Abstract
Epidemiological studies show that anxiety disorders are highly prevalent and an important cause of functional impairment; they constitute the most frequent menial disorders in the community. Phobias are the most common with the highest rates for simple phobia and agoraphobia. Panic disorder (PD) and obsessive-compulsive disorder (OCD) are less frequent (2% lifetime prevalence), and there are discordant results for social phobia (SP) (2%-16%) and generalized anxiety disorder (GAD) (3%-30%). These studies underline the importance of an accurate definition of disorders using unambiguous diagnostic and assessment criteria. The boundaries between anxiety disorders are often ill defined and cases may vary widely according to the definition applied. Simple phobia, agoraphobia, and GAD are more common in vmrnen, while there is no gender différence for SP, PD, and OCD, Anxiety disorders are more common in separated, divorced, and widowed subjects; their prevalence is highest in subjects aged 25 to 44 years and lowest in subjects aged >65 years. The age of onset of the different types of anxiety disorders varies widely: phobic disorders begin early in life, whereas PD occurs in young adulthood. Clinical - rather than epidemiological - studies have examined risk factors such as life events, childhood experiences, and familial factors. Anxiety disorders have a chronic and persistent course, and are frequently comorbid with other anxiety disorders, depressive disorders, and substance abuse. Anxiety disorders most frequently precede depressive disorders or substance abuse, Comorbid diagnoses may influence risk factors like functional impairment and quality of life. It remains unclear whether certain anxiety disorders (eg, PD) are risk factors for suicide. The comorbidity of anxiety disorders has important implications for assessment and treatment and the risk factors should be explored. The etiology, natural history, and outcome of these disorders need to be further addressed in epidemiological studies.
Los estudios epidemiológicos muestran que los trastornos de ansiedad presentan una elevada prevalencia y son una causa importante de alteraciones funcionales; de hecho constituyen el trastorno menial más frecuente en nuestra comunidad. Las fobias son el trastorno más comun, siendo la fobia simple y la agorafobia las que presentan las prevalencias más elevadas. El trastorno de pánico y el trastorno obsesivo-complusivo (OCD) son menos frecuentes (prevalencia a lo largo de la vida de 2%), existiendo datos discordantes en el caso de fobia social (2%-16%) y el trastorno de ansiedad generalizada (3%-30%). Estos estudios destacan la importancia de realizar una definición exacta de estos trastornos utilizando criterios de diagnóstico y de valoración claros que eviten ninguna ambigüedad, La frontera entre los trastornos de ansiedad está a menudo mal definida y en algunos casos puede variar ampliamente en función de la definición utilizada. La fobia simple, agorafobia y el trastorno de ansiedad generalizada son más frecuentes en la mujer, mientras que no se observan différencias significativas entre géneros en el caso de la fobia social, el trastorno de pánico y OCD. Los trastornos de ansiedad son más frecuentes entre las personas separadas, divorciadas y viudas; su prevalencia es superior entre los 25 y 44 años e inferior entre los mayores de 65 aóos. La edad de inicio de los disiinios tipos de trastornos de ansiedad varia ampliamente: las fobias comienzan en una edad muy temprana, mientras que los trastornos de pânico comienzan en la adolescencia y juventud. Los estudios clinicos - más que los epidemiológicos - ban examinado los factures de riesgo, como los acontecimientos de la vida, experiencias de la infancia y factores familiares. Los trastornos de ansiedad presentan un desarrollo crónico y continuo y aparecen frecueniemente de forma concomitante con otros trastornos de ansiedad, trastornos depresivos y problemas de toxicomanias. Los trastornos de ansiedad preceden frecueniemente a los trastornos depresivos o problemas de toxicomanias. El diagnóstico de estas comorbilidades pueden influenciar ciertos factores de riesgo como incapacidad funcional o la calidad de vida. Queda por aclarar si algunos trastornos de ansiedad (por ejemplo el trastorno de pánico) son factores de riesgo de suicidio. La comorbilidad de los trastornos de ansiedad presenta importantes implicaciones en el momenta de la exploración y el tratamiento debiendose además examinar los factores de riesgo, La etilogía, el desarrollo natural de la enfermedad y la evolución de estos trastornos requieren una mayor exploración en los estudios epidemiológicos.
Les études épidémiologiques montrent que les troubles anxieux ont une forte prévalence et sont une cause importante de handicap fonctionnel ; ils représentent les troubles mentaux les plus fréquents de la collectivité. Les phobies sont les plus courantes avec les taux les plus élevés pour la phobie simple et l'agoraphobie. Les troubles paniques (TP) et les troubles obsessionnels compulsifs (TOC) sont moins fréquents (2 % de prévalence sur la vie) tandis que les résultats pour la phobie sociale (PS) (2%-16 %) et l'anxiété généralisée (AG) (3 %-30 %) sont discordants. Ces études soulignent l'importance d'une définition exacte des troubles en utilisant des critères diagnostiques et d'évaluation sans ambiguïté. Les limites entre les troubles anxieux sont souvent mal définies et les cas peuvent considérablement différer selon la définition retenue. La phobie simple, l'agoraphobie et TAG sont plus courantes chez les femmes, alors qu'il n'y a pas de différence selon le sexe pour la PS, les TP et les TOC Les troubles anxieux sont plus habituels chez les sujets séparés, divorcés et veufs ; leur prévalence est la plus élevée chez les sujets âgés de 25 à 44 ans et la plus faible chez les sujets âgés de plus de 65 ans. L'âge de début des différents types de troubles anxieux varie largement ; les phobies apparaissent précocement, alors que le TP apparaît chez l'adulte jeune. Des études cliniques - plus qu'êpidêmiologiques - ont analysé les facteurs de risque, tels que les événements de la vie, les expériences de l'enfance et les facteurs familiaux. Les troubles anxieux ont une évolution chronique et durable et présentent souvent une comorbidité avec d'autres troubles anxieux, des troubles dépressifs et l'abus d'une substance. Le plus souvent, les troubles anxieux précèdent les troubles dépressifs ou l'abus d'une substance. Les diagnostics de comorbidité peuvent influer sur les facteurs de risque comme le handicap fonctionnel et la qualité de vie. Le doute persiste sur la responsabilité de certains troubles anxieux (p. ex, le TP) comme facteurs de risque de suicide, La comorbidité des troubles anxieux a d'importantes implications pour l'évaluation et le traitement et les facteurs de risque devraient être explorés. Les études épidémiologiques devront davantage aborder l'étiologie, l'histoire naturelle et l'évolution de ces troubles.
Anxiety is a common psychiatrie disorder.Citation1 It is usually associated with fear, nervousness, apprehension, and panic, but may also involve the cardiovascular, respiratory, gastrointestinal, or nervous systems, individually or in combination.Citation2
Anxiety has been recognized as a symptom for centuries. However, it was only recently, with the incorporation of Klein'sCitation3 conceptualization of panic disorder (PD) as a separate entity into Diagnostic and Statistical Manual of Mental Disorders, Third Edition Citation4 and Revised Third Edition Citation5 (DSM-III and DSM-FII-R) that anxiety states began to be subdivided into distinct entities such as PD with and without agoraphobia, social phobia (SP), posttraumatic stress disorder (PTSD), obsessive-compulsive disorder (OCD), and generalized anxiety disorder (GAD). The epidemiological approach to the study of anxiety disorders is associated with certain strengths and weaknesses. Epidemiological studies arc very informative because they gather data from large numbers of subjects, use powerful statistical techniques, and survey community samples of people who are not in treatment. The study of large numbers of subjects allows for comparisons across relevant groups based on differences in gender, race, education, occupation, ethnicity, and other factors. Large numbers also provide the statistical power to use sophisticated analytical strategies, such as multivariate regression analysis, which can dissect the effects of complex sociodemographic variables. Community surveys can sample nonclinical populations, leading to the investigation of many variables without the confounding factor of treatment seeking, which is strongly influenced by gender, education, and other sociodemographic and cultural factors.
Epidemiological studies have limitations in their capacity to answer certain questions about anxiety disorders. Complex sociodemographic variables, such as gender, race, education, ethnicity, language, and religion, are measured in epidemiological surveys in an attempt to identify some of the factors that may influence psychiatric symptom formation.
