiolytic drug.Clin Pharmacokinet.19993627728710320950
- FultonB.BrogdenRN.Buspirone: an updated version of its clinical pharmacology and therapeutic applications.CNS Drugs.199776888
- PittlerMH.ErnstE.Kava extract for treating anxiety.Cochrane Database Syst Rev. 2003:CD003383.
- BiliaAR.GallonS.VincieriFF.Kava-kava and anxiety: growing knowledge about the efficacy and safety.Life Sci.2002702581259712269386
- SinghYN.SinghNN.Therapeutic potential of kava in the treatment of anxiety disorders.CNS Drugs.20021673174312383029
- IzzoAA.ErnstE.Interactions between herbal medicines and prescribed drugs: a systematic review.Drugs.2001612163217511772128
- ErnstE.Harmless herbs? A review of the recent literature.Am J Med.19981041701789528737
- Hepatic toxicity possibly associated with kava-containing products - United States, Germany and Switzerland.MMWR Mo it Mortal VVklyRep.20025110651067
- BallengerJC.Treatment of anxiety disorders to remission.J Clin Psychiatry.200162(suppl 12)5911430617
- GreenblattDJ.ShaderRl.Benzodiazepines in Clinical Practice. New York, NY: Raven Press;.1974
- BatesonAN.Basic pharmacologic mechanisms involved in benzodiazepine tolerance and withdrawal.Current Pharm Design.20028521
- MillerLG.Chronic benzodiazepine administration: from the patient to the gene.J Clin Pharmacol.1991314924951652596
- MillerLG.GreenblattDJ.BarnhillJG.ShaderRl.Chronic benzodiazepine administration. I. Tolerance is associated with benzodiazepine receptor downregulation and decreased y-aminobutyric acidA receptor function.J Pharmacol Exp Ther.19882461701762839660
- MillerLG.GreenblattDJ.RoyRB.SummerWR.ShaderRl.Chronic benzodiazepine administration. II. Discontinuation syndrome is associated with upregulation of y-aminobutyric acidA receptor complex binding and function.J Pharmacol Exp Ther.19882461771822455789
- GreenblattDJ.MillerLG.ShaderRl.Benzodiazepine discontinuation syndromes.J Psychiatr Res.199024(suppl 2)73791980702
- GreenblattDJ.ShaderRl.Pharmacokinetics of antianxiety agents In: Meltzer HY, ed.Psychopharmacology: The Third Generation of Progress. New York, NY: Raven Press;198713771386
- RickelsK.FoxIL.GreenblattDJ.SandlerKR.SchlessA.Clorazepate and lorazepam: clinical improvement and rebound anxiety.Am J Psychiatry.19881453123172894175
- RickelsK.SchweizerE.CaseWG.GreenblattDJ.Long-term therapeutic use of benzodiazepines I. Effects of abrupt discontinuation.Arch Gen Psychiatry.1990478999072222129
- SchweizerE.RickelsK.CaseWG.GreenblattDJ.Long-term therapeutic use of benzodiazepines. II. Effects of gradual taper.Arch Gen Psychiatry.1990479089162222130
- GreenblattDJ.SethyVH.Benzodiazepine concentrations in brain directly reflect receptor occupancy: Studies of diazepam, lorazepam, and oxazepam.Psychopharmacology.19901023733781979181
- GreenblattDJ.EhrenbergBL.GundermanJ.et al.Pharmacokinetic and electroencephalographic study of intravenous diazepam, midazolam, and placebo.Clin Pharmacol Ther.1989453563652702793
- RickelsK.DeMartinisN.RynnM.MandosL.Pharmacologic strategies for discontinuing benzodiazepine treatment.J Clin Psychopharrnacol.199919(6 suppl 2)12S16S
- SpiegelDA.Psychological strategies for discontinuing benzodiazepine treatment.J Clin Psychopharrnacol.199919(6suppl2)17S22S
- RickelsK.DeMartinisN.Garcia-EspanaF.GreenblattDJ.MandosLA.RynnM.Imipramine and buspirone in treatment of patients with generalized anxiety disorder who are discontinuing long-term benzodiazepine therapy.Am J Psychiatry.20001571973197911097963
- WestraHA.StewartSH.As-needed use of benzodiazepines in managing clinical anxiety: incidence and implications.Curr Pharm Design.200285974
- PetrovicM.VandierendonckA.MarimanA.van MaeleG.AfschriftM.PevernagieD.Personality traits and socio-epidemiological status of hospitalised elderly benzodiazepine users.Int J Geriatr Psychiatry.20021773373812211123
- FarrellM.HowesS.TaylorC.et al.Substance misuse and psychiatric comorbidity: an overview of the OPCS National Psychiatric Morbidity Survey.Addict Behav.1998239099189801725