The ever-increasing attention paid to anxiety disorders is rooted in evidence that anxiety disorders are forms of mental disorders that obviously start early in life, and negatively affect school and work performance, as well as later psychosocial functioning, much more than previously thought. Furthermore, the traditional belief that most anxieties are short in duration and remit spontaneously has not been confirmed. On the contrary, the few prospective studies on course and outcome suggest that anxiety disorders belong to the most chronic forms of mental disorders. More recent epidemiological studies try to identify the mechanism involved in the persistence and chronicity of these disorders, as well as to quantify the degree of associated suffering and impairments. Another important trend in epidemiological research is that the critical role of anxiety disorders in primary care is now being acknowledged. Thus, attempts have been made to specify in detail how frequently anxiety disorders are seen and treated by general practitioners and other nonpsychiatric specialists in medicine, as well as their implications and consequences.
However, our ability to successfully capture these concepts in fairly simple variables across large community surveys is far from perfect. Further, the diagnostic constructs used in epidemiological surveys may be well established in industrially developed, Western societies, but their reliability and validity has not been adequately tested in other cultures.
Since the 1980s, with the introduction of the new DSM-III neurobiological and cognitive model, we have found that, although the traditional neurotic syndrome may be helpful for psychodynamic treatment, this is no longer the case for behavioral, neurobiological, and pharmacological interventions.
Thus, the traditional division between International Classification of Diseases, Ninth Revision Citation6 (ICD-9) anxiety neurosis and phobia should no longer be used. What used to be anxiety neurosis now includes PD, GAD, and possibly certain forms of mixed anxiety and depressive disorders. Phobia is now divided into SP, specific isolated phobia, and agoraphobia. Some reactionary disorders to severe stress, like PTSD, should be classified along with anxiety disorders because the biological and behavioral mechanisms are very similar.
Aside from the fact that new basic and clinical knowledge no longer matches the traditional grouping of anxiety disorders within neurotic disorders, there are also several practical advantages that make the new diagnostic approaches superior. They are easy to use because the diagnosis is now based on clearly specified descriptive and reliable diagnostic criteria. Because of this specificity, we have been able to translate the criteria for each form of anxiety disorder into simple-to-use diagnostic questions as part of direct diagnostic instruments like the World Health Organization (WHO) composite international diagnostic interview (CIDI).Citation6 The CIDI has very high reliability and validity, and can be used even by nonspccialists without time-consuming diagnosis. Another advantage is that this new nosography has brought psychiatry closer to medical science in general. Mental disorders are no longer vaguely defined expressions of craziness, but are specific, well-defined disorders. This leads to a better acceptance by patients and their families. Having a PD is no longer a psychological defect, a personal weakness, or the result of a neurotic development.
This very important point has been confirmed by Wittchen et alCitation7 in the Munich Study: anxiety disorders almost never improve spontaneously. In the past, these disorders were called “minor” and thus they were rarely specifically treated, unless severe complications occurred. We have shown that 80% of the people presenting with such so-called minor disorders did not receive any treatment, with the consequence that they still present the disorder 14 years later, with severe implications for everyday life. Even those few receiving treatment did not recover completely. It is thus essential to help patients and their families accept the illness and live with residual symptoms.
Epidemiology of anxiety disorders: general studies
A number of epidemiological studies have shown that anxiety disorders are highly prevalent and important causes of functional impairment. Several previous studies conducted in the USA, UK, and Germany have highlighted these problems.
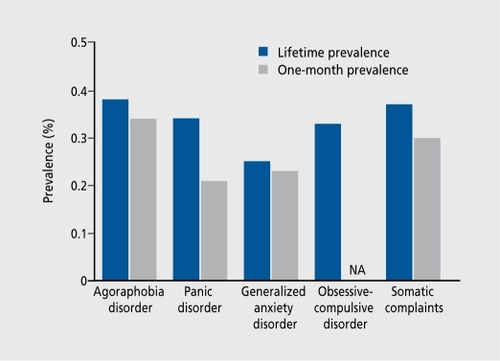
The Epidemiological Catchment Area (ECA) surveyCitation8 is the largest and most famous psychiatric epidemiological study carried out in a general population of five American states (Connecticut, Maryland, Missouri, North Carolina, and California). Here, we will refine ourselves to discussing the ECA results on neurotic and anxiety disorders. The other anxiety disorders were evaluated in only some of the study areas. The prevalence of PTSD was 1% in Saint Louis (0.5% in men, 1.3% in women; 3.5% in crime victims, 20% in Vietnam veterans). GAD has a 12-month prevalence of 2.3% in Durham, NC (0.8% in men and 2.6% in women) and is not comorbid with another psychiatric disorder in two cases out of three. As in most other investigations, the ECA study stresses the high rate of comorbidity of neurotic and anxiety disorders, whether they are associated with other anxiety disorders or other psychiatric disorders. The 1-month prevalence data for anxiety disorders are presented in Table I.
Table I. One-month prevalence data for anxiety disorders as evaluated by the Epidemiological Catchment Area (ECA) study.Citation7 PD, panic disorder; OCD, obsessive-compulsive disorder.
Another important epidemiological survey, the National Comorbidity Survey (NCS), was the first study to be carried out in a representative sample of the North American population; in contrast, the ECA survey only covered five states. The NCS employed a scmistructured interview approach, enabling investigators to obtain a diagnosis according to DSM-III-R criteria.Citation5 The subjects included in the study were aged 15 to 54 years and not receiving inpatient psychiatric treatment. They were interviewed by nonmedical interviewers, using a revised version of CIDI. This revised edition of CIDI was designed to enable diagnosis according to DSM-III-R criteria, as well as Diagnostic and Statistical Manual of Mental Health Disorders, Fourth Edition Citation9 (DSM-IV) and the International Statistical Classification of Diseases, Tenth Revision Citation10 (ICD-10) criteria. Its aim, which was complementary to that of the EGA study, was not only to evaluate prevalence of psychiatric disorders in the general population, but also to identify certain risk factors and evaluate psychiatric care needs in inhabitants throughout the USA.
Approximately half of the subjects who took part suffered from, or had suffered from, at least one psychiatric event (lifetime prevalence). At the time of the study, a third of the subjects presented an event or had presented an event in the previous 12 months (12-month prevalence). The most common diagnoses were major depressive events, alcohol dependence, SP, or simple phobia. More than half of the diagnosed lifetime events were found in only 14% of the population. This group of patients had past medical history featuring at least in three comorbid pathologies, and it is among this group that the most severe disorders were found. Furthermore, 40% of the subjects who had presented a psychiatric event in their lifetime had previously received treatment, while only 20% of those who had an event during the previous 6 months had been treated.Citation11
The main feature of the NCS is that prevalence rates for mental disorders in the general population were much higher that those generally found in most previous studies, notably ECA study (Table II), in spite of the fact that the ECA methodology was very similar:
Table II. Lifetime prevalence of psychiatric disorders in the Epidemiological Catchment Area (ECA) survey and the National Comorbidity Survey (NCS).Citation11 GAD, generalized anxiety disorder; PD, panic disorder; OCD, obsessive-compulsive disorder; SP, social phobia.
Use of a semi-structured interview and similar diagnostic criteria (revised CIDI and DSM-III-R in the NCS; and diagnostic interview schedule [DIS] and DSM-III in the ECA).
Performed in the general population in North America (nationwide sample of 8000 subjects aged 15 to 54 years in the NCS; and 20 000 subjects ≥18 years from five states in the ECA).
Lifetime and 12-month prevalence in both studies.
Noninstitutionalized general population in the NCS and general population weighted by institutionalized subjects in the ECA.
Adjusted to correct for nonresponder biases in the NCS study.
The modest methodological differences between the two studies would not even have tended to bias results in any way. The younger NCS study population should have increased the yearly prevalence of depression, anxietylinked disorders, and substance abuse (which are more common between ages 20 and 50 than after 65 years) and increased the lifetime prevalence of all types of disorders. However, the equivalent prevalence rates for mental disorders were only 32% (at least one diagnosis over a lifetime period) and 20% (at least one diagnosis over a 12-month period) in the ECA study.
Analysis of the lifetime prevalence rates for each clinical entity (in decreasing order) provides an explanation. The difference mainly lies in depressive disorders and addictions, whose prevalence could arguably have increased. The difference in data between the ECA and NCS studies concerning phobic disorders is comparable to that observed in data originating between different ECA study centers, and is probably attributable to semiological data recording methods. Finally, the prevalence of schizophrenia is lower, which could be partly due to a lower prevalence of schizophrenia and partly due to the fact that institutionalized patients were excluded from the NCS study. On the other hand, Angst and WickiCitation12 conducted a study in Zurich to identify recurrent brief anxiety (RBA) syndromes. The concept of brief and transient psychiatric pathologies has long been known, but has received an increasing amount of attention in the past few years. The terms recurrent brief depression (RED), RBA, recurrent brief hypomania, neurasthenia, and insomnia have all been coined recently. All these syndromes last 1 to 3 days on average, and are highly recurrent (at least once a month over a whole year). The authors who developed these concepts have defined them by means of the following diagnostic criteriaCitation12:
Anxiety (fear of being alone, apprehension of impending doom, fear of the next day dawning).
Three of the four GAD symptoms as described in DSM-III (motor tension, neurovegetative hyperactivity, apprehension, exacerbated awareness while exploring surroundings).
Anxious mood for 1 to 13 days, at least once a month during the previous year.
Subjective professional impairment of handicap.
The authorsCitation12 noticed that RBA morbidity was often associated with PDs and RED, and that many RBA patients had past familial and personal history of anxiety and depression. Angst and Wicki therefore suggested that the association of RBA and RBD could reflect a shared genetic predisposition for depression and anxiety.Citation12
The comorbidity rate of RBA with other diagnoses is such (>75% with depression, >25% with phobias, >16% with PD, and >6% with GAD) that one can understandably challenge the authenticity of this clinical entity. Furthermore, the symptomatic definition of RBA does not identify any distinctive characteristic from those of GAD, aside from duration.
These concepts can be questioned in the same way that one can challenge the existence of subsyndromic states. These states are related to entities defined by classical criteria systems (DSM-III, DSM-IV, or ICD-10), but differ only because they consist of n-1 or n-2 symptoms. In the case of brief recurrent syndromes, the duration of psychological suffering is significantly shortened. There are still few studies in France concerning the prevalence of anxiety and somatoform disorders among outpatients. Lepine et alCitation13 examined a general psychiatric outpatients sample (n=1271), gathered through a crossnational French survey. Anxiety and somatoform syndromes were assessed according to DSM-III and DSM-III-R criteria. Lifetime and 1 -month prevalence rates in this population were reported and a high level of comorbidity between anxiety syndromes was observed.
Another epidemiological survey was conducted by Lepine and LellouchCitation14 in the general population in an suburban development of the greater Paris area, and evaluated the prevalence of risk factor for anxiety and depressive disorders, based on the DSM-III-R criteria, using standardized interviews (DIS and CIDI).
Data were obtained for 1787 subjects randomly chosen from a telephone directory. One problem was the high rate of refusal to participate (35%). Furthermore, the study area greatly influenced the sociodemographic characteristics of the study population: young age (average: 36 years in women and 38 years in men), mostly married, working primarily in the tertiary sector, with 71% of the women aged 20 to 64 years being part of the active work force. The anxiety and depression disorder prevalence data found in this study are consistent with those found in the international literature (). They are, however, to be compared with the data found in the upper limit of this bracket. As was the case in the NCS, these data underline the high rate of comorbidity between anxiety and depressive disorders. Furthermore, in this study of French population, Lepine and LellouchCitation14 find the same cohort effect as that found in other Western countries: an increase in the prevalence of depression in cohorts of subjects born after the end of the Second World War.
The epidemiology of anxiety disorders: focused studies
Generalized anxiety disorder
Diagnosis
The DSM-III criteria for GAD require the presence of unrealistic or excessive anxiety and worry, accompanied by symptoms from three of the following categories: motor tension, autonomic hyperactivity, vigilance and scanning, and apprehensive expectation. The anxious mood must continue for at least a month, and the diagnosis is not made if phobia, PD, or OCD is present, or if the disturbance is due to another physical or mental disorder, such as hyperthyroidism, major depression, or schizophrenia. By this definition, GAD is treated primarily as a residual category after exclusion of the other major anxiety disorders. DSM-III-R narrowed the definition further by requiring a minimum of six symptoms and a duration of 6 months. DSM-IV required only three symptoms from a list of six, but added the requirement that the anxiety causes clinically significant distress or functional impairment.
Symptoms
Pervasive anxiety and worry persisting for at least 6 month (to a degree out of proportion to actual likelihood of effect of the event), motor tension, hyperarousal; many patients may report being anxious all their lives.
Significant impairment of daily life: sleep problems, headaches, the “jitters,” nausea, tense muscles, and trembling or hot flashes are common; fatigue and difficulty concentrating may cause difficulties at work or home.
Prevalence
The literature reviewed here is consistent in showing that GAD is common mental disorder that typically has an early age of onset, a chronic course, and a high degree of comorbidity with other anxiety and mood disorders. Comorbidity GAD is often temporally primary, especially in relation to mood disorders, and is associated with an increased risk for the subsequent onset and severity of secondary disorders. The weight of evidence reviewed here argues against the view expressed by early commentators that GAD is better conceptualized as a prodrome, residual, or severity marker of other disorders than as an independent disorder. Focused studies of comorbidity between GAD and major depression, in which comorbidity is high, reached the same conclusion.Citation15 The crucial evidence for this conclusion includes the following:
Contrary the findings of clinical studies, GAD in the community docs not have a higher comorbidity than most other anxiety or mood disorders.
The symptoms of GAD form an empirical cluster distinct from the symptoms of major depression in studies of symptom profiles.
Family studies show distinct aggregation of GAD and major depression.
Twin studies show that the environmental determinants of GAD are different from those of major depression.
The sociodemographic predictors of GAD in epidemiological studies are different from those of major depression.Citation16
The clinical course of GAD is less consistently related to comorbidity than the course of other anxiety and mood disorders.Citation17
The impairments associated with GAD are equivalent to - or greater than - those associated with other severely impairing chronic physical and mental disorders.Citation18-Citation20
These findings show that the status of GAD as an independent disorder is at least as strongly supported by available evidence as other anxiety or mood disorders.Citation21 Despite the fact that there have been many changes in the diagnostic criteria for GAD over recent years, reported lifetime prevalence estimates in the general population (Table III) are remarkably stable, especially compared with the considerable variance observed with other psychiatric disorders, such as depression and PD, over a similar age span. On the basis of more recent studies, the most likely lifetime prevalence rate for GAD in the general population is 5% using DSM criteria and may be slightly higher when using the broader ICD-10 criteria (6.5%) (Table III).Citation13,Citation22-Citation27 Current and 12-month prevalence rates for GAD are reported in Tables IV Citation22,Citation25,Citation26,Citation28-Citation32 and V, Citation22,Citation25,Citation26,Citation27,Citation33-Citation37 although these estimates depend largely on the rigidity of the definition of current prevalence (for current prevalence [also known as point prevalence], the exposure and outcome are both determined at the same point or cross-section in time, using a cross-sectional study) and are subject to more variation than lifetime prevalence estimates. The most likely current prevalence rate in the general population seems to be in the range of 2% to 3% (DSM criteria). The NCS,Citation11 which was performed in a representative sample of the US general population, is the largest study to report epidemiological findings for GAD to date.Citation26 Using CIDI/DSM-III-R criteria in more than 8000 respondents, a lifetime prevalence estimate of 5.1 % (3.6% in men and 6.61 % in women) and a 12-month prevalence rate of 3.1 % (2.0% in men and 4.3% in women) were reported. The lifetime prevalence estimate is in relatively good agreement with the findings of several other large epidemiological studies that have been conducted throughout the world in recent years. The 12-month prevalence rate found by the NCS should be regarded with caution, however, since the CIDI is designed to gather lifetime prevalence rates and did not assess the presence of all of the disorder's criteria in the preceding 12 months, and thus might include a high proportion of people with lifetime GAD who have only had some significant signs of the disorder during the previous month. The 12-month prevalence estimates of threshold GAD were recently found to be lower in the German National Health Interview and Examination Survey (GHS), Mental Health Supplement.Citation37 This study used the slightly stricter DSM-IV criteria (which use the additional criteria of difficulty controlling worry and a restricted range of associated symptoms), which increase the duration criterion from 1 to 6 months compared with DSM-III-R, to examine GAD and other disorders in a representative sample of the German population (over 7200 adults). Using a 12-month version of the Munich CIDI,Citation38 the 12-month prevalence rate for GAD (meeting all DSM-IV criteria) was found to be 1.5% (1.0% in men and 2.1% in women).
Table III. Lifetime prevalence of generalized anxiety disorder (GAD) in general population surveys. EC A, Epidemiological Catchment Area; NCS, National Comorbidity Survey; WHO, World Health Organization; DSM, Diagnostic and Statistical Manual of Mental Disorders.