- KandelDB.HuangFY.DaviesM.Comorbidity between patterns of substance use dependence and psychiatric syndromes.Drug Alcohol Depend.20016423324111543993
- ConwayKP.SwendsenJD.RounsavilleBJ.MerikangasKR.Personality, drug of choice, and comorbid psychopathology among substance abusers.Drug Alcohol Depend.20026522523411841894
- BurnsL.TeessonM.Alcohol use disorders comorbid with anxiety, depression and drug use disorders. Findings from the Australian National Survey of Mental Health and Well-being.Drug Alcohol Depend.20026829930712393224
- SchneiderU.AltmannA.BaumannM.et al.Comorbid anxiety and affective disorder in alcohol-dependent patients seeking treatment: the first multicenter study in Germany.Alcohol Alcohol.20013621922311373258
- KanCC.BretelerMH.van der VenAH.et al.Assessment of benzodiazepine dependence in alcohol and drug dependent outpatients: a research report.Subst Use Misuse.2001361085109611504154
- RossJ.DarkeS.The nature of benzodiazepine dependence among heroin users in Sydney, Australia.Addiction.2000951785179311177494
- BeconaE.VazquezFL.MiguezMC.Smoking cessation and anxiety in a clinical sample.Personality individual Differences.200232489494
- SchuckitMA.HesselbrockV.Alcohol dependence and anxiety disorders: what is the relationship?.Am J Psychiatry.19941511723347977877
- KushnerMG.Relationship between alcohol problems and anxiety disorders.Am J Psychiatry.19961531391408540583
- PosternakMA.MuellerTl.Assessing the risks and benefits of benzodiazepines for anxiety disorders in patients with a history of substance abuse or dependence.Am J Addict.200110486811268828
- BarbeyJT.RooseSP.SSRI safety in overdose.J Clin Psychiatry.199859(suppl 15)42489786310
- HaddadPM.Antidepressant discontinuation syndromes.Drug Safety.20012418319711347722
- HaddadP.The SSRI discontinuation syndrome.J Psychopharrnacol.199812305313
- SchatzberAF.HaddadP.KaplanEM.et al.Serotonin reuptake inhibitor discontinuation syndrome: a hypothetical definition. Discontinuation Consensus Panel.J Clin Psychiatry.199758(suppl 7)510
- MarkowitzJS.DeVaneCL.ListonHL.MontgomerySA.An assessment of selective serotonin reuptake inhibitor discontinuation symptoms with citalopram.Int Clin Psychopharrnacol.200015329333
- TamamL.OzpoyrazN.Selective serotonin reuptake inhibitor discontinuation syndrome: a review.Adv Ther.200219172612008858
- JudgeR.ParryMG.QuailD.JacobsonJG.Discontinuation symptoms: comparison of brief interruption in fluoxetine and paroxetine treatment.Int Clin Psychopharrnacol.200217217225
- UhlenhuthEH.BaiterMB.BanTA.YangK.International study of expert judgment on therapeutic use of benzodiazepines and other psychotherapeutic medications. IV. Therapeutic dose dependence and abuse liability of benzodiazepines in the long-term treatment of anxiety disorders.J Clin Psychopharrnacol.199919(6 suppl 2) 23S29S
- BrauerHR.NowickiPW.CatalaneG.CatalaneMC.Panic attacks associated with citalopram.South Medj.20029510881089
- CatalanoG.HakalaSM.CatalaneMC.Sertraline-induced panic attacks.Clin Neuropharmacol.20002316416810895401
- GreenblattDJ.von MoltkeLL.HarmatzJS.ShaderRl.Human cytochromes and some newer antidepressants: kinetics, metabolism, and drug interactions.J Clin Psychopharrnacol.199919(5 suppl 1)23S35S
- LiuB.AndersonG.MittmannN.et al.Use of selective serotonin-reuptake inhibitors of tricyclic antidepressants and risk of hip fractures in elderly people,.Lancet.1998351130313079643791
- ThapaPB.GideonP.CostTW.et al.Antidepressants and the risk of falls among nursing home residents.N Engl J Med.19983398758829744971
- ArfkenCL.WilsonJG.AronsonSM.Retrospective review of selective serotonin reuptake inhibitors and falling in older nursing home residents.Int Psychogeriatr.200113859111352338
- SleeperR.BondCA.Rojas-FernandezC.Psychotropic drugs and falls: new evidence pertaining to serotonin reuptake inhibitors.Pharmacotherapy.20002030831710730686