Table IV. Current prevalence of generalized anxiety disorder (GAD) in general population surveys. ECA, Epidemiological Catchment Area; NCS, National Comorbidity Survey; WHO, World Health Organization; RDC, research diagnostic criteria; DSM, Diagnostic and Statistical Manual of Mental Disorders: ICD, International Classification of Diseases.
Table V. Twelve-month prevalence of generalized anxiety disorder (GAD) in general population surveys. ECA, Epidemiological Catchment Area; NCS, National Comorbidity Survey; GHS, German National Health Interview and Examination Survey; WHO, World Health Organization; DSM, Diagnostic and Statistical Manual of Mental Disorders; ICD, international Classification of Diseases.
When, however, lifetime GAD cases with still-existing, 12-month subthreshold GAD syndromes are counted as well - as was the case in the NCS study - an almost identical 12-month rate of 3.6% (2.4% in men and 4.9% in women) was confirmed. In addition, the disorder was found to be significantly more frequent in women than in men (odds ratio [OR] =21;P<0.05).The investigators also determined prevalence rates for subthreshold expressions of GAD by using different time criteria for duration, such as worrying for at least 1 month (7.8%) or worrying for at least 3 months (4.1%), and concluded that long periods of anxious worrying associated with subthreshold GAD symptoms are much more widespread in the community than threshold GAD.
When prevalence data from the NCS and GHS are examined by age, it is clear that for both lifetime and 12-month prevalence rates, the lowest rates for GAD occur in the younger age groups and the highest rates are found in the older study participants.Citation26,Citation37 In the GHS, the likelihood of receiving a diagnosis of GAD increased significantly with age (18-34 versus 35-65 years; OR=l .0; P<0.05) when controlling for differences in gender, with point prevalence rates up to 4.4% in women aged 45 or older. These findings arc consistent with the lower prevalence rates for GAD recorded in studies of adolescents and young adults. Despite differences in diagnostic criteria, the ECA,Citation22 the NCS,Citation26 and the Savigny studyCitation13 rates of GAD were quite similar. Lifetime prevalence varied considerably more in the Iceland and Hong Kong studiesCitation24 from 7.8% in Hong Kong (women) to 21.7% in Iceland.Citation25 The Florence studyCitation26 provides an interesting example of the effects of requiring the longer 6-month duration of DSM-III-R. For DSM-III, the lifetime prevalence rate was 5.4%, while the narrower DSM-III-R definition resulted in the lower rate of 3.9%. Another clinical and epidemiological study of GAD in general practiceCitation39 indicates that, among a sample of 1117 patients, 15.4% were given a GAD diagnosis (DSM-III); there were predominantly women and aged between 35 and 50 years. On the other hand, GAD (and PD) is unique among anxiety disorders in that patients commonly present to primary care physicians for treatment:Citation40
An international WHO study used ICD-10 criteria and the CIDI to assess GAD and estimated the current prevalence of GAD to be approximately 8% of all primary care attendees.Citation41 A more recent reanalysis confirmed these results by using more sophisticated analyses, finding a mean current prevalence rate of 7.9%. Citation40 This study also found a wide range of prevalence rates across the participating countries, for example, 3.8% in Italy and 14.8% in Greece, possibly owing to differences in the way that countries and regions organize the provision of primary care services. It is noteworthy that this study suggests that the point prevalence rate of GAD is considerably higher in primary care than that reported in the general population, suggesting that GAD patients are high utilizers of primary care resources.Citation42 This is in contrast to social anxiety disorder and most other anxiety disorders, for which the point prevalence rates in the general population are much higher than in primary care, and subjects are unlikely to present to their family doctor owing to the nature of the condition.Citation43,Citation44
Panic disorder
Diagnosis
The key feature of PD in DSM-III is the occurrence of three or more panic attacks within a 3-week period. These attacks must not have been precipitated simply by exposure to a feared situation, must not be due to a physical disorder, and must be accompanied by at least four of the following symptoms: dyspnea, palpitations, chest pain, smothering or choking, dizziness, feelings of unreality, paresthesias, hot and cold flashes, sweating, faintness, trembling, or shaking. In DSM-III-R, the definition was revised to require four attacks in 4 weeks, or one or more attacks followed by a persistent fear of having another attack, and the list of potential symptoms was revised to include nausea or abdominal distress and to exclude depersonalization or derealization.
More importantly, DSM-III-R changed the diagnostic hierarchy such that PD could be diagnosed as a primary disorder with or without agoraphobia, and also dropped the category of agoraphobia with panic attacks. This change emphasized identifying PD as a discrete entity, and reflected the clinical experience that panic attacks tended to occur prior to the development of agoraphobia, which was increasingly viewed as a phobic avoidance response to the frightening experience of spontaneous panic attacks, near panic experiences, or limited symptom attacks.Citation45
DSM-IV criteria require recurrent unexpected panic attacks and persistent concern about having further attacks, worry about the implications of the attacks, or a significant change in behavior due to the attacks. Epidemiological data using these criteria are not available.
Symptoms (with or without agoraphobia)
Unexpected, recurrent, abrupt episode of intense fear or discomfort (ie, panic attacks) that peak within 10 min and may involve multiple systems.
Feelings of unreality, detachment from self, and intense fear of losing control, choking, going crazy, having a heart attack, or dying during a panic attack.
Recurrent and unexpected panic attacks and, for at least 1 month after an episode, concerns about the consequences of a prior attack or having another attack (ie, PD).
Symptoms of agoraphobia may be present: fear of getting into situations or going to places where a panic attack may occur and there is no escape or availability of help.
Prevalence
Table VI Citation7,Citation8,Citation11,Citation14,Citation25,Citation46-Citation52 shows prevalence rates for PD from a cross-national collaborative study in 10 countries, using DIS and DSM-III criteria. These 10 community studies included over 40 000 subjects, who were analyzed with appropriate standardization for age and sex differences among subjects from different countries. For comparison purposes, Table VI also includes data from the NCS,Citation11 a representative sample of 8098 persons living in the 48 coterminous states in the USA and conducted between 1990 and 1992, using the University of Michigan version of the Composite International Diagnostic Interview (UM-CIDI) and DSM-III-R criteria. The annual rate of DSM-III PD ranged from 0.2% in Taiwan to 2.1% in Beirut, Lebanon. The NCS reported an annual prevalence of 2.2% for DSM-III-R PD.Citation53,Citation54
Table VI. Lifetime prevalence rates for panic disorder (PD) in several community studies (age 18 to 64 years). ECA, Epidemiologic Catchment Area survey; NCS, National Comorbidity Survey.
Lifetime prevalence rates of DSM-III PD showed excellent agreement, with the prevalence varying from 1.4% in Edmonton, Canada, to 2.9% in Florence, Italy. The exception to this narrow range was Taiwan, where DSM-III PD had a lifetime prevalence of 0.4%. The lower rates of PD in Taiwan are consistent with lower Taiwanese rates for most other disorders studied. The reasons for these lower rates are not clear. The only study that reported on lifetime DSM-III-R PD was the NCS, which found a rate of 3.5%, somewhat higher than the lifetime prevalence rates based on DSM-III. The higher annual and lifetime rates reported in the NCS may be caused by a period effect, with increasing rates between the ECA of the early 1980s and the NCS of the early 1990s. Other contributors to the higher rate in the NCS may include the broadening of the concept of PD in DSM-III-R compared with DSM-III and the differences in memory probes used in the NCS interview (the UM-CIDI) compared with the crossnational study (the DIS interview).Citation28
The age at onset of PD is usually in the early to middle twenties, with a later onset in West Germany (Munich)Citation7 and KoreaCitation50 (age 35.5 and 32.1, respectively). In the NCS data, a bimodal distribution of age of onset was reported, with an early mode for PD in the 15- to 24-year age range for both men and women, and a later mode in the 45- to 54-year age range.
Most of the evidence regarding clinical course comes from clinical studies, which suggest that PD has a fluctuating course with varying levels of severity over time. Two longitudinal epidemiological studies, the Munich Follow-up Study (MP'S)Citation7 and the Zurich study, showed that a substantial proportion of persons with PD go on to develop comorbid panic and depression and that these cases are associated with a less favorable course and outcome. Longitudinally, cases with both disorders have very high treatment rates and a high rate of suicide attempt.
At every cross-national site and in the NCS, PD was associated strongly with an increased risk for major depression and agoraphobia. The ORs for comorbidity of lifetime PD with agoraphobia ranged from OR=7.5 in the ECA to OR=21.4 in Puerto Rico, with the NCS reporting OR=10.6 (Table VI).Citation8,Citation11,Citation14,Citation46,Citation47,Citation49-Citation51 On the basis of lifetime prevalence rates, the OR for comorbidity of PD with major depression ranged from OR=3.8 in Savigny, France, to OR=20.1 in Edmonton, Canada, with OR=5.7 reported in the NCS (Table VII).
Table VII. Comorbidity of panic disorder (PD) with lifetime agoraphobia and major depression. ECA, Epidemiological Catchment Area survey; NCS, National Comorbidity Survey; OR, odds ratio; CI, confidence interval.
Finally, comparing lifetime prevalence rates, all of the studies reporting on PD showed higher rates for women than for men. In an analysis of the data, Eaton and colleaguesCitation45 found uniformly higher rates of panic attacks and PD for women over men within every age group. Of interest, Keyl and EatonCitation55 analyzed incidence rates from the ECA study and found a twofold increased risk of incident PD in women over men.Citation56 This finding is analogous to the increased incidence and prevalence rates for major depression in women versus men. It suggests that for both PD and major depression, the higher rates in women reflect a true increase in the risk for new-onset PD and major depression, rather than a greater tendency to seek treatment or have longer episodes of illness.
Agoraphobia
Diagnosis
DSM-III agoraphobia is defined as a fear and avoidance of being in places or situations from which escape might be difficult or in which help might not be available in the event of sudden incapacitation. As a result of such fears, the agoraphobic person avoids travel outside the home or requires a companion when away from home. Moderate cases may cause some constriction in lifestyle, while severe cases of agoraphobia may result in the person being completely housebound or unable to leave home unaccompanied.
As outlined in the PD section above, DSM-III-R revised the diagnosis of agoraphobia to a condition accompanying PD (PD with agoraphobia) or panic-like symptoms. Although the diagnosis of agoraphobia without history of PD was retained, this category emphasized avoidance behavior as a response to the sudden development of anxiety or somatic symptoms. DSM-IV has further emphasized that the agoraphobic avoidance behavior occurs specifically in response to the fear of developing panic-like symptoms.
Prevalence
Lifetime prevalence rates of agoraphobia have been reported in a number of studies. If one considers only the studies carried out in primarily English-speaking countries, the lifetime prevalence rates vary over a narrow range from 2.9% in Edmonton, Canada, to 6.7% in the NCS.Citation11 Despite the changes in the diagnostic definition between DSM-III and DSM-III-R, the lifetime rates from the ECA and NCS studies showed remarkable consistency (5.6% and 6%-7%, respectively). As with other disorders, Taiwan reported a lower rate of agoraphobia (1.3%).
On the other hand, as shown in Table VIII,Citation8,Citation11,Citation14,Citation46,Citation47,Citation49 -Citation51 the Cross-national Collaborative Study and the NCS identified PD as a uniformly powerful risk factor for agoraphobia across a wide array of study sites. Nonetheless, in DSM-III, agoraphobia was considered to be a separate phobic disorder that may or may not be accompanied by panic attacks. Largely due to the influence of Klein's hypothesis that agoraphobia is a conditioned avoidance response to the aversive stimulus of spontaneous panic attacks, the diagnostic view of agoraphobia changed considerably in DSM-III-R, in which PD is viewed as primary, with or without secondary development of agoraphobia. An important factor in this change was the observation by KleinCitation3 and others that, in clinical settings, agoraphobia rarely occurs without preceding spontaneous panic attacks or limited symptom attacks. However, Marks and other investigatorsCitation57 have questioned the temporal precedence and causal role of panic attacks in the development of agoraphobia.
Table VIII. Comorbidity of panic disorder (PD) with lifetime agoraphobia. ECA, Epidemiological Catchment Area survey; NCS, National Comorbidity Survey.
The large differences between clinic and community studies in estimates of the relative prevalence of agoraphobia with and without panic attacks contribute to the controversy. Population-based surveys have identified a substantial number of subjects with agoraphobia and no history of panic attacks. For the most part, subjects in these surveys were interviewed by laypersons using the DIS. In contrast, clinic-based studies, using less structured interviews administered by clinicians, almost invariably found much lower rates of agoraphobia without panic.
Several explanations for this discrepancy have been suggested. One is that treated samples of persons with any illness have higher rates of comorbidity than untreated samples. An alternative explanation is that population studies may have overestimated the rate of agoraphobia without PD.
In a reanalysis of the ECA data on agoraphobia without panic, 22 community cases of agoraphobia without panic were clinically reappraised and only a single case of probable agoraphobia without panic was found.Citation28 The diagnostic reappraisal found that 19 (87%) of the cases had simple or SPs rather than agoraphobia, or no DSM-III phobia at all. The reappraisal also identified 6 cases of PD, panic attacks, or limited symptom attacks that had been missed by the DIS interview. The authors concluded that community studies using the DIS may have overestimated the prevalence of agoraphobia without panic attacks in the community.
An initial analysis of the NCS data found that only about one-third of NCS agoraphobics reported a history of panic attack. More detailed analyses of the NCS data are under way to determine whether agoraphobia without panic is in fact as common as the initial analyses suggest.
Social phobia
Diagnosis
SP is a common disorder associated with significant psychosocial impairment, representing a substantial public health problem, largely determined by high prevalence and lifelong chronicity. SP starts in early childhood or adolescence, and is often comorbid with depression, other anxiety disorders, alcohol and substance abuse, or eating disorders.Citation58 This cascade of comorbidity, usually secondary to SP, increases the disability associated with the condition.
The central feature of DSM-III SP is a persistent, irrational fear accompanied by a compelling desire to avoid situations in which a person may act in a humiliating or embarrassing way while under the scrutiny of others. DSM-III-R allowed for the phobic situation to be avoided or endured with intense anxiety, and added the requirement that the avoidant behavior interferes with occupational or social functioning or that there is marked distress about having the fear. DSM-IV adds that the person recognizes the fear as excessive or unreasonable.Citation59
Common SPs involve fears of speaking or eating in public, urinating in public lavatories, writing in front of others, or saying foolish things in social situations.
Symptoms (social specific)
Unreasonable or excessive fear of social situations (eg, being embarrassed during a performance), specific objects (eg, cats, clowns, spiders), or situations (eg, being in tunnels or darkness).
Avoidance of feared situation or object, or endurance of it with intense anxiety.
Significant distress or social and occupational dysfunction.
Prevalence
Table IX Citation8,Citation11,Citation46,Citation47,Citation50 shows the lifetime prevalence of DSMIII SP from a cross-national study reporting from the US, Canada, Puerto Rico, and Korea; for comparison, the lifetime prevalence of DSM-III-R SP is also included. Lifetime prevalence rates of DSM-III SP varied somewhat, with a low of 0.5% in Korea and a high of 2.6% in the US. It is not clear whether these contrasting rates reflect true cross-cultural differences or differences in methodology or translation of the DIS.
Table IX. Lifetime prevalence rates for social phobia (SP) disorder in several community studies. ECA, Epidemiological Catchment Area survey; NCS, National Comorbidity Survey.
The lifetime prevalence of DSM-III-R SP from the NCS was considerably higher (13.3%) than in any of the DIS/DSM-III studies. Magee and colleaguesCitation60 attributed the higher prevalence to differences between the DIS and UM-CIDI. The UM-CIDI uses a stem question based on the broader DSM-III-R criteria allowing either avoidance of a feared situation or endurance with intense anxiety. It also asks about six specific SP fears (versus three in the DIS), including the high prevalence fears of using a public toilet, writing in front of others, or talking to people and sounding foolish or having nothing to say.
In the Cross-national Collaborative Study data reported in Table IX, the mean age at onset of first phobia ranged from the mid- teens to early twenties. The NCS reported a median age at onset for SP of 16 years. SP appears to be a chronic disorder, which can disrupt academic achievement, and impair social development and job performance.
The vast majority of SPs occurred in persons who reported at least one other psychiatric disorder. Both the NCS and the cross-national studies reported that persons with SP usually suffered a first onset of phobia prior to the onset of other psychiatric disorders.Citation61 The course of SP is often marked by development of other comorbid psychiatric disorders. As in other instances of comorbid disorders, these cases may be associated with greater degrees of functional impairment and treatment seekingCitation62 and suicide.Citation63
Obsessive-compulsive disorder
Diagnosis
DSM-III diagnostic criteria for OCD require the presence of obsessions or compulsions that arc sources of significant distress or impairment and are not due to another mental disorder/Citation4 DSM-III-R requires that the obsessions or compulsions cause marked distress, consume more than 1 hour a day, or significantly interfere with the person's normal routine or occupational or social functioning.Citation65 DSM-IV adds the requirement that the person has recognized that the obsessions or compulsions are excessive or unreasonable. Obsessions are defined as recurrent, persistent thoughts, images, or impulses that are experienced as intrusive and inappropriate. Compulsions are repetitive behaviors (eg, checking locked doors or gas jets, hand washing) or mental acts (eg, counting, repeating words) that the person feels driven to perform in response to an obsession or according to rigid rules.Citation66
Symptoms
Intrusive and recurrent thoughts, impulses and images that cause distress and impairment (obsessions); performance of ritualized behaviors (compulsions) to relieve anxiety obsessions or compulsions that interfere with daily life and usually take up at least 1 hour of the patient's day.
Realization that compulsive behaviors are senseless.
Common obsessions involve germs and disease (becoming sick or making others sick), of being harmed or harming others; cleanliness, neatness, symmetry, disturbing sexual images.
Common compulsions include repeated hand washing, tooth brushing, avoiding touching “contaminated” objects, counting, and checking.
Prevalence
Table X Citation7,Citation8,Citation46,Citation47,Citation49-Citation51 shows lifetime prevalence rates of DSMIII OCD from the Cross-national Collaborative Group. Lifetime prevalence of OCD varied from 0.7% in Taiwan to 2.5% in Puerto Rico. The studies in Englishlanguage sites showed excellent agreement, with lifetime prevalence of 2.2% to 2.3% in the USA, Canada, and New Zealand. Most remarkable about these rates is that they contradict the previous traditional view of OCD as a rare disorder on the basis of published clinical reports.Citation67
Table X. Lifetime prevalence rates for obsessive-compulsive disorder (OCD) in several community studies. ECA, Epidemiological Catchment Area survey.
On the other hand, in the Cross-national Collaborative Group data, the mean age at onset of OCD was the midtwenties to early thirties. The youngest mean age at onset was reported in Edmonton, Canada (21.9 years) and the oldest in Puerto Rico (35.5 years).
One epidemiological study has investigated the prevalence of OCD among adolescents and provided followup data regarding the course of OCD symptoms. ValleniBasile et alCitation68 surveyed a community sample of 3283 adolescents in the southeastern USA and found a 3% prevalence of OCD. They also identified a group of adolescents who had symptoms of OCD, but were not considered impaired. The prevalence of subclinical OCD, by this definition, was 19%. In a separate study, Valleni-Basile et alCitation68 found that the 1-year incidence rate of OCD in this population was 0.7%. Interestingly, an initial diagnosis of subclinical OCD was not significantly predictive of a diagnosis of OCD at 1-year follow-up. The authors concluded that an initial diagnosis of subclinical OCD was not a precursor to the development of clinical OCD with impairment of functioning.
In the ECA study, prevalence rates of OCD were higher among women than men. However, when gender comparisons were controlled for marital status, employment status, job status, ethnicity, and age, there were no remaining differences in prevalence rates for women and men. In the Cross-national Collaborative Study, rates were generally higher in women, except in Munich, where the rates were higher among men.
At least one prospective epidemiological study has suggested candidate risk factors for OCD. Crum and Anthony used data from the ECA study to estimate the degree to which the risk of OCD might be elevated among adults actively using cocaine.Citation69 Using 1-year prospective follow-up data, they identified 105 incident cases of OCD among 13 306 at-risk study participants. Subjects actively using cocaine were at substantially increased risk for OCD.
In the Cross-national Collaborative Study, persons with OCD were found to have a substantially greater risk of having comorbid major depression or another anxiety disorder compared with persons without OCD across all sites, even though the comorbidity rates and the magnitude of the risk varied by site. The proportion of persons with OCD and any anxiety disorder was higher than the proportion with major depression at all sites.Citation70
Posttraumatic stress disorder
Diagnosis
PTSD is defined in DSM-III as a constellation of symptoms in response to a stressor, including reexperiencing a traumatic event, a numbing of responsiveness, and symptoms of an increased level of arousal.Citation71,Citation72
In DSM-III-R, the symptoms are required to persist for at least 1 month and the criteria are broadened by adding intense psychological distress in response to events that symbolize or resemble an aspect of the trauma and avoidance of stimuli associated with the event.Citation73 In DSM-IV, the requirement for functional impairment or clinically significant distress is added.Citation74
Symptoms (acute 2-4 weeks; chronic >4 weeks)
Reexperiencing a traumatic event in recollections, dreams, flashbacks.
Avoidance of stimuli associated with the event.
Sleep disturbances, hypervigilance.
Prevalence
Until recently, accurate information on the prevalence of PTSD was not available. Earlier studies on the effects of traumatic experiences tended to focus on groups who had been exposed to a common trauma, such as Vietnam War veterans or survivors of natural disasters. However, in the last decade, several surveys have gathered general population data, which have enhanced our knowledge of the extent and seriousness of the impact of PTSD on the community.
Table XI Citation75-Citation78 presents lifetime prevalence rates of PTSD from five surveys conducted in the USA using DSM-III or DSM-III-R diagnostic criteria.Citation79 The DSM-III studies, which were both part of the ECA and used the DIS as the diagnostic instrument, found a low lifetime prevalence rate of 1.0 to 1.3 per 100 subjects. More importantly, these and other studies using DSM-III generated reliable, systematic data on the nature of the response to various traumas, including criminal victimization, sexual assault, natural disaster, and combat.Citation80 This empirical information contributed to the revisions of the diagnostic criteria in DSM-III-R. The early studies also resulted in a better understanding of the effects of trauma and improvements in the assessment of populations for the presence of traumatic life events and the symptoms of PTSD.
Table XI. Lifetime prevalence rates of posttraumatic stress disorder (PTSD) in several community studies. DSM, Diagnostic and Statistical Manual of Mental Disorders.
Later studies using DSM-III-R criteria found a lifetime prevalence of PTSD ranging from 10.4 to 12.3 per 100 women and 5.0 to 6.0 per 100 men. The latter studies seem to confirm that PTSD is a highly prevalent disorder, and also provide evidence that the traumatic events causing PTSD are experienced quite commonly in the community. In the NCS, 61% of men and 51% of women reported at least one traumatic event.Citation81 Men were more likely than women to experience physical attacks, combat, being threatened with a weapon, held captive, or kidnapped. Women were more likely to experience rape, sexual molestation, childhood parental neglect, and childhood physical abuse.
However, epidemiological studies of PTSD have often assessed at-risk groups of survivors of specific type of trauma, such as veterans of armed conflicts, displaced persons and refugees, and victims of range of criminal acts, including sexual assaults,Citation82 terrorist attacks,Citation83 and torture.Citation84 On the other hand, the epidemiological data suggest that the relationship between trauma exposure and development of PTSD is complex. Men and women differ in the types of traumas to which they are likely to be exposed, and they differ in their liability to develop PTSD once exposed. The lifetime prevalence of PTSD is significantly higher in women than in men. Women are more likely than men to be exposed to ”high-impact“ traumas, or traumas that are associated with a high probability of developing PTSD. Furthermore, once exposed to traumatic events, a higher proportion of women than men go on to develop PTSD. The vast majority of men and women who met criteria for DSM-III-R PTSD also had a lifetime history of at least one other psychiatric disorder.
Conclusion
Epidemiology can contribute to resolution of several key issues. More generally speaking, the epidemiological methodology is a prerequisite for our knowledge about how frequent mental disorders are in different countries, regions, and settings (primary care, schools, hospitals) and how they vary with time and with other individual and social and cultural characteristics. Epidemiology is, from this perspective, important for public health, notably the planning and harmonizing of health care components in the European Community, for example.
Epidemiology is also essential for basic and applied research questions. Clinical and laboratory research can never answer some questions because of their specific selection effect of patients, which usually includes a disproportionally high number of more severe complex cases. Needless to say, such selection effects can modify the results and may lead to erroneous conclusions about the effectiveness of one particular intervention or the mechanisms involved. This is particularly clear for preventive programs. For instance, we cannot simply use data from university hospitals, which frequently treat the most complicated cases, for designing such programs.Citation23 Perhaps the most fascinating use of epidemiology lies, however, in the field of causal epidemiology, ie, the identification of the complex interactions between the various pathogenic factors that appear to be responsible for most forms of mental disorders. Current state-of-the-art research on mental disorders suggests that the onset - as well as the whole illness progression - of most forms of mental disorders, can best be described by a disorderspecific vulnerability stress model. Given vulnerabilities - either genetically transmitted or learned by socialization - come together or interact with specific triggers, frequently summarized under various stress models leading to the development of the disorder. In this respect, epidemiology offers several methods for specifically identifying these critical interactions, such as familial genetic methods and more complex statistical manipulations (multivariate, discrete survival models) that require large and unbiased representative data sets.
Despite methodological limitations, lifetime prevalence rates of PD are remarkably consistent across community studies and across cultural, racial, and ethnic boundaries. The exception of higher rates in the NCS may relate to differences in interview method and the much lower rates in Taiwan, where lower rates were reported for several disorders. Cross-nationally, PD is consistently associated with substantial levels of occupational impairment and is more common among women than men. PD is highly comorbid with agoraphobia and major depression.
In contrast to PD, the epidemiological data on agoraphobia show considerable variation in rates across studies and cross-culturally. A recent clinical reappraisal of the ECA data suggests that community studies relying on the DIS and DSM-IV may have overestimated the prevalence of agoraphobia without panic. Therefore, the prevalence estimates from studies such as these should be regarded with caution until the accuracy of their prevalence figures on agoraphobia can be more thoroughly tested.
The ECA and NCS studies found that prevalence rates of SP were highest among women, those with less education or income, and those who have never been married. PTSD and GAD are more prevalent among women than men. On the basis of community data, OCD is a much more prevalent disorder than suggested by previous clinical studies.
Community studies have shown that anxiety disorders are highly prevalent and important causes of functional impairment. Data on anxiety disorders are interesting both for their consistency across quite different settings and for some of the questions they raise. Further study is needed to better understand the comorbidity between anxiety disorders, the consistently higher rates of anxiety disorders in women, and the differential effects of socioeconomic and cultural factors on PD and phobias. Further investigation of the complex relationship between exposure to traumatic events and the development of PTSD is needed.
There are three lines of research in epidemiology that will be of increasing importance in the near future:
The development of assessment of disability and quality of life.
Longitudinal studies of the progression of the symptoms, such as early symptoms.
Familial genetic studies.
Finally, for all of the anxiety disorders, we need epidemiological data to answer basic questions regarding etiology and prevention, as well as clinical studies to improve treatment and prevent disability caused by these highly prevalent disorders.
Selected abbreviations and acronyms
| CIDI | = | composite international diagnostic interview |
| IMS | = | diagnostic interview schedule |
| ECA | = | Epidemiological Catchment Area (survey) |
| GAD | = | generalized anxiety disorder |
| GHS | = | The German National Health Interview and Examination Survev |
| NCS | = | National Comorbidity Survey |
| OCD | = | obsessive-compulsive disorder |
| PD | = | panic disorder |
| PTSD | = | posttraumatic stress disorder |
| RBA | = | recurrent brief anxiety |
| RBD | = | recurrent brief depression |
| SP | = | social phobia |
REFERENCES
- DickeyM.Anxiety Disorders. Washington, DC: National Institute of Mental Health;1997
- RakelRE.Differential diagnosis of anxiety.Psychiatr Ann.198111(suppl 11)1114
- KleinDF.Anxiety reconceptualized. In: Klein DF, Rabkin JG, eds.Anxiety. New Research and Changing Concepts. New York, NY: Raven Press;1981235264
- American Psychiatric Association.Diagnostic and Statistical Manual of Mental Disorders. 3rd ed. Washington, DC: American Psychiatric Association;1980
- American Psychiatric Association.Diagnostic and Statistical Manual of Mental Disorders. 3rd ed, revised. Washington, DC: American Psychiatric Association;1987
- World Health Organization.International Classification of Diseases. 9th Revision. Geneva, Switzerland: World Health Organization;1977177213
- WittchenHU.Natural Course and Spontaneous Remissions of Untreated Anxiety Disorders: Results of the Munich Follow-up Study (MFS). Panics and Phobias. Vol 2. Berlin, Germany: Springer Verlag;1986
- RégnierD.MyersJK.KramerM.et al.The epidemiology of anxiety disorders: the Epidemiological Catchment Area (ECA) experience.J Psychiatr Res.199024(suppl 2)3142280373
- American Psychiatric Association.Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association;1994
- World Health Organization.The ICD-10 Classification of Mental and Behavioral Disorders. Clinical descriptions and diagnostic guidelines. Geneva, Switzerland: World Health Organization;1992
- KesslerRC.McGonagleKA.ZhaoS.et al.Lifetime and 12 month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch GenPsychiatry.199451819
- AngstJ.WickiW.The Zurich study. XIII. Recurrent brief anxiety.Eur Arch Psychiatry Clin Neurosci.19922412963001606193
- LepineJP.ParienteP.BoulangerJP.et al.Anxiety disorders in a French general psychiatric outpatient sample.Soc Psychiatry Psychiatr Epidemiol.1989243013082512648
- LepineJP.LellouchJ.Etude épidémiologique des troubles dépressifs et anxieux dans une population générale.Ann Med Psychol.1993151618623
- KesslerRC.KellerMB.WittchenHU.The epidemiology of generalized anxiety disorder.Psychiatr Clin North Am.200124193911225507
- BrownGW.HarrisTQ.EalsMJ.Social factors and comorbidity of depressive and anxiety disorders.Br J Psychiatry.1996168(suppl 30)5057
- WittchenHU.HoyerJ.Generalized anxiety disorder: nature and course.J Clin Psychiatry.200162(suppl 11)151911414546
- WittchenHU.Generalized anxiety disorder: prevalence, burden and cost to society.Depress Anxiety.20021616217112497648
- MartinP.Richard-BertheC.LepineJP.Disability and mental disorders among primary care patients: a French perspective.Fund Clin Pharmacol.2000897
- MartinP.BayleF.SeptienL.et al.Comparative pharmacoepidemiologic studies in primary care and psychiatric pratice: assessments of disability, quality of life and mental disorders.Pharmacologist.200244(suppl 1)16
- KesslerRC.The epidemiology of pure and comorbid generalized anxiety disorder: a review and evaluation of recent research.Acta Psychiatr Scand Suppl.200040671311131470
- BlazerDG.HughesD.GeorgesLK.et al.Generalized anxiety disorder. In: Robins LN, Regier DA, eds.Psychiatric Disorders in America: The Epidemiological Catchment Area Study. New York, NY: The Free Press;1991180203
- StefansonJG.LindalE.BjornssonJK.et al.Lifetime prevalence of specific mental disorders among people born in Iceland in 1931 .Acta Psychiatr Scand.1991841421491950608
- ChenC.WongJ.LeeN.et al.The Shatin community mental health survey in Hong Kong. II. Major findings.Arch Gen Psychiatry.1993501251338427552
- FavarelliC.Degl'innocentiBG.GiardinelliL.Epidemiology of anxiety disorders in Florence.Acta Psychiatr Scand.1989793083122786666
- WittchenHU.ZhaoS.KesslerR.et al. DSM-III-R generalized anxiety disorder in the national comorbidity survey.Arch Gen Psychiatry.1994513553648179459
- WittchenHU.NelsonCB.LachnerG.Prevalence of mental disorders and psychosocial impairments in adolescents and young adults.Psychol Med.199828287294
- WeissmanMM.MyersJK.HardingPS.Psychiatric disorders in a US urban community: 1975-1976.Am J Psychiatry.1978135459462637143
- CanalsJ.DomenechE.CarbajoG.et al.Prevalence of DSM-III-R and ICD10 psychiatric disorders in a Spanish population of 18 years olds.Acta Psychiatr Scand.1997962872949350958
- JenkinsR.LewisG.BebbingtonP.et al.The National Psychiatric Morbidity surveys of Great Britain: initial findings from the household survey.Psychol Med.1997277757899234456
- BhagwanjeeA.ParekhA.ParukZ.et al.Prevalence of minor psychiatric disorders in an adult African rural community in South Africa.Psychol Med.199828113711479794021
- GaterR.TransellaM.KortenA.et al.Sex differences in the prevalence and detection of depressive and anxiety disorders in general health care settings.Am J Psychiatry.199855405413
- AngstJ.Dobler-MikolaA.ScheideggerP.A panel study of anxiety states, panic attacks, and phobia among young adults. Presented at the Research Conference on Anxiety Disorders, Panic Attacks and Phobia. December 9, 1982; Key Biscayne, Fla.
- AngstJ.Dobler-MikolaA.BinderJ.The Zurich Study: a prospective epidemiological study of depressive, neurotic and psychosomatic syndromes.Eur Arch Psychiatr Neurol Sci.19842341320
- OffordDR.BoyleMH.CampbellD.et al.One-year prevalence of psychiatric disorder in Ontarians 15-64 years of age.Can J Psychiatry.1996415595638946078
- FeehanM.McGeeR.RajaSN.et al. DSM-III-R disorders in New Zealand 18 years olds.Aust N Z J Psychiatry.19942887998067973
- CarterRM.WittchenHU.PfisterH.et al.One year prevalence of subthreshold and threshold DSM-IV generalized anxiety disorder in a nationally representative sample.Depress Anxiety.20013788811301924
- WittchenHU.PfisterH.eds.Manual und Durchfuehrungsbeschreibung des DIA-X-M-CIDI. Frankfurt, Germany: Swets and Zeitlinger;1997
- RouillonF.ThalassinosM.FerreriM.et al.Clinical and epidemiological study of general anxiety disorders in general pratice.L'Encéphale.199420103110
- MaierW.GaensickeM.FreybergerHJ.et al.Generalized anxiety disorder (ICD-10) in primary care from a cross-cultural perspective a valid diagnostic entity? ActaPsychiatr Scand.20001012936
- UstunTB.SartoriusN.eds.Mental Illness in General Health Care. An international Study. Chichester UK: John Wiley and sons;1995
- RakelRE.Anxiety and the primary care physian.Primary Psychiatry.200185258
- LecrubierY.WittchenHU.FaravelliC.et al.A European perspective on social anxiety disorder.Eur Psychiatry.20001551610713797
- WeillerE.BisserbeJC.MaierW.et al.Prevalence and recognition of anxiety syndromes in five European primary care settings.Br J Psychiatry.1998173(suppl 34)1823
- EatonWW.KesslerRC.WittchenHU.MageeWJ.Panic and panic disorder in the United States.Am J Psychiatry.19941514134208109651
- BlandRC.NewmanSC.OrnH.Period prevalence of psychiatric disorders in Edmonton.Acta Psychiatr Scand.198877(suppl 338)32423279720
- CaninoGJ.BirdHR.ShroutPE.et al.The prevalence of specific psychiatric disorders in Puerto Rico.Arch Gen Psychiatry.1987447277353498456
- KaramE.War events and depression in Lebanon. Presented at a seminar of the International Traumatic Stress Society, Washington DC, October 26, 1991
- HwuHG.YehEK.ChangLY.Prevalence of psychiatric disorders in Taiwan defined by the Chinese Diagnostic Interview Schedule.Acta Psychiatr Scand.1989791361472923007
- LeeCK.HanJH.ChoiJO.The epidemiological study of mental disorders in Korea (IX). Alcoholism anxiety and depression.Seoul J Psychiatry.198712183191
- Oakley-BrowneMA.JoycePR.WellsJE.BushnellJA.HornblowAR.Christchurch Psychiatric Epidemiology Study. Part II: Six month and other period prevalences for specific psychiatric disorders.Aust N Z J Psychiatry.1989233273402803145
- LindalE.StefanssonJG.The lifetime prevalence of anxiety disorders in Iceland as estimated by the US National Institute of Mental Health Diagnostic Interview Schedule.Acta Psychiatr Scand.19938829348372693
- WeissmanMM.CaninoGJ.GreenwaldS.et al.Current rates and symptom profiles of panic disorder in six cross-national studies.Clin Neuropharmacol.199518(suppl 2)5156
- WeissmanMM.BlandRC.CaninoGJ.et al.The Cross-national epidemiology of panic disorder.Arch Gen Psychiatry.1997543053099107146
- KeylPM.EatonWW.Risk factor for the onset of panic attack and panic disorder.Am J Epidemiol.19901313013112296982
- KesslerRC.StangPE.WittchenHU.et al.Lifetime panic depression comorbidity in the national comorbidity survey.Arch Gen Psychiatry.1998558018089736006
- MarksIM.Fears, Phobias and Rituals. Panic, Anxiety and Their Disorders. New York, NY: Oxford University Press;1978
- LepineJP.PelissoloA.Comorbidity and social phobia: clinical and epidemiological issues.IntChin Psychopharmacol.199611(suppl 3)3541
- BurnLe.ThorpeGL.Epidemiology of fears and phobias (with particular reference to the national survey of agoraphobics).J Int Med Res.1977517
- MageeWS.EatonWW.WittchenHU.McGonagleKA.KesslerRC.Agoraphobia, simple phobia, and social phobia in National Comorbidity Survey.Arch Gen Psychiatry.1996531591688629891
- KesslerRC.StangP.WittchenHU.et al.Lifetime comorbidities between social phobia and mood disorders in the US National comorbidity survey.Psychol Med.19992955556710405077
- AngstJ.Dobler-MikolaA.The Zurich study V. Anxiety and phobia in young adults.Eur Arch Psychiatry Neurosci.1985235171178
- SchneierFR.JohnsonJ.HornigCD.et al.Social phobia: comorbidity and morbidity in an epidemiologic sample.Arch Gen Psychiatry.1992492822881558462
- HollanderE.Obsessive-compulsive disorder: the hidden epidemic.J Clin Psychiatry.199758(suppl 12)369393389
- SteketeeG.Disability and family burden in obsessive-compulsive disorder.Can J Psychiatry.1997429199289429061
- Van OppenP.HoekstraRJ.EmmelkampPMG.The structure of obsessive-compulsive symptoms.Behav Res Ther.19953315237872933
- BebbingtonPE.Epidemiology of obsessive-compulsive disorder.Br J Psychiatry.1998173(suppl 35)26
- Valleni-BasileLA.GarrisonCZ.JacksonKL.et al.Frequency of obsessive-compulsive disorder in a community sample of young adolescents.J Am Acad Child Adoiesc Psychiatry.199433782791
- CrumRM.AnthonyJC.Cocaine use and other suspected risk factors for obsessive-compulsive disorder: a prospective study with data from ECA surveys.Drug Alcohol Depend.1993312812958462416
- HollanderE.GreenwaldS.NevilleD.JohnsonJ.HornigCD.WeissmanMM.Uncomplicated and comorbid obsessive compulsive disorder in an epidemiologic sample.Depress Anxiety.1996-9741111199166639
- HalesRE.ZatzickDF.What is PTSD?Am J Psychiatry.19971541431459016259
- JonesJC.BarlowDH.The etiology of post-traumatic stress disorder.Clin Psychol Rev.199010299328
- EmilienG.PenasseC.CharlesG.et al.Posttraumatic stress disorder: hypotheses from clinical neuropsychology and psychopharmacology research.Int J Psychol Clin Pract.20004318
- BirmesP.HattonL.BurnetA.SchmittL.Early historical literature for posttraumatic symptomatology.Stress Health.2003191726
- HelzerJE.RobinsLN.McEvoyL.Posttraumatic stress disorder in the general population: findings of Epidemiological Catchment Area survey.N Engl J Med.1987317163016343683502
- DavidsonJRT.HughesD.BlazerDG.et al.Posttraumatic stress disorder in the community: an epidemiologic study.Psychol Med.1991217137211946860
- KesslerRC.SonegaA.BrometE.et al.Posttraumatic stress disorder in the National Comorbidity Survey.Arch Gen Psychiatry.199552104810607492257
- BreslauN.KesslerRC.ChilcoatHD.et al.Traumatic and posttraumatic stress disorders in the community: the 1996 Detroit Area Survey of Trauma.Arch Gen Psychiatry.1995556266319672053
- BreslauN.DavisGC.AndreskiP.et al.Epidemiologic findings on PTSD and comorbid disorders in the general population. In: Dohrenwend B, ed.Adversity, Stress and Psychopathology. New York, NY: Oxford University Press;1998319330
- NorrisFH.Epidemiology of trauma: frequency and impact of different potentially traumatic events on different demographic groups.J Consult Clin Psychol.1992604094181619095
- PerkoniggA.KesslerRC.StorzS.et al.Traumatic events and posttraumatic stress disorder in the community prevalence risk factors and comorbidity. ActaPsychiatr Scand.20001014659
- BrunelloN.DavidsonJR.DeahlM.et al.Posttraumatic stress disorder: diagnosis and epidemiology, comorbidity and social consequences, biology and treatment.Neuropsychobiology.20014315016211287794
- AbenhaimL.DabW.SalmiL.Study of civilian victims of terrorist attacks.J Clin Epidemiol.1992451031091573426
- BasogluM.MinekaS.ParkerM.et al.Psychological preparedness for trauma as a protection factor in survivors of torture.Psychol Med.199727142114339403